Application of Behaviour Change Techniques in Promoting Physical Activity Among Adults with Chronic Conditions: An Umbrella Review
Abstract
1. Introduction
2. Methods
2.1. Search Strategy
2.2. Eligibility Criteria
2.2.1. Population
2.2.2. Intervention
2.2.3. Comparison
2.2.4. Outcomes
2.2.5. Study Design
2.2.6. Eligibility Assessment and Data Extraction
2.3. Quality Assessment
2.4. Data Analysis and Synthesis
3. Results
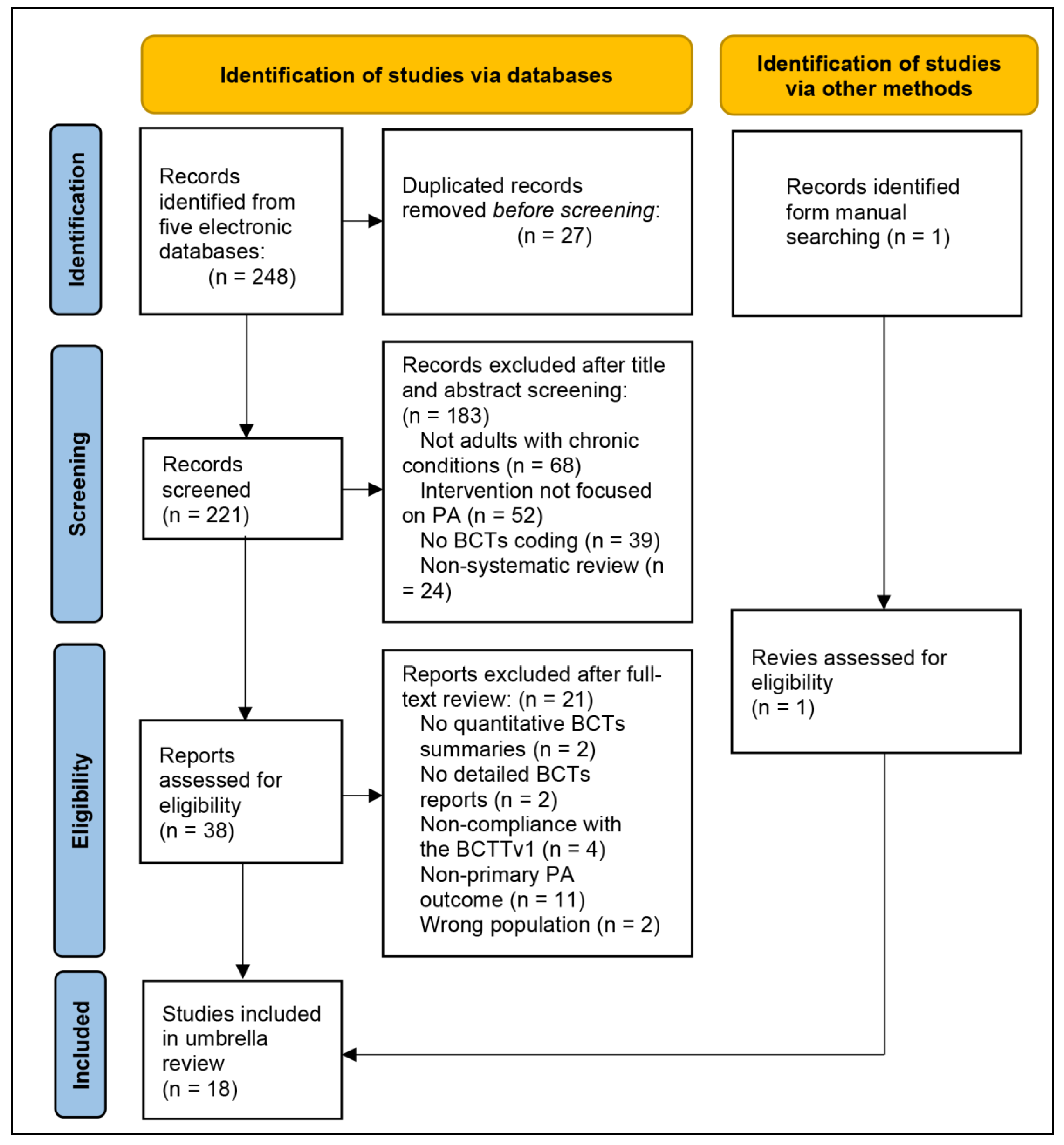
3.1. Study Inclusion
3.2. Quality of the Evidence
3.3. Characteristics of Included Studies
3.4. PA Intervention Efficiency and BCT Applications
3.5. Characteristics of BCT Application Across Different CC
3.5.1. Metabolic Conditions
3.5.2. Cardiovascular Conditions
3.5.3. Musculoskeletal Conditions
3.5.4. Mixed/General Chronic Conditions
3.5.5. Cancer
4. Discussion
4.1. Overview of Key Findings on BCT Effectiveness
4.2. Condition-Specific BCT Application
4.3. Integration and Implications
4.4. Strengths and Limitations of the Evidence Base
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Agirre-Elordui, S., Fernandez-Landa, J., Olasagasti-Ibargoien, J., & Castaneda-Babarro, A. (2024). Physical activity maintenance in colorectal cancer survivors after an exercise intervention applying behaviour change techniques: A systematic review and meta-analysis. Journal of Cancer Survivorship. early access. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, S., Lazo Green, K., McGarrigle, L., Money, A., Pendleton, N., & Todd, C. (2024). Interventions based on behaviour change techniques to encourage physical activity or decrease sedentary behaviour in community-dwelling adults aged 50–70: Systematic review with intervention component analysis. Journal of Aging and Physical Activity, 32(4), 554–577. [Google Scholar] [CrossRef] [PubMed]
- Alqahtani, S. (2022). Are Us Adults with Chronic Health Conditions Meeting Public Health Recommendations For Physical Activity? Medicine & Science in Sports & Exercise, 54(9S), 53. [Google Scholar] [CrossRef]
- Anderson, E., & Durstine, J. L. (2019). Physical activity, exercise, and chronic diseases: A brief review. Sports Medicine and Health Science, 1(1), 3–10. [Google Scholar] [CrossRef]
- Aromataris, E., Fernandez, R., Godfrey, C., Holly, C., Khalil, H., & Tungpunkom, P. (2020). Chapter 10: Umbrella reviews. In E. Aromataris, & Z. Munn (Eds.), Joanna Briggs Institute reviewer’s manual. The Joanna Briggs Institute. Available online: https://synthesismanual.jbi.global (accessed on 2 May 2025).
- Ashley, K., Tang, M. Y., Flynn, D., Cooper, M., Errington, L., & Avery, L. (2024). Identifying the active ingredients of training interventions for healthcare professionals to promote and support increased levels of physical activity in adults with heart failure: A systematic review. Health Psychology Review, 18(2), 319–340. [Google Scholar] [CrossRef]
- Bandura, A. (2013). Health promotion from the perspective of social cognitive theory. In Understanding and changing health behaviour (pp. 299–339). Psychology Press. [Google Scholar]
- Beaglehole, R., Bonita, R., Horton, R., Adams, C., Alleyne, G., Asaria, P., Baugh, V., Bekedam, H., Billo, N., Casswell, S., Cecchini, M., Colagiuri, R., Colagiuri, S., Collins, T., Ebrahim, S., Engelgau, M., Galea, G., Gaziano, T., Geneau, R., … Alliance, N. C. D. (2011). Priority actions for the non-communicable disease crisis. The Lancet, 377(9775), 1438–1447. [Google Scholar] [CrossRef]
- Blicher-Hansen, J., Chilcot, J., & Gardner, B. (2024). Experiences of successful physical activity maintenance among adults with type 2 diabetes: A theory-based qualitative study. Psychology & Health, 39(3), 399–416. [Google Scholar]
- Bull, F. C., Al-Ansari, S. S., Biddle, S., Borodulin, K., Buman, M. P., Cardon, G., Carty, C., Chaput, J. P., Chastin, S., Chou, R., Dempsey, P. C., DiPietro, L., Ekelund, U., Firth, J., Friedenreich, C. M., Garcia, L., Gichu, M., Jago, R., Katzmarzyk, P. T., … Willumsen, J. F. (2020). World Health Organization 2020 guidelines on physical activity and sedentary behaviour. British Journal of Sports Medicine, 54(24), 1451–1462. [Google Scholar] [CrossRef]
- Carraca, E., Encantado, J., Battista, F., Beaulieu, K., Blundell, J., Busetto, L., van Baak, M., Dicker, D., Ermolao, A., Farpour-Lambert, N., Pramono, A., Woodward, E., Bellicha, A., & Oppert, J. M. (2021). Effective behaviour change techniques to promote physical activity in adults with overweight or obesity: A systematic review and meta-analysis. Obesity Reviews, 22(Suppl. 4), e13258. [Google Scholar] [CrossRef]
- Carver, C., & Scheier, M. (1998). On the self-regulation of behaviour. Cambridge University Press. [Google Scholar] [CrossRef]
- Cooper, K. B., Lapierre, S., Carrera Seoane, M., Lindstrom, K., Pritschmann, R., Donahue, M., Christou, D. D., McVay, M. A., & Jake-Schoffman, D. E. (2023). Behaviour change techniques in digital physical activity interventions for breast cancer survivors: A systematic review. Translational Behavioral Medicine, 13(4), 268–280. [Google Scholar] [CrossRef] [PubMed]
- de Leeuwerk, M. E., Bor, P., van der Ploeg, H. P., de Groot, V., van der Schaaf, M., van der Leeden, M., & consortium, O. (2022). The effectiveness of physical activity interventions using activity trackers during or after inpatient care: A systematic review and meta-analysis of randomized controlled trials. International Journal of Behavioral Nutrition and Physical Activity, 19(1), 59. [Google Scholar] [CrossRef]
- Duff, O. M., Walsh, D. M., Furlong, B. A., O’Connor, N. E., Moran, K. A., & Woods, C. B. (2017). Behaviour change techniques in physical activity eHealth interventions for people with cardiovascular disease: Systematic review. Journal of Medical Internet Research, 19(8), e281. [Google Scholar] [CrossRef]
- Ester, M., Eisele, M., Wurz, A., McDonough, M. H., McNeely, M., & Culos-Reed, S. N. (2021). Current evidence and directions for future research in eHealth physical activity interventions for adults affected by cancer: Systematic review. JMIR Cancer, 7(3), e28852. [Google Scholar] [CrossRef]
- Finne, E., Glausch, M., Exner, A. K., Sauzet, O., Stolzel, F., & Seidel, N. (2018). Behaviour change techniques for increasing physical activity in cancer survivors: A systematic review and meta-analysis of randomized controlled trials. Cancer Management and Research, 10, 5125–5143. [Google Scholar] [CrossRef]
- Forechi, L., Mill, J. G., Griep, R. H., Santos, I., Pitanga, F., & Molina, M. (2018). Adherence to physical activity in adults with chronic diseases: ELSA-Brasil. Revista de Saúde Pública, 52, 31. [Google Scholar] [CrossRef]
- GBD 2019 Diseases and Injuries Collaborators. (2020). Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet, 396(10258), 1204–1222. [Google Scholar] [CrossRef]
- GBD 2019 Risk Factors Collaborators. (2020). Global burden of 87 risk factors in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. The Lancet, 396(10258), 1223–1249. [Google Scholar] [CrossRef] [PubMed]
- Gillison, F. B., Rouse, P., Standage, M., Sebire, S. J., & Ryan, R. M. (2019). A meta-analysis of techniques to promote motivation for health behaviour change from a self-determination theory perspective. Health Psychology Review, 13(1), 110–130. [Google Scholar] [CrossRef] [PubMed]
- Greaves, C. J., Sheppard, K. E., Abraham, C., Hardeman, W., Roden, M., Evans, P. H., Schwarz, P., & Group, I. S. (2011). Systematic review of reviews of intervention components associated with increased effectiveness in dietary and physical activity interventions. BMC Public Health, 11, 119. [Google Scholar] [CrossRef] [PubMed]
- Grimmett, C., Corbett, T., Brunet, J., Shepherd, J., Pinto, B. M., May, C. R., & Foster, C. (2019). Systematic review and meta-analysis of maintenance of physical activity behaviour change in cancer survivors. International Journal of Behavioral Nutrition and Physical Activity, 16(1), 37. [Google Scholar] [CrossRef]
- Gude, W. T., & Peek, N. (2019). Control theory to design and evaluate audit and feedback interventions. In Applied interdisciplinary theory in health informatics (pp. 159–170). IOS Press. [Google Scholar]
- Hagger, M. S., Moyers, S., McAnally, K., & McKinley, L. E. (2020). Known knowns and known unknowns on behaviour change interventions and mechanisms of action. Health Psychology Review, 14(1), 199–212. [Google Scholar] [CrossRef]
- Hailey, V., Rojas-Garcia, A., & Kassianos, A. P. (2022). A systematic review of behaviour change techniques used in interventions to increase physical activity among breast cancer survivors. Breast Cancer, 29(2), 193–208. [Google Scholar] [CrossRef]
- Hallward, L., Patel, N., & Duncan, L. R. (2020). Behaviour change techniques in physical activity interventions for men with prostate cancer: A systematic review. Journal of Health Psychology, 25(1), 105–122. [Google Scholar] [CrossRef]
- Kirvalidze, M., Abbadi, A., Dahlberg, L., Sacco, L. B., Calderon-Larranaga, A., & Morin, L. (2023). Estimating pairwise overlap in umbrella reviews: Considerations for using the corrected covered area (CCA) index methodology. Research Synthesis Methods, 14(5), 764–767. [Google Scholar] [CrossRef]
- Knittle, K., Nurmi, J., Crutzen, R., Hankonen, N., Beattie, M., & Dombrowski, S. U. (2018). How can interventions increase motivation for physical activity? A systematic review and meta-analysis. Health Psychology Review, 12(3), 211–230. [Google Scholar] [CrossRef] [PubMed]
- Lau, Y., Chew, H. S. J., Ang, W. H. D., Ang, W. W., Yeo, C. Y., Lim, G. Z. Q., Wong, S. H., Lau, S. T., & Cheng, L. J. (2024). Effects of digital health interventions on the psychological outcomes of perinatal women: Umbrella review of systematic reviews and meta-analyses. Health Psychology Review, 18(2), 229–254. [Google Scholar] [CrossRef] [PubMed]
- Lin, H., Xu, D., Yang, M., Ma, X., Yan, N., Chen, H., He, S., & Deng, N. (2022). Behaviour change techniques that constitute effective planning interventions to improve physical activity and diet behaviour for people with chronic conditions: A systematic review. BMJ Open, 12(8), e058229. [Google Scholar] [CrossRef] [PubMed]
- Ma, J. K., Ramachandran, S., Sandhu, A., Tsui, K., Hoens, A., Hu, D., & Li, L. C. (2022). Tailored interventions for supporting physical activity participation in people with arthritis and related conditions: A systematic review. Current Treatment Options in Rheumatology, 8, 117–142. [Google Scholar] [CrossRef]
- Marley, J., Tully, M. A., Porter-Armstrong, A., Bunting, B., O’Hanlon, J., Atkins, L., Howes, S., & McDonough, S. M. (2017). The effectiveness of interventions aimed at increasing physical activity in adults with persistent musculoskeletal pain: A systematic review and meta-analysis. BMC Musculoskeletal Disorders, 18(1), 482. [Google Scholar] [CrossRef]
- Mbous, Y. P., Patel, J., & Kelly, K. M. (2020). A systematic review and meta-analysis of physical activity interventions among colorectal cancer survivors. Translational Behavioral Medicine, 10(5), 1134–1143. [Google Scholar] [CrossRef]
- Meade, L. B., Bearne, L. M., Sweeney, L. H., Alageel, S. H., & Godfrey, E. L. (2019). Behaviour change techniques associated with adherence to prescribed exercise in patients with persistent musculoskeletal pain: Systematic review. British Journal of Health Psychology, 24(1), 10–30. [Google Scholar] [CrossRef] [PubMed]
- Meyer-Schwickerath, C., Morawietz, C., Baumann, F. T., Huber, G., & Wiskemann, J. (2022). Efficacy of face-to-face behaviour change counseling interventions on physical activity behaviour in cancer survivors—A systematic review and meta-analysis. Disability and Rehabilitation, 44(19), 5386–5401. [Google Scholar] [CrossRef]
- Michaelsen, M. M., & Esch, T. (2021). Motivation and reward mechanisms in health behaviour change processes. Brain Research, 1757, 147309. [Google Scholar] [CrossRef]
- Michie, S., Abraham, C., Whittington, C., McAteer, J., & Gupta, S. (2009). Effective techniques in healthy eating and physical activity interventions: A meta-regression. Health Psychology, 28(6), 690–701. [Google Scholar] [CrossRef]
- Michie, S., Ashford, S., Sniehotta, F. F., Dombrowski, S. U., Bishop, A., & French, D. P. (2011). A refined taxonomy of behaviour change techniques to help people change their physical activity and healthy eating behaviours: The CALO-RE taxonomy. Psychology & Health, 26(11), 1479–1498. [Google Scholar] [CrossRef]
- Michie, S., Richardson, M., Johnston, M., Abraham, C., Francis, J., Hardeman, W., Eccles, M. P., Cane, J., & Wood, C. E. (2013). The behaviour change technique taxonomy (v1) of 93 hierarchically clustered techniques: Building an international consensus for the reporting of behaviour change interventions. Annals of Behavioral Medicine, 46(1), 81–95. [Google Scholar] [CrossRef] [PubMed]
- Mozafarinia, M., Mate, K. K. V., Brouillette, M. J., Fellows, L. K., Knauper, B., & Mayo, N. E. (2024). An umbrella review of the literature on the effectiveness of goal setting interventions in improving health outcomes in chronic conditions. Disability and Rehabilitation, 46(4), 618–628. [Google Scholar] [CrossRef] [PubMed]
- Murray, J. M., Brennan, S. F., French, D. P., Patterson, C. C., Kee, F., & Hunter, R. F. (2017). Effectiveness of physical activity interventions in achieving behaviour change maintenance in young and middle aged adults: A systematic review and meta-analysis. Social Science & Medicine, 192, 125–133. [Google Scholar] [CrossRef]
- Olander, E. K., Fletcher, H., Williams, S., Atkinson, L., Turner, A., & French, D. P. (2013). What are the most effective techniques in changing obese individuals’ physical activity self-efficacy and behaviour: A systematic review and meta-analysis. International Journal of Behavioral Nutrition and Physical Activity, 10, 29. [Google Scholar] [CrossRef]
- Page, M. J., McKenzie, J. E., Bossuyt, P. M., Boutron, I., Hoffmann, T. C., Mulrow, C. D., Shamseer, L., Tetzlaff, J. M., Akl, E. A., Brennan, S. E., Chou, R., Glanville, J., Grimshaw, J. M., Hrobjartsson, A., Lalu, M. M., Li, T., Loder, E. W., Mayo-Wilson, E., McDonald, S., … Moher, D. (2021). The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ, 372, n71. [Google Scholar] [CrossRef]
- Patel, M. L., Cleare, A. E., Smith, C. M., Rosas, L. G., & King, A. C. (2022). Detailed versus simplified dietary self-monitoring in a digital weight loss intervention among racial and ethnic minority adults: Fully remote, randomized pilot study. JMIR Formative Research, 6(12), e42191. [Google Scholar] [CrossRef]
- Pedersen, B. K., & Saltin, B. (2015). Exercise as medicine—Evidence for prescribing exercise as therapy in 26 different chronic diseases. Scandinavian Journal of Medicine & Science in Sports, 25(Suppl. 3), 1–72. [Google Scholar] [CrossRef]
- Piercy, K. L., Troiano, R. P., Ballard, R. M., Carlson, S. A., Fulton, J. E., Galuska, D. A., George, S. M., & Olson, R. D. (2018). The physical activity guidelines for Americans. JAMA, 320(19), 2020–2028. [Google Scholar] [CrossRef]
- Pollock, M., Fernandes, R. M., Pieper, D., Tricco, A. C., Gates, M., Gates, A., & Hartling, L. (2019). Preferred Reporting Items for Overviews of Reviews (PRIOR): A protocol for development of a reporting guideline for overviews of reviews of healthcare interventions. Systematic Reviews, 8(1), 335. [Google Scholar] [CrossRef]
- Presseau, J., Ivers, N. M., Newham, J. J., Knittle, K., Danko, K. J., & Grimshaw, J. M. (2015). Using a behaviour change techniques taxonomy to identify active ingredients within trials of implementation interventions for diabetes care. Implementation Science, 10, 55. [Google Scholar] [CrossRef] [PubMed]
- Presseau, J., McCleary, N., Lorencatto, F., Patey, A. M., Grimshaw, J. M., & Francis, J. J. (2019). Action, actor, context, target, time (AACTT): A framework for specifying behaviour. Implementation Science, 14(1), 102. [Google Scholar] [CrossRef] [PubMed]
- Pynnonen, K., Hassandra, M., Tolvanen, A., Siltanen, S., Portegijs, E., & Rantanen, T. (2023). Do the integrated theories of self-determination and planned behaviour explain the change in active life engagement following a motivational counseling intervention among older people? Social Science & Medicine, 339, 116409. [Google Scholar] [CrossRef]
- Rezende, M., Brito, N., Farias, F., Silva, C., Cernigoy, C., da Silva, J. R., Moreira, M., Santana, O., Hissadomi, M., & Frucchi, R. (2021). Improved function and strength in patients with knee osteoarthritis as a result of adding a two-day educational program to usual care. Prospective randomized trial. Osteoarthritis and Cartilage Open, 3(1), 100137. [Google Scholar] [CrossRef]
- Rhodes, R. E., & Dickau, L. (2012). Experimental evidence for the intention-behaviour relationship in the physical activity domain: A meta-analysis. Health Psychology, 31(6), 724–727. [Google Scholar] [CrossRef]
- Samdal, G. B., Eide, G. E., Barth, T., Williams, G., & Meland, E. (2017). Effective behaviour change techniques for physical activity and healthy eating in overweight and obese adults; systematic review and meta-regression analyses. International Journal of Behavioral Nutrition and Physical Activity, 14(1), 42. [Google Scholar] [CrossRef]
- Sequeira, M., Pereira, C., & Alvarez, M.-J. (2023). Promoting physical activity within breast cancer survivors using behaviour change techniques: N-of-1 randomized controlled trials. Health Promotion International, 38(4), daad075. [Google Scholar] [CrossRef]
- Shea, B. J., Reeves, B. C., Wells, G., Thuku, M., Hamel, C., Moran, J., Moher, D., Tugwell, P., Welch, V., Kristjansson, E., & Henry, D. A. (2017). AMSTAR 2: A critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ, 358, j4008. [Google Scholar] [CrossRef]
- Sniehotta, F. F., Scholz, U., & Schwarzer, R. (2005). Bridging the intention–behaviour gap: Planning, self-efficacy, and action control in the adoption and maintenance of physical exercise. Psychology & Health, 20(2), 143–160. [Google Scholar]
- Stevens, M., Cruwys, T., & Murray, K. (2020). Social support facilitates physical activity by reducing pain. British Journal of Health Psychology, 25(3), 576–595. [Google Scholar] [CrossRef]
- Tamuleviciute-Prasciene, E., Beigiene, A., Lukauskaite, U., Gerulyte, K., Kubilius, R., & Bjarnason-Wehrens, B. (2022). Effectiveness of additional resistance and balance training and telephone support program in exercise-based cardiac rehabilitation on quality of life and physical activity: Randomized control trial. Clinical Rehabilitation, 36(4), 511–526. [Google Scholar] [CrossRef]
- Tang, H., Zhang, W., Weng, Y., Zhang, X., Shen, H., Li, X., Liu, Y., Liu, W., Xiao, H., & Jing, H. (2025). Dietary self-management behaviour and associated factors among breast cancer patients receiving chemotherapy: A latent profile analysis. European Journal of Oncology Nursing, 75, 102825. [Google Scholar] [CrossRef]
- Voss, M. L., Brick, R., Padgett, L. S., Wechsler, S., Joshi, Y., Ammendolia Tome, G., Arbid, S., Campbell, G., Campbell, K. L., El Hassanieh, D., Klein, C., Lam, A., Lyons, K. D., Sabir, A., Sleight, A. G., & Jones, J. M. (2024). Behaviour change theory and behaviour change technique use in cancer rehabilitation interventions: A secondary analysis. European Journal of Physical and Rehabilitation Medicine, 60(6), 1036–1050. [Google Scholar] [CrossRef]
- Warburton, D. E., Nicol, C. W., & Bredin, S. S. (2006). Health benefits of physical activity: The evidence. CMAJ, 174(6), 801–809. [Google Scholar] [CrossRef] [PubMed]
- Webb, J., Baker, A., Palmer, T., Hall, A., Ahlquist, A., Darlow, J., Olaniyan, V., Horlock, R., & Stewart, D. (2022). The barriers and facilitators to physical activity in people with a musculoskeletal condition: A rapid review of reviews using the COM-B model to support intervention development. Public Health in Practice, 3, 100250. [Google Scholar] [CrossRef] [PubMed]
- Willett, M., Duda, J., Fenton, S., Gautrey, C., Greig, C., & Rushton, A. (2019). Effectiveness of behaviour change techniques in physiotherapy interventions to promote physical activity adherence in lower limb osteoarthritis patients: A systematic review. PLoS ONE, 14(7), e0219482. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. (2023a). Noncommunicable diseases. Available online: https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases (accessed on 2 May 2025).
- World Health Organization. (2023b). Noncommunicable diseases: Key facts. Available online: https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases (accessed on 2 May 2025).
- Zhang, J., Brackbill, D., Yang, S., Becker, J., Herbert, N., & Centola, D. (2016). Support or competition? How online social networks increase physical activity: A randomized controlled trial. Preventive Medicine Reports, 4, 453–458. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X., Qiao, X., Peng, K., Gao, S., & Hao, Y. (2024). Digital behaviour change interventions to reduce sedentary behaviour and promote physical activity in adults with diabetes: A systematic review and meta-analysis of randomized controlled trials. International Journal of Behavioral Medicine, 31(6), 959–973. [Google Scholar] [CrossRef] [PubMed]
| BCT | Metabolic Conditions | Cardiovascular Conditions | Musculoskeletal Conditions | Mixed/General Chronic Conditions | Cancer | ✓ |  | ▲ | ▼ | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| (X. Zhang et al., 2024) | (Carraca et al., 2021) | (Ashley et al., 2024) | (Duff et al., 2017) | (Marley et al., 2017) | (Meade et al., 2019) | (Willett et al., 2019) | (de Leeuwerk et al., 2022) | (Lin et al., 2022) | (Agirre-Elordui et al., 2024) | (Cooper et al., 2023) | (Ester et al., 2021) | (Finne et al., 2018) | (Grimmett et al., 2019) | (Hailey et al., 2022) | (Hallward et al., 2020) | (Mbous et al., 2020) | (Meyer-Schwickerath et al., 2022) | |||||
| 1.1 | ✓ | ✓ ▲ ▲ | ✓ ▲ ▲ | ✓ ▲ ▲ | ✓▲ | ✓ ▲ ▲ | ✓ ▲ ▲ | ✓ ▲ ▲ | ✓ | ✓ ▲ ▲ | ✓ ▲ ▲ | ✓ | ✓ | ✓ ▲ ▲ | ✓ | ✓ | ✓ | 17 | 15 | 10 | 0 | |
| 1.2 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 17 | 9 | 0 | 0 | |
| 1.3 | ✓ | ✓▲ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 11 | 2 | 1 | 0 | |||||||
| 1.4 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓▲ | ✓ | ✓ ▲ ▲ | ✓ | ✓ | ✓ | ✓▲ | 16 | 6 | 3 | 0 | ||
| 1.5 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 16 | 3 | 0 | 0 | ||
| 1.6 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 9 | 0 | 0 | 0 | |||||||||
| 1.7 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 7 | 0 | 0 | 0 | |||||||||||
| 1.8 | ✓ | ✓ | ✓ | ✓▲ | ✓ | ✓ | 6 | 0 | 1 | 0 | ||||||||||||
| 1.9 | ✓ | ✓ | ✓ | ✓ | ✓ | 5 | 0 | 0 | 0 | |||||||||||||
| 2.1 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 7 | 0 | 0 | 0 | |||||||||||
| 2.2 | ✓ | ✓ | ✓ | ✓▲ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 17 | 8 | 1 | 0 | |
| 2.3 | ✓ | ✓ ▼ ▼ | ✓ | ✓ ▲ ▲ | ✓ | ✓ ▲ ▲ | ✓ | ✓ | ✓ | ✓ ▲ ▲ | ✓ | ✓ | ✓ | ✓▲ | ✓ | ✓ | ✓ | 17 | 15 | 4 | 1 | |
| 2.4 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 7 | 1 | 0 | 0 | |||||||||||
| 2.5 | ✓ | ✓ | ✓ | 3 | 0 | 0 | 0 | |||||||||||||||
| 2.6 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 6 | 0 | 0 | 0 | ||||||||||||
| 2.7 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 7 | 0 | 0 | 0 | |||||||||||
| 3.1 | ✓ | ✓ | ✓ | ✓▲ | ✓▲ | ✓ | ✓ ▲ ▲ | ✓ | ✓ | ✓ | ✓ ▲ ▲ | ✓ | ✓ ▲ ▲ | ✓ | ✓ | 15 | 8 | 5 | 0 | |||
| 3.2 | ✓ | ✓ | ✓▲ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 9 | 1 | 1 | 0 | |||||||||
| 3.3 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 7 | 1 | 0 | 0 | |||||||||||
| 4.1 | ✓ | ✓ | ✓▲ | ✓▲ | ✓ ▲ ▲ | ✓ ▲ ▲ | ✓ | ✓▲ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ ▲ ▲ | ✓ | 17 | 12 | 6 | 0 | |
| 4.2 | ✓ | ✓ | ✓ | ✓▲ | ✓ | 5 | 0 | 1 | 0 | |||||||||||||
| 4.3 | ✓ | 1 | 0 | 0 | 0 | |||||||||||||||||
| 5.1 | ✓ | ✓ | ✓ | ✓ ▲ ▲ | ✓ | ✓ | ✓▲ | ✓ | ✓ | ✓ | ✓ | ✓▼ | ✓ | ✓ | ✓ | ✓ | 16 | 7 | 2 | 1 | ||
| 5.2 | ✓ | ✓ | ✓ | 3 | 0 | 0 | 0 | |||||||||||||||
| 5.3 | ✓ | ✓▲ | ✓ | ✓ | ✓ | ✓ | ✓▲ | ✓ | 8 | 2 | 0 | 0 | ||||||||||
| 5.4 | ✓ | ✓ | 2 | 0 | 0 | 0 | ||||||||||||||||
| 5.6 | ✓ | ✓ | ✓▼ | ✓ | 4 | 0 | 0 | 1 | ||||||||||||||
| 6.1 | ✓ | ✓ | ✓ | ✓ | ✓ ▲ ▲ | ✓ | ✓ | ✓ ▲ ▲ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 15 | 3 | 2 | 0 | |||
| 6.2 | ✓ | ✓ | ✓▲ | ✓▲ | ✓ | ✓▼ | ✓ | 7 | 0 | 2 | 1 | |||||||||||
| 6.3 | ✓ | 1 | 0 | 0 | 0 | |||||||||||||||||
| 7.1 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓▲ | ✓ | ✓ | ✓▲ | ✓ | ✓ | 15 | 4 | 2 | 0 | |||
| 7.3 | ✓▲ | 1 | 0 | 1 | 0 | |||||||||||||||||
| 8.1 | ✓ ▲ ▲ | ✓ | ✓ | ✓ ▲ ▲ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 14 | 8 | 2 | 0 | ||||
| 8.2 | ✓ | ✓ | ✓ | 3 | 0 | 0 | 0 | |||||||||||||||
| 8.3 | ✓ | ✓ | ✓ | ✓ | 4 | 1 | 0 | 0 | ||||||||||||||
| 8.4 | ✓ | ✓▲ | 2 | 0 | 1 | 0 | ||||||||||||||||
| 8.6 | ✓ | ✓ | ✓ | ✓ | ✓ | 5 | 2 | 0 | 0 | |||||||||||||
| 8.7 | ✓ | ✓ ▲ ▲ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓▲ | ✓ ▲ ▲ | ✓ | ✓▲ | ✓ ▲ ▲ | 13 | 6 | 5 | 0 | |||||
| 9.1 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓▲ | ✓▲ | 13 | 5 | 2 | 0 | |||||
| 9.2 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 8 | 1 | 0 | 0 | ||||||||||
| 9.3 | ✓ | ✓ | 2 | 0 | 0 | 0 | ||||||||||||||||
| 10.1 | ✓ | ✓ | 2 | 0 | 0 | 0 | ||||||||||||||||
| 10.2 | ✓ | ✓ | 2 | 0 | 0 | 0 | ||||||||||||||||
| 10.3 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓▲ | ✓ | 10 | 0 | 1 | 0 | ||||||||
| 10.4 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓▲ | ✓ | ✓ | 9 | 0 | 1 | 0 | |||||||||
| 10.5 | ✓▲ | ✓ | 2 | 0 | 1 | 0 | ||||||||||||||||
| 10.6 | ✓ | ✓ | 2 | 0 | 0 | 0 | ||||||||||||||||
| 10.7 | ✓ | 1 | 0 | 0 | 0 | |||||||||||||||||
| 10.8 | ✓ | 1 | 0 | 0 | 0 | |||||||||||||||||
| 10.9 | ✓ | ✓▲ | ✓▲ | ✓ | ✓ | ✓ | 6 | 0 | 2 | 0 | ||||||||||||
| 10.11 | ✓ | 1 | 0 | 0 | 0 | |||||||||||||||||
| 11.1 | ✓ | ✓ | 2 | 0 | 0 | 0 | ||||||||||||||||
| 11.2 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 6 | 0 | 0 | 0 | ||||||||||||
| 12.1 | ✓ | ✓ | ✓ ▲ ▲ | ✓ | ✓ | ✓ | 6 | 1 | 1 | 0 | ||||||||||||
| 12.2 | ✓ | ✓ | 2 | 0 | 0 | 0 | ||||||||||||||||
| 12.3 | ✓ | ✓ | 2 | 0 | 0 | 0 | ||||||||||||||||
| 12.4 | ✓ | ✓ | 2 | 0 | 0 | 0 | ||||||||||||||||
| 12.5 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ ▲ ▲ | ✓ ▲ ▲ | ✓ | 13 | 9 | 2 | 0 | |||||
| 12.6 | ✓ | ✓ | 2 | 1 | 0 | 0 | ||||||||||||||||
| 13.1 | ✓ | 1 | 0 | 0 | 0 | |||||||||||||||||
| 13.2 | ✓ | ✓ | ✓ | ✓ | ✓ ▼ ▼ | ✓ | ✓ | ✓ | 8 | 1 | 0 | 1 | ||||||||||
| 13.4 | ✓ | ✓ | 2 | 0 | 0 | 0 | ||||||||||||||||
| 13.5 | ✓ | ✓ | ✓ | 3 | 0 | 0 | 0 | |||||||||||||||
| 14.1 | ✓ | 1 | 0 | 0 | 0 | |||||||||||||||||
| 14.4 | ✓ | 1 | 0 | 0 | 0 | |||||||||||||||||
| 14.6 | ✓ | 1 | 0 | 0 | 0 | |||||||||||||||||
| 14.8 | ✓ | 1 | 0 | 0 | 0 | |||||||||||||||||
| 15.1 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 6 | 1 | 0 | 0 | ||||||||||||
| 15.3 | ✓ | 1 | 0 | 0 | 0 | |||||||||||||||||
| 15.4 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 6 | 0 | 0 | 0 | ||||||||||||
| 16.2 | ✓ | 1 | 0 | 0 | 0 | |||||||||||||||||
| 16.3 | ✓ | 1 | 0 | 0 | 0 | |||||||||||||||||
 = BCTs that were frequently used (reported in ≥50% of included studies); ▲ = BCTs positively associated with improvements in physical activity; ▼ = BCTs negatively associated with improvements in physical activity.
= BCTs that were frequently used (reported in ≥50% of included studies); ▲ = BCTs positively associated with improvements in physical activity; ▼ = BCTs negatively associated with improvements in physical activity.Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Peng, S.; Yuan, F.; Yang, H.; Li, M.; Yang, X. Application of Behaviour Change Techniques in Promoting Physical Activity Among Adults with Chronic Conditions: An Umbrella Review. Behav. Sci. 2025, 15, 1448. https://doi.org/10.3390/bs15111448
Peng S, Yuan F, Yang H, Li M, Yang X. Application of Behaviour Change Techniques in Promoting Physical Activity Among Adults with Chronic Conditions: An Umbrella Review. Behavioral Sciences. 2025; 15(11):1448. https://doi.org/10.3390/bs15111448
Chicago/Turabian StylePeng, Sanying, Fang Yuan, Hongchang Yang, Meilin Li, and Xiaoming Yang. 2025. "Application of Behaviour Change Techniques in Promoting Physical Activity Among Adults with Chronic Conditions: An Umbrella Review" Behavioral Sciences 15, no. 11: 1448. https://doi.org/10.3390/bs15111448
APA StylePeng, S., Yuan, F., Yang, H., Li, M., & Yang, X. (2025). Application of Behaviour Change Techniques in Promoting Physical Activity Among Adults with Chronic Conditions: An Umbrella Review. Behavioral Sciences, 15(11), 1448. https://doi.org/10.3390/bs15111448








