Quantification of Liver Fibrosis—A Comparative Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data Sources
- Google Scholar, a web engine ideal for searching free academic publications along with conference papers;
- ScienceDirect®, characterized as the leading web source in the access to a large database, emphatically composed of medical research works;
- PubMed®, a free search engine of the National Center for Biotechnology Information (NCBI) which is part of the National Library of Medicine (NLM) in the United States;
- Scopus®, the official database of Elsevier® and ideal for navigation between many citations, according to their research field;
- IEEE Xplore®, a digital library that provides research materials, especially related to computer science and engineering.
2.2. Search Terms
- In the Google Scholar engine, the keywords “CPA, Fibrosis, Liver, Image” were applied, where the process was completed on the 11th tab as the results included more and more posts not related to the subject of interest.
- In ScienceDirect® and the “Keywords” field, the input of “Liver Biopsy, CPA, Collagen, Fibrosis and Biopsy Image” was included.
- All of the above steps were also followed in the PubMed® database to verify the publications obtained with the research. In Scopus® and the “Author” field, the name of five researchers who have been distinguished in this field of research was declared.
- In IEEE Xplore®, the research process with all the previous search terms plus the addition of other keywords, such as “Hepatitis B, Hepatitis C, Sirius red, Masson’s trichrome.” The full search command is displayed in Figure 4. At the end of the search, a large number of results appeared was limited to less than 120 papers by applying system-proposed checkbox filters, including “conference” and “journal” papers, “liver,” and “medical image processing.”
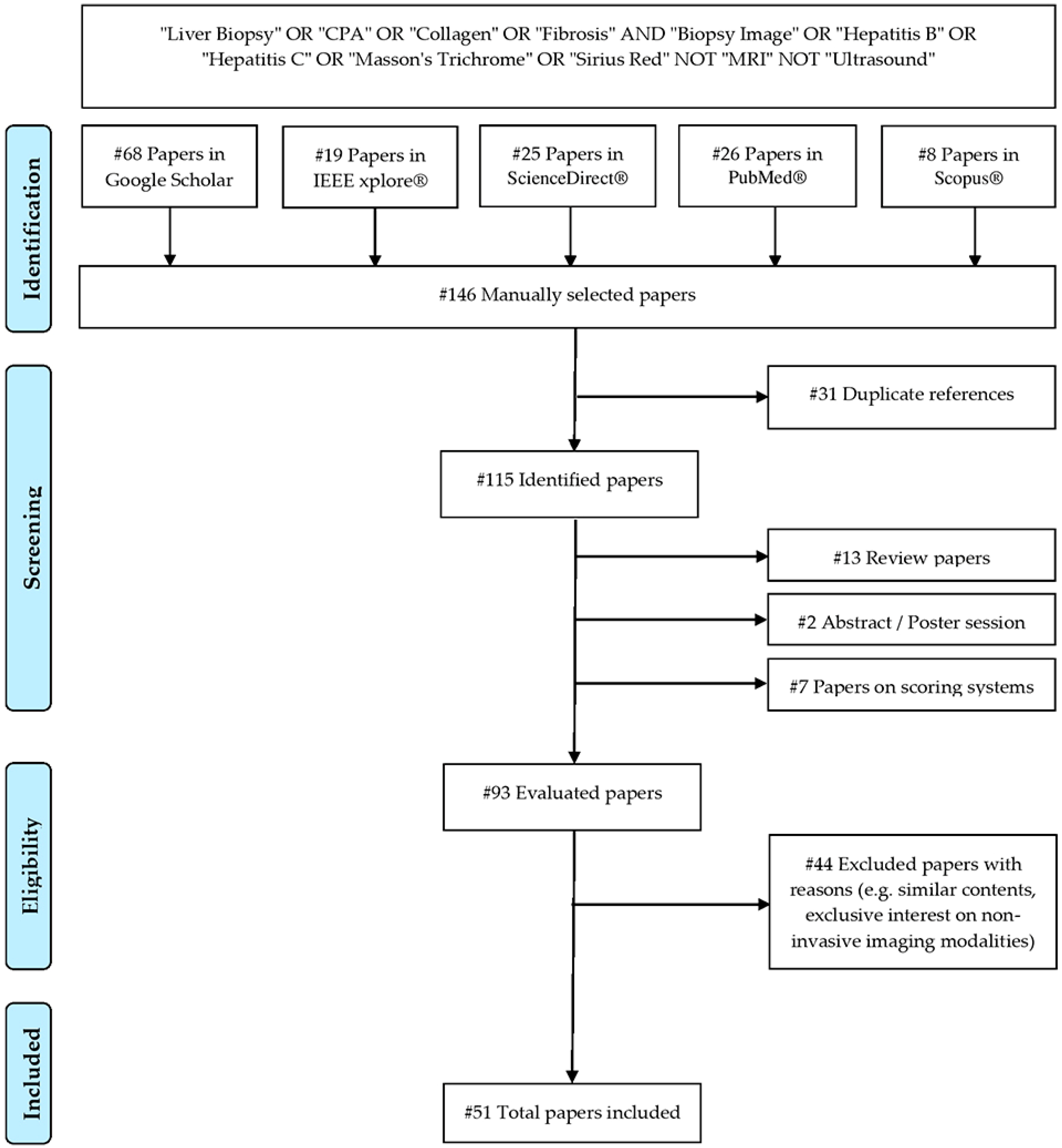
2.3. Study Selection Process
2.4. Analysis Method
3. Literature Review
3.1. Aim of Study
3.1.1. Early Studies Using Semi-Quantitative CPA Evaluations
3.1.2. Comparison of Biopsy Imaging with Non-Invasive Imaging Modalities
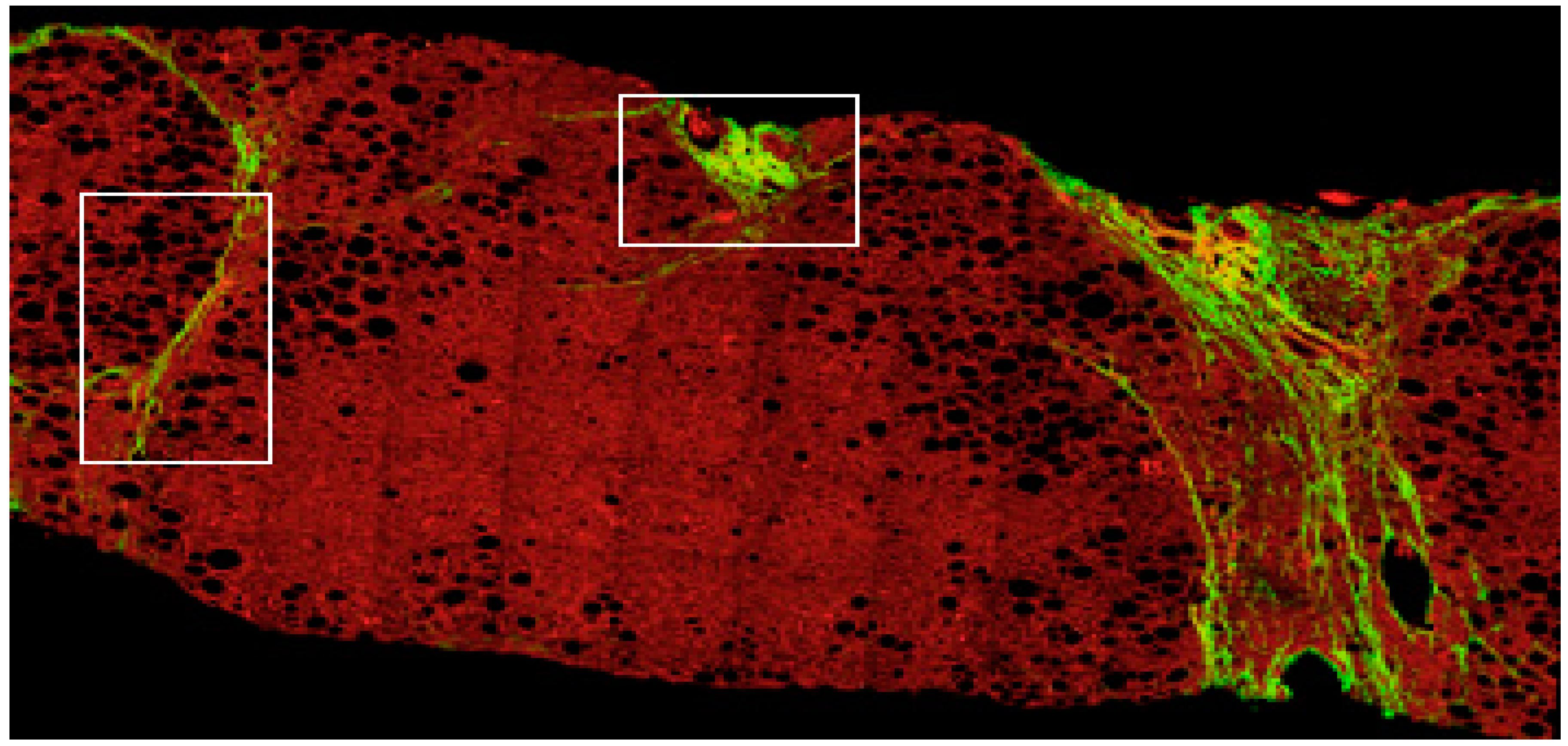
3.1.3. Methodologies Based on SHG/TPEF Imaging Microscopy
3.1.4. Intelligent Diagnostic Systems for Automated CPA Detection
3.2. Histological Samples
3.2.1. Number of Histological Samples in Early Methodologies
3.2.2. Number of Histological Samples in Later Methodologies
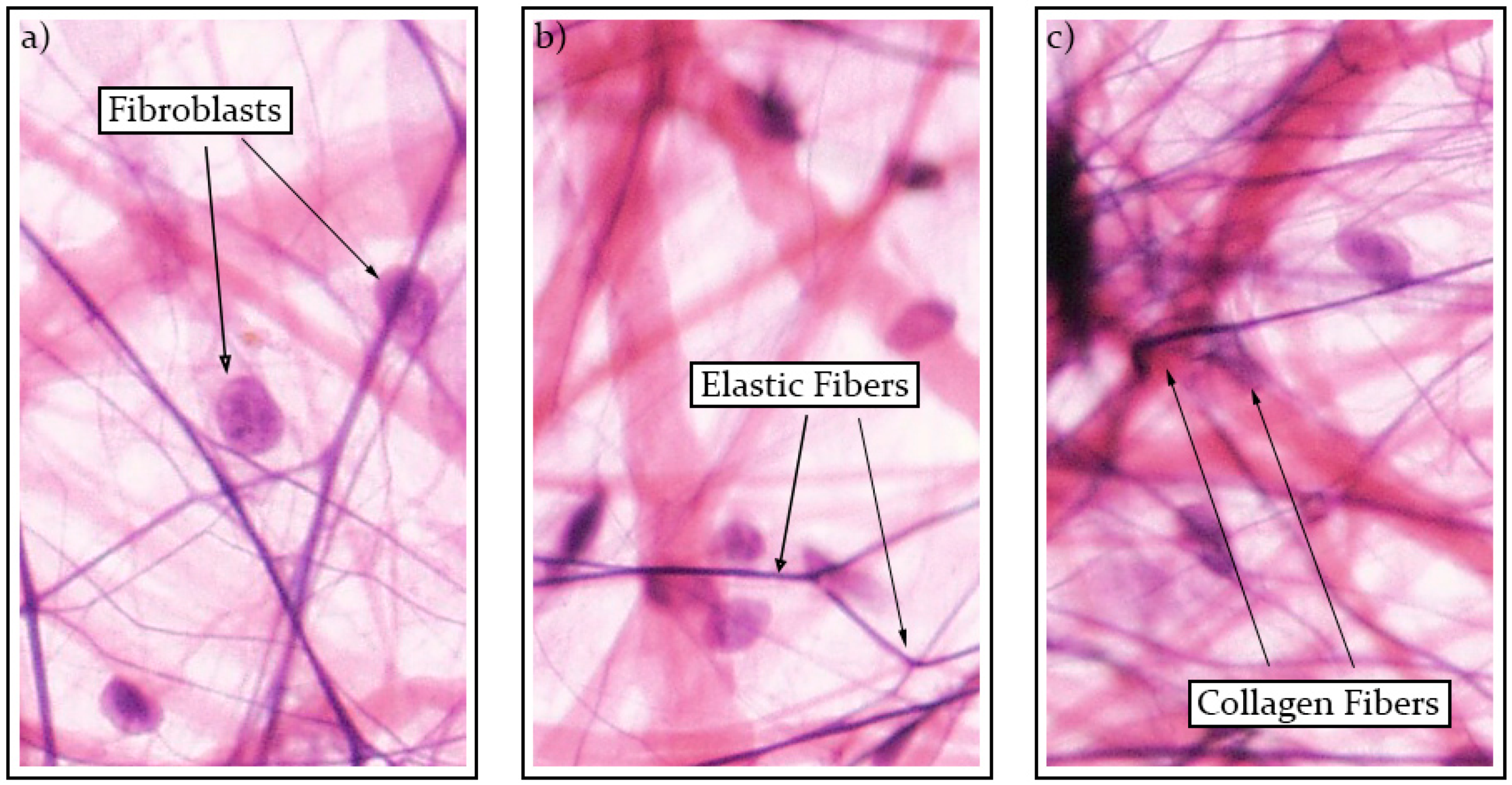
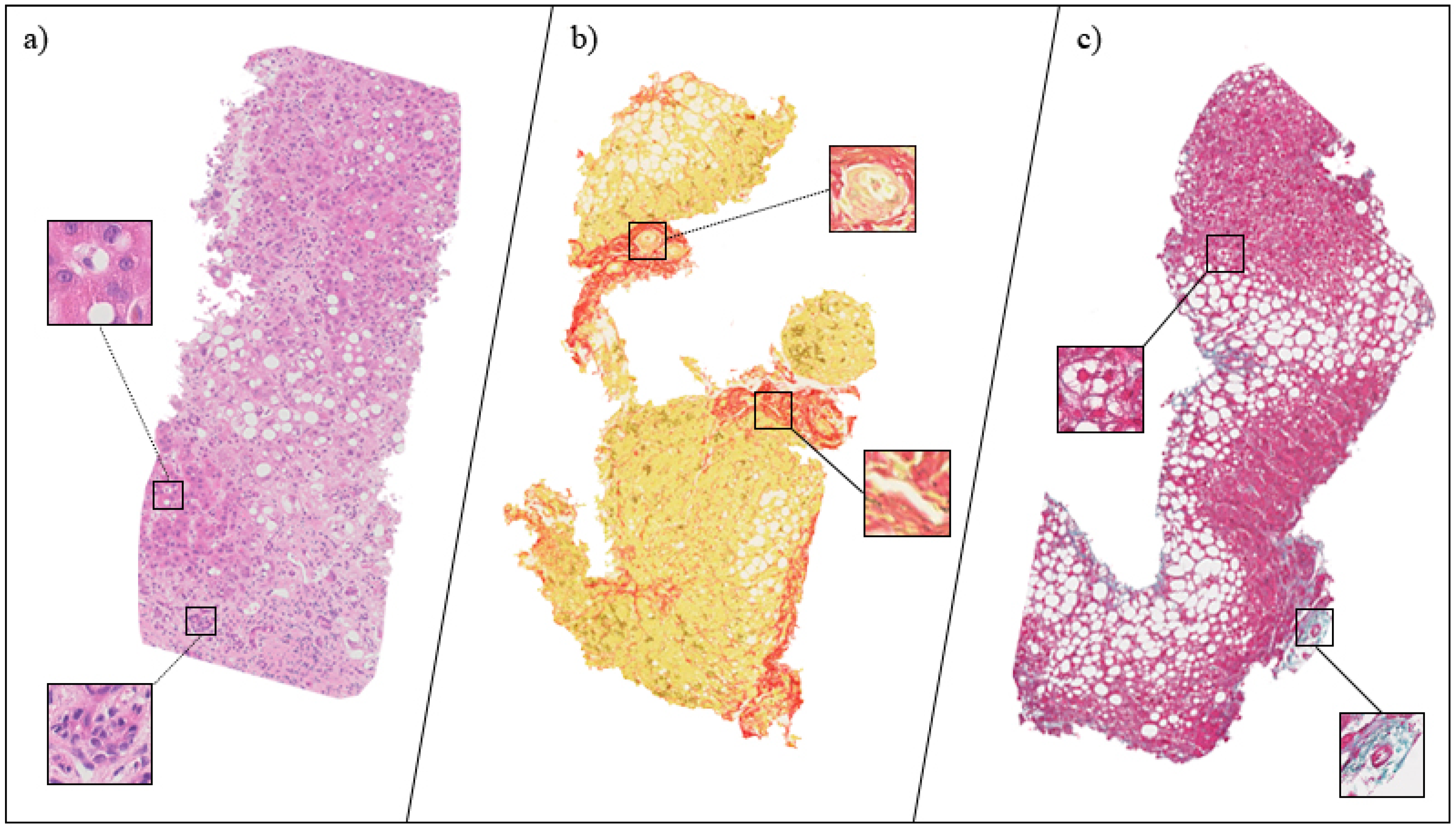
3.3. Tissue Staining
3.3.1. Histological Stains in Early Year Experiments
3.3.2. Histological Stains Used in Recent Years
3.4. Fibrosis Staging
3.4.1. Semi-Quantitative Evaluations with the Knodell and Scheuer HAIs
3.4.2. Newer Methodologies Relying on the Ishak HAI
3.4.3. Recent Research Works Employing the METAVIR HAI
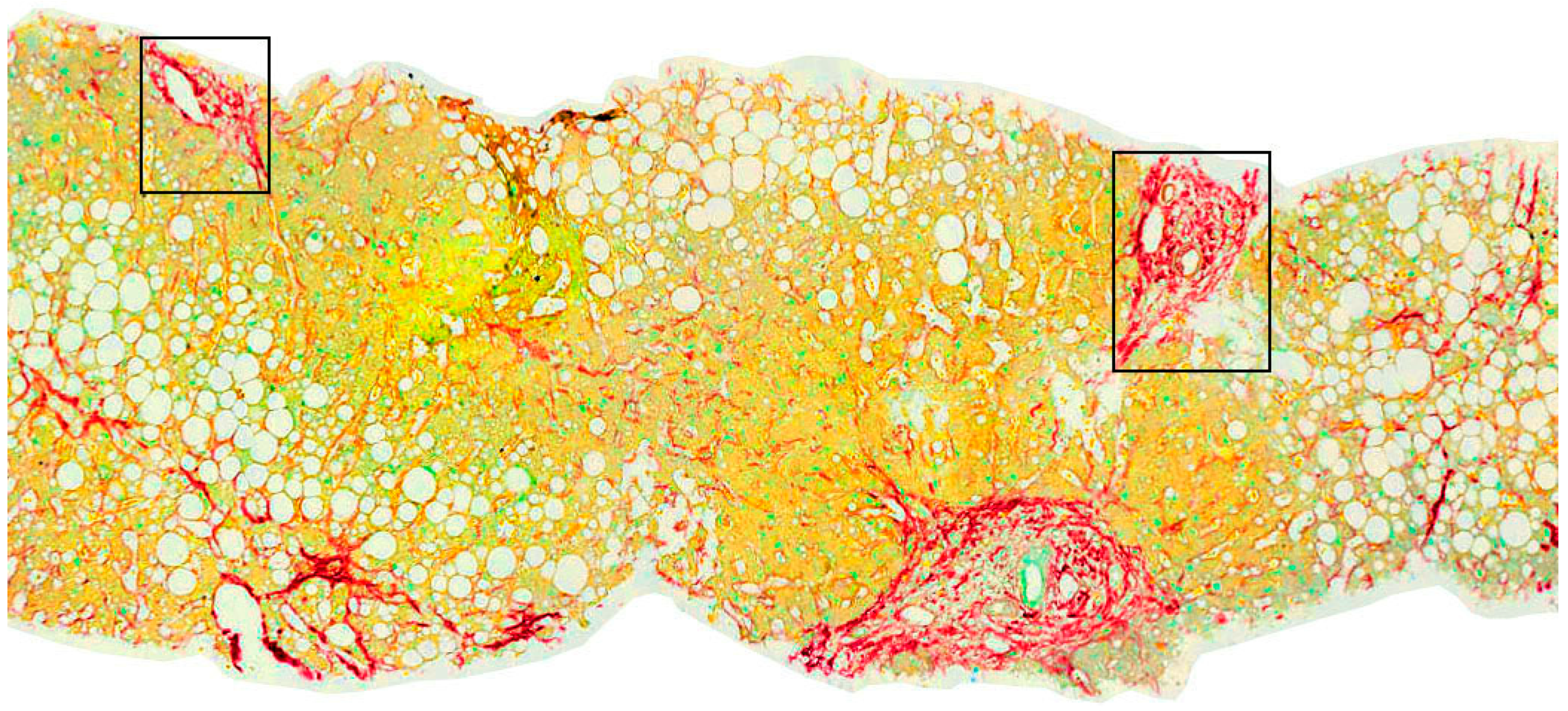
3.5. Image Analysis Method
3.5.1. Early Methodologies Relying on Morphometric Analysis
3.5.2. DIA Systems Using Manual Thresholding
3.5.3. Application of Advanced Image Segmentation Techniques
3.5.4. Application of Automated Fibrosis Detection Techniques
4. Results and Discussion
4.1. Results from Earlier Works Employing DIA and HAI Systems
4.2. Correlation of Histology Imaging with Non-Invasive Markers of Fibrosis
4.3. Results from SHG/TPEF Microscopy Methodologies
4.4. CPA Results Produced by Automated Intelligent Systems
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Koumbi, L. Gut microbiota alterations in liver diseases. EC Gastroenterol. Dig. Syst. 2018, 5, 191–198. [Google Scholar]
- Lo, R.C. Histopathological evaluation of liver fibrosis and cirrhosis regression. Clin. Mol. Hepatol. 2017, 4, 302–307. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Asselah, T.; Marcellin, P.; Bedossa, P. Improving performance of liver biopsy in fibrosis assessment. J. Hepatol. 2014, 61, 193–195. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Desmet, V.J.; Gerber, M.; Hoofnagle, J.H.; Manns, M.; Scheuer, P.J. Classification of chronic hepatitis: Diagnosis, grading and staging. Hepatology 1994, 19, 1513–1520. [Google Scholar] [CrossRef] [PubMed]
- Knodell, R.G.; Ishak, K.G.; Black, W.C.; Chen, T.S.; Craig, R.; Kaplowitz, N.; Kiernan, T.W.; Wollman, J. Formulation and application of a numerical scoring system for assessing histological activity in asymptomatic chronic active hepatitis. Hepatology 1981, 1, 431–435. [Google Scholar] [CrossRef]
- Scheuer, P.J. Classification of chronic viral hepatitis: A need for reassessment. J. Hepatol. 1991, 13, 372–374. [Google Scholar] [CrossRef]
- Bedossa, P.; Poynard, T. An algorithm for grading activity in chronic hepatitis C. Hepatology 1996, 24, 289–293. [Google Scholar] [CrossRef]
- Ishak, K.; Baptista, A.; Bianchi, L.; Callea, F.; De Groote, J.; Gudat, F.; Denk, H.; Desmet, V.; Korb, G.; MacSween, R.N. Histological grading and staging of chronic hepatitis. J. Hepatol. 1995, 22, 696–699. [Google Scholar] [CrossRef]
- Brunt, E.M. Grading and staging the histopathological lesions of chronic hepatitis: The Knodell histology activity index and beyond. Hepatology 2000, 31, 241–246. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6. [Google Scholar] [CrossRef] [Green Version]
- Jimenez, W.; Pares, A.; Caballeria, J.; Heredia, D.; Bruguera, M.; Torres, M.; Rojkind, M.; Rodes, J. Measurement of fibrosis in needle liver biopsies: Evaluation of a colorimetric method. Hepatology 1985, 5, 815–818. [Google Scholar] [CrossRef] [PubMed]
- Manabe, N.; Chevallier, M.; Chossegros, P.; Causse, X.; Guerret, S.; Trepo, C.; Grimaud, J.A. Interferon-alpha 2b therapy reduces liver fibrosis in chronic non-A, non-B hepatitis: A quantitative histological evaluation. Hepatology 1993, 18, 1344–1349. [Google Scholar] [CrossRef] [PubMed]
- Nakayashi, H.; Takamatsu, S.; Nakano, H. A simple estimation of liver collagen content by the computed color image analyzer using sirius red stained sections. Kanzo 1993, 34, 212–218. [Google Scholar] [CrossRef] [Green Version]
- Chevallier, M.; Guerret, S.; Chossegros, P.; Gerard, F.; Grimaud, J.A. A histological semiquantitative scoring system for evaluation of hepatic fibrosis in needle liver biopsy specimens: Comparison with morphometric studies. Hepatology 1994, 20, 349–355. [Google Scholar] [CrossRef]
- Nakabayashi, H.; Takamatsu, S.; Tsujii, H.; Okamoto, Y.; Nakano, H.; Yamada, E.; Ichijima, K. Collagen content of liver biopsy specimens in patients with chronic hepatitis. Int. Hepatol. Commun. 1996, 4, 311–315. [Google Scholar] [CrossRef]
- Kage, M.; Shimamatu, K.; Nakashima, E.; Kojiro, M.; Inoue, O.; Yano, M. Long-term evolution of fibrosis from chronic hepatitis to cirrhosis in patients with hepatitis C: Morphometric analysis of repeated biopsies. Hepatology 1997, 25, 1028–1031. [Google Scholar] [CrossRef]
- Pilette, C.; Rousselet, M.C.; Bedossa, P.; Chappard, D.; Oberti, F.; Rifflet, H.; Maiga, M.Y.; Gallois, Y.; Cales, P. Histopathological evaluation of liver fibrosis: Quantitative image analysis vs semi-quantitative scores. J. Hepatol. 1998, 28, 439–446. [Google Scholar] [CrossRef]
- Masseroli, M.; Caballero, T.; O’Valle, F.; Del Moral, R.M.; Perez-Milena, A.; Del Moral, R.G. Automatic quantification of liver fibrosis: Design and validation of a new image analysis method: Comparison with semi-quantitative indexes of fibrosis. J. Hepatol. 2000, 32, 453–464. [Google Scholar] [CrossRef]
- Caballero, T.; Perez-Milena, A.; Masseroli, M.; O’Valle, F.; Salmeron, F.J.; Del Moral, R.M.; Sanchez-Salgado, G. Liver fibrosis assessment with semiquantitative indexes and image analysis quantification in sustained-responder and non-responder interferon-treated patients with chronic hepatitis C. J. Hepatol. 2001, 34, 740–747. [Google Scholar] [CrossRef]
- Colloredo, G.; Guido, M.; Sonzogni, A.; Leandro, G. Impact of liver biopsy size on histological evaluation of chronic viral hepatitis: The smaller the sample, the milder the disease. J. Hepatol. 2003, 39, 239–244. [Google Scholar] [CrossRef]
- Tanano, H.; Hasegawa, T.; Kimura, T.; Sasaki, T.; Kawahara, H.; Kubota, A.; Okada, A. Proposal of fibrosis index using image analyzer as a quantitative histological evaluation of liver fibrosis in biliary atresia. Pediatric Surg. Int. 2003, 19, 52–56. [Google Scholar] [CrossRef] [PubMed]
- Wright, M.; Thursz, M.; Pullen, R.; Thomas, H.; Goldin, R. Quantitative versus morphological assessment of liver fibrosis: Semi-quantitative scores are more robust than digital image fibrosis area estimation. Liver Int. 2003, 23, 28–34. [Google Scholar] [CrossRef] [PubMed]
- O’Brien, M.J.; Keating, N.M.; Elderiny, S.; Cerda, S.; Keaveny, A.P.; Afdhal, N.H.; Nunes, D.P. An assessment of digital image analysis to measure fibrosis in liver biopsy specimens of patients with chronic hepatitis C. Am. Soc. Clin. Pathol. 2000, 114, 712–718. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ryder, S.D.; Irving, W.L.; Jones, D.A.; Neal, K.R.; Underwood, J.C. Progression of hepatic fibrosis in patients with hepatitis C: A prospective repeat liver biopsy study. Gut 2004, 53, 451–455. [Google Scholar] [CrossRef]
- Lazzarini, A.L.; Levine, R.A.; Ploutz-Snyder, R.J.; Sanderson, S.O. Advances in digital quantification technique enhance discrimination between mild and advanced liver fibrosis in chronic hepatitis C. Liver Int. 2005, 25, 1142–1149. [Google Scholar] [CrossRef]
- Arima, M.; Terao, H.; Kashima, K.; Arita, T.; Nasu, M.; Nishizono, A. Regression of liver fibrosis in cases of chronic liver disease type C: Quantitative evaluation by using computed image analysis. Intern. Med. 2004, 43, 902–910. [Google Scholar] [CrossRef] [Green Version]
- Xie, S.B.; Ma, C.; Lin, C.S.; Zhang, Y.; Zhu, J.Y.; Ke, W.M. Collagen proportionate area of liver tissue determined by digital image analysis in patients with HBV-related decompensated cirrhosis. Hepatobiliary Pancreat. Dis. Int. 2011, 10, 497–501. [Google Scholar] [CrossRef]
- Manousou, P.; Dhillon, A.P.; Isgro, G.; Calvaruso, V.; Luong, T.V.; Tsochatzis, E.; Xirouchakis, E.; Kalambokis, G.; Cross, T.J.; Rolando, N.; et al. Digital image analysis of liver collagen predicts clinical outcome of recurrent hepatitis C virus 1 year after liver transplantation. Liver Transplant. 2011, 17, 178–188. [Google Scholar] [CrossRef]
- Manousou, P.; Burroughs, A.K.; Tsochatzis, E.; Isgro, G.; Hall, A.; Green, A.; Calvaruso, V.; Ma, G.L.; Gale, J.; Burgess, G.; et al. Digital image analysis of collagen assessment of progression of fibrosis in recurrent HCV after liver transplantation. J. Hepatol. 2013, 58, 962–968. [Google Scholar] [CrossRef] [Green Version]
- Calvaruso, V.; Burroughs, A.K.; Standish, R.; Manousou, P.; Grillo, F.; Leandro, G.; Maimone, S.; Pleguezuelo, M.; Xirouchakis, I.; Guerrini, G.P.; et al. Computer-assisted image analysis of liver collagen: Relationship to Ishak scoring and hepatic venous pressure gradient. Hepatology 2009, 49, 1236–1244. [Google Scholar] [CrossRef]
- Calvaruso, V.; Dhillon, A.P.; Tsochatzis, E.; Manousou, P.; Grillo, F.; Germani, G.; Patch, D.; O’Beirne, J.; Burroughs, A.K. Liver collagen proportionate area predicts decompensation in patients with recurrent hepatitis C virus cirrhosis after liver transplantation. J. Gastroenterol. Hepatol. 2012, 27, 1227–1232. [Google Scholar] [CrossRef] [PubMed]
- Tsochatzis, E.; Bruno, S.; Isgro, G.; Hall, A.; Theocharidou, E.; Manousou, P.; Dhillon, A.P.; Burroughs, A.K.; Luong, T.V. Collagen proportionate area is superior to other histological methods for sub-classifying cirrhosis and determining prognosis. J. Hepatol. 2014, 60, 948–954. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Huang, Y.; de Boer, W.B.; Adams, L.A.; MacQuillan, G.; Rossi, E.; Rigby, P.; Raftopoulos, S.C.; Bulsara, M.; Jeffrey, G.P. Image analysis of liver collagen using sirius red is more accurate and correlates better with serum fibrosis markers than trichrome. Liver Int. 2013, 33, 1249–1256. [Google Scholar] [CrossRef]
- Huang, Y.; de Boer, W.B.; Adams, L.A.; MacQuillan, G.; Bulsara, M.K.; Jeffrey, G.P. Image analysis of liver biopsy samples measures fibrosis and predicts clinical outcome. J. Hepatol. 2014, 61, 22–27. [Google Scholar] [CrossRef]
- Naveau, S.; Gaude, G.; Asnacios, A.; Agostini, H.; Abella, A.; Barri-Ova, N.; Dauvois, B.; Prevot, S.; Ngo, Y.; Munteanu, M.; et al. Diagnostic and prognostic values of noninvasive biomarkers of fibrosis in patients with alcoholic liver disease. Hepatology 2009, 49, 97–105. [Google Scholar] [CrossRef]
- Raftopoulos, S.C.; George, J.; Bourliere, M.; Rossi, E.; de Boer, W.P.; Jeffrey, G.P.; Bulsara, M.; Speers, D.J.; MacQuillan, G.; Ching, H.L.; et al. Comparison of noninvasive models of fibrosis in chronic hepatitis B. Hepatol. Int. 2012, 6, 457–467. [Google Scholar] [CrossRef]
- Campos, C.F.; Paiva, D.D.; Perazzo, H.; Moreira, P.S.; Areco, L.F.; Terra, C.; Perez, R.; Figueiredo, F.A. An inexpensive and worldwide available digital image analysis technique for histological fibrosis quantification in chronic hepatitis C. J. Viral Hepat. 2014, 21, 216–222. [Google Scholar] [CrossRef]
- Zhou, Y.; Ru, G.Q.; Yan, R.; Wang, M.S.; Chen, M.J.; Yu, L.L.; Wang, H. An inexpensive digital image analysis technique for liver fibrosis quantification in chronic hepatitis B patients. Ann. Hepatol. 2017, 16, 881–887. [Google Scholar] [CrossRef]
- Banerjee, R.; Pavlides, M.; Tunnicliffe, E.M.; Piechnik, S.K.; Sarania, N.; Philips, R.; Collier, J.D.; Booth, J.C.; Schneider, J.E.; Wang, L.M.; et al. Multiparametric magnetic resonance for the non-invasive diagnosis of liver disease. J. Hepatol. 2014, 60, 69–77. [Google Scholar] [CrossRef] [Green Version]
- Marino, Z.; Mensa, L.; Crespo, G.; Miquel, R.; Bruguera, M.; Perez-Del-Pulgar, S.; Bosch, J.; Forns, X.; Navasa, M. Early periportal sinusoidal fibrosis is an accurate marker of accelerated HCV recurrence after liver transplantation. J. Hepatol. 2014, 61, 270–277. [Google Scholar] [CrossRef]
- Chen, S.H.; Peng, C.Y.; Lai, H.C.; Chang, I.P.; Lee, C.J.; Su, W.P.; Lin, C.H.; Kao, J.T.; Chuang, P.H. Head-to-head comparison between collagen proportionate area and acoustic radiation force impulse elastography in liver fibrosis quantification in chronic hepatitis C. PLoS ONE 2015, 10, e0140554. [Google Scholar] [CrossRef] [PubMed]
- Ding, H.; Ma, J.J.; Wang, W.P.; Zeng, W.J.; Jiang, T.; Huang, B.J.; Chen, S.Y. Assessment of liver fibrosis: The relationship between point shear wave elastography and quantitative histological analysis. J. Gastroenterol. Hepatol. 2015, 30, 553–558. [Google Scholar] [CrossRef] [PubMed]
- Thiele, M.; Detlefsen, S.; Sevelsted, M.L.; Madsen, B.S.; Fuglsang, H.J.; Fialla, A.D.; Trebicka, J.; Krag, A. Transient and 2-dimensional shear-wave elastography provide comparable assessment of alcoholic liver fibrosis and cirrhosis. Gastroenterology 2016, 150, 123–133. [Google Scholar] [CrossRef] [PubMed]
- Rastellini, S.; Goossens, N.; Clement, S.; Lanthier, N.; Negro, F.; Rubbia-Brandt, L.; Spahr, L. Collagen proportionate area correlates to hepatic venous pressure gradient in non-abstinent cirrhotic patients with alcoholic liver disease. World J. Hepatol. 2018, 10, 73–81. [Google Scholar] [CrossRef] [PubMed]
- Ali, G.; Mohsin, S.; Khan, M.; Nasir, G.A.; Shams, S.; Khan, S.N.; Riazuddin, S. Nitric oxide augments mesenchymal stem cell ability to repair liver fibrosis. J. Transl. Med. 2012, 10, 75. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sun, W.; Chang, S.; Tai, D.C.; Tan, N.; Xiao, G.; Tang, H.; Yu, H. Nonlinear optical microscopy: Use of second harmonic generation and two-photon microscopy for automated quantitative liver fibrosis studies. J. Biomed. Opt. 2008, 13, 064010. [Google Scholar] [CrossRef]
- Tai, D.C.; Tan, N.; Xu, S.; Kang, C.H.; Chia, S.M.; Cheng, C.L.; Wee, A.; Wei, C.L.; Raja, A.M.; Xiao, G.; et al. Fibro-C-Index: Comprehensive, morphology-based quantification of liver fibrosis using second harmonic generation and two-photon microscopy. J. Biomed. Opt. 2009, 14, 044013. [Google Scholar] [CrossRef]
- Guilbert, T.; Odin, C.; Le Grand, Y.; Gailhouste, L.; Turlin, B.; Ezan, F.; Desille, Y.; Baffet, G.; Guyader, D. A robust collagen scoring method for human liver fibrosis by second harmonic microscopy. Opt. Express 2010, 18, 25794–25807. [Google Scholar] [CrossRef] [Green Version]
- Sun, Y.; Zhou, J.; Wang, L.; Wu, X.; Chen, Y.; Piao, H.; Lu, L.; Jiang, W.; Xu, Y.; Feng, B.; et al. New classification of liver biopsy assessment for fibrosis in chronic hepatitis B patients before and after treatment. Hepatology 2017, 65, 1438–1450. [Google Scholar] [CrossRef] [Green Version]
- Matalka, I.I.; Al-Jarrah, O.M.; Manasrah, T.M. Quantitative assessment of liver fibrosis: A novel automated image analysis method. Liver Int. 2006, 26, 1054–1064. [Google Scholar] [CrossRef]
- Stanciu, S.G.; Xu, S.; Peng, Q.; Yan, J.; Stanciu, G.A.; Welsch, R.E.; So, P.T.; Csucs, G.; Yu, H. Experimenting liver fibrosis diagnostic by two photon excitation microscopy and Bag-of-Features image classification. Sci. Rep. 2014, 4. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Xu, S.; Wang, Y.; Tai, D.C.S.; Wang, S.; Cheng, C.L.; Peng, Q.; Jan, J.; Chen, Y.; Sun, J.; Liang, X.; et al. qFibrosis: A fully-quantitative innovative method incorporating histological features to facilitate accurate fibrosis scoring in animal model and chronic hepatitis B patients. J. Hepatol. 2014, 61, 260–269. [Google Scholar] [CrossRef] [Green Version]
- Sun, Y.; Zhou, J.; Wu, X.; Chen, Y.; Piao, H.; Lu, L.; Ding, H.; Nan, Y.; Jiang, W.; Wang, T.; et al. Quantitative assessment of liver fibrosis (qFibrosis) reveals precise outcomes in Ishak "stable" patients on anti-HBV therapy. Sci. Rep. 2018, 8, 2989. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, T.H.; Chen, T.C.; Teng, X.; Liang, K.H.; Yeh, C.T. Automated biphasic morphological assessment of hepatitis B-related liver fibrosis using second harmonic generation microscopy. Sci. Rep. 2015, 11, 12962. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Meejaroen, K.; Chaweechan, C.; Khodsiri, W.; Khu-smith, V.; Watchareeruetai, U.; Sornmagura, P.; Kittiyakara, T. Detection of fibrosis in liver biopsy images by using Bayesian classifier. In Proceedings of the 7th International Conference on Knowledge and Smart Technology (KST), Chon Buri, Thailand, 28–31 January 2015; Institute of Electrical and Electronics (IEEE): Piscataway, NJ, USA, 2015. [Google Scholar] [CrossRef]
- Thong-on, P.; Watchareeruetai, U. Detection of fibrosis in liver biopsy images using multi-objective genetic programming. In Proceedings of the 9th International Conference on Information Technology and Electrical Engineering (ICITEE), Phuket, Thailand, 12–13 October 2017; Institute of Electrical and Electronics (IEEE): Piscataway, NJ, USA, 2017. [Google Scholar] [CrossRef]
- Giannakeas, N.; Tsipouras, M.G.; Tzallas, A.T.; Kyriakidi, K.; Tsianou, Z.E.; Manousou, P.; Hall, A.; Karvounis, E.C.; Tsianos, V.; Tsianos, E. A clustering based method for collagen proportional area extraction in liver biopsy images. Proc. IEEE Eng. Med. Biol. Soc. Annu. Conf. 2015, 2015, 3097–30100. [Google Scholar] [CrossRef]
- Tsipouras, M.G.; Giannakeas, N.; Tzallas, A.T.; Tsianou, Z.E.; Manousou, P.; Hall, A.; Tsoulos, I.; Tsianos, E. A methodology for automated CPA extraction using liver biopsy image analysis and machine learning techniques. Comput. Methods Progr. Biomed. 2017, 140, 31–68. [Google Scholar] [CrossRef] [PubMed]
- Tsouros, D.C.; Smyrlis, P.N.; Tsipouras, M.G.; Tsalikakis, D.G.; Giannakeas, N.; Tzallas, A.T.; Manousou, P. Automated collagen proportional area extraction in liver biopsy images using a novel classification via clustering algorithm. In Proceedings of the 30th International Symposium on Computer-Based Medical Systems, Thessaloniki, Greece, 22–24 June 2017; Institute of Electrical and Electronics (IEEE): Piscataway, NJ, USA, 2017; pp. 30–34. [Google Scholar] [CrossRef]
- Vicas, C.; Rusu, I.; Al Hajjar, N.; Lupsor-Platon, M. Deep convolutional neural nets for objective steatosis detection from liver samples. In Proceedings of the 13th IEEE International Conference on Intelligent Computer Communication and Processing (ICCP), Cluj-Napoca, Romania, 7–9 September 2017; Institute of Electrical and Electronics Engineers (IEEE): Piscataway, NJ, USA, 2017; pp. 385–390. [Google Scholar] [CrossRef]
- Yu, Y.; Wang, J.; Ng, C.W.; Ma, Y.; Mo, S.; Fong, E.L.S.; Xing, J.; Song, Z.; Xie, Y.; Si, K.; et al. Deep learning enables automated scoring of liver fibrosis stages. Sci. Rep. 2018, 30, 16016. [Google Scholar] [CrossRef] [Green Version]


| Knodell [5] | Scheuer [6] | ||
| Grade | Description | Grade | Description |
| 0 | No fibrosis | 0 | None |
| 1 | Fibrous portal expansion | 1 | Enlarged, fibrotic portal tracts |
| 2 | Bridging fibrosis (portal-portal or portal-central linkage) | 2 | Periportal or portal-portal septa but intact architecture |
| 3 | Cirrhosis | 3 | Periportal or portal-portal septa but intact architecture |
| 4 | Probable or definite cirrhosis | ||
| METAVIR [7] | Ishak [8] | ||
| Grade | Description | Grade | Description |
| 0 | No fibrosis | 0 | No fibrosis |
| 1 | Stellate enlargement of portal tract, but without septa formation | 1 | Fibrous expansion of some portal areas, with or without short fibrous septa |
| 2 | Enlargement of portal tract with rare septa formation | 2 | Fibrous expansion of most portal areas, with or without short fibrous septa |
| 3 | Numerous septa without cirrhosis | 3 | Fibrous expansion of most portal areas with an occasional portal to portal (P-P) bridging |
| 4 | Cirrhosis | 4 | Fibrous expansion of portal areas with marked bridging (P-P) as well as portal-central (P-C) |
| 5 | Marked bridging (P-P and/or P-C) with occasional nodules (incomplete cirrhosis) | ||
| 6 | Cirrhosis, probable or definite | ||
| Author/Year | Dataset/Histological Stain | HAI | Image Analysis Method | Results/Remarks |
|---|---|---|---|---|
| Jimenez et al. 1985 [11] | 38 samples (8 steatosis w/o fibrosis, 8 chronic hepatitis, 7 fibrotic, 15 alcoholic cirrhotic patients) Stains: Sirius red, Fast green | - | - | Histomorphometric—colorimetric CPA correlation (r = 0.77, p < 0.001) |
| Manabe et al. 1993 [12] | 59 samples (54 HCV antibody patients) Stains: Gordon-Sweet’s silver, Sirius Fast red | Knodell | Histomorphometric analysis (Biocom 200) | Histomorphometric—colorimetric CPA correlation (r = 0.778) |
| Nakayashi et al. 1993 [13] | 24 samples (autopsy, hepatic transfusion patients) Stains: Sirius red, Fast green, Azan, Van Gieson | - | Biochemical analysis. Planimetric measurement (SPICCA II) | Hydroxyproline—fibrosis content correlation (r = 0.887) |
| Chevallier et al. 1994 [14] | 200 samples (alcoholic and viral patients) Stain: picro-Sirius red | METAVIR (modified) | Histomorphometric analysis (Biocom 200) | SSS—SDTC correlation (r = 0.73, p < 10−5) |
| Nakabayashi et al. 1996 [15] | 65 samples (liver disease patients) 5 normal as controls | Knodell (modified) | Biochemical analysis. Planimetric measurement (SPICCA II) | CI—Biochemical analysis correlation (r = 0.88, p < 0.0001) |
| Kage et al. 1997 [16] | 45 samples (25 CHC patients. 20 CHB patients as controls) Stains: H&E, Azan | Scheuer | Image analysis (Nexus Qube) | Fibrosis stage—area correlations: hepatitis B (r = 0.67, p < 0.001), hepatitis C (r = 0.75, p < 0.001) |
| Pilette et al. 1998 [17] | 243 samples (83 viral liver disease. 160 ALD patients) Stains: H&E-Saffran, MT, picro-Sirius red | METAVIR. Knodell | Manual thresholding. Semi-automated artifact elimination | DIA—semi-quantitative scores correlation (r = 0.84, p < 10−4) |
| Masseroli et al. 2000 [18] | 48 samples (CHC patients), 11 normal as controls Stain: picro-Sirius red | Knodell. Scheuer | Adaptive thresholding. User interference (FibroQuant) | FibroQuant—HAI correlations (0.72 < r < 0.83, p < 0.0001) |
| Caballero et al. 2001 [19] | 98 samples (HCV-chronic hepatitis patients) Stain: picro-Sirius red | Knodell (modified). Scheuer (modified) | Automatic segmentation & CPA quantification (FibroQuant) | FibroQuant: porto-periportal—septal fibrosis correlation (p ≤ 0.05) |
| Colloredo et al. 2003 [20] | 161 samples (chronic viral hepatitis patients (B, C or D) Stains: H&E, Periodic Acid Schiff, MT, Perl’s | Ishak | - | Biopsy length Reduction—Ishak correlation (p < 0.001) |
| Tanano et al. 2003 [21] | 46 samples (BA fibrosis index patients) Stain: Azan Mallory | - | Monochrome image production. Morphometric editing. Adequate thresholding | CV of FI range (%): 2.9–7.7 in ×40 magnification |
| Wright et al. 2003 [22] | 30 sections (from 300 CHC samples) Stain: picro-Sirius red | Ishak (modified) | Grayscale conversion. Optimal thresholding (Scion) | DIA—HAI intra, inter-observer correlations: DIA (r = 0.889, r = 0.837), HAI (r = 0.878, r = 0.776) |
| O’Brien et al. 2000 [23] | 30 samples (CHC patients) Stains: H&E, Mallory trichrome | Ishak | Interactive thresholding (Optimas 5.0) | Fibrosis ratio—Ishak correlation (r = 0.58, p < 0.001) |
| Ryder et al. 2004 [24] | 214 samples (HCV patients) Stain: Perl’s | Knodell. Ishak | - | Knodell—Ishak correlation (p = 0.0001) |
| Lazzarini et al. 2005 [25] | 164 samples (CHC patients) Stains: H&E, trichrome | Ishak | Binary interactive thresholding. Direct pixel counting (Image-Pro Plus 4.5) | CPA—Ishak correlation (p < 0.001). AUROC = 0.982–1.00 |
| Arima et al. 2004 [26] | 25 samples (from HVC, 20 IFN treatment patients) Stains: H&E, Azan-Mallory | - | Image editing (Adobe Photoshop 5.02i). CPA quantification (NIH) | Significant fibrosis regression (%): viral eradication (7.2 ± 1.5), IFN treatment (2.7 ± 0.5) |
| Xie et al. 2011 [27] | 53 samples (CHB cirrhosis patients) Stains: H&E, Masson’s trichrome | - | Intensity adjustment. Random selection of non-overlapping visual fields (Image-Pro plus 6.0) | CPA: MELD score—serum TBIL—prothrombin B ISR correlation (p < 0.001) |
| Manousou et al. 2011 [28] | 155 samples (HCV patients after LT) Stain: picro-Sirius red | Ishak | Direct CPA determination, quantification | MVA in CPA decompensation (p = 0.010) |
| Manousou et al. 2013 [29] | 155 samples (HCV patients after LT) Stain: picro-Sirius red | Ishak | Direct CPA determination, quantification | MVA in CPA decompensation (p = 0.001) |
| Calvaruso et al. 2009 [30] | 250 samples (from HCV 115 patients) Stain: picro-Sirius red | Ishak | Manual thresholding, artifact elimination (Zeiss KS300) | Median CPA—Ishak 6—HVPG (r = 0.62, p < 0.001) |
| Calvaruso et al. 2012 [31] | 62 samples (HCV patients after LT) Stain: picro-Sirius red | Ishak | Manual thresholding, artifact elimination (Zeiss KS300) | CPA—HVPG ≥ 10 mmHg correlation (p = 0.04) |
| Tsochatzis et al. 2014 [32] | 69 samples (post-LT CLD patients) Stains: H&E, DPAS, Orcein, Victoria Blue, Perl’s | Laennec. Kumar & Nagula | RGB thresholding. Manual artifacts elimination. CPA measurement (Zeiss KS300) | CPA AUROC = 0.909. CPA correlation: Laennec (p < 0.001), Kumar (p = 0.003) |
| Huang et al. 2013 [33] | 201 samples (CHC patients) Stains: picro-Sirius red, MT | METAVIR | Threshold determination. Fibrotic areas manual extraction. | CPAs > CPAt—METAVIR correlation (p < 0.001) |
| Huang et al. 2014 [34] | 533 samples (CHC patients) Stain: Masson’s trichrome | METAVIR | Manual area exclusion. Optimus threshold determination (Aperio) | CPA—METAVIR correlation (p < 0.001) |
| Author/Year | Dataset/Histological Stain | HAI | Image Analysis Method | Results/Remarks |
|---|---|---|---|---|
| Naveau et al. 2009 [35] | 218 samples (ALD patients) Stains: H&E-Saffran, MT, picro-Sirius red | METAVIR | - | FibrometerA, Hepascore vs. FibroTest fibrosis (AUROC = 0.83 ± 0.03), vs. APRI—Forns—FIB4 correlation (p < 0.01) |
| Raftopoulos et al. 2012 [36] | 179 samples (CHB patients) Stain: Masson’s trichrome | METAVIR | Manual areas exclusion (Aperio ImageScope). Batch analysis (Pixelcount 9.0) | Morphometry correlation: Hepascore (r = 0.603, p < 0.001), FibroTest (r = 0.392, p = 0.03), HBeAg-positive (r = 0.492, p = 0.001) |
| Campos et al. 2014 [37] | 282 samples (CHC patients) Stain: Masson’s trichrome | METAVIR. Ishak | Image enhancement. Background removal. Fibrotic area extraction (Adobe Photoshop) | DIA—Ishak, METAVIR correlation (r = 0.95, 0.92, p < 0.001) |
| Zhou et al. 2017 [38] | 142 samples (CHB patients) Stain: Sirius red, Masson’s trichrome | Laennec. METAVIR (modified). Ishak. METAVIR | Background, undesired areas exclusion (Adobe Photoshop) | DIA—Ishak, METAVIR, Laennec correlation (r = 0.83, 0.86, 0.84, p < 0.001) |
| Banerjee et al. 2014 [39] | 79 samples, 7 normal as controls | Ishak (modified) | ROI volume assessment | MR—Histology fibrosis correlation (r = 0.68, p < 0.0001). Fibrosis AUROC (0.94) |
| Marino et al. 2014 [40] | 101 samples (HCV patients after LT) Stain: H&E, MT, Sirius red | METAVIR | - | MT—SR stains SF correlation (p < 0.01) |
| Chen et al. 2015 [41] | 137 samples (CHC patients) Stain: Masson’s trichrome | METAVIR | Threshold setting (Adobe Photoshop CS6). CPA calculation (Image-Pro 7.0) | CPA—SWV correlation (p < 0.2585) |
| Ding et al. 2015 [42] | 78 samples (CHB patients) | Scheuer | Intensity adjustment. Random selection of non-overlapping visual fields. CPA assessment (Image-Pro plus 6.0) | PSWE correlation: CPA (r = 0.628, p < 0.05), Scheuer (r = 0.473, p < 0.05), [13] system (r = 0.487, p < 0.05) |
| Thiele et al. 2016 [43] | 99 samples (chronic ALD patients) Stain: Sirius red | Ishak | Samples digitization (Nanozoomer 2.0 HT). Image analyzing (VISIOmorph 4.3.6) | TE—2D-SWE AUC ≥ 0.92 |
| Rastellini et al. 2018 [44] | 61 samples (cALD patients), 9 normal as controls Stain: picro-Sirius red | - | CPA quantification (Qwin Leica Q550IW) | Mean CPA in ALD (7.1%, p = 0.17). Fibrosis—HVPG correlation (p = 0.02) |
| Ali et al. 2012 [45] | 11 samples (SNP-pretreated mice) Stain: Sirius red | - | Fibrosis areas quantification (Image J) | Fibrosis: SNP-MSc (0.4 ± 0.3), CCl4 (4.4 ± 2.4), MSc (1.9 ± 1.5), SNP (1.3 ± 0.4) |
| Author/Year | Dataset/Histological Stain | HAI | Image Analysis Method | Results/Remarks |
|---|---|---|---|---|
| Sun et al. 2008 [46] | 3 samples (CLD Wistar rats) Stains: Sirius red, Masson’s trichrome | - | SHG background removal. Frequency domain filtering. Otsu segmentation. Morphological erosion & dilation | CPA (%): SHG > MT stain, SHG = SR stain |
| Tai et al. 2009 [47] | 3 human samples, 20 animal samples (15 viral Wistar rats. 5 normal as controls) Stain: Masson’s trichrome | Ishak (modified). Ishak | Threshold levels determination (MATLAB) | Human CPA (4.21 ± 0.67%) vs. Fibro-C-Index (2.78% ± 0.44%) |
| Guilbert et al. 2014 [48] | 12 samples (CLD, ALD, hepatitis B or C patients) Stain: with Sirius red | METAVIR | Mean SHG intensity. Intensity threshold determination (Fluoview) | CPA—METAVIR (F3, F4) linear correlations (R2 = 0.997, 0.9944) |
| Sun et al. 2017 [49] | 71 samples (CHB patients) Stain: H&E, reticulin and MT (at a later stage) | Ishak. METAVIR. Laennec | SHG image collagen area extraction and normalization with TPEF signals | CPA—HAIs correlation (p = 0.001) |
| Author/Year | Dataset/Histological Stain | HAI | Image Analysis Method | Results/Remarks |
|---|---|---|---|---|
| Matalka et al. 2006 [50] | 210 samples (CLD patients), 50 normal samples Stain: Van Geison | Ishak | Contrast enhancement. Morphological opening. K-means clustering. ANN classification (MATLAB 6.5) | AQS testing accuracy: 94.69%. AQS—Ishak correlations (Ph1: 0.889, Ph2: 0.815) |
| Stanciu et al. 2014 [51] | 200 samples (TAA-induced rats) Stain: MT (at a later stage) | METAVIR | SHG/TPEF image preprocessing. K-means clustering. BoF, k-NN classification | Mean PR-area ≤ 0.9719 |
| Xu et al. 2014 [52] | 162 samples (CHB patients), 25 TAA-induced rats) Stain: MT (at a later stage) | METAVIR. Ishak | Automated SHG/TPEF image preprocessing. MLR classification (qFibrosis) | qFibrosis—Ishak 5, 6 (AUC = 0.73, p = 0.008). qFibrosis—METAVIR: animals (AUC ≤ 0.99, p < 0.001), humans (AUC ≤ 0.97, p < 0.05) |
| Sun et al. 2018 [53] | 162 samples (CHB patients) Stain: H&E, MT, Reticulin | Ishak (modified) | Automated SHG/TPEF image preprocessing. (qFibrosis). Feature selection, model fitting (MATLAB 2015a) | qFibrosis—Ishak correlation: LS (r = 0.6, p < 0.001), LS after treatment (r = 0.3, p < 0.001) |
| Wang et al. 2015 [54] | 175 samples (cHBV patients) Stain: MT (at a later stage) | Ishak | Binary image conversion. Collagen area segmentation GLM, SVM classification | GLM—Ishak 1–4 vs. 5–6 (AUC = 0.829). SVM—Ishak AUC (1 vs. 2–6 = 0.745, 1–2 vs. 3–6 = 0.774, 1–3 vs. 4–6 = 0.797) |
| Meejaroen et al. 2015 [55] | 34 samples (fibrosis patients) | - | Image enhancement. Low-pass filtering. Bayesian classification | Classification accuracy = 91.42% |
| Thong-on and Watchareeruetai 2017 [56] | 32 samples (fibrosis patients) | - | MOGP Segmentation (NSGA-II). Bayesian classification | NSGA-II segmentation accuracy = 93.05%. Bayesian classification accuracy = 92.33% |
| Giannakeas et al. 2015 [57] | 25 samples (CHC patients) Stain: picro-Sirius Red | Ishak | Manual fibrotic area annotation. K-means color image clustering | CPA segmentation error rates ≤ 2.93% |
| Tsipouras et al. 2017 [58] | 79 samples (HCV patients) Stain: picro-Sirius red | - | K-means, Fuzzy C-means clustering. KNN, C4.5, RF, MLP, SVM fibrosis regions classification | Mean CPA classification error (abs) = 1.31%. CCC = 0.923 |
| Tsouros et al. 2017 [59] | 8 samples (HCV patients) | - | K-means algorithm (parameterized) image clustering. Bayesian classification | Mean classification accuracy = 97.79%, 1/2 of image dataset error < 1% |
| Vicas et al. 2017 [60] | 107 samples (fibrosis and steatosis prevalence) | - | Image preprocessing. GBT, SVM, LR, RF, CNN classification. U-Net Segmentation | R2 ≤ 89.3 1 |
| Yu et al. 2018 [61] | 25 samples (21 TAA-induced rats and 4 as controls) Stain: picro-Sirius red (at a later stage) | METAVIR | SHG contrast enhancement. Morphological closing. ANN, MLR, SVM, RF, AlexNet-CNN classification | AUROC: CNN ≤ 0.95, ANN ≤ 1.00, MLR ≤ 1.00, SVM ≤ 0.99, RF ≤ 0.99 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Arjmand, A.; Tsipouras, M.G.; Tzallas, A.T.; Forlano, R.; Manousou, P.; Giannakeas, N. Quantification of Liver Fibrosis—A Comparative Study. Appl. Sci. 2020, 10, 447. https://doi.org/10.3390/app10020447
Arjmand A, Tsipouras MG, Tzallas AT, Forlano R, Manousou P, Giannakeas N. Quantification of Liver Fibrosis—A Comparative Study. Applied Sciences. 2020; 10(2):447. https://doi.org/10.3390/app10020447
Chicago/Turabian StyleArjmand, Alexandros, Markos G. Tsipouras, Alexandros T. Tzallas, Roberta Forlano, Pinelopi Manousou, and Nikolaos Giannakeas. 2020. "Quantification of Liver Fibrosis—A Comparative Study" Applied Sciences 10, no. 2: 447. https://doi.org/10.3390/app10020447
APA StyleArjmand, A., Tsipouras, M. G., Tzallas, A. T., Forlano, R., Manousou, P., & Giannakeas, N. (2020). Quantification of Liver Fibrosis—A Comparative Study. Applied Sciences, 10(2), 447. https://doi.org/10.3390/app10020447









