Acute Effects of Whole-Body Vibration Exercise on Pain Level, Functionality, and Rating of Exertion of Elderly Obese Knee Osteoarthritis Individuals: A Randomized Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Trial Design
2.2. Inclusion Criteria
2.3. Exclusion Criteria
2.4. Randomization
2.5. Participants
3. Measurements
3.1. The First Day of Evaluation
Pain Level Analysis
3.2. Oswestry Disability Index
3.3. Lequesne’s Functional Index
3.3.1. The Second Day of Evaluation
3.3.2. Evaluation of Height and Waist Circumference
3.3.3. Body Composition Analysis
3.3.4. TUG Test
3.4. Flexibility
3.5. Subjective Perceived Exertion Rating
3.6. Protocol Interventions
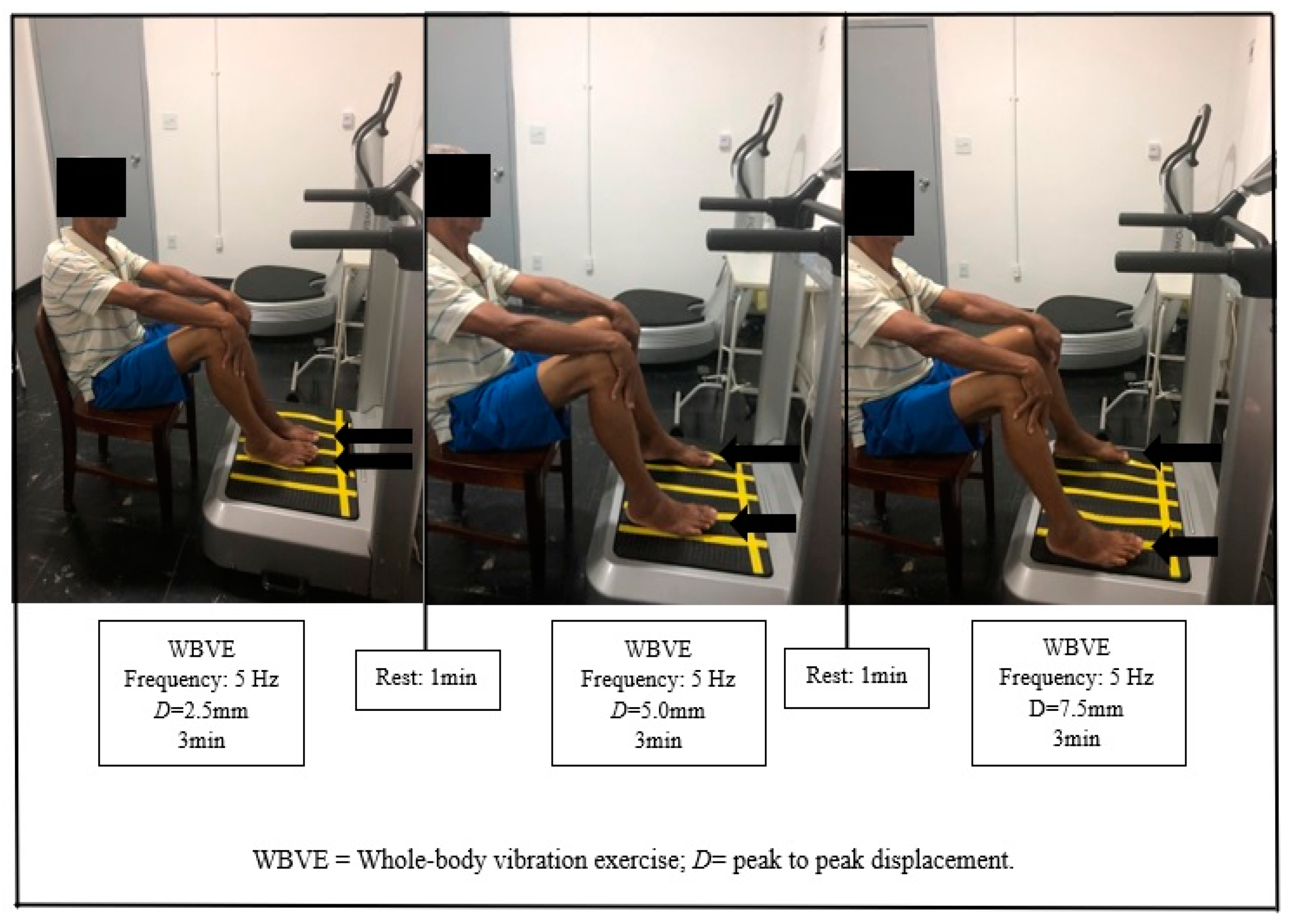
3.7. WBV Exercise Protocol
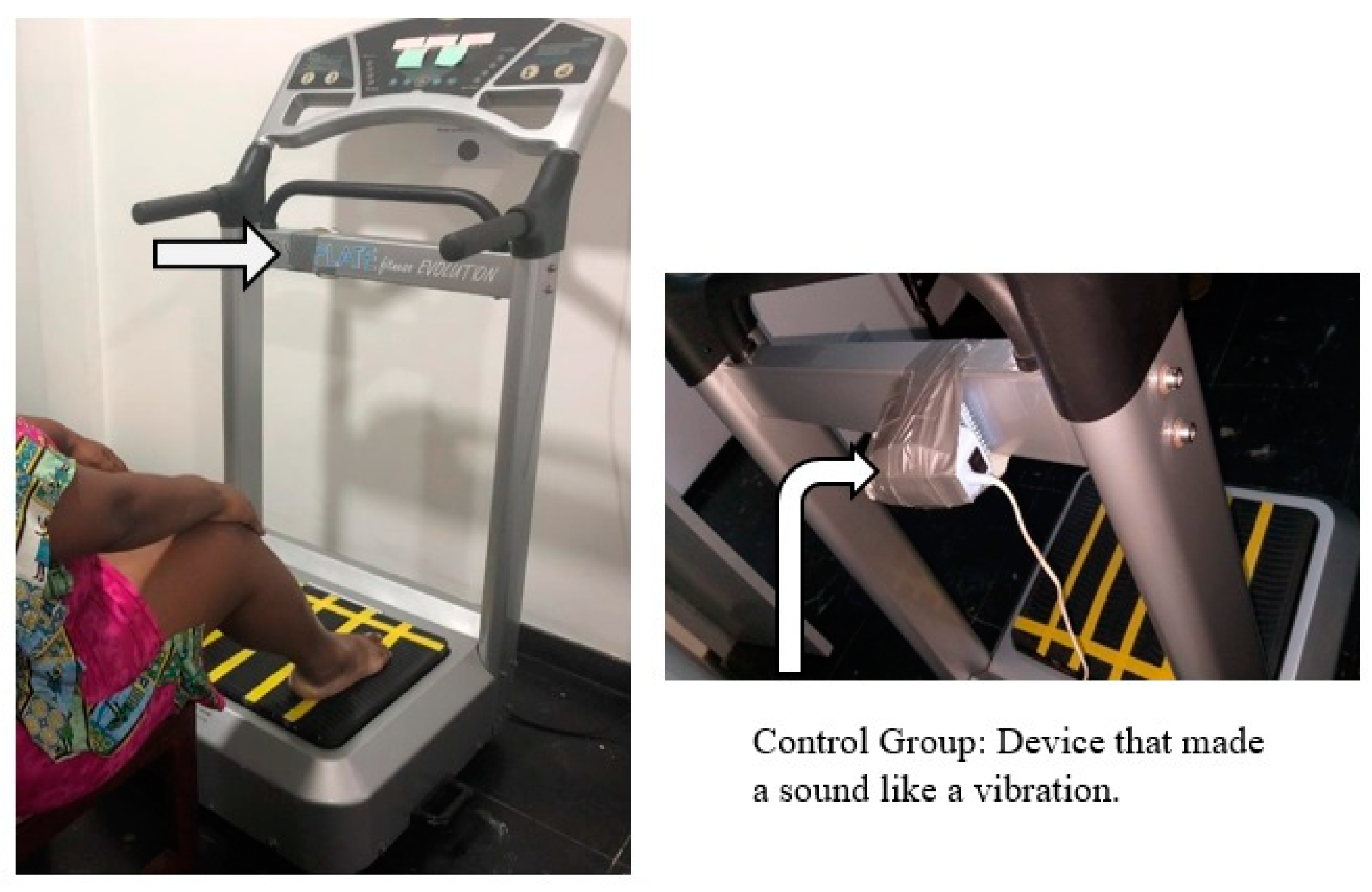
3.8. CG Protocol
3.9. Sample Size
3.10. Data Analysis
4. Results
5. Discussion
6. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Kolasinski, S.L.; Neogi, T.; Hochberg, M.C.; Oatis, C.; Guyatt, G.; Block, J.; Callahan, L.; Copenhaver, C.; Dodge, C.; Felson, D.; et al. 2019 American College of Rheumatology/Arthritis Foundation Guideline for the Management of Osteoarthritis of the Hand, Hip, and Knee. Arthritis Rheumatol. 2020, 72, 220–233. [Google Scholar] [CrossRef] [PubMed]
- Bannuru, R.R.; Osani, M.; Vaysbrot, E.; Arden, N.; Bennell, K.; Bierma-Zeinstra, S.; Kraus, V.; Lohmander, L.; Abbott, J.; Bhandari, M.; et al. OARSI guidelines for the non-surgical management of knee, hip, and polyarticular osteoarthritis. Osteoarthr. Cartil. 2019, 27, 1578–1589. [Google Scholar] [CrossRef] [Green Version]
- De Campos, G.C.; De Sousa, E.B.; Hamdan, P.C.; Júnior, C.S.D.A.; Tieppo, A.M.; De Rezende, M.U.; Alchaar, A.A.D.A.; Pinheiro, C.B.; Rocha, E.D.M.C.; Cunha, F.G.; et al. Brazilian consensus statement on viscosupplementation of the knee (COBRAVI). Acta Ortopédica Brasileira 2019, 27, 230–236. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- De Rezende, M.U.; De Campos, G.C. Is osteoarthritis a mechanical or inflammatory disease? Rev. Bras. Ortop. 2013, 48, 471–474. [Google Scholar] [CrossRef] [Green Version]
- Ahlbäck, S. Osteoarthrosis of the knee. A radiographic investigation. Acta Radiol. Diagn. 1968, 277, 7–72. [Google Scholar]
- Keyes, G.W.; Carr, A.J.; Miller, R.K.; Goodfellow, J.W. The radiographic classification of medial gonarthrosis. Correlation with operation methods in 200 knees. Acta Orthop Scand 1992, 63, 497–501. [Google Scholar] [CrossRef]
- McAlindon, T.; Bannuru, R.R.; Sullivan, M.; Arden, N.K.; Berenbaum, F.; Bierma-Zeinstra, S.; Hawker, G.A.; Henrotin, Y.; Hunter, D.J.; Kawaguchi, H.; et al. OARSI guidelines for the non-surgical management of knee osteoarthritis. Osteoarthr. Cartil. 2014, 22, 363–388. [Google Scholar] [CrossRef] [Green Version]
- Altman, R.D.; Fries, J.F.; Bloch, D.A.; Carstens, J.; Mb, T.C.D.; Genant, H.; Gofton, P.; Groth, H.; McShane, D.J.; Murphy, W.A.; et al. Radiographic assessment of progression in osteoarthritis. Arthritis Rheum. 1987, 30, 1214–1225. [Google Scholar] [CrossRef]
- Apold, H.; Meyer, H.E.; Nordsletten, L.; Furnes, O.; Baste, V.; Flugsrud, G. Risk factors for knee replacement due to primary osteoarthritis, a population based, prospective cohort study of 315,495 individuals. BMC Musculoskelet. Disord. 2014, 15, 217. [Google Scholar] [CrossRef] [Green Version]
- Soh, S.-E.; Barker, A.L.; Morello, R.; Ackerman, I.N. Applying the International Classification of Functioning, Disability and Health framework to determine the predictors of falls and fractures in people with osteoarthritis or at high risk of developing osteoarthritis: Data from the Osteoarthritis Initiative. BMC Musculoskelet. Disord. 2020, 21, 138. [Google Scholar] [CrossRef]
- Foley, S.; Lord, S.R.; Srikanth, V.; Cooley, H.; Jones, G. Falls risk is associated with pain and dysfunction but not radiographic osteoarthritis in older adults: Tasmanian Older Adult Cohort study. Osteoarthr. Cartil. 2006, 14, 533–539. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fisher, N.M.; Pendergast, D.R. Reduced muscle function in patients with osteoarthritis. Scand. J. Rehabil. Med. 1997, 29, 213. [Google Scholar] [PubMed]
- Silva, N.A.; Montadon, A.C.O.S.; Cabral, M.V.S.P. Peripheral degenerative joint diseases. Einsten. São Paulo. 2008, 66 (Suppl. 1), S21–S28. [Google Scholar]
- Rezende, M.U.; de Campos, G.C. Viscosuplplementation. Rev. Bras. Ortop. 2012, 47, 160–164. [Google Scholar] [CrossRef] [PubMed]
- Donnelly, J.E.; Blair, S.N.; Jakicic, J.M.; Manore, M.M.; Rankin, J.W.; Smith, B.K. Appropriate Physical Activity Intervention Strategies for Weight Loss and Prevention of Weight Regain for Adults. Med. Sci. Sports Exerc. 2009, 41, 459–471. [Google Scholar] [CrossRef]
- American Heart Association. Available online: http:https://www.heart.org/en/healthy-living/fitness/fitness-basics/aha-recs-for-physical-activity-in-adults (accessed on 17 April 2020).
- Gay, C.; Chabaud, A.; Guilley, E.; Coudeyre, E. Educating patients about the benefits of physical activity and exercise for their hip and knee osteoarthritis. Systematic literature review. Ann. Phys. Rehabil. Med. 2016, 59, 174–183. [Google Scholar] [CrossRef]
- De Rooij, M.; Van Der Leeden, M.; Cheung, J.; Van Der Esch, M.; Häkkinen, A.; Haverkamp, D.; Roorda, L.D.; Twisk, J.; Vollebregt, J.; Lems, W.F.; et al. Efficacy of Tailored Exercise Therapy on Physical Functioning in Patients with Knee Osteoarthritis and Comorbidity: A Randomized Controlled Trial. Arthritis Rheum. 2017, 69, 807–816. [Google Scholar] [CrossRef]
- Tittlemier, B.J.; Wittmeier, K.D.; Webber, S.C. Quality and content analysis of clinical practice guidelines which include nonpharmacological interventions for knee osteoarthritis. J. Eval. Clin. Pract. 2020. [Google Scholar] [CrossRef]
- Dell’Isola, A.; Jönsson, T.; Ranstam, J.; Dahlberg, L.E.; Hansson, E.E. Education, Home Exercise, and Supervised Exercise for People with Hip and Knee Osteoarthritis As Part of a Nationwide Implementation Program: Data from the Better Management of Patients With Osteoarthritis Registry. Arthritis Rheum. 2020, 72, 201–207. [Google Scholar] [CrossRef]
- Rauch, F.; Sievanen, H.; Boonen, S.; Cardinale, M.; Degens, H.; Felsenberg, D.; Roth, J.; Schoenau, E.; Verschueren, S.; Rittweger, J. Reporting whole-body vibration intervention studies: Recommendations of the International Society of Musculoskeletal and Neuronal Interactions. J. Musculoskelet. Neuronal Interact. 2010, 10, 193–198. [Google Scholar]
- Rittwger, J. Vibration as an exercise modality: How it may work, and what its potential might be. Eur. J. Appl. Physiol. 2010, 108, 877–904. [Google Scholar] [CrossRef] [PubMed]
- Moreira-Marconi, E.; Dionello, C.F.; Morel, D.S.; Sá-caputo, D.C.; Souza-Gonçalves, C.R.; Paineira-Domingos, L.L.; Silva-Teixeira, Y.; dos Santos Pereira, M.J.; Bernardo-Filho, M. Whole body vibration and auriculotherapy improve handgrip strength in individuals with knee osteoarthritis. J. Tradit. Chin. Med. 2019, 39, 707–715. [Google Scholar]
- Lai, Z.; Lee, S.; Hu, X.; Wang, L. Effect of adding whole-body vibration training to squat training on physical function and muscle strength in individuals with knee osteoarthritis. J. Musculoskelet. Neuronal Interact. 2019, 19, 333–341. [Google Scholar] [PubMed]
- Sá-Caputo, D.; Paineiras-Domingos, L.L.; Oliveira, R.; Neves, M.F.; Brandão, A.; Marin, P.J.; Sañudo, B.; Furness, T.; Taiar, R.; Bernardo-Filho, M. Acute Effects of Whole-Body Vibration on the Pain Level, Flexibility, and Cardiovascular Responses in Individuals With Metabolic Syndrome. Dose-Response 2018, 16. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Paiva, P.C.; Figueiredo, C.A.; Reis-Silva, A.; Francisca-Santos, A.; Paineiras-Domingos, L.L.; Martins-Anjos, E.; Melo-Oliveira, M.E.S.; Lourenço-Revelles, G.M.G.; Moreira-Marconi, E.; Guedes-Aguiar, E.O.; et al. Acute and Cumulative Effects with Whole-Body Vibration Exercises Using 2 Biomechanical Conditions on the Flexibility and Rating of Perceived Exertion in Individuals With Metabolic Syndrome: A Randomized Clinical Trial Pilot Study. Dose-Response 2019, 17. [Google Scholar] [CrossRef] [Green Version]
- Lage, V.; Lacerda, A.C.R.; Neves, C.D.C.; Chaves, M.G.A.; Soares, A.A.; Lima, L.P.; Martins, J.B.; Matos, M.A.; Vieira, É.L.M.; Teixeira, A.L.; et al. Acute Effects of Whole-Body Vibration on Inflammatory Markers in People with Chronic Obstructive Pulmonary Disease: A Pilot Study. Rehabil. Res. Pract. 2018, 2018, 1–7. [Google Scholar] [CrossRef] [Green Version]
- World Health Organization. Physical Status: The Use and Interpretation of Anthropometry; WHO Technical Report Series, 854; World Health Organization: Geneva, Swizterland, 1995. [Google Scholar]
- Schulz, K.F.; Altman, D.G.; Moher, D. CONSORT 2010 Statement. Obstet. Gynecol. 2010, 115, 1063–1070. [Google Scholar] [CrossRef]
- Random.org. Available online: http://www.random.org (accessed on 13 November 2018).
- Galli, M.; De Santis, V.; Tafuro, L. Reliability of the Ahlbäck classification of knee osteoarthritis. Osteoarthr. Cartil. 2003, 11, 580–584. [Google Scholar] [CrossRef] [Green Version]
- Weidow, J.; Cederlund, C.-G.; Ranstam, J.; Kärrholm, J. Ahlbäck grading of osteoarthritis of the knee: Poor reproducibility and validity based on visual inspection of the joint. Acta Orthop. 2006, 77, 262–266. [Google Scholar] [CrossRef]
- Kesiktas, F.N.; Dernek, B.; Sen, E.I.; Albayrak, H.N.; Aydin, T.; Yildiz, M. Comparison of the short-term results of single-dose intra-articular peptide with hyaluronic acid and platelet-rich plasma injections in knee osteoarthritis: A randomized study. Clin. Rheumatol. 2020, 1–8. [Google Scholar] [CrossRef]
- Ishimoto, Y.; Kawakami, M.; Curtis, E.; Cooper, C.; Harvey, N.; Westbury, L.; Teraguchi, M.; Horie, K.; Nakagawa, Y. The Impact of Lumbar Spinal Stenosis, Knee Osteoarthritis, and Loss of Lumbar Lordosis on the Quality of Life: Findings from the Katsuragi Low Back Pain Study. Spine Surg. Relat. Res. 2018, 3, 157–162. [Google Scholar] [CrossRef] [PubMed]
- Marx, F.C.; Oliveira, L.M.; Bellini, C.G.; Ribeiro, M.C.C. Translation and cultural validation of the Lequesne’s algofunctional questionnaire for osteoarthritis of knee and hip for portuguese language. Rev. Bras. Reumatol. 2006, 46, 253–260. [Google Scholar]
- Sá-Caputo, D.; Paineiras-Domingos, L.L.; Francisca-Santos, A.; Dos Anjos, E.M.; Reis-Silva, A.; Neves, M.F.; Oigman, W.; Oliveira, R.; Brandão, A.A.; Machado, C.B.; et al. Whole-body vibration improves the functional parameters of individuals with metabolic syndrome: An exploratory study. BMC Endocr. Disord. 2019, 19, 6. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Khalil, S.F.; Mohktar, M.S.; Ibrahim, F. The Theory and Fundamentals of Bioimpedance Analysis in Clinical Status Monitoring and Diagnosis of Diseases. Sensors 2014, 14, 10895–10928. [Google Scholar] [CrossRef]
- Cômodo AR, O.; Dias AC, F.; Tomaz, B.A.; Silva Filho, A.A.; Werustsky, C.A.; Ribas, D.F.; Spolidoro, J.; Marchini, J.S. Utilização da bioimpedância para avaliação da massa corpórea; Associação Médica Brasileira: São Paulo, Brazil, 2009; pp. 1–13. [Google Scholar]
- Kyle, U.G.; Bosaeus, I.; De Lorenzo, A.D.; Deurenberg, P.; Elia, M.; Gómez, J.M.; Heitmann, B.L.; Kent-Smith, L.; Melchior, J.-C.; Pirlich, M.; et al. Bioelectrical impedance analysis-part II: Utilization in clinical practice. Clin. Nutr. 2004, 23, 1430–1453. [Google Scholar] [CrossRef]
- Kear, B.M.; Guck, T.P.; McGaha, A.L. Timed Up and Go (TUG) Test. J. Prim. Care Community Health 2016, 8, 9–13. [Google Scholar] [CrossRef] [Green Version]
- Shariat, A.; Cleland, J.A.; Danaee, M.; Alizadeh, R.; Sangelaji, B.; Kargarfard, M.; Ansari, N.N.; Sepehr, F.H.; Tamrin, S.B.M. Borg CR-10 scale as a new approach to monitoring office exercise training. Work 2018, 60, 549–554. [Google Scholar] [CrossRef]
- Neto, S.B.S.; Moreira-Marconi, E.; Kutter, C.R.; Frederico, É.H.F.F.; Paiva, P.D.C.D.; Meyer, P.F.; Chang, S.; Sá-Caputo, D.; Bernardo-Filho, M. Beneficial effects of whole body mechanical vibration alone or combined with auriculotherapy in the pain and in flexion of knee of individuals with knee osteoarthritis. Acupunct. Electro-Ther. Res. 2017, 42, 185–201. [Google Scholar] [CrossRef]
- Miot, H.A. Tamanho da amostra em estudos clínicos e experimentais. J. Vasc. Bras. 2011, 10, 275–278. [Google Scholar] [CrossRef] [Green Version]
- Trans, T.; Aaboe, J.; Henriksen, M.; Christensen, R.; Bliddal, H.; Lund, H. Effect of whole body vibration exercise on muscle strength and proprioception in females with knee osteoarthritis. Knee 2009, 16, 256–261. [Google Scholar] [CrossRef]
- Bade, M.J.; Kohrt, W.M.; Stevens-Lapsley, J.E. Outcomes before and after total knee arthroplasty compared to healthy adults. J. Orthop. Sports Phys. Ther. 2010, 40, 559–567. [Google Scholar] [CrossRef] [Green Version]
- Mizner, R.L.; Petterson, S.C.; Stevens, J.E.; Vandenborne, K.; Snyder-Mackler, L. Early quadriceps strength loss after total knee arthroplasty. The contributions of muscle atrophy and failure of voluntary muscle activation. J. Bone Jt. Surg. Am. 2005, 87, 1047–1053. [Google Scholar] [CrossRef] [PubMed]
- Hsiao, Y.-H.; Chien, S.-H.; Tu, H.-P.; Fu, J.C.-M.; Tsai, S.-T.; Chen, Y.-S.; Chen, Y.-J.; Chen, C.-H. Early Post-Operative Intervention of Whole-Body Vibration in Patients After Total Knee Arthroplasty: A Pilot Study. J. Clin. Med. 2019, 8, 1902. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mikami, Y.; Amano, J.; Kawamura, M.; Nobiro, M.; Kamijyo, Y.; Kawae, T.; Maeda, N.; Hirata, K.; Kimura, H.; Adachi, N. Whole-body vibration enhances effectiveness of “locomotion training” evaluated in healthy young adult women. J. Phys. Ther. Sci. 2019, 31, 895–900. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Coghill, R.C.; Talbot, J.D.; Evans, A.C.; Meyer, E.; Gjedde, A.; Bushnell, M.C.; Duncan, G.H. Distributed processing of pain and vibration by the human brain. J. Neurosci. 1994, 14, 4095–4108. [Google Scholar] [CrossRef] [Green Version]
- Zafar, H.; Alghadir, A.; Anwer, S.; Al-Eisa, E. Therapeutic Effects of Whole-Body Vibration Training in Knee Osteoarthritis: A Systematic Review and Meta-Analysis. Arch. Phys. Med. Rehabil. 2015, 96, 1525–1532. [Google Scholar] [CrossRef]
- Wang, P.; Yang, X.; Yang, Y.; Yang, L.; Zhou, Y.; Liu, C.; Reinhardt, J.D.; He, C. Effects of whole body vibration on pain, stiffness and physical functions in patients with knee osteoarthritis: A systematic review and meta-analysis. Clin. Rehabil. 2014, 29, 939–951. [Google Scholar] [CrossRef]
- Li, X.; Wang, X.Q.; Chen, B.L.; Huang, L.Y.; Liu, Y. Whole-Body Vibration Exercise for Knee Osteoarthritis: A Systematic Review and Meta-Analysis. Evid. Based Complement. Altern. Med. 2015, 2015, 636435. [Google Scholar] [CrossRef] [Green Version]
- Ferreira, R.M.; Duarte, J.A.; Gonçalves, R.S. Non-pharmacological and non-surgical interventions to manage patients with knee osteoarthritis: An umbrella review. Acta Reum. Port. 2018, 43, 182–200. [Google Scholar]
- Simão, A.P.; Avelar, N.C.; Tossige-Gomes, R.; Neves, C.D.; Mendonça, V.A.; Miranda, A.S.; Teixeira, M.M.; Teixeira, A.L.; De Andrade, A.G.P.; Coimbra, C.C.; et al. Functional Performance and Inflammatory Cytokines After Squat Exercises and Whole-Body Vibration in Elderly Individuals With Knee Osteoarthritis. Arch. Phys. Med. Rehabil. 2012, 93, 1692–1700. [Google Scholar] [CrossRef]
- Salmon, J.R.; Roper, J.A.; Tillman, M.D. Does Acute Whole-Body Vibration Training Improve the Physical Performance of People with Knee Osteoarthritis? J. Strength Cond. Res. 2012, 26, 2983–2989. [Google Scholar] [CrossRef] [PubMed] [Green Version]




| CG (n = 18) | WBVEG (n = 19) | p-Value | |
|---|---|---|---|
| Mean (SE) | Mean (SE) | ||
| Sex | F = 15/M = 3 | F = 15/M = 4 | 1.000 |
| Age (year) | 68.06 (2.02) | 62.32 (2.52) | 0.112 |
| Height (m) | 1.54 (0.01) | 1.58 (0.01) | 0.123 |
| Body mass (kg) | 75.67 (3.18) | 86.15 (4.50) | 0.091 |
| Waist circumference (cm) | 103.9 (2.54) | 106.9 (3.65) | 0.851 |
| BMI (kg/m2) | 31.71 (1.22) | 34.75 (2.10) | 0.420 |
| ODI (%) | 30.61 (2.86) | 35.39 (2.95) | 0.201 |
| LFI (score) | 11.81 (3.66) | 11.85 (3.89) | 0.989 |
| VAS (0–10) | 4.33 (0.52) | 4.36 (0.60) | 0.981 |
| CG before Mean (SE) | CG after Mean (SE) | p-Value | WBVEG before Mean (SE) | WBVEG after Mean (SE) | p-Value | p-Value # | |
|---|---|---|---|---|---|---|---|
| VAS (0–10) | 4.11 (0.56) | 3.94 (0.57) | 0.564 | 4.58 (0.62) | 3.23 (0.61) | 0.001 * | 0.041 * |
| TUG-test (s) | 14.87 (0.88) | 13.84 (0.78) | 0.002* | 19.42 (1.96) | 16.44 (1.50) | <0.001 * | 0.045 * |
| BORG SCALE (score) | 1.66 (0.56) | 1.58 (0.51) | >0.999 | 2.15 (0.54) | 2.15 (0.54) | 0.627 | 0.452 |
| ATF (cm) | 17.53 (2.54) | 16.31 (2.53) | 0.103 | 18.81 (2.08) | 14.64 (2.05) | <0.001 * | 0.043 * |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Moura-Fernandes, M.C.; Moreira-Marconi, E.; de Meirelles, A.G.; Reis-Silva, A.; de Souza, L.F.F.; Lírio Pereira da Silva, A.; de Oliveira, B.B.M.; de Souza Gama, M.A.; de Oliveira, A.C.C.; Batouli-Santos, D.; et al. Acute Effects of Whole-Body Vibration Exercise on Pain Level, Functionality, and Rating of Exertion of Elderly Obese Knee Osteoarthritis Individuals: A Randomized Study. Appl. Sci. 2020, 10, 5870. https://doi.org/10.3390/app10175870
Moura-Fernandes MC, Moreira-Marconi E, de Meirelles AG, Reis-Silva A, de Souza LFF, Lírio Pereira da Silva A, de Oliveira BBM, de Souza Gama MA, de Oliveira ACC, Batouli-Santos D, et al. Acute Effects of Whole-Body Vibration Exercise on Pain Level, Functionality, and Rating of Exertion of Elderly Obese Knee Osteoarthritis Individuals: A Randomized Study. Applied Sciences. 2020; 10(17):5870. https://doi.org/10.3390/app10175870
Chicago/Turabian StyleMoura-Fernandes, Marcia Cristina, Eloá Moreira-Marconi, Alexandre Gonçalves de Meirelles, Aline Reis-Silva, Luiz Felipe Ferreira de Souza, Adriana Lírio Pereira da Silva, Bruno Bessa Monteiro de Oliveira, Marco Antonio de Souza Gama, Ana Carolina Coelho de Oliveira, Daniel Batouli-Santos, and et al. 2020. "Acute Effects of Whole-Body Vibration Exercise on Pain Level, Functionality, and Rating of Exertion of Elderly Obese Knee Osteoarthritis Individuals: A Randomized Study" Applied Sciences 10, no. 17: 5870. https://doi.org/10.3390/app10175870
APA StyleMoura-Fernandes, M. C., Moreira-Marconi, E., de Meirelles, A. G., Reis-Silva, A., de Souza, L. F. F., Lírio Pereira da Silva, A., de Oliveira, B. B. M., de Souza Gama, M. A., de Oliveira, A. C. C., Batouli-Santos, D., da Silva, Y. T., Torres-Nunes, L., da Silva Caiado, V., de Souza Melo-Oliveira, M. E., de Aguiar, E. d. O. G., de Oliveira, L. P., de Paula Mozella, A., Paineiras-Domingos, L. L., dos Santos Pereira, M. J., ... Bernardo-Filho, M. (2020). Acute Effects of Whole-Body Vibration Exercise on Pain Level, Functionality, and Rating of Exertion of Elderly Obese Knee Osteoarthritis Individuals: A Randomized Study. Applied Sciences, 10(17), 5870. https://doi.org/10.3390/app10175870














