Do Grade II Ankle Sprains Have Chronic Effects on the Functional Ability of Ballet Dancers Performing Single-Leg Flat-Foot Stance? An Observational Cross-Sectional Study
Abstract
1. Introduction
2. Materials and Methods
3. Sample Size Calculation
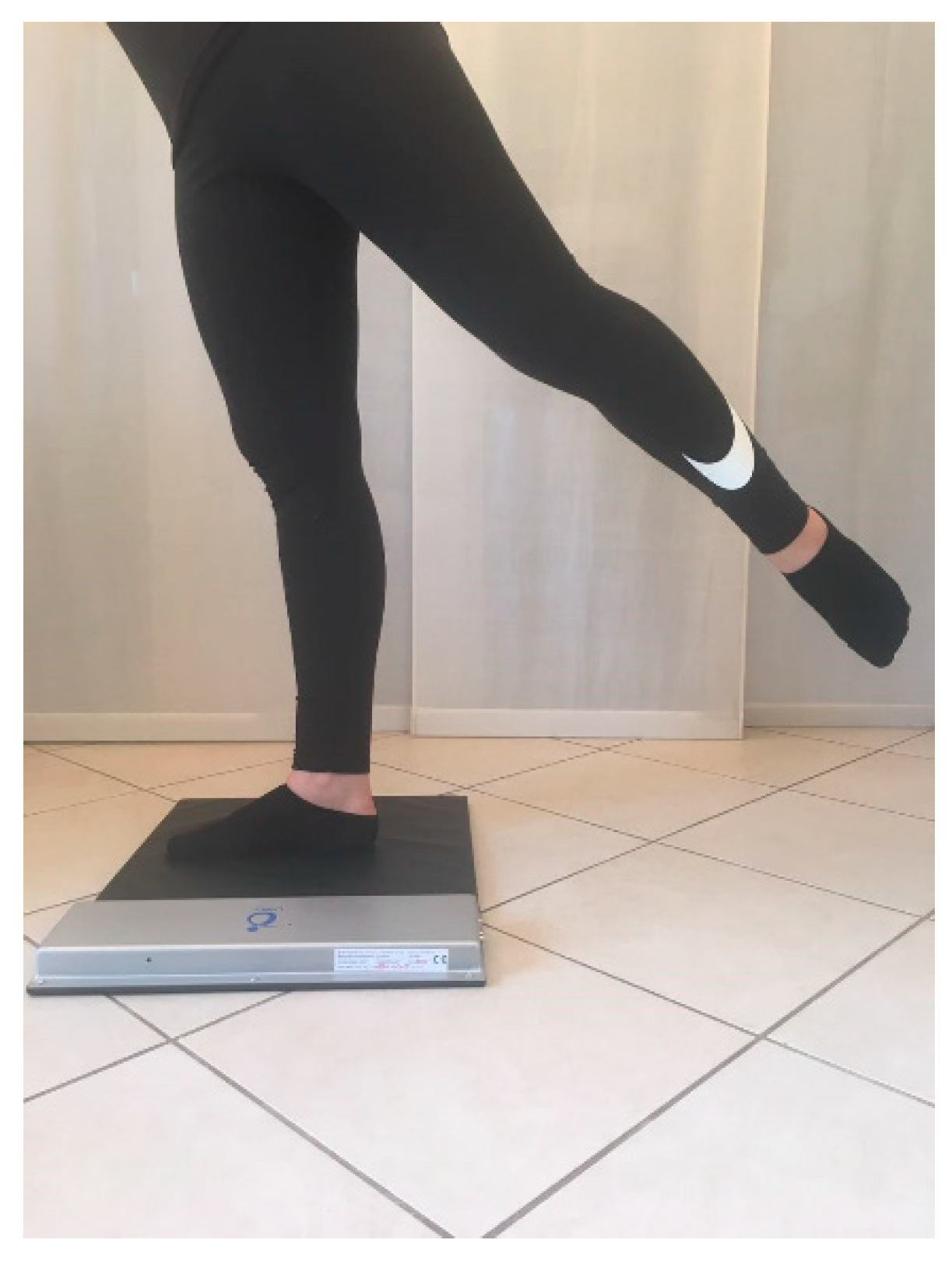
4. Tools and Procedures
5. Statistical Analysis
6. Results
7. Discussion
8. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Steinberg, N.; Tenenbaum, S.; Stern, M.; Zeev, A.; Siev-Ner, I. The association between menarche, intensity of training and passive joint ROM in young pre-professional female dancers: A longitudinal follow-up study. Phys. Ther. Sport 2018, 32, 59–66. [Google Scholar] [CrossRef]
- Krityakiarana, W.; Jongkamonwiwat, N. Comparison of Balance Performance between Thai Classical Dancers and Non-Dancers. J. Dance Med. Sci. 2016, 20, 72–78. [Google Scholar] [CrossRef]
- Tekin, D.; Agopyan, A.; Baltaci, G. Balance Training in Modern Dancers: Proprioceptive-Neuromuscular Training vs. Kinesio Taping. Med. Probl. Perform. Art. 2018, 33, 156–165. [Google Scholar] [CrossRef] [PubMed]
- Bruyneel, A.V.; Mesure, S.; Paré, J.C.; Bertrand, M. Organization of postural equilibrium in several planes in ballet dancers. Neurosci. Lett. 2010, 485, 228–232. [Google Scholar] [CrossRef]
- Yin, A.X.; Geminiani, E.; Quinn, B.; Owen, M.; Kinney, S.; McCrystal, T.; Stracciolini, A. The Evaluation of Strength, Flexibility, and Functional Performance in the Adolescent Ballet Dancer during Intensive Dance Training. PM & R 2019, 11, 722–730. [Google Scholar]
- Krasnow, D.; Wilmerding, M.V.; Stecyk, S.; Wyon, M.; Koutedakis, Y. Biomechanical research in dance: A literature review. Med. Probl. Perform. Art. 2011, 26, 3–23. [Google Scholar] [PubMed]
- da Silveira Costa, M.S.; de Sá Ferreira, A.; Felicio, L.R. Static and dynamic balance in ballet dancers: A literature review. Fisioter. Pesqui. 2013, 20, 299–305. [Google Scholar]
- Vassallo, A.J.; Hiller, C.; Stamatakis, E.; Pappas, E. Epidemiology of Dance-Related Injuries Presenting to Emergency Departments in the United States, 2000-2013. Med. Probl. Perform. Art. 2017, 32, 170–175. [Google Scholar] [CrossRef]
- Smith, T.O.; Davies, L.; de Medici, A.; Hakim, A.; Haddad, F.; Macgregor, A. Prevalence and profile of musculoskeletal injuries in ballet dancers: A systematic review and meta-analysis. Phys. Ther. Sport 2016, 19, 50–56. [Google Scholar] [CrossRef]
- Smith, P.J.; Gerrie, B.J.; Varner, K.E.; McCulloch, P.C.; Lintner, D.M.; Harris, J.D. Incidence and Prevalence of Musculoskeletal Injury in Ballet: A Systematic Review. Orthop. J. Sports Med. 2015, 3. [Google Scholar] [CrossRef]
- Lin, C.-W.; Su, F.-C.; Lin, C.-F. Influence of ankle injury on muscle activation and postural control during ballet grand plié. J. Appl. Biomech. 2014, 30, 37–49. [Google Scholar] [CrossRef] [PubMed]
- Glencross, D.; Thornton, E. Position sense following joint injury. J. Sports Med. Phys. Fitness 1981, 21, 23–27. [Google Scholar] [PubMed]
- Malliaropoulos, N.; Ntessalen, M.; Papacostas, E.; Longo, U.G.; Maffulli, N. Reinjury after acute lateral ankle sprains in elite track and field athletes. Am. J. Sports Med. 2009, 37, 1755–1761. [Google Scholar] [CrossRef] [PubMed]
- Sousa, A.S.P.; Leite, J.; Costa, B.; Santos, R. Bilateral Proprioceptive Evaluation in Individuals with Unilateral Chronic Ankle Instability. J. Athl. Train. 2017, 52, 360–367. [Google Scholar] [CrossRef] [PubMed]
- Leanderson, J.; Eriksson, E.; Nilsson, C.; Wykman, A. Proprioception in classical ballet dancers. A prospective study of the influence of an ankle sprain on proprioception in the ankle joint. Am. J. Sports Med. 1996, 24, 370–374. [Google Scholar] [CrossRef] [PubMed]
- Attenborough, A.S.; Hiller, C.E.; Smith, R.M.; Stuelcken, M.; Greene, A.; Sinclair, P.J. Chronic ankle instability in sporting populations. Sports Med. Auckl. NZ 2014, 44, 1545–1556. [Google Scholar] [CrossRef]
- Simon, J.; Hall, E.; Docherty, C. Prevalence of chronic ankle instability and associated symptoms in university dance majors: an exploratory study. J. Dance Med. Sci. 2014, 18, 178–184. [Google Scholar] [CrossRef]
- Fusca, M.; Negrini, F.; Perego, P.; Magoni, L.; Molteni, F.; Andreoni, G. Validation of a Wearable IMU System for Gait Analysis: Protocol and Application to a New System. Appl. Sci. 2018, 8, 1167. [Google Scholar] [CrossRef]
- Ghislieri, M.; Gastaldi, L.; Pastorelli, S.; Tadano, S.; Agostini, V. Wearable Inertial Sensors to Assess Standing Balance: A Systematic Review. Sensors 2019, 19. [Google Scholar] [CrossRef]
- Lee, Y.-J.; Liang, J.N.; Wen, Y.-T. Characteristics of Postural Muscle Activity in Response to a Motor-Motor Task in Elderly. Appl. Sci. 2019, 9, 4319. [Google Scholar] [CrossRef]
- McKeon, P.O.; Hertel, J. Systematic review of postural control and lateral ankle instability, part I: Can deficits be detected with instrumented testing. J. Athl. Train. 2008, 43, 293–304. [Google Scholar] [CrossRef] [PubMed]
- Nardone, A.; Godi, M.; Grasso, M.; Guglielmetti, S.; Schieppati, M. Stabilometry is a predictor of gait performance in chronic hemiparetic stroke patients. Gait Posture 2009, 30, 5–10. [Google Scholar] [CrossRef] [PubMed]
- Bruyneel, A.-V.; Humbert, A.; Bertrand, M. Comparison of balance strategies in mountain climbers during real altitude exposure between 1.500m and 3.200m: Effects of age and expertise. Neurosci. Lett. 2017, 657, 16–21. [Google Scholar] [CrossRef] [PubMed]
- de Mello, M.C.; de Sá Ferreira, A.; Ramiro Felicio, L. Postural Control During Different Unipodal Positions in Professional Ballet Dancers. J. Dance Med. Sci. 2017, 21, 151–155. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.-W.; Lin, C.-F.; Hsue, B.-J.; Su, F.-C. A comparison of ballet dancers with different level of experience in performing single-leg stance on retiré position. Motor Control 2014, 18, 199–212. [Google Scholar] [CrossRef] [PubMed]
- Witchalls, J.; Waddington, G.; Adams, R.; Blanch, P. Evaluation of the relative contribution of peripheral and focal vision to proprioceptive differentiation of underfoot inversion angles in young elite athletes. Percept. Mot. Skills 2013, 117, 923–934. [Google Scholar] [CrossRef]
- Han, J.; Anson, J.; Waddington, G.; Adams, R.; Liu, Y. The Role of Ankle Proprioception for Balance Control in relation to Sports Performance and Injury. BioMed Res. Int. 2015, 2015, 842804. [Google Scholar] [CrossRef]
- Marulli, T.A.; Harmon-Matthews, L.E.; Davis-Coen, J.H.; Willigenburg, N.W.; Hewett, T.E. Eyes-Closed Single-Limb Balance is Not Related to Hypermobility Status in Dancers. J. Dance Med. Sci. 2017, 21, 70–75. [Google Scholar] [CrossRef]
- Casabona, A.; Leonardi, G.; Aimola, E.; La Grua, G.; Polizzi, C.M.; Cioni, M.; Valle, M.S. Specificity of foot configuration during bipedal stance in ballet dancers. Gait Posture 2016, 46, 91–97. [Google Scholar] [CrossRef]
- Asseman, F.; Caron, O.; Crémieux, J. Is there a transfer of postural ability from specific to unspecific postures in elite gymnasts? Neurosci. Lett. 2004, 358, 83–86. [Google Scholar] [CrossRef]
- Giboin, L.-S.; Gruber, M.; Kramer, A. Three months of slackline training elicit only task-specific improvements in balance performance. PLoS ONE 2018, 13, e0207542. [Google Scholar] [CrossRef] [PubMed]
- Thalassinos, M.; Fotiadis, G.; Arabatzi, F.; Isableu, B.; Hatzitaki, V. Sport Skill-Specific Expertise Biases Sensory Integration for Spatial Referencing and Postural Control. J. Mot. Behav. 2018, 50, 426–435. [Google Scholar] [CrossRef] [PubMed]
- Biernacki, J.L.; Stracciolini, A.; Fraser, J.; Micheli, L.J.; Sugimoto, D. Risk Factors for Lower-Extremity Injuries in Female Ballet Dancers: A Systematic Review. Clin. J. Sport Med. 2018. [Google Scholar] [CrossRef] [PubMed]
- Malliaropoulos, N.; Papacostas, E.; Papalada, A.; Maffulli, N. Acute lateral ankle sprains in track and field athletes: an expanded classification. Foot Ankle Clin. 2006, 11, 497–507. [Google Scholar] [CrossRef]
- Scoppa, F.; Capra, R.; Gallamini, M.; Shiffer, R. Clinical stabilometry standardization: Basic definitions--acquisition interval--sampling frequency. Gait Posture 2013, 37, 290–292. [Google Scholar] [CrossRef]
- Cuccia, A.M. Validity and reliability of spatio-temporal gait parameters in adolescents. Iran. J. Pediatr. 2013, 23, 610–611. [Google Scholar]
- Lin, C.-W.; Chen, S.-J.; Su, F.-C.; Wu, H.-W.; Lin, C.-F. Differences of ballet turns (pirouette) performance between experienced and novice ballet dancers. Res. Q. Exerc. Sport 2014, 85, 330–340. [Google Scholar] [CrossRef]
- Sansone, V.; Maiorano, E.; Applefield, R.C.; Gandola, M.; Negrini, F. Strength Reduction in Unilateral Shoulder Pain: Is the Healthy Side Really Healthy in Rotator Cuff Disease? Am. J. Phys. Med. Rehabil. 2019, 98, 382–386. [Google Scholar] [CrossRef]
- Heales, L.J.; Lim, E.C.W.; Hodges, P.W.; Vicenzino, B. Sensory and motor deficits exist on the non-injured side of patients with unilateral tendon pain and disability--implications for central nervous system involvement: a systematic review with meta-analysis. Br. J. Sports Med. 2014, 48, 1400–1406. [Google Scholar] [CrossRef]
- Cavallari, P.; Bolzoni, F.; Bruttini, C.; Esposti, R. The Organization and Control of Intra-Limb Anticipatory Postural Adjustments and Their Role in Movement Performance. Front. Hum. Neurosci. 2016, 10, 525. [Google Scholar] [CrossRef]


| Post-Injury (N = 11) | Healthy (N = 11) | p-Values | |
|---|---|---|---|
| Age (years) | 16.36 ± 2.81 | 17.5 ± 3.37 | >0.05 |
| BMI (Kg/m²) | 19.85 ± 2.43 | 19.37 ± 2.33 | >0.05 |
| Years of Practice | 11.91 ± 2.11 | 12.37 ± 4.07 | >0.05 |
| Age When They Started Practicing (years) | 4.36 ± 1.23 | 5.18 ± 1.47 | >0.05 |
| Right Foot | Left Foot | p-Values | |
|---|---|---|---|
| Monopodalic Ellipse Area (mm2) | 105.91 ± 67.87 | 82.06 ± 47.43 | >0.05 |
| Monopodalic CoP Speed (mm/s) | 13.84 ± 3.24 | 13.20 ± 5.34 | >0.05 |
| Arabesque Ellipse Area (mm2) | 274.40 ± 255.50 | 152.23 ± 87.54 | >0.05 |
| Arabesque CoP Speed (mm/s) | 21.84 ± 8.46 | 19.65 ± 5.60 | >0.05 |
| Passè Ellipse Area (mm2) | 222.49 ± 130.06 | 133.26 ± 72.00 | >0.05 |
| Passè CoP Speed (mm/s) | 22.22 ± 4.98 | 18.17 ± 5.58 | >0.05 |
| Trauma | No Trauma | p-Values | |
|---|---|---|---|
| Monopodalic Ellipse Area (mm2) | 128.25 ± 93.83 | 83.23 ± 49.15 | >0.05 |
| Monopodalic CoP Speed (mm/s) | 14.23 ± 5.05 | 13.28 ± 5.55 | >0.05 |
| Arabesque Ellipse Area (mm2) | 165.17 ± 127.18 | 117.16 ± 59.89 | >0.05 |
| Arabesque CoP Speed (mm/s) | 19.32 ± 4.38 | 18.54 ± 5.63 | >0.05 |
| Passè Ellipse Area (mm2) | 148.15 ± 82.43 | 119.66 ± 66.75 | >0.05 |
| Passè CoP Speed (mm/s) | 20.75 ± 6.92 | 18.58 ± 5.97 | >0.05 |
| Trauma | No Trauma | p-Values | |
|---|---|---|---|
| Monopodalic Ellipse Area (mm2) | 321.47 ± 151.77 | 358.42 ± 310.67 | >0.05 |
| Monopodalic CoP Speed (mm/s) | 15.77 ± 3.77 | 16.88 ±7.81 | >0.05 |
| Arabesque Ellipse Area (mm2) | 449.63 ± 203.33 | 440.82 ±378.02 | >0.05 |
| Arabesque CoP Speed (mm/s) | 15.28 ± 9.60 | 15.29 ±9.60 | >0.05 |
| Passè Ellipse Area (mm2) | 330.93 ± 294.15 | 302.69 ± 216.10 | >0.05 |
| Passè CoP Speed (mm/s) | 16.90 ± 9.22 | 12.66 ± 7.53 | >0.05 |
| Right Foot Post-Injury (N = 11) | Right Foot Healthy (N = 11) | p-Values | |
|---|---|---|---|
| Monopodalic Ellipse Area (mm2) | 105.91 ± 67.87 | 128.25 ± 93.83 | >0.05 |
| Monopodalic CoP Speed (mm/s) | 13.84 ± 3.24 | 14.23 ± 5.05 | >0.05 |
| Arabesque Ellipse Area (mm2) | 274.40 ± 255.50 | 165.17 ± 127.18 | >0.05 |
| Arabesque CoP Speed (mm/s) | 21.84 ± 8.46 | 19.32 ± 4.38 | >0.05 |
| Passè Ellipse Area (mm2) | 222.49 ± 130.06 | 148.15 ± 82.43 | >0.05 |
| Passè CoP Speed (mm/s) | 22.22 ± 4.98 | 20.75 ± 6.92 | >0.05 |
| Right Foot POST-Injury (N = 11) | Right Foot Healthy (N = 11) | p-Values | |
|---|---|---|---|
| Monopodalic Ellipse Area (mm2) | 321.47 ± 151.77 | 397.47 ± 252.87 | >0.05 |
| Monopodalic CoP Speed (mm/s) | 15.77 ± 3.77 | 15.85 ± 5.29 | >0.05 |
| Arabesque Ellipse Area (mm2) | 449.63 ± 203.33 | 307.73 ± 252.13 | >0.05 |
| Arabesque CoP Speed (mm/s) | 15.28 ± 9.60 | 14.64 ± 5.04 | >0.05 |
| Passè Ellipse Area (mm2) | 330.93 ± 294.15 | 294.46 ± 85.47 | >0.05 |
| Passè CoP Speed (mm/s) | 16.90 ± 9.22 | 15.32 ± 7.14 | >0.05 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bodini, B.D.; Lucenteforte, G.; Serafin, P.; Barone, L.; Vitale, J.A.; Serafin, A.; Sansone, V.; Negrini, F. Do Grade II Ankle Sprains Have Chronic Effects on the Functional Ability of Ballet Dancers Performing Single-Leg Flat-Foot Stance? An Observational Cross-Sectional Study. Appl. Sci. 2020, 10, 155. https://doi.org/10.3390/app10010155
Bodini BD, Lucenteforte G, Serafin P, Barone L, Vitale JA, Serafin A, Sansone V, Negrini F. Do Grade II Ankle Sprains Have Chronic Effects on the Functional Ability of Ballet Dancers Performing Single-Leg Flat-Foot Stance? An Observational Cross-Sectional Study. Applied Sciences. 2020; 10(1):155. https://doi.org/10.3390/app10010155
Chicago/Turabian StyleBodini, Bruno Dino, Giacomo Lucenteforte, Pietro Serafin, Lorenzo Barone, Jacopo A. Vitale, Antonio Serafin, Valerio Sansone, and Francesco Negrini. 2020. "Do Grade II Ankle Sprains Have Chronic Effects on the Functional Ability of Ballet Dancers Performing Single-Leg Flat-Foot Stance? An Observational Cross-Sectional Study" Applied Sciences 10, no. 1: 155. https://doi.org/10.3390/app10010155
APA StyleBodini, B. D., Lucenteforte, G., Serafin, P., Barone, L., Vitale, J. A., Serafin, A., Sansone, V., & Negrini, F. (2020). Do Grade II Ankle Sprains Have Chronic Effects on the Functional Ability of Ballet Dancers Performing Single-Leg Flat-Foot Stance? An Observational Cross-Sectional Study. Applied Sciences, 10(1), 155. https://doi.org/10.3390/app10010155








