MobiDiabet: Mobile Telemonitoring System for Patients with Type 2 Diabetes Mellitus (T2DM)
Abstract
:1. Introduction
- Recommendations by specialists (physicians and nutritionists) mainly in potential risk situations,
- Diet control that includes menus and eating patterns prepared by specialists and assigned according to the calories needed by each patient, and
- An educational approach that guides and sensitizes patients about the possible complications of their condition.
2. Materials and Methods
2.1. Use Case Diagrams
- Doctor/physician: This actor is a general physician, with an intermediate level in the use of technology, which provides care to different patients monthly and with access to consultations with internet infrastructure.
- Nutritionist: The nutritionist actor is a nutrition specialist, with an intermediate level in the use of technology, serving multiple patients monthly, and with access to internet infrastructure.
- Patient: This actor is a person with a diagnosis of T2DM, with first level care, i.e., medical care, provided in family medicine units. For this type of user, the experience in the use of technology is not mandatory.
- Administrator: This actor can be a general physician, with an intermediate level in the use of technology, with access to internet infrastructure.
2.1.1. Security UC Diagram
- UC-01 Authenticate: In this UC, users enter their user information, such as username and password, to get access to their respective applications.
- UC-02 CRUD Users: The user who interacts with this UC is only the administrator who is the exclusive actor who can create, read, update, and delete physicians, nutritionists, and patients of the system.
- UC-03 Videos Management: This UC aims to handle the health education material and add links to videos.
2.1.2. General Physician Follow-Up UC Diagram
- UC-04 CRUD Clinical history: This UC is for the management of the patient’s medical history; the general physician is in charge to create, update, and delete the medical history information concerning the patient’s health status.
- UC-05 Consult glucose results: In this case, the physician can review the glucose results that the patient has been recording and are presented in a table indicating the test date, type of blood glucose test, and the glucose result.
- UC-06 Consult patient progress: The physician can review monthly all the results of a patient, which are displayed in graphs, to see the progress.
- UC-07 Consult video report: This section of health education shows the videos that the patient has seen.
- UC-08 Consult alert history: In this section, the physician can review all alerts generated to a patient when recording glucose results.
- UC-09 CR Laboratory studies: The physician can record the results of the different laboratory studies such as blood chemistry test, liver biometrics, thyroid profile test, general urine test, and liver function test, which have been performed on the patient. Furthermore, the physician can also see the records with reference values.
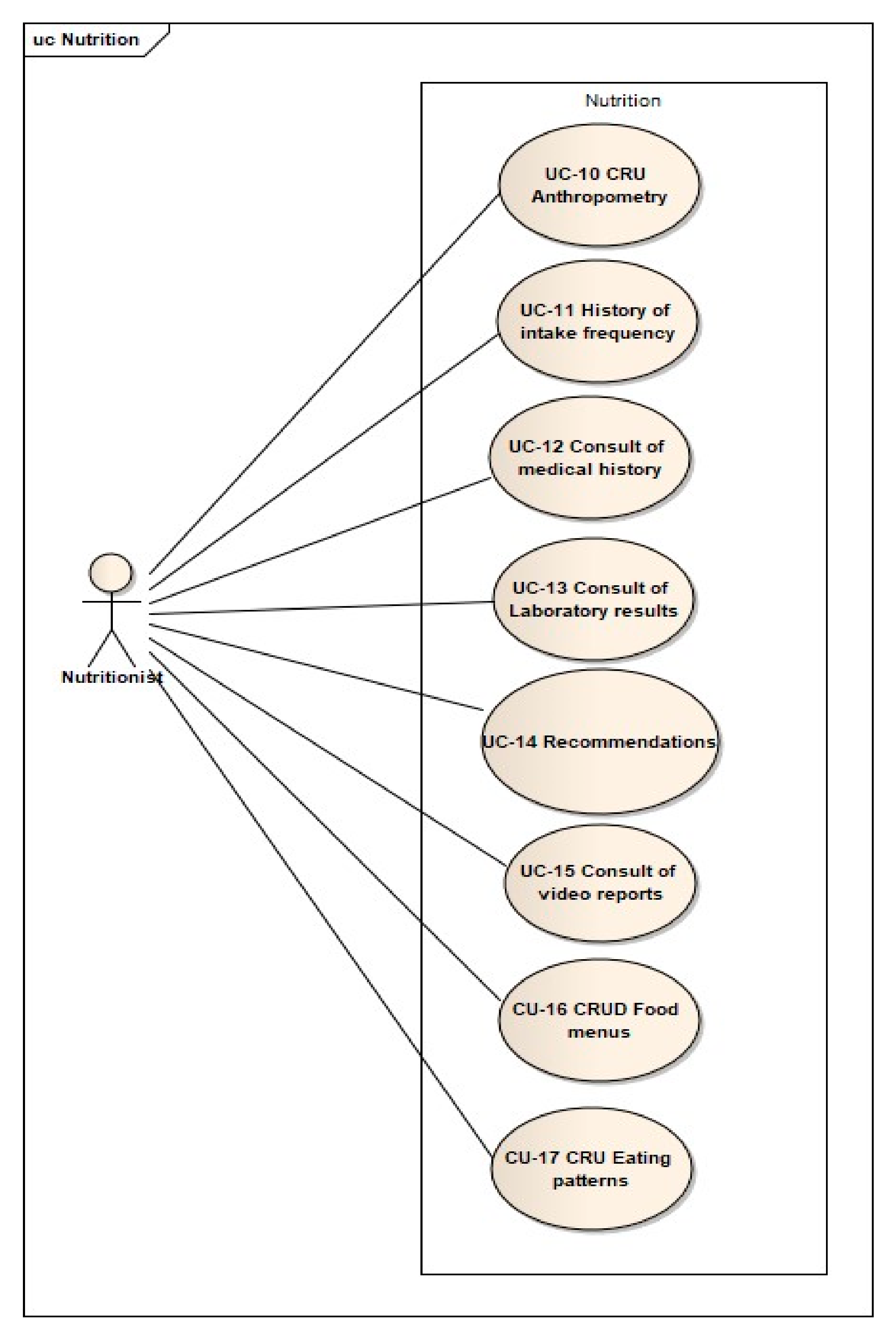
2.1.3. Nutrition UC Diagram
- UC-10 CRUD Anthropometry: This allows the nutritionist to record the anthropometry data of patients, to assign an appropriate food plan, and to monitor their treatment.
- UC-11 History of intake frequency: This UC allows the nutritionist to review the responses to the frequency of food intake questionnaire, which patients respond to before an appointment.
- UC-12 Consult of medical history: This enables the nutritionist to monitor the information about the patient’s medical history.
- UC-13 Consult of Laboratory results: This allows the nutritionist to review patient laboratory data and the general physician reports.
- UC-14 Recommendations: This UC allows the nutritionist to submit personal recommendations to patients.
- UC-15 Consult of video reports: Through this UC, the nutritionist can see the list of videos that each patient has seen from the health education section.
- UC-16 CRUD Food menus: This use case allows the nutritionist to manage the food menus that will be consulted by the patients.
- UC-17 CRU Eating patterns: This use case allows the administration of eating patterns that the nutritionist can add and modify, which patients can consult.
2.1.4. Patient Application UC Diagram
- UC-18 Consult food menu: The patient can consult the different food menus with the calories previously assigned by the nutritionist.
- UC-19 Consult eating pattern: The patient sees the eating pattern assigned by the nutritionist.
- UC-20 Consult equivalent foods: The patient can choose the food groups containing a list of foods that have the quantity and measure unit appropriate to intake.
- UC-21 Record questionnaire responses: the patient answers to the questionnaires in this UC to know the type and frequency of the food that he eats. The nutritionist will consult the answers in UC-11.
- UC-22 Consult recommendations: The patient can see the recommendations that the nutritionist sent before.
- UC-23 Record glucose results: This allows the patient to records glucose results depending on the type of blood glucose test performed.
- UC-24 Consult glucose history: The patient can check the history of all glucose reports.
- UC-25 Consult laboratory results: This allows the patient to review the results of laboratory tests that the physician previously recorded.
- UC-26 Consult health education videos: Through this UC, the patient can consult and view videos recommended by physicians in the health education section, and mark those the patient has seen.
2.2. Data Model
- FoodsItems: This table contains the food items with the details of the equivalent system.
- AlertsToDoctor: This table stores the generated alerts when patients record inadequate glucose levels.
- Anthropometry: The nutritionist uses this table for allocating caloric intake. This table is associated with a specific food group and is related to the patient’s table.
- HematicBiometry: This table contains all registers of the patient’s laboratory results.
- QuestionnaireIF: This stores all the responses to the food intake frequency questionnaire.
- VideoStatus: This table is linked to Videos and Patients tables, and this has the registers of the videos seen by the patients.
- Urinalysis: This table contains the results of the patient’s laboratory studies.
- LiverFunction: This table has the results of the liver function test of a patient.
- FoodGroups: This table contains food groups such as vegetables, fruits, legumes, among others.
- MedicalHistory: This table contains fields concerning the management of the patient’s medical history.
- Doctor: This contains the ID number, specialty, and other information on the health personnel.
- FoodMenus: This stores the description, calories, and food menus.
- Nutritionist: This contains the nutritionist’s ID number that is related to multiple patients.
- Patients: This table contains patients′ data and relationships with the health personnel in charge of each one among other useful information.
- NutritionalPattern: This table contains the nutritional pattern assigned by the nutritionist.
- ThyroidProfile: This contains the results of thyroid function tests.
- BloodChemistry: This table contains the laboratory results recorded by the patient of his blood chemistry tests.
- RecomendationsToPatient: This stores the recommendations that the nutritionist makes to patients.
- GlucoseResults: This table is one of the most important, because this contains the glucose results that the patient records, and this is related to the Patients and AlertsToDoctor tables
- LaboratoryResults: This contains the relationship with the table of patients and the different laboratory results such as blood chemistry test, thyroid profile test, general urine test, liver function test, and complete blood count.
- Rols: This table is one of the main ones, because it holds the types of users that can access the system.
- Users: This is one of the main tables, because it contains the general information of the users registered in the system, both health personnel and patients.
- Videos: This contains the description and link of the videos for the health education section.
2.3. Component Diagram
- Model: This component is exclusively responsible for managing the application data and storing the information that users add.
- View: This represents the model state, without being directly linked to this component; its goal is to show the information to the user.
- Controller: This component represents the link between the model and the view. It is responsible for notifying the model when the user manipulates the view and is responsible for managing the changes that the user makes.
- Web mobile application: Handles elements present in the graphical user interface.
- Data Access Object: Maps the information that is stored in the database. This mapping is performed to manipulate the information from code before appearing at the graphical interface or database.
- Spring MVC controller: Controls the application logic and responds to requests from the graphical interface or some other process that perform requests.
- Database: Manages the system’s database.
- PostgreSQL is an open-source relational database system.
- Angular is a web application development framework made in JavaScript by Google. Angular is flexible to work with different patterns.
- Java is a multiplatform programming language that can be used to create different applications for personal computers, mobile devices, or the web.
- Spring MVC is an open-source framework that works as a framework for the Java platform.
3. Results: Telemonitoring System
3.1. Mobile-Web-Application Focused on Health Personnel
3.1.1. Administrator User Services
3.1.2. Physician User Services
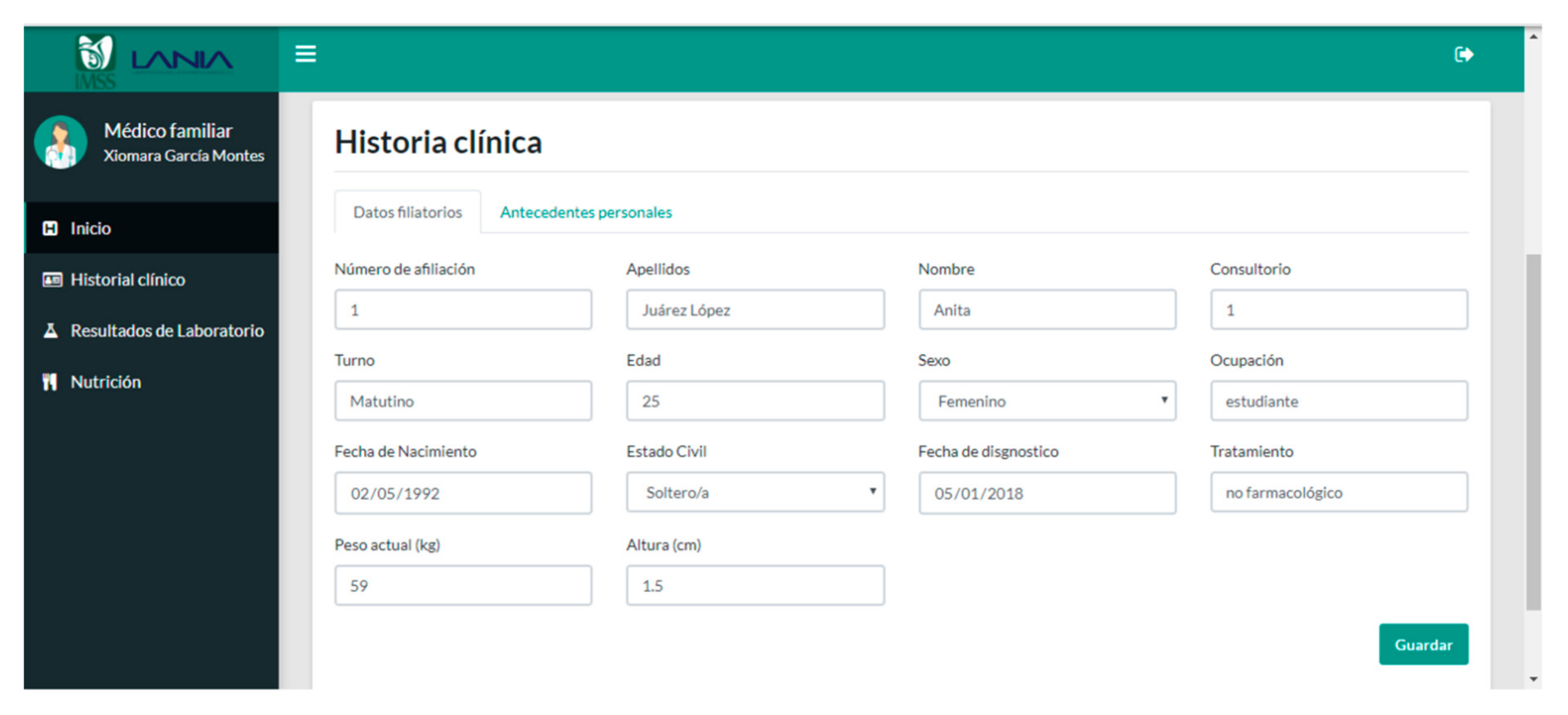
- Clinical history: This option is composed of two sections (see Figure 16). The first section shows the patient’s data, such as membership number, name, birth date, occupation, weight, height, age, marital status, date of diagnosis, and treatment. On the other hand, the second section is composed of personal history, which is divided into two groups: harmful habits and pathological personal background (see Figure 17). The option of harmful habits is recorded if the patient consumes alcohol, tobacco, or drugs. Concerning pathological personal background, chronic diseases, allergies, trauma, and surgical issues that the patient has suffered are recorded.
- Glucose results: In the glucose result sub-module, the physician can visualize the results that the patient enters from the patients′ application, with the details of the date, type of blood glucose test, and result. In this service, the physician can filter the results by periods of specific dates and types of blood glucose test (see Figure 18).
- Patient treatment progress: This sub-module shows to the physician the evolution of the patient’s glucose levels in graph format. The patient’s glucose levels are represented with a blue line, and the red lines represent the acceptable ranges of upper and lower glucose levels; the graph is consulted for a date period and the type of blood glucose test (preprandial and postprandial) (see Figure 19).
- Video report: The video report sub-module is proposed to report to the physician the videos that have been consulted by the patient through the patients′ application. This section shows a table with the name and status of the video; if the video is not in the table, it means that the patient has not seen it (Figure 20).
- Alert history: In this sub-module, the physician has a list of different alerts that the system reports based on the data entered by the patient. These alerts are generated when a patient records glucose levels outside the fixed acceptable range (see Figure 21). The physician can see the date on which the alert was generated, the type of blood glucose test, and the description.
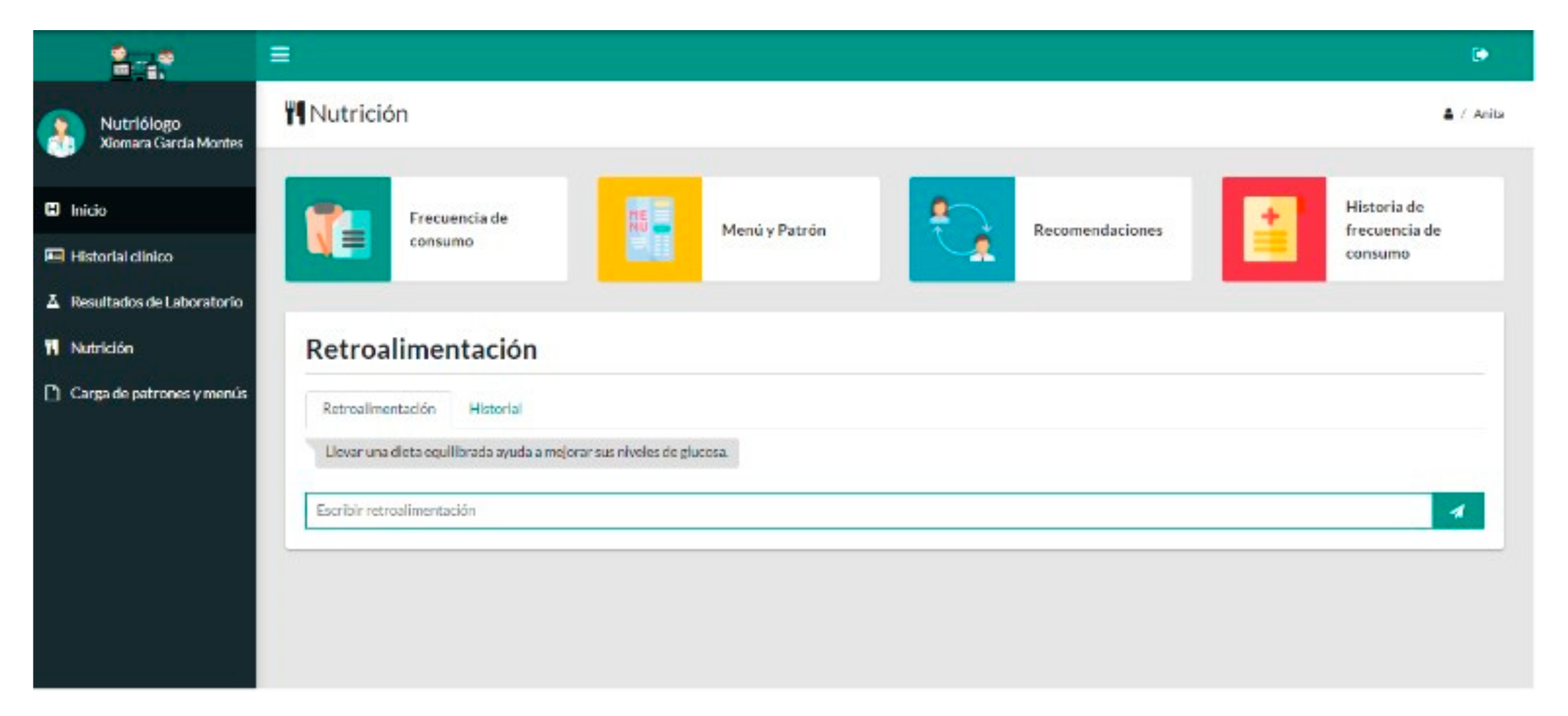
3.1.3. Nutritionist User Services
- Anthropometry: For the patient’s anthropometry record, the nutritionist first verifies or adjusts the current height and weight fields, and the system automatically calculates the ideal weight, overweight (additional body weight), body mass index, total calorie requirement, fiber intake, total caloric value (TCV), and adjusted weight (see Figure 28). This module assists the nutritionist in determining the eating plan to be assigned to the patient. This sub-module also provides a history of anthropometry records.
- Menu and eating pattern: In this service, the menu and eating pattern assigned to the patient is presented (see Figure 29). This section shows to the nutritionist and general physician the nutritional plan of the patient in order to provide information for adjustment or change of treatment of the patient.
- Recommendations: This sub-module provides a service that allows the nutritionist to make recommendations in real-time to the patient to adjust the progress of nutritional management (see Figure 30). This service allows the nutritionist to communicate with the patient continuously and remotely. It also provides a history of the recommendations sent to the patient. Based on the current monitoring and control process carried out for patients with T2DM, which aligns with the official Mexican standard NOM-015-SSA2-2018 [4], the physician must only make recommendations and/or modifications to pharmacological treatment of the patient in-person medical consultations through a medical prescription. Therefore, this functionality was not integrated into the physician’s services.
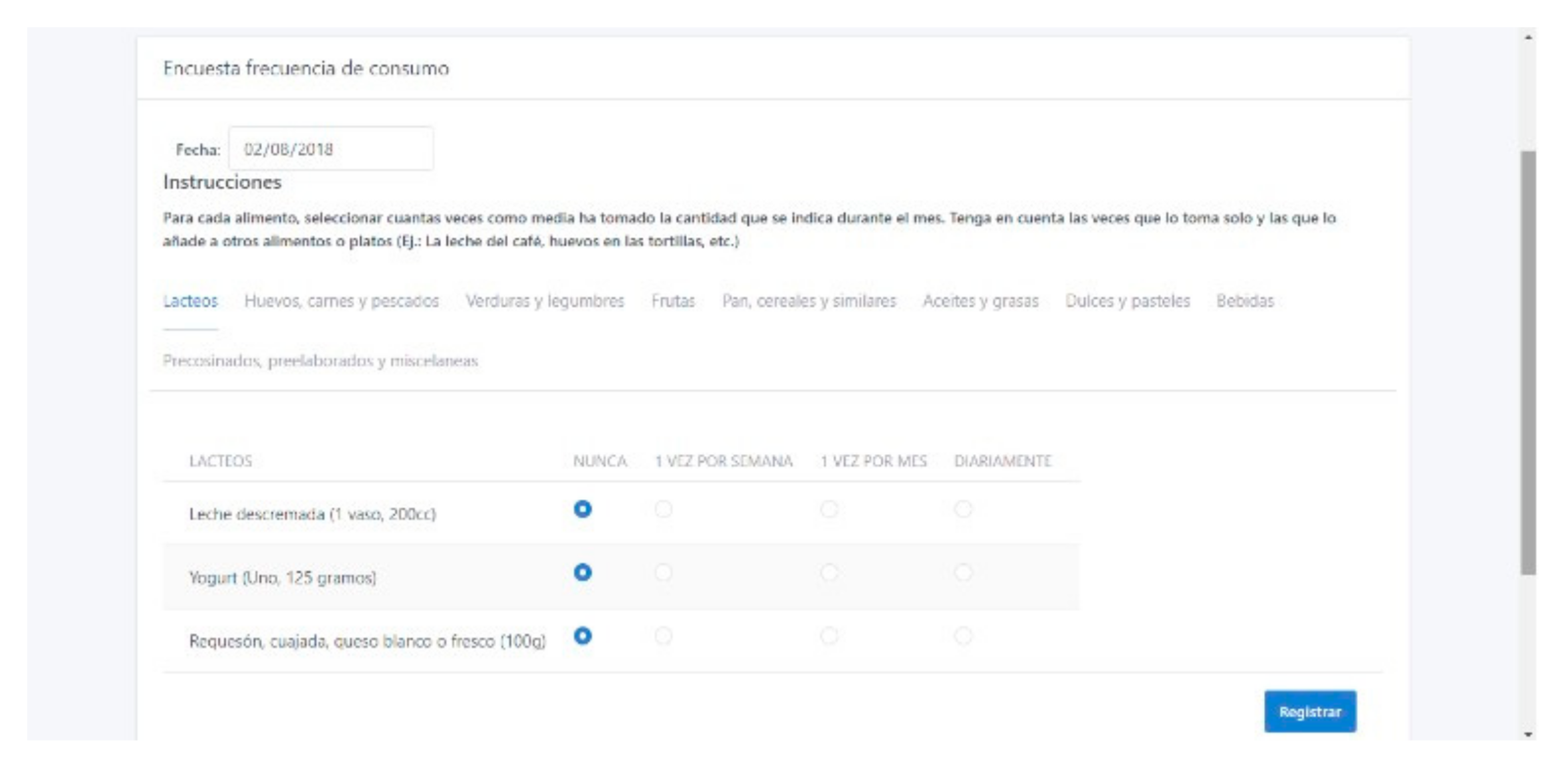
- History of intake frequency: This section is for the visualization of responses in the food intake frequency questionnaire that patients complete from their application (see Figure 31). This section helps the nutritionist observe foods frequently eaten by the patient to consider them in the elaboration of food menus assigned to the patient.
- Patterns: In this service, the nutritionist records and edits the eating patterns that are assigned to patients (see Figure 33).
3.2. Mobile-Web-Application Focused on the Patient
3.2.1. Glucose Record
3.2.2. Health Education Module
3.2.3. Laboratory Result Module
3.2.4. Nutrition Module
- Pattern: This service shows the patient a scheme for the distribution of rations by food groups assigned by the nutritionist. These eating patterns are previously registered by the nutritionist and are changing according to the indicated calories (see Figure 40). This scheme provides each food group’s list with the different foods and the suggested portions for consuming (see Figure 41).
- Menus: This service shows the patient, based on the calories established by the nutritionist, different food menu options so that the diet can be varied (see Figure 42).
- Food intake frequency questionnaire: In this sub-module, the patient answers the food intake frequency questionnaire to inform on food intake preferences (see Figure 43).
- Recommendations: This sub-module shows recommendations that the nutritionist sends to the patient; the information includes the date and the details of the recommendations. The patient can also search for the recommendations that the nutritionist sent in some range of dates (see Figure 44).
3.3. System Tests
4. Preliminary Usability Assessment of the Proposed System
4.1. Description of the Preliminary Usability Assessment of the System Based on a Field Study
- Instrument 1: List of tasks to measure effectiveness and efficiency.
- Instrument 2: User interface satisfaction questionnaire.
- Instrument 3: Questionnaire of product quality metrics to measure presentation, content, and navigation.
4.1.1. Field Study Description
4.1.2. Description of Usability Instruments
- Global reaction to the system: Includes questions to know the user’s perception regarding utility, flexibility, facility, among other aspects.
- Screen: Includes questions aimed at evaluating screen characteristics such as typography, design, distribution, and sequence.
- System terminology and information: Evaluates whether the terms applied help users to reach their goals and if there is consistency in the positioning and content of the messages.
- Learning: Collects information about user facility in learning to use the software.
- System capabilities: It allows identifying the performance and recovery capacity of the system before errors are caused by the user.
- Ease of use and user interface: Evaluates general aspects of the software interface design.
4.2. Description of the Usability Assessment of the System by Experts
4.2.1. Cognitive Walkthrough Method
- Description of system services to expert evaluators.
- List the tasks to be developed and create a list of actions for each task necessary to be completed by the evaluators.
- When performing each action, the evaluator examines the system by answering four questions:
- Will the user try and get the correct result?
- Will the user notice that the correct action is available to him/her?
- Does the user associate the correct action with the result he/she intends to achieve?
- If the correct action is executed, does the user observe that there is progress towards the objective he/she intends to achieve?
- The evaluator writes the answers for each action, discussing the results between them.
- A document is written with the answers and comments on the system.
- Through this method, errors or failures are detected and corrected within the system, specifically in performing tasks in each of the services for the three types of users.
4.2.2. Heuristic Usability Review Based on SIRIUS
- It can be applied to any website.
- It generates a percentage value of the level of usability of the evaluated site, therefore a quantitative data.
- It facilitates the detection of elements with a low degree of usability on the site, setting priorities.
- The evaluation classifies the websites according to their functionality.
- It provides a metric that allows measuring the degree of usability achieved in percentage.
4.3. Preliminary Usability Assessment Results
4.3.1. Results of the Preliminary Usability Assessment of the System Based on a Field Study
| 0 ≤ % effectiveness/efficiency ≤ 45: | Not satisfactory |
| 46 ≤ %effectiveness/efficiency ≤ 80: | Acceptable |
| 81 ≤ %effectiveness/efficiency ≤ 100: | Satisfactory |
| 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 |
| Not satisfactory | Acceptable | Satisfactory | |||||||
| Strongly Disagree | Disagree | Neutral | Agree | Strongly Agree |
| 1 | 2 | 3 | 4 | 5 |
4.3.2. Results of the Usability Assessment of the System by Experts
5. Discussion
- Registration of biomedical data by the patient (PR): Consultation and registration of different biomedical data relevant for monitoring and control of treatment
- Consultation of information by the physician (CD): Access to relevant patient information in real-time for the monitoring and control of patients with T2DM.
- Clinical history (CH): Record the patient’s medical history, which should include personal data of the patient and medical history.
- Alert generation (AG): Generation of alerts indicating that the patient is at some risk based on the biomedical parameters recorded.
- Laboratory analysis record (LR): The record of the results of the laboratory tests requested of the patient, such as blood chemistry test, complete blood count, general urine test, liver function test, and thyroid profile test.
- Nutrition (N): Have personalized nutritional menus and options for equivalent foods. This service brings the patient the benefit of knowing what foods and in what quantity they can substitute, in case of not having those established in the menu.
- Health education (HE): Help material is provided with topics related to diabetes, and the care that patients should have. In order to achieve the adoption of habits that help avoid health complications.
- Recommendations (R): The medical specialist and nutritionist can make suggestions to the patient for their health care.
- The system must show clear messages to users when an error occurs.
- Lack of contextual help to the user in some services of medical staff and patients.
- The system must show help messages to the user for entering some data.
6. Conclusions and Future Work
- To implement our system in a public or private health institution, we consider performing usability tests with patients and physicians during a year.
- Automatic calculation of proteins, carbohydrates, and fats that the patient consumes. This for the nutrition module as a complement to the intake frequency answer.
- A specialized module for physical activity orientation that allows the patient to perform some exercises in support of the treatment.
- Develop a system version integrated with native applications for Android and iOS mobile devices.
- Implement a sensor network to obtain medical data of the patients.
Author Contributions
Funding
Conflicts of Interest
References
- Saeedi, P.; Petersohn, I.; Salpea, P.; Malanda, B.; Karuranga, S.; Unwin, N.; Colagiuri, S.; Guariguata, L.; Motala, A.A.; Ogurtsova, K.; et al. Global and Regional Diabetes Prevalence Estimates for 2019 and Projections for 2030 and 2045: Results from the International Diabetes Federation Diabetes Atlas, 9th ed.; Diabetes Research and Clinical Practice: Amsterdam, The Netherlands, 2019; Volume 157, p. 107843. Available online: https://www.sciencedirect.com/science/article/pii/S0168822719312306 (accessed on 17 September 2020).
- Shamah-Levy, T.; Cuevas-Nasu, L.; Rivera-Dommarco, J.; Hernández-Ávila, M. Encuesta Nacional de Salud y Nutrición de Medio Camino. 2016. Available online: http://transparencia.insp.mx/2017/auditorias-insp/12701_Resultados_Encuesta_ENSANUT_MC2016.pdf (accessed on 17 September 2020).
- Oviedo Mota, M.A.; Espinosa Larrañaga, F.; Reyes Morales, H.; Trejo y Pérez, J.A.; Gil Velázquez, E. Guía clínica para el diagnóstico y tratamiento de la diabetes mellitus tipo 2. Rev. Med. IMSS 2003, 41, 27–46. Available online: https://www.medigraphic.com/pdfs/imss/im-2003/ims031d.pdf (accessed on 17 September 2020).
- DOF. NORMA Oficial Mexicana NOM-015-SSA2-2018, Para la Prevención, Detección, Diagnóstico, Tratamiento y Control de la Diabetes Mellitus. Obtained from Diario Oficial de la Federación. April 2018. Available online: https://www.dof.gob.mx/nota_detalle.php?codigo=5521405&fecha=03/05/2018 (accessed on 17 September 2020).
- Morales-Rocha, V.; Fernández-Martínez, L.; Rodas OSillo, J.; Olmos Sánchez, K. Monitoreo Remoto de Pacientes con Diabetes Utilizando Tecnologías Móviles Inalámbricas. RevistaeSalud.com 2012, 8, 2–7. Available online: https://www.academia.edu/20556350/Monitoreo_Remoto_de_Pacientes_con_Diabetes_Utilizando_Tecnolog%C3%ADas_M%C3%B3viles_Inal%C3%A1mbricas (accessed on 17 September 2020).
- Coll-Clavero, J.I.; Angles-Barbastro, R.A.; Sierra-Callau, M.; Clemente, E.T.; Leris Oliva, J.M.; Romero Marco, D.; Ibáñez Castellar, L.; Castillón Loscertales, A. PITES: Telemedicine and e-Health Innovation Platform; Instituto de Salud Carlos III—Ministerio de economía y competitividad: Madrid, Spain, 2014; Chapter 1; pp. 9–38. [Google Scholar]
- PALANTE, un Proyecto Europeo—Servicio Andaluz de Salud. Juntadeandalucia.es. 2017. Available online: http://www.juntadeandalucia.es/servicioandaluzdesalud/principal/documentosacc.asp?pagina=pr_palante_1 (accessed on 22 November 2017).
- Cytron Medical. VITADAT®. (Version 2.0.1) [Mobile application]. Available online: https://play.google.com/store/apps/details?id=com.cytronmedical.vitadatdietas&hl=es_MX (accessed on 20 September 2020).
- SquareMed Software GmbH. Diabetes Connect. (Version 2.4.1) [Mobile application]. Available online: https://play.google.com/store/apps/details?id=com.squaremed.diabetesconnect.android&hl=es_MX (accessed on 20 September 2020).
- Klimaszewski Szymon. Diabetes—Diario. (Version 4.1.5) [Mobile application]. Available online: https://play.google.com/store/apps/details?id=com.szyk.diabetes&hl=es (accessed on 20 September 2020).
- Sirma Medical Systems. Diabetes:M. (Version 7.3.0) [Mobile application]. Available online: https://play.google.com/store/apps/details?id=com.mydiabetes&hl=es (accessed on 20 September 2020).
- mHealthAlert. myDiabeticAlert. (Version 4.12.0) [Mobile application]. Available online: https://play.google.com/store/apps/details?id=com.cystelcom.attcr.mydiabeticalert&hl=es (accessed on 20 September 2020).
- ySugr GmbH. mySugr. (Version 3.62.3) [Mobile application]. Available online: https://play.google.com/store/apps/details?id=com.mysugr.android.companion&hl=es (accessed on 21 September 2020).
- Patrón Modelo Vista Controlador| Marco de Desarrollo de la Junta Andalucía. Available online: http://www.juntadeandalucia.es/servicios/madeja/contenido/recurso/122 (accessed on 15 October 2018).
- Torrente Suárez, M.C. SIRIUS: Sistema de Evaluación de la Usabilidad Web Orientado al Usuario y Basado en la Determinación de Tareas Críticas. 2011. Available online: http://di002.edv.uniovi.es/~cueva/investigacion/tesis/Sirius.pdf (accessed on 5 September 2020).
- ISO-International Organization for Standardization ISO 25000. 2014. Available online: https://iso25000.com/index.php/en/iso-25000-standards/iso-25010 (accessed on 17 September 2020).
- Chin, P.J.; Diel, V.A.; Norman, L.K. Questionnaire for User Interface Satisfaction (QUIS) version 7, Hp Repository. 2012. Available online: http://webprisme.cfmu.eurocontrol.int/ehp (accessed on 15 January 2019).
- Sierra, G.J.C. Metodología de Evaluación de Usabilidad para Sistemas de Información basados en Web. 2016. Available online: https://repositorio.unal.edu.co/bitstream/handle/unal/57766/juliocesarsierragonzalez.2016.pdf?sequence=1&isAllowed=y (accessed on 20 September 2020).
- Domínguez Zárate, R.F. Aplicación de Métricas de Calidad en uso Utilizando la ISO 9126 Para Determinar el Grado de Satisfacción del Sistema Único de Matrícula, Chapter 4. 2016. Available online: https://cybertesis.unmsm.edu.pe/handle/20.500.12672/6704 (accessed on 20 September 2020).
- Mañas, B.C. Comunicación en Salud: Efectividad de las Aplicaciones Móviles de Salud en la Diabetes; Facultad de Ciencias de la Comunicación, Universidad Autónoma de Barcelona: Barcelona, Spain, 2016. [Google Scholar]
- Muñoz, G.O. USKAYSMS: Desarrollo y Evaluación de la Usabilidad de una Aplicación Informática de Envío y Recepción de Mensajes de Texto Para la Comunicación Entre Profesionales de Salud del Primer Nivel y Pacientes. Master’s Thesis, Universidad Peruana Cayetano Heredia, Lima, Perú, 2018. [Google Scholar]
- Aguirre, R.B. Evaluación de sistema de monitoreo remoto de pacientes con diabetes utilizando una guía de usabilidad. Revista Culcyt Tecnología 2013, 51, 105–113. [Google Scholar]
- Nielsen, J. Why You Only Need to Test with 5 Users, NN/g Nielsen Norman Group. 2000. Available online: https://www.nngroup.com/articles/why-you-only-need-to-test-with-5-users/ (accessed on 14 October 2020).








































| Module | Name of the Tested Module | User | The User Role | Test | Test Identifier |
|---|---|---|---|---|---|
| Submodule | Name of the Tested Submodule/Service | ||||
| Purpose | Description of the service goal. | ||||
| Requirements | Previous steps for the service action | ||||
| Entry | Information occupied to perform the test. | ||||
| Action | Description of the service action | Result: Indicates if the service works correctly | |||
| Module | Sub-Module/Services | EF | ES | PE | I |
|---|---|---|---|---|---|
| Authentication | 0 | 0 | 0 | 3 | |
| Select patient | 0 | 0 | 0 | 3 | |
| Medical history | Personal data | 0 | 0 | 0 | 3 |
| Personal history | 0 | 0 | 0 | 3 | |
| Glucose results | 0 | 0 | 0 | 3 | |
| Patient progress | 0 | 0 | 0 | 3 | |
| Video report | 1 | 1 | 0 | 3 | |
| Alert History | 0 | 0 | 0 | 3 | |
| Laboratory results | Blood chemistry test | 1 | 1 | 0 | 3 |
| Complete blood count | 1 | 1 | 0 | 3 | |
| General urine test | 0 | 0 | 0 | 3 | |
| Liver function test | 0 | 0 | 0 | 3 | |
| Thyroid profile test | 1 | 1 | 0 | 3 | |
| Nutrition | Menu and pattern | 0 | 0 | 0 | 3 |
| Anthropometry, | 0 | 0 | 0 | 3 | |
| Record | 1 | 1 | 0 | 3 | |
| Recommendations | 0 | 0 | 0 | 3 | |
| Load patterns and menus | History of intake frequency | 0 | 0 | 0 | 3 |
| Pattern | 1 | 1 | 0 | 3 |
| Module | Sub-Module/Services | EF | ES | PE | I |
|---|---|---|---|---|---|
| Authentication | 0 | 0 | 0 | 3 | |
| Health Education | 0 | 0 | 0 | 3 | |
| Nutrition | Patterns | 0 | 0 | 0 | 3 |
| Menus | 0 | 0 | 0 | 3 | |
| Intake frequency questionnaire | 0 | 0 | 0 | 3 | |
| Feedback | 1 | 1 | 0 | 3 | |
| Glucose record | Record | 0 | 0 | 0 | 3 |
| History | 1 | 1 | 0 | 3 | |
| Laboratory results | Blood chemistry test | 1 | 1 | 0 | 3 |
| Complete blood count | 0 | 0 | 0 | 3 | |
| General urine test | 0 | 0 | 0 | 3 | |
| Liver function test | 0 | 0 | 0 | 3 | |
| Thyroid profile test | 1 | 1 | 0 | 3 |
| Type of User | Average Effectiveness Percentage | Average Efficiency Percentage |
|---|---|---|
| Physicians | 95.8% | 90.1% |
| Nutritionist | 94.1% | 83.0% |
| Patients | 92.4% | 63.4% |
| Position | Section | Average Score | Total Average Score |
|---|---|---|---|
| 1 | Screen | 8.75 | 8.28 |
| 2 | Terminology and Information | 8.54 | |
| 3 | System capabilities | 8.25 | |
| 4 | Learning capacity | 8.17 | |
| 5 | Usability and user interface | 8.15 | |
| 6 | General reactions | 7.83 |
| Position | Section | Average Score | Total Average Score |
|---|---|---|---|
| 1 | Terminology and Information | 8.42 | 7.56 |
| 2 | Screen | 8.25 | |
| 3 | System capabilities | 7.6 | |
| 4 | General reactions | 7.58 | |
| 5 | Usability and user interface | 6.8 | |
| 6 | Learning capacity | 6.75 |
| Position | Section | Average Score | Total Average Score |
|---|---|---|---|
| 1 | General reactions | 7.64 | 7.33 |
| 2 | Screen | 7.61 | |
| 3 | Terminology and Information | 7.5 | |
| 4 | Usability and user interface | 7.27 | |
| 5 | System capabilities | 7.2 | |
| 6 | Learning capacity | 6.76 |
| Position | Attribute | Average Score | Total Score |
|---|---|---|---|
| 1 | Presentation | 4.92 | 4.74 |
| 2 | Content | 4.67 | |
| 3 | Navigation | 4.64 |
| Position | Attribute | Average Score | Total Score |
|---|---|---|---|
| 1 | Content | 4.75 | 4.37 |
| 2 | Navigation | 4.21 | |
| 3 | Presentation | 4.17 |
| Position | Attribute | Average Score | Total Score |
|---|---|---|---|
| 1 | Presentation | 4.1 | 4.0 |
| 2 | Content | 4.0 | |
| 3 | Navigation | 3.9 |
| Evaluator | Percentages of Each Evaluated Profile | ||
|---|---|---|---|
| Physician | Nutritionist | Patient | |
| Evaluator 1 | 82.61% | 82.61% | 81.16% |
| Evaluator 2 | 85.90% | 85.90% | 85.07% |
| Evaluator 3 | 79.03% | 79.03% | 84.20% |
| Mean | 82.51% | 82.51% | 83.48% |
| Related Works | PR | CD | CH | AG | LR | N | R | H |
|---|---|---|---|---|---|---|---|---|
| MRPDUTMI [5] | ✓ | ✓ | ✓ | ✓ | ||||
| Proyecto PITES T-YUDA [6] | ✓ | ✓ | ✓ | |||||
| PALANTE [7] | ✓ | ✓ | ✓ | ✓ | ✓ | |||
| VITADAT [8] | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||
| Diabetes conect [9] | ✓ | |||||||
| Diabetes diario [10] | ✓ | ✓ | ||||||
| Diabetes M [11] | ✓ | ✓ | ✓ | |||||
| MyDiabeticAlert [12] | ✓ | ✓ | ✓ | ✓ | ||||
| MySugr [13] | ✓ | ✓ | ✓ | ✓ | ||||
| Social Diabetes [20] | ✓ | ✓ | ✓ | ✓ | ✓ | |||
| USKAYSMS [21] | ✓ | ✓ | ✓ | |||||
| S.M.R.P.D. [22] | ✓ | ✓ | ✓ | ✓ | ||||
| Our proposed | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Related Works | FS | US | HM | EM | IM | UE | EE | IAE |
|---|---|---|---|---|---|---|---|---|
| Social Diabetes [20] | ✓ | ✓ | ✓ | |||||
| USKAYSMS [21] | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||
| S.M.R.P.D. [22] | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alcala Juárez, A.; Hernández Villegas, M.A.; Domínguez, E.L.; Hernández Velázquez, Y.; Domínguez Isidro, S.; Ovando Diego, L.; Hernández Sánchez, O.; De La Calleja, J.; Pomares Hernández, S.E.; Medina Nieto, M.A. MobiDiabet: Mobile Telemonitoring System for Patients with Type 2 Diabetes Mellitus (T2DM). Appl. Sci. 2020, 10, 8036. https://doi.org/10.3390/app10228036
Alcala Juárez A, Hernández Villegas MA, Domínguez EL, Hernández Velázquez Y, Domínguez Isidro S, Ovando Diego L, Hernández Sánchez O, De La Calleja J, Pomares Hernández SE, Medina Nieto MA. MobiDiabet: Mobile Telemonitoring System for Patients with Type 2 Diabetes Mellitus (T2DM). Applied Sciences. 2020; 10(22):8036. https://doi.org/10.3390/app10228036
Chicago/Turabian StyleAlcala Juárez, Anakaren, Manuel Alejandro Hernández Villegas, Eduardo López Domínguez, Yesenia Hernández Velázquez, Saúl Domínguez Isidro, Liliana Ovando Diego, Olivia Hernández Sánchez, Jorge De La Calleja, Saúl Eduardo Pomares Hernández, and María Auxilio Medina Nieto. 2020. "MobiDiabet: Mobile Telemonitoring System for Patients with Type 2 Diabetes Mellitus (T2DM)" Applied Sciences 10, no. 22: 8036. https://doi.org/10.3390/app10228036
APA StyleAlcala Juárez, A., Hernández Villegas, M. A., Domínguez, E. L., Hernández Velázquez, Y., Domínguez Isidro, S., Ovando Diego, L., Hernández Sánchez, O., De La Calleja, J., Pomares Hernández, S. E., & Medina Nieto, M. A. (2020). MobiDiabet: Mobile Telemonitoring System for Patients with Type 2 Diabetes Mellitus (T2DM). Applied Sciences, 10(22), 8036. https://doi.org/10.3390/app10228036






