Mechanical Properties and Characteristics of the Anterolateral and Collateral Ligaments of the Knee
Abstract
:1. Introduction
2. Materials and Methods
2.1. Specimen Preparation
2.2. Dissection and Specimen Preparation
2.3. Material Testing
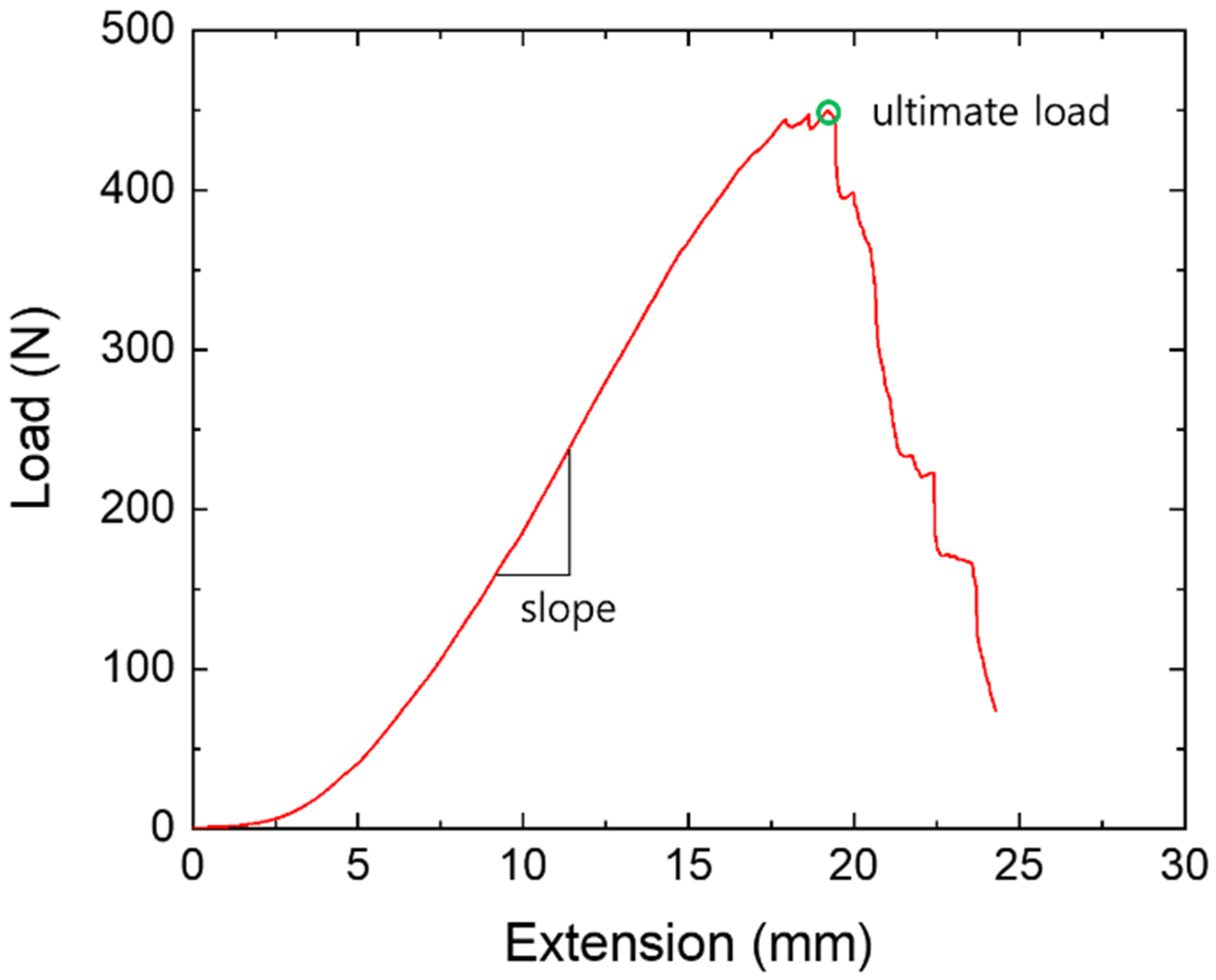
2.4. Data Acquisition and Analysis
3. Results
4. Discussion
Author Contributions
Funding
Conflicts of Interest
Ethics Statement
References
- Flandry, F.; Hommel, G. Normal anatomy and biomechanics of the knee. Sports Med. Arthrosc. Rev. 2011, 19, 82–92. [Google Scholar] [CrossRef] [PubMed]
- LaPrade, R.F.; Engebretsen, A.H.; Ly, T.V.; Johansen, S.; Wentorf, F.A.; Engebretsen, L. The anatomy of the medial part of the knee. J. Bone Joint Surg. Am. 2007, 89, 2000–2010. [Google Scholar] [CrossRef] [PubMed]
- Amis, A.A. Anterolateral knee biomechanics. Knee Surg. Sports Traumatol. Arthrosc. 2017, 25, 1015–1023. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kraeutler, M.J.; Welton, K.L.; Chahla, J.; LaPrade, R.F.; McCarty, E.C. Current concepts of the anterolateral ligament of the knee: Anatomy, biomechanics, and reconstruction. Am. J. Sports Med. 2018, 46, 1235–1242. [Google Scholar] [CrossRef]
- Becker, R.; Hirschmann, M.T.; Karlsson, J. The role of ligament tension and sensomotoric system in total knee arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 2017, 25, 1663–1665. [Google Scholar] [CrossRef] [Green Version]
- Riviere, C.; Iranpour, F.; Auvinet, E.; Howell, S.; Vendittoli, P.-A.; Cobb, J.; Parratte, S. Alignment options for total knee arthroplasty: A systematic review. Orthop. Traumatol. Surg. Res. 2017, 103, 1047–1056. [Google Scholar] [CrossRef]
- Vicenti, G.; Solarino, G.; Carrozzo, M.; De Giorgi, S.; Moretti, L.; De Crescenzo, A.; Moretti, B. Major concern in the multiligament-injured knee treatment: A systematic review. Injury 2019, 50 (Suppl. S2), S89–S94. [Google Scholar] [CrossRef]
- Kennedy, J.C.; Hawkins, R.J.; Willis, R.B.; Danylchuck, K.D. Tension studies of human knee ligaments. Yield point, ultimate failure, and disruption of the cruciate and tibial collateral ligaments. J. Bone Joint Surg. Am. 1976, 58, 350–355. [Google Scholar] [CrossRef]
- Woo, S.L.; Hollis, J.M.; Adams, D.J.; Lyon, R.M.; Takai, S. Tensile properties of the human femur-anterior cruciate ligament-tibia complex. The effects of specimen age and orientation. Am. J. Sports Med. 1991, 19, 217–225. [Google Scholar] [CrossRef]
- Chandrashekar, N.; Mansouri, H.; Slauterbeck, J.; Hashemi, J. Sex-based differences in the tensile properties of the human anterior cruciate ligament. J. Biomech. 2006, 39, 2943–2950. [Google Scholar] [CrossRef]
- Harner, C.D.; Xerogeanes, J.W.; Livesay, G.A.; Carlin, G.J.; Smith, B.A.; Kusayama, T.; Kashiwaguchi, S.; Woo, S.L. The human posterior cruciate ligament complex: An interdisciplinary study. Ligament morphology and biomechanical evaluation. Am. J. Sports Med. 1995, 23, 736–745. [Google Scholar] [CrossRef] [PubMed]
- Race, A.; Amis, A.A. The mechanical properties of the two bundles of the human posterior cruciate ligament. J. Biomech. 1994, 27, 13–24. [Google Scholar] [CrossRef]
- Trent, P.S.; Walker, P.S.; Wolf, B. Ligament length patterns, strength, and rotational axes of the knee joint. Clin. Orthop. Relat. Res. 1976, 117, 263–270. [Google Scholar] [CrossRef]
- Butler, D.L.; Kay, M.D.; Stouffer, D.C. Comparison of material properties in fascicle-bone units from human patellar tendon and knee ligaments. J. Biomech. 1986, 19, 425–432. [Google Scholar] [CrossRef]
- Robinson, J.R.; Bull, A.M.; Amis, A.A. Structural properties of the medial collateral ligament complex of the human knee. J. Biomech. 2005, 38, 1067–1074. [Google Scholar] [CrossRef]
- Wilson, W.T.; Deakin, A.H.; Payne, A.P.; Picard, F.; Wearing, S.C. Comparative analysis of the structural properties of the collateral ligaments of the human knee. J. Orthop. Sports Phys. Ther. 2012, 42, 345–351. [Google Scholar] [CrossRef]
- Vincent, J.P.; Magnussen, R.A.; Gezmez, F.; Uguen, A.; Jacobi, M.; Weppe, F.; Al-Saati, M.F.; Lustig, S.; Demey, G.; Servien, E.; et al. The anterolateral ligament of the human knee: An anatomic and histologic study. Knee Surg. Sports Traumatol. Arthrosc. 2012, 20, 147–152. [Google Scholar] [CrossRef]
- Claes, S.; Vereecke, E.; Maes, M.; Victor, J.; Verdonk, P.; Bellemans, J. Anatomy of the anterolateral ligament of the knee. J. Anat. 2013, 223, 321–328. [Google Scholar] [CrossRef]
- Cho, H.J.; Kwak, D.S. Anatomical consideration of the anterolateral ligament of the knee. Biomed. Res. Int. 2019, 2019, 5740473. [Google Scholar] [CrossRef] [Green Version]
- Zens, M.; Feucht, M.J.; Ruhhammer, J.; Bernstein, A.; Mayr, H.O.; Südkamp, N.P.; Woias, P.; Niemeyer, P. Mechanical tensile properties of the anterolateral ligament. J. Exp. Orthop. 2015, 2, 7. [Google Scholar] [CrossRef] [Green Version]
- Kennedy, M.I.; Claes, S.; Freitas Fuso, F.A.; Williams, B.T.; Goldsmith, M.T.; Lee Turnbull, T.; Wijdicks, C.A.; LaPrade, R.F. The anterolateral ligament: An anatomic, radiographic, and biomechanical analysis. Am. J. Sports Med. 2015, 43, 1606–1615. [Google Scholar] [CrossRef] [PubMed]
- Helito, C.P.; Bonadio, M.B.; Rozas, J.S.; Wey, J.M.P.; Pereira, C.A.M.; Cardoso, T.P.; Pécora, J.R.; Camanho, G.L.; Demange, M.K. Biomechanical study of strength and stiffness of the knee anterolateral ligament. BMC Musculoskelet. Disord. 2016, 17, 193. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wytrykowski, K.; Swider, P.; Reina, N.; Murgier, J.; Laffosse, J.M.; Chiron, P.; Cavaignac, E. Cadaveric study comparing the biomechanical properties of grafts used for knee anterolateral ligament reconstruction. Arthroscopy 2016, 32, 2288–2294. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chong, S.; Kwak, D.-S.; Balasubramanian, D.; Song, Y.D.; Na, Y.G.; Kim, T.K. A new femoral fixation device for anterior cruciate ligament reconstruction using the outside-in technique and hamstring tendon graft: A comparison between two devices in cadaveric human knee models. Knee 2017, 24, 925–932. [Google Scholar] [CrossRef]
- Dodds, A.L.; Halewood, C.; Gupte, C.M.; Williams, A.; Amis, A.A. The anterolateral ligament: Anatomy, length changes and association with the Segond fracture. Bone Joint J. 2014, 96, 325–331. [Google Scholar] [CrossRef]
- Hughston, J.C.; Andrews, J.R.; Cross, M.J.; Moschi, A. Classification of knee ligament instabilities. Part II. The lateral compartment. J. Bone Joint Surg. Am. 1976, 58, 173–179. [Google Scholar] [CrossRef] [Green Version]
- Spencer, L.; Burkhart, T.A.; Tran, M.N.; Rezansoff, A.J.; Deo, S.; Caterine, S.; Getgood, A.M. Biomechanical analysis of simulated clinical testing and reconstruction of the anterolateral ligament of the knee. Am. J. Sports Med. 2015, 43, 2189–2197. [Google Scholar] [CrossRef]
- Arnoux, P.-J.; Subit, D.; Masson, C.; Chabrand, P.; Brunet, C. Knee ligaments mechanics. Rev. Eur. Élém. Finis 2012, 14, 577–600. [Google Scholar] [CrossRef]
- Kittl, C.; Inderhaug, E.; Williams, A.; Amis, A.A. Biomechanics of the anterolateral structures of the knee. Clin. Sports Med. 2018, 37, 21–31. [Google Scholar] [CrossRef]
- Rahnemai-Azar, A.A.; Miller, R.M.; Guenther, D.; Fu, F.H.; Lesniak, B.P.; Musahl, V.; Debski, R.E. Structural properties of the anterolateral capsule and iliotibial band of the knee. Am. J. Sports Med. 2016, 44, 892–897. [Google Scholar] [CrossRef]

| ID | Sex | Age | Height (cm) | Weight (kg) | Side (21 Sides) |
|---|---|---|---|---|---|
| S01 | M | 68 | 130 | 44 | Left |
| S02 | M | 73 | 160 | 70 | Right |
| S03 | F | 76 | 156 | 48 | Both |
| S04 | F | 85 | 137 | 38 | Right |
| S05 | M | 71 | 157 | 46 | Right |
| S06 | M | 77 | 163 | 78 | Both |
| S07 | M | 68 | 162 | 42 | Left |
| S08 | M | 62 | 166 | 28 | Right |
| S09 | F | 77 | 147 | 40 | Both |
| S10 | M | 78 | 172 | 50 | Both |
| S11 | F | 86 | 150 | 26 | Both |
| S12 | F | 93 | 152 | 44 | Both |
| S13 | F | 95 | 162 | 36 | Both |
| S14 | F | 71 | 155 | 52 | Right |
| F: 7 M: 7 | 77.1 | 154.9 | 45.9 | Rt: 5 Lt: 2 Both: 7 |
| MCL | ALL | LCL | |
|---|---|---|---|
| Width (mm) | 11.19 ± 2.78 | 5.49 ± 1.90 | 3.96 ± 0.98 |
| Thickness (mm) | 2.14 ± 0.70 | 1.52 ± 0.64 | 2.58 ± 0.95 |
| Length (mm) | 68.99 ± 19.01 | 34.00 ± 9.90 | 48.15 ± 5.79 |
| Cross-sectional area (mm2) | 24.54 ± 11.94 | 8.50 ± 5.06 | 8.76 ± 3.77 |
| MCL | ALL | LCL | |
|---|---|---|---|
| Ultimate load (N) | 498.57 ± 119.56 | 146.64 ± 53.56 | 263.22 ± 93.09 |
| Stiffness (N/mm) | 71.97 ± 23.47 | 42.62 ± 21.26 | 69.70 ± 22.89 |
| Elastic modulus (MPa) | 326.75 ± 225.22 | 345.27 ± 293.03 | 493.86 ± 98.97 |
| Damaged Area | MCL | ALL | LCL |
|---|---|---|---|
| Proximal attachment | 7 | - | 10 |
| Mid-substance | 10 | 14 | 4 |
| Distal attachment | 4 | 7 | 7 |
| Side | Sex | ||||||
|---|---|---|---|---|---|---|---|
| Left (n = 9) | Right (n = 12) | p-Value | Female (n = 12) | Male (n = 9) | p-value | ||
| MCL | Failure load (N) | 479.6 ± 83.3 | 512.8 ± 142.9 | 0.542 | 461.2 ± 102.4 | 568.5 ± 108.2 | 0.049 |
| Stiffness (N/mm) | 68.5 ± 24.8 | 74.6 ± 23.2 | 0.569 | 67.6 ± 25.5 | 77.8 ± 20.4 | 0.338 | |
| Elastic modulus (MPa) | 214.4 ± 109.2 | 382.9 ± 205.0 | 0.321 | 248.1 ± 145.0 | 425.1 ± 289.9 | 0.268 | |
| ALL | Failure load (N) | 160.5 ± 69.5 | 136.3 ± 37.7 | 0.317 | 122.0 ± 17.8 | 179.5 ± 67.9 | 0.035 |
| Stiffness (N/mm) | 42.5 ± 17.3 | 42.7 ± 24.6 | 0.985 | 37.8 ± 18.1 | 49.1 ± 24.5 | 0.236 | |
| Elastic modulus (MPa) | 423.7 ± 135.5 | 306.0 ± 152.8 | 0.604 | 288.2 ± 174.5 | 416.6 ± 319.7 | 0.550 | |
| LCL | Failure load (N) | 275.8 ± 127.6 | 253.8 ± 60.7 | 0.642 | 214.1 ± 27.3 | 328.7 ± 110.5 | 0.014 |
| Stiffness (N/mm) | 61.3 ± 17.3 | 76.0 ± 25.1 | 0.149 | 63.2 ± 24.3 | 78.3 ± 18.8 | 0.139 | |
| Elastic modulus (MPa) | 438.7 ± 74.3 | 521.5 ± 103.6 | 0.263 | 476.0 ± 119.8 | 516.2 ± 76.0 | 0.579 | |
| Author (Year) | N | Mean Age | Ultimate Load (N) | Stiffness (N/mm) | Elastic Modulus (MPa) | Failure Site | |||
|---|---|---|---|---|---|---|---|---|---|
| Femoral Attachment | Mid-Substance | Tibial Attachment | Bony Avulsion | ||||||
| This study (2020) | 21 | 77.1 | 146.6 ± 53.6 | 42.6 ± 21.3 | 345.3 ± 293.0 | 0 | 14 | 7 | |
| Zens et al. (2015) | 4 | 86.5 | 49.9 ± 14.6 | 2.6 ± 0.9 | 1.2 ± 0.4 | 4 | 0 | 0 | 0 |
| Kennedy et al. (2015) | 15 | 58.2 | 175.0 | 20.0 | - | 4 | 4 | 1 | 6 |
| Wytrykowski et al. (2016) | 15 | 54 | 141.0 ± 40.6 | 21.0 ± 8.2 | - | 0 | 15 | 0 | 0 |
| Helito et al. (2016) | 14 | 62.6 | 204.8 ± 114.9 | 41.9 ± 25.7 | - | 2 | 10 | 1 | 1 |
| Ligament | Author (Year) | N | Mean Age | Ultimate Load (N) | Stiffness (N/mm) | Elastic Modulus (MPa) |
|---|---|---|---|---|---|---|
| LCL | This study (2020) | 21 | 77.1 | 263.2 ± 93.1 | 69.7 ± 22.9 | 493.9 ± 99.0 |
| Sugita et al. (2001) | 10 | About 70 | 309.0 ± 91.0 | 58.1 ± 22.8 | - | |
| LaPrade et al. (2005) | 8 | 57.5 | 295.0 ± 96.0 | 33.5 ±13.4 | 183.5 ± 110.7 | |
| Ciccone et al. (2006) | 13 | 70 | 460.0 ± 163.0 | 82.0 ± 25.0 | - | |
| Wilson et al. (2012) | 9 | 81 | 392.0 ± 104.0 | 59.0 ± 12.0 | - | |
| MCL | This study (2020) | 21 | 77.1 | 498.6 ± 119.6 | 72.0 ± 23.5 | 326.8 ± 225.2 |
| Marinozzi et al. (1983) | 5 | 55–90 | 465.0 ± 190.0 | 60.0 ± 22.0 | - | |
| Wilson et al. (2012) | 9 | 81 | 799.0 ± 209.0 | 63.0 ± 14.0 | - |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cho, H.-J.; Kwak, D.-S. Mechanical Properties and Characteristics of the Anterolateral and Collateral Ligaments of the Knee. Appl. Sci. 2020, 10, 6266. https://doi.org/10.3390/app10186266
Cho H-J, Kwak D-S. Mechanical Properties and Characteristics of the Anterolateral and Collateral Ligaments of the Knee. Applied Sciences. 2020; 10(18):6266. https://doi.org/10.3390/app10186266
Chicago/Turabian StyleCho, Ho-Jung, and Dai-Soon Kwak. 2020. "Mechanical Properties and Characteristics of the Anterolateral and Collateral Ligaments of the Knee" Applied Sciences 10, no. 18: 6266. https://doi.org/10.3390/app10186266





