Numerical Investigation of the Effects of Prosthetic Aortic Valve Design on Aortic Hemodynamic Characteristics
Abstract
1. Introduction
2. Materials and Methods
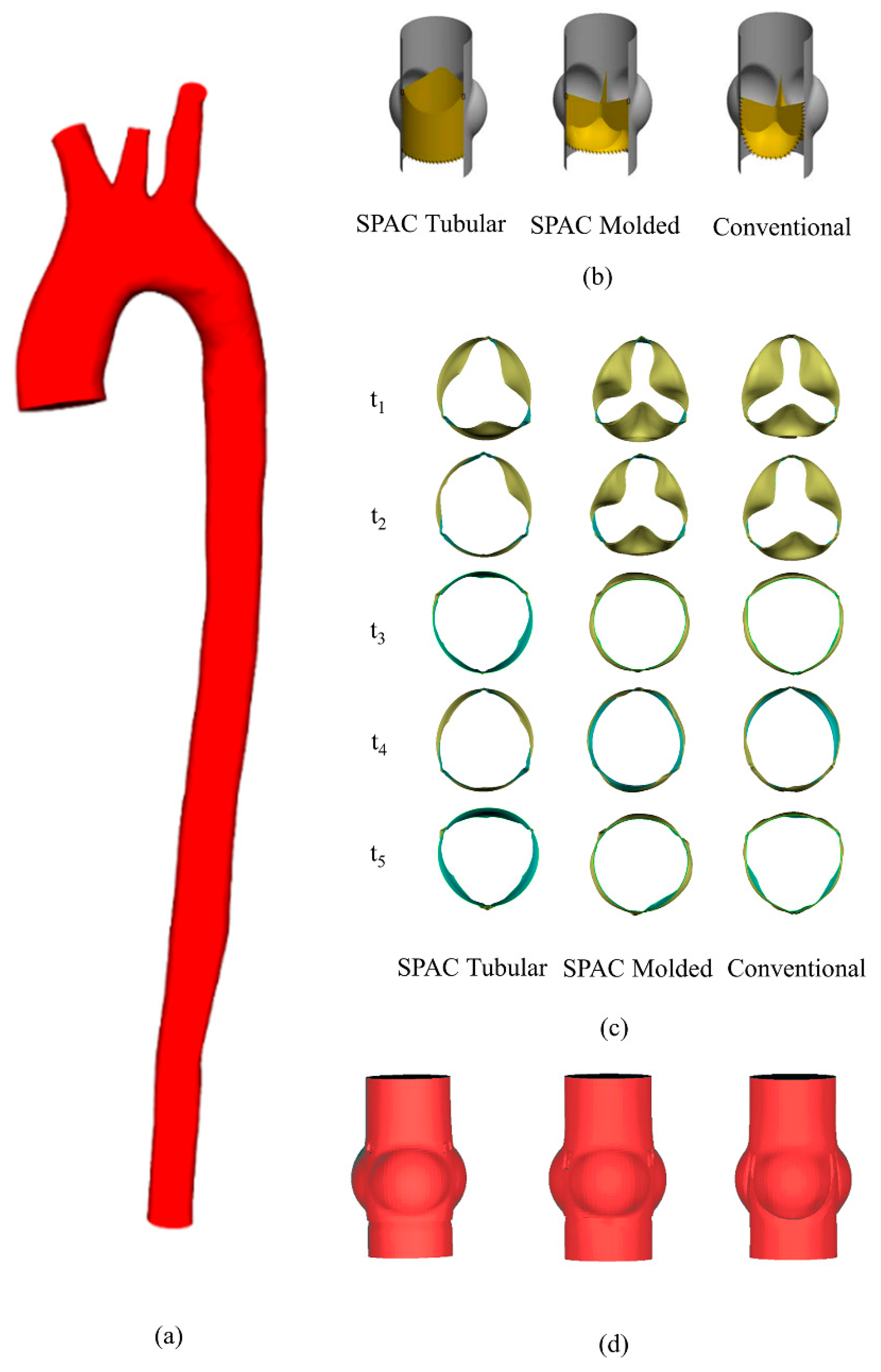
2.1. Geometric Modeling
2.1.1. Patient-Specific Aorta Model
2.1.2. Valve Geometry
2.2. Numerical Methods
2.3. Data Analysis
3. Results
3.1. The Impacts of Valve Designs on the Efferent Flow
3.2. The Impacts of Valve Designs on the Flow Pattern
3.3. The Impacts of Valve Designs on Hemodynamic Characteristics
3.3.1. Wall Shear Stress (WSS)
3.3.2. Secondary Flow
3.3.3. Q-Criterion
4. Discussion
4.1. Modeling Simplifications
4.2. Helical Flow
4.3. Secondary Flow
4.4. WSS Distribution
4.5. Vortex Distribution
4.6. Limitations and Future Works
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Timmis, A.; Townsend, N.; Gale, C.; Grobbee, R.; Maniadakis, N.; Flather, M.; Wilkins, E.; Wright, L.; Vos, R.; Bax, J.; et al. European Society of Cardiology: Cardiovascular Disease Statistics 2017. Eur. Heart J. 2018, 39, 508–579. [Google Scholar] [CrossRef]
- Søndergaard, L.; Saraste, A.; Christersson, C.; Vahanian, A. The year in cardiology 2017: Valvular heart disease. Eur. Heart J. 2018, 39, 650–657. [Google Scholar] [CrossRef]
- Climie, R.E.D.; Picone, D.S.; Blackwood, S.; Keel, S.E.; Qasem, A.; Rattigan, S.; Sharman, J.E. Pulsatile interaction between the macro-vasculature and micro-vasculature: Proof-of-concept among patients with type 2 diabetes. Eur. J. Appl. Physiol. 2018, 118, 2455–2463. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez-Gabella, T.; Voisine, P.; Puri, R.; Pibarot, P.; Rodés-Cabau, J. Aortic Bioprosthetic Valve Durability. J. Am. Coll. Cardiol. 2017, 70, 1013–1028. [Google Scholar] [CrossRef] [PubMed]
- Choi, C.H.; Cheng, V.; Malaver, D.; Kon, N.; Kincaid, E.H.; Gandhi, S.K.; Applegate, R.J.; Zhao, D.X.M. A comparison of valve-in-valve transcatheter aortic valve replacement in failed stentless versus stented surgical bioprosthetic aortic valves. Catheter. Cardiovasc. Interv. 2019, 93, 1106–1115. [Google Scholar] [CrossRef]
- Capelli, C.; Corsini, C.; Biscarini, D.; Ruffini, F.; Migliavacca, F.; Kocher, A.; Laufer, G.; Taylor, A.M.; Schievano, S.; Andreas, M.; et al. Pledget-Armed Sutures Affect the Haemodynamic Performance of Biologic Aortic Valve Substitutes: A Preliminary Experimental and Computational Study. Cardiovasc. Eng. Technol. 2017, 8, 17–29. [Google Scholar] [CrossRef] [PubMed]
- O’Brien, M.F. The cryolife-O’Brien composite aortic stentless xenograft: Surgical technique of implantation. Ann. Thorac. Surg. 1995, 60, S410–S413. [Google Scholar] [CrossRef]
- Doss, M.; Martens, S.; Wood, J.P.; Miskovic, A.; Christodoulou, T.; Wimmer-Greinecker, G.; Moritz, A. Aortic Leaflet Replacement With the New 3F Stentless Aortic Bioprosthesis. Ann. Thorac. Surg. 2005, 79, 682–685. [Google Scholar] [CrossRef] [PubMed]
- Cox, J.L.; Ad, N.; Myers, K.; Gharib, M.; Quijano, R.C. Tubular heart valves: A new tissue prosthesis design—Preclinical evaluation of the 3F aortic bioprosthesis. J. Thorac. Cardiovasc. Surg. 2005, 130, 520–527. [Google Scholar] [CrossRef]
- Goetz, W.A.; Tan, T.E.; Lim, K.H.; Salgues, S.L.H.; Grousson, N.; Xiong, F.L.; Chua, Y.L.; Yeo, J.H.; Ee, T.; Hiang, K.; et al. Truly stentless molded autologous pericardial aortic valve prosthesis with single point attached commissures in a sheep model. Eur. J. Cardio Thorac. Surg. 2008, 33, 548–553. [Google Scholar] [CrossRef][Green Version]
- Duran, C.M.G.; Gallo, R.; Kumar, N. Aortic Valve Replacement with Autologous Pericardium: Surgical Technique. J. Card. Surg. 1995, 10, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Xiong, F.L.; Goetz, W.A.; Chong, C.K.; Chua, Y.L.; Pfeifer, S.; Wintermantel, E.; Yeo, J.H. Finite element investigation of stentless pericardial aortic valves: Relevance of leaflet geometry. Ann. Biomed. Eng. 2010, 38, 1908–1918. [Google Scholar] [CrossRef] [PubMed]
- Goetz, W.A.; Lim, K.H.; Ibled, R.; Grousson, N.; Salgues, S.L.H.; Yeo, J.H. Forces at single point attached commissures (SPAC) in pericardial aortic valve prosthesis. Eur. J. Cardiothorac. Surg. 2006, 29, 150–155. [Google Scholar] [CrossRef] [PubMed]
- Morbiducci, U.; Ponzini, R.; Rizzo, G.; Cadioli, M.; Esposito, A.; De Cobelli, F.; Del Maschio, A.; Montevecchi, F.M.; Redaelli, A. In Vivo Quantification of Helical Blood Flow in Human Aorta by Time-Resolved Three-Dimensional Cine Phase Contrast Magnetic Resonance Imaging. Ann. Biomed. Eng. 2009, 37, 516–531. [Google Scholar] [CrossRef]
- Morbiducci, U.; Ponzini, R.; Rizzo, G.; Cadioli, M.; Esposito, A.; Montevecchi, F.M.; Redaelli, A. Mechanistic insight into the physiological relevance of helical blood flow in the human aorta: An in vivo study. Biomech. Model. Mechanobiol. 2011, 10, 339–355. [Google Scholar] [CrossRef]
- Liu, X.; Sun, A.; Fan, Y.; Deng, X. Physiological Significance of Helical Flow in the Arterial System and its Potential Clinical Applications. Ann. Biomed. Eng. 2014, 43, 3–15. [Google Scholar] [CrossRef]
- Morbiducci, U.; Gallo, D.; Cristofanelli, S.; Ponzini, R.; Deriu, M.A.; Rizzo, G.; Steinman, D.A. A rational approach to defining principal axes of multidirectional wall shear stress in realistic vascular geometries, with application to the study of the influence of helical flow on wall shear stress directionality in aorta. J. Biomech. 2015, 48, 899–906. [Google Scholar] [CrossRef]
- De Nisco, G.; Kok, A.M.; Chiastra, C.; Gallo, D.; Hoogendoorn, A.; Migliavacca, F.; Wentzel, J.J.; Morbiducci, U. The Atheroprotective Nature of Helical Flow in Coronary Arteries. Ann. Biomed. Eng. 2019, 47, 425–438. [Google Scholar] [CrossRef]
- Barker, A.J.; Markl, M.; Bürk, J.; Lorenz, R.; Bock, J.; Bauer, S.; Schulz-Menger, J.; von Knobelsdorff-Brenkenhoff, F. Bicuspid Aortic Valve Is Associated With Altered Wall Shear Stress in the Ascending Aorta. Circ. Cardiovasc. Imaging 2012, 5, 457–466. [Google Scholar] [CrossRef]
- Barker, A.J.; Lanning, C.; Shandas, R. Quantification of Hemodynamic Wall Shear Stress in Patients with Bicuspid Aortic Valve Using Phase-Contrast MRI. Ann. Biomed. Eng. 2010, 38, 788–800. [Google Scholar] [CrossRef]
- Cheng, Z.; Kidher, E.; Jarral, O.A.; O’Regan, D.P.; Wood, N.B.; Athanasiou, T.; Xu, X.Y. Assessment of Hemodynamic Conditions in the Aorta Following Root Replacement with Composite Valve-Conduit Graft. Ann. Biomed. Eng. 2016, 44, 1392–1404. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Trauzeddel, R.F.; Löbe, U.; Barker, A.J.; Gelsinger, C.; Butter, C.; Markl, M.; Schulz-Menger, J.; von Knobelsdorff-Brenkenhoff, F. Blood flow characteristics in the ascending aorta after TAVI compared to surgical aortic valve replacement. Int. J. Cardiovasc. Imaging 2016, 32, 461–467. [Google Scholar] [CrossRef] [PubMed]
- Saikrishnan, N.; Mirabella, L.; Yoganathan, A.P. Bicuspid aortic valves are associated with increased wall and turbulence shear stress levels compared to trileaflet aortic valves. Biomech. Model. Mechanobiol. 2015, 14, 577–588. [Google Scholar] [CrossRef] [PubMed]
- Youssefi, P.; Gomez, A.; He, T.; Anderson, L.; Bunce, N.; Sharma, R.; Figueroa, C.A.; Jahangiri, M. Patient-specific computational fluid dynamics—Assessment of aortic hemodynamics in a spectrum of aortic valve pathologies. J. Thorac. Cardiovasc. Surg. 2017, 153, 8–20. [Google Scholar] [CrossRef] [PubMed]
- Hedayat, M.; Asgharzadeh, H.; Borazjani, I. Platelet activation of mechanical versus bioprosthetic heart valves during systole. J. Biomech. 2017, 56, 111–116. [Google Scholar] [CrossRef]
- Khalili, F.; Gamage, P.; Sandler, R.; Mansy, H. Adverse Hemodynamic Conditions Associated with Mechanical Heart Valve Leaflet Immobility. Bioengineering 2018, 5, 74. [Google Scholar] [CrossRef]
- Thubrikar, M. The Aortic Valve; Routledge: Abingdon-on-Thames, UK, 2018; ISBN 9780203737163. [Google Scholar]
- Updegrove, A.; Wilson, N.M.; Merkow, J.; Lan, H.; Marsden, A.L.; Shadden, S.C. SimVascular: An Open Source Pipeline for Cardiovascular Simulation. Ann. Biomed. Eng. 2017, 45, 525–541. [Google Scholar] [CrossRef]
- Ni, M.W.; Prather, R.O.; Rodriguez, G.; Quinn, R.; Divo, E.; Fogel, M.; Kassab, A.J.; DeCampli, W.M. Computational Investigation of a Self-Powered Fontan Circulation. Cardiovasc. Eng. Technol. 2018, 9, 202–216. [Google Scholar] [CrossRef]
- Ceballos, A.; Prather, R.; Divo, E.; Kassab, A.J.; DeCampli, W.M. Patient-Specific Multi-Scale Model Analysis of Hemodynamics Following the Hybrid Norwood Procedure for Hypoplastic Left Heart Syndrome: Effects of Reverse Blalock–Taussig Shunt Diameter. Cardiovasc. Eng. Technol. 2019, 10, 136–154. [Google Scholar] [CrossRef]
- Vignon-Clementel, I.I.E.; Alberto Figueroa, C.; Jansen, K.E.; Taylor, C.A. Outflow boundary conditions for three-dimensional finite element modeling of blood flow and pressure in arteries. Comput. Methods 2006, 195, 3776–3796. [Google Scholar] [CrossRef]
- Keller, E.J.; Malaisrie, S.C.; Kruse, J.; McCarthy, P.M.; Carr, J.C.; Markl, M.; Barker, A.J.; Collins, J.D. Reduction of aberrant aortic haemodynamics following aortic root replacement with a mechanical valved conduit†. Interact. Cardiovasc. Thorac. Surg. 2016, 23, 416–423. [Google Scholar] [CrossRef] [PubMed]
- Ravensbergen, J.; Krijger, J.K.B.; Hillen, B.; Hoogstraten, H.W. The influence of the angle of confluence on the flow in a vertebro-basilar junction model. J. Biomech. 1996, 29, 281–299. [Google Scholar] [CrossRef]
- Zhang, Z.; Che, X.; Nie, W.; Li, J.; Zheng, T.; Li, L.; Chen, Q.; Zheng, Z. Study of vortex in flow fields induced by surface dielectric barrier discharge actuator at low pressure based on Q criterion. Plasma Sci. Technol. 2018, 20, 14006. [Google Scholar] [CrossRef]
- Qin, W.D.; Zhang, F.; Qin, X.J.; Wang, J.; Meng, X.; Wang, H.; Guo, H.P.; Wu, Q.Z.; Wu, D.W.; Zhang, M.X. Notch1 inhibition reduces low shear stress-induced plaque formation. Int. J. Biochem. Cell Biol. 2016, 72, 63–72. [Google Scholar] [CrossRef]
- Goetz, W.A.; Tan, T.E.; Lim, K.H.; Xiong, F.L.; Salgues, S.L.H.; Grousson, N.; Chua, Y.L.; Yeo, J.H. Autologous pericardial pulmonary conduit with single point attached commissures in a sheep model. Eur. J. Cardio Thorac. Surg. 2008, 33, 48–52. [Google Scholar] [CrossRef][Green Version]
- Gilmanov, A.; Stolarski, H.; Sotiropoulos, F. Flow–Structure Interaction Simulations of the Aortic Heart Valve at Physiologic Conditions: The Role of Tissue Constitutive Model. J. Biomech. Eng. 2018, 140, 1–9. [Google Scholar] [CrossRef]
- Luraghi, G.; Migliavacca, F.; Rodriguez Matas, J.F. Study on the Accuracy of Structural and FSI Heart Valves Simulations. Cardiovasc. Eng. Technol. 2018, 9, 723–738. [Google Scholar] [CrossRef]
- Mao, W.; Caballero, A.; McKay, R.; Primiano, C.; Sun, W. Fully-coupled fluid-structure interaction simulation of the aortic and mitral valves in a realistic 3D left ventricle model. PLoS ONE 2017, 12, 1–21. [Google Scholar] [CrossRef]
- Hsu, M.C.; Kamensky, D.; Xu, F.; Kiendl, J.; Wang, C.; Wu, M.C.H.; Mineroff, J.; Reali, A.; Bazilevs, Y.; Sacks, M.S. Dynamic and fluid? structure interaction simulations of bioprosthetic heart valves using parametric design with T-splines and Fung-type material models. Comput. Mech. 2015, 55, 1211–1225. [Google Scholar] [CrossRef]
- Morsi, Y.S.; Yang, W.W.; Wong, C.S.; Das, S. Transient fluid–structure coupling for simulation of a trileaflet heart valve using weak coupling. J. Artif. Organs 2007, 10, 96–103. [Google Scholar] [CrossRef]
- Luraghi, G.; Migliavacca, F.; García-González, A.; Chiastra, C.; Rossi, A.; Cao, D.; Stefanini, G.; Rodriguez Matas, J.F. On the Modeling of Patient-Specific Transcatheter Aortic Valve Replacement: A Fluid–Structure Interaction Approach. Cardiovasc. Eng. Technol. 2019, 10, 437–455. [Google Scholar] [CrossRef] [PubMed]
- Vy, P.; Auffret, V.; Badel, P.; Rochette, M.; Le Breton, H.; Haigron, P.; Avril, S. Review of patient-specific simulations of transcatheter aortic valve implantation. Int. J. Adv. Eng. Sci. Appl. Math. 2016, 8, 2–24. [Google Scholar] [CrossRef]
- Chen, Y.; Luo, H. A computational study of the three-dimensional fluid–structure interaction of aortic valve. J. Fluids Struct. 2018, 80, 332–349. [Google Scholar] [CrossRef]
- De Hart, J.; Peters, G.W.M.; Schreurs, P.J.G.; Baaijens, F.P.T. A three-dimensional computational analysis of fluid–structure interaction in the aortic valve. J. Biomech. 2003, 36, 103–112. [Google Scholar] [CrossRef]
- Nicosia, M.A.; Cochran, R.P.; Einstein, D.R.; Rutland, C.J.; Kunzelman, K.S. A coupled fluid-structure finite element model of the aortic valve and root. J. Heart Valve Dis. 2003, 12, 781–789. [Google Scholar] [PubMed]
- Le, T.B.; Sotiropoulos, F. Fluid–structure interaction of an aortic heart valve prosthesis driven by an animated anatomic left ventricle. J. Comput. Phys. 2013, 244, 41–62. [Google Scholar] [CrossRef] [PubMed]
- Spühler, J.H.; Jansson, J.; Jansson, N.; Hoffman, J. 3D Fluid-Structure Interaction Simulation of Aortic Valves Using a Unified Continuum ALE FEM Model. Front. Physiol. 2018, 9, 363. [Google Scholar] [CrossRef]
- Luraghi, G.; Wu, W.; De Gaetano, F.; Rodriguez Matas, J.F.; Moggridge, G.D.; Serrani, M.; Stasiak, J.; Costantino, M.L.; Migliavacca, F. Evaluation of an aortic valve prosthesis: Fluid-structure interaction or structural simulation? J. Biomech. 2017, 58, 45–51. [Google Scholar] [CrossRef]
- Chandran, K.B. Role of Computational Simulations in Heart Valve Dynamics and Design of Valvular Prostheses. Cardiovasc. Eng. Technol. 2010, 1, 18–38. [Google Scholar] [CrossRef]
- Votta, E.; Le, T.B.; Stevanella, M.; Fusini, L.; Caiani, E.G.; Redaelli, A.; Sotiropoulos, F. Toward patient-specific simulations of cardiac valves: State-of-the-art and future directions. J. Biomech. 2013, 46, 217–228. [Google Scholar] [CrossRef]
- Wu, W.; Pott, D.; Mazza, B.; Sironi, T.; Dordoni, E.; Chiastra, C.; Petrini, L.; Pennati, G.; Dubini, G.; Steinseifer, U.; et al. Fluid–Structure Interaction Model of a Percutaneous Aortic Valve: Comparison with an In Vitro Test and Feasibility Study in a Patient-Specific Case. Ann. Biomed. Eng. 2016, 44, 590–603. [Google Scholar] [CrossRef] [PubMed]
- Lavon, K.; Halevi, R.; Marom, G.; Ben Zekry, S.; Hamdan, A.; Joachim Schäfers, H.; Raanani, E.; Haj-Ali, R. Fluid–Structure Interaction Models of Bicuspid Aortic Valves: The Effects of Nonfused Cusp Angles. J. Biomech. Eng. 2018, 140, 031010. [Google Scholar] [CrossRef]
- Kamensky, D.M. Immersogeometric Fluid—Structure Interaction Analysis of Bioprosthetic Heart Valves. Doctoral Thesis, The University of Texas at Austin, Austin, TX, USA, 2016. [Google Scholar]
- Mao, W.; Li, K.; Sun, W. Fluid–Structure Interaction Study of Transcatheter Aortic Valve Dynamics Using Smoothed Particle Hydrodynamics. Cardiovasc. Eng. Technol. 2016, 7, 374–388. [Google Scholar] [CrossRef]
- Bahraseman, H.G.; Languri, E.M.; Yahyapourjalaly, N.; Espino, D.M. Fluid structure interaction modeling of aortic valve stenosis at different heart rates. Acta Bioeng. Biomech. 2016, 18, 11–20. [Google Scholar] [PubMed]
- Su, B.; Zhong, L.; Wang, X.-K.; Zhang, J.-M.; Tan, R.S.; Allen, J.C.; Tan, S.K.; Kim, S.; Leo, H.L. Numerical simulation of patient-specific left ventricular model with both mitral and aortic valves by FSI approach. Comput. Methods Programs Biomed. 2014, 113, 474–482. [Google Scholar] [CrossRef] [PubMed]
- Ghosh, R.P.; Marom, G.; Rotman, O.M.; Slepian, M.J.; Prabhakar, S.; Horner, M.; Bluestein, D. Comparative Fluid–Structure Interaction Analysis of Polymeric Transcatheter and Surgical Aortic Valves’ Hemodynamics and Structural Mechanics. J. Biomech. Eng. 2018, 140, 121002. [Google Scholar] [CrossRef]
- Hughes, T.J.R.; Liu, W.K.; Zimmermann, T.K. Lagrangian-Eulerian finite element formulation for incompressible viscous flows. Comput. Methods Appl. Mech. Eng. 1981, 29, 329–349. [Google Scholar] [CrossRef]
- Peskin, C.S. Flow patterns around heart valves: A numerical method. J. Comput. Phys. 1972, 10, 252–271. [Google Scholar] [CrossRef]
- Monaghan, J.J. Smoothed Particle Hydrodynamics and Its Diverse Applications. Annu. Rev. Fluid Mech. 2012, 44, 323–346. [Google Scholar] [CrossRef]
- Brown, A.G.; Shi, Y.; Marzo, A.; Staicu, C.; Valverde, I.; Beerbaum, P.; Lawford, P.V.; Hose, D.R. Accuracy vs. computational time: Translating aortic simulations to the clinic. J. Biomech. 2012, 45, 516–523. [Google Scholar] [CrossRef]
- Chen, H.Y.; Kassab, G.S. Computational Modeling in Biomechanics; Springer: Dordrecht, The Netherlands, 2010; pp. 207–220. [Google Scholar]
- Borazjani, I. Fluid–structure interaction, immersed boundary-finite element method simulations of bio-prosthetic heart valves. Comput. Methods Appl. Mech. Eng. 2013, 257, 103–116. [Google Scholar] [CrossRef]
- Hoeijmakers, M.J.M.M.; Silva Soto, D.A.; Waechter-Stehle, I.; Kasztelnik, M.; Weese, J.; Hose, D.R.; de Vosse, F.N. van Estimation of valvular resistance of segmented aortic valves using computational fluid dynamics. J. Biomech. 2019, 94, 49–58. [Google Scholar] [CrossRef] [PubMed]
- Vu, H.-H.; Hsu, C.-H. Quasi-Steady Flow Dynamics Study of Human Aortic Valve with Numerical Techniques. J. Mech. 2012, 28, 637–646. [Google Scholar] [CrossRef]
- Vincent, P.E.; Plata, A.M.; Hunt, A.A.E.; Weinberg, P.D.; Sherwin, S.J. Blood flow in the rabbit aortic arch and descending thoracic aorta. J. R. Soc. Interface 2011, 8, 1708–1719. [Google Scholar] [CrossRef] [PubMed]
- De Nisco, G.; Zhang, P.; Gallo, D.; Liu, X.; Deng, X.; Ponzini, R.; Rizzo, G.; Morbiducci, U. On the Impact of Modeling Assumptions in Subject-Specific Hemodynamic Simulations of Low-Density Lipoproteins Transport in Aorta. In Proceedings of the GNB2016, Naples, Italy, 20–22 June 2016. [Google Scholar]
- Ge, L.; Leo, H.-L.; Sotiropoulos, F.; Yoganathan, A.P. Flow in a mechanical bileaflet heart valve at laminar and near-peak systole flow rates: CFD simulations and experiments. J. Biomech. Eng. 2005, 127, 782–797. [Google Scholar] [CrossRef] [PubMed]
- Smadi, O.; Fenech, M.; Hassan, I.; Kadem, L. Flow through a defective mechanical heart valve: A steady flow analysis. Med. Eng. Phys. 2009, 31, 295–305. [Google Scholar] [CrossRef]
- Caballero, A.D.; Laín, S. A Review on Computational Fluid Dynamics Modelling in Human Thoracic Aorta. Cardiovasc. Eng. Technol. 2013, 4, 103–130. [Google Scholar] [CrossRef]
- Bruening, J.; Hellmeier, F.; Yevtushenko, P.; Kelm, M.; Nordmeyer, S.; Sündermann, S.H.; Kuehne, T.; Goubergrits, L. Impact of patient-specific LVOT inflow profiles on aortic valve prosthesis and ascending aorta hemodynamics. J. Comput. Sci. 2018, 24, 91–100. [Google Scholar] [CrossRef]
- Ku, D.N.; Giddens, D.P.; Zarins, C.K.; Glagov, S. Pulsatile flow and atherosclerosis in the human carotid bifurcation. Positive correlation between plaque location and low oscillating shear stress. Arter. Thromb. Vasc. Biol. 1985, 5, 293–302. [Google Scholar] [CrossRef]
- Hillen, B.; Drinkenburg, A.; Hoogstraten, H. Analysis of flow and vascular resistance in a model of the circle of Willis. J. Biomech. 1988, 21, 807–814. [Google Scholar] [CrossRef]
- Kobayashi, N.; Karino, T. Flow patterns and velocity distributions in the human vertebrobasilar arterial system. Laboratory investigation. J. Neurosurg. 2010, 113, 810–819. [Google Scholar] [CrossRef]
- Chen, L. Hemodynamics in the Cerebral Circulation: Numerical Studies and Experimetal Investigation. Doctoral Thesis, Nanyang Technological University, Singapore, 2005. [Google Scholar]
- Fahy, P.; McCarthy, P.; Sultan, S.; Hynes, N.; Delassus, P.; Morris, L. An experimental investigation of the hemodynamic variations due to aplastic vessels within three-dimensional phantom models of the circle of Willis. Ann. Biomed. Eng. 2014, 42, 123–138. [Google Scholar] [CrossRef]
- Caballero, A.D.; Laín, S. Numerical simulation of non-Newtonian blood flow dynamics in human thoracic aorta. Comput. Methods Biomech. Biomed. Eng. 2015, 18, 1200–1216. [Google Scholar] [CrossRef] [PubMed]
- Benim, A.C.; Nahavandi, A.; Assmann, A.; Schubert, D.; Feindt, P.; Suh, S.H. Simulation of blood flow in human aorta with emphasis on outlet boundary conditions. Appl. Math. Model. 2011, 35, 3175–3188. [Google Scholar] [CrossRef]
- Morbiducci, U.; Ponzini, R.; Gallo, D.; Bignardi, C.; Rizzo, G. Inflow boundary conditions for image-based computational hemodynamics: Impact of idealized versus measured velocity profiles in the human aorta. J. Biomech. 2013, 46, 102–109. [Google Scholar] [CrossRef] [PubMed]
- Youssefi, P.; Gomez, A.; Arthurs, C.; Sharma, R.; Jahangiri, M.; Alberto Figueroa, C. Impact of Patient-Specific Inflow Velocity Profile on Hemodynamics of the Thoracic Aorta. J. Biomech. Eng. 2018, 140. [Google Scholar] [CrossRef] [PubMed]
- Gallo, D.; De Santis, G.; Negri, F.; Tresoldi, D.; Ponzini, R.; Massai, D.; Deriu, M.A.; Segers, P.; Verhegghe, B.; Rizzo, G.; et al. On the Use of In Vivo Measured Flow Rates as Boundary Conditions for Image-Based Hemodynamic Models of the Human Aorta: Implications for Indicators of Abnormal Flow. Ann. Biomed. Eng. 2011, 40, 729–741. [Google Scholar] [CrossRef] [PubMed]
- Mohammadi, H.; Cartier, R.; Mongrain, R. The impact of the aortic valve impairment on the distant coronary arteries hemodynamics: A fluid–structure interaction study. Med. Biol. Eng. Comput. 2017, 55, 1859–1872. [Google Scholar] [CrossRef]
- Singh, S.D.; Xu, X.Y.; Wood, N.B.; Pepper, J.R.; Izgi, C.; Treasure, T.; Mohiaddin, R.H. Aortic flow patterns before and after personalised external aortic root support implantation in Marfan patients. J. Biomech. 2016, 49, 100–111. [Google Scholar] [CrossRef]
- Pirola, S.; Jarral, O.A.; O’Regan, D.P.; Asimakopoulos, G.; Anderson, J.R.; Pepper, J.R.; Athanasiou, T.; Xu, X.Y. Computational study of aortic hemodynamics for patients with an abnormal aortic valve: The importance of secondary flow at the ascending aorta inlet. APL Bioeng. 2018, 2, 026101. [Google Scholar] [CrossRef]
- Stijnen, J.M.A.; de Hart, J.; Bovendeerd, P.H.M.; van de Vosse, F.N. Evaluation of a fictitious domain method for predicting dynamic response of mechanical heart valves. J. Fluids Struct. 2004, 19, 835–850. [Google Scholar] [CrossRef]
- Wei, Z.A.; Sonntag, S.J.; Toma, M.; Singh-Gryzbon, S.; Sun, W. Computational Fluid Dynamics Assessment Associated with Transcatheter Heart Valve Prostheses: A Position Paper of the ISO Working Group. Cardiovasc. Eng. Technol. 2018, 9, 289–299. [Google Scholar] [CrossRef]
- Markl, M.; Draney, M.T.; Miller, D.C.; Levin, J.M.; Williamson, E.E.; Pelc, N.J.; Liang, D.H.; Herfkens, R.J. Time-resolved three-dimensional magnetic resonance velocity mapping of aortic flow in healthy volunteers and patients after valve-sparing aortic root replacement. J. Thorac. Cardiovasc. Surg. 2005, 130, 456–463. [Google Scholar] [CrossRef]
- Hope, T.A.; Markl, M.; Wigström, L.; Alley, M.T.; Miller, D.C.; Herfkens, R.J. Comparison of flow patterns in ascending aortic aneurysms and volunteers using four-dimensional magnetic resonance velocity mapping. J. Magn. Reson. Imaging 2007, 26, 1471–1479. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Fan, Y.; Deng, X.; Zhan, F. Effect of non-Newtonian and pulsatile blood flow on mass transport in the human aorta. J. Biomech. 2011, 44, 1123–1131. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Pu, F.; Fan, Y.; Deng, X.; Li, D.; Li, S. A numerical study on the flow of blood and the transport of LDL in the human aorta: The physiological significance of the helical flow in the aortic arch. Am. J. Physiol. Circ. Physiol. 2009, 297, H163–H170. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Fan, Y.; Deng, X. Effect of spiral flow on the transport of oxygen in the aorta: A numerical study. Ann. Biomed. Eng. 2010, 38, 917–926. [Google Scholar] [CrossRef]
- Zhan, F.; Fan, Y.-B.; Deng, X.-Y. Effect of swirling flow on platelet concentration distribution in small-caliber artificial grafts and end-to-end anastomoses. Acta Mech. Sin. 2011, 27, 833–839. [Google Scholar] [CrossRef]
- Clough, R.E.; Waltham, M.; Giese, D.; Taylor, P.R.; Schaeffter, T. A new imaging method for assessment of aortic dissection using four-dimensional phase contrast magnetic resonance imaging. J. Vasc. Surg. 2012, 55, 914–923. [Google Scholar] [CrossRef]
- Kilner, P.J.; Yang, G.Z.; Mohiaddin, R.H.; Firmin, D.N.; Longmore, D.B. Helical and retrograde secondary flow patterns in the aortic arch studied by three-directional magnetic resonance velocity mapping. Circulation 1993, 88, 2235–2247. [Google Scholar] [CrossRef]
- Oechtering, T.H.; Sieren, M.M.; Hunold, P.; Hennemuth, A.; Huellebrand, M.; Scharfschwerdt, M.; Richardt, D.; Sievers, H.-H.; Barkhausen, J.; Frydrychowicz, A. Time-resolved 3-dimensional magnetic resonance phase contrast imaging (4D Flow MRI) reveals altered blood flow patterns in the ascending aorta of patients with valve-sparing aortic root replacement. J. Thorac. Cardiovasc. Surg. 2019. [Google Scholar] [CrossRef] [PubMed]
- Hellmeier, F.; Nordmeyer, S.; Yevtushenko, P.; Bruening, J.; Berger, F.; Kuehne, T.; Goubergrits, L.; Kelm, M. Hemodynamic Evaluation of a Biological and Mechanical Aortic Valve Prosthesis Using Patient-Specific MRI-Based CFD. Artif. Organs 2018, 42, 49–57. [Google Scholar] [CrossRef] [PubMed]
- Vergara, C.; Viscardi, F.; Antiga, L.; Luciani, G.B. Influence of Bicuspid Valve Geometry on Ascending Aortic Fluid Dynamics: A Parametric Study. Artif. Organs 2012, 36, 368–378. [Google Scholar] [CrossRef] [PubMed]
- Sotiropoulos, F.; Le, T.B.; Gilmanov, A. Fluid Mechanics of Heart Valves and Their Replacements. Annu. Rev. Fluid Mech. 2016, 48, 259–283. [Google Scholar] [CrossRef]
- Toninato, R.; Salmon, J.; Susin, F.M.; Ducci, A.; Burriesci, G. Physiological vortices in the sinuses of Valsalva: An in vitro approach for bio-prosthetic valves. J. Biomech. 2016, 49, 2635–2643. [Google Scholar] [CrossRef]
- D’Antonio, G.C.; Weidner, B.V.; Rowe, S.A.; Pierrakos, O. Evaluating the Performance of Prosthetic Heart Valves: Transvalvular Pressure Drop vs. In Vortex Ring Formation Number. In Proceedings of the 2015 Systems and Information Engineering Design Symposium, Charlottesville, VA, USA, 24–24 April 2015; pp. 41–44. [Google Scholar]
- Gilmanov, A.; Sotiropoulos, F. Comparative hemodynamics in an aorta with bicuspid and trileaflet valves. Theor. Comput. Fluid Dyn. 2016, 30, 67–85. [Google Scholar] [CrossRef]
- Torii, R.; Oshima, M.; Kobayashi, T.; Takagi, K.; Tezduyar, T.E. Influence of wall thickness on fluid—Structure interaction computations of cerebral aneurysms. Int. J. Numer. Methods Biomed. Eng. 2010, 26, 336–347. [Google Scholar] [CrossRef]
- Zhu, G.-Y.; Wei, Y.; Su, Y.-L.; Yuan, Q.; Yang, C.-F. Impacts of Internal Carotid Artery Revascularization on Flow in Anterior Communicating Artery Aneurysm: A Preliminary Multiscale Numerical Investigation. Appl. Sci. 2019, 9, 4143. [Google Scholar] [CrossRef]










| Case | Element Number (Million) |
|---|---|
| 1 | 0.93 |
| 2 | 2.19 |
| 3 | 4.30 |
| 4 | 6.42 |
| 5 | 10.21 |
| 6 | 17.63 |
| 7 | 34.47 |
| 8 | 40.21 |
| Time Point | Vmean (cm/s) | Vmax (cm/s) | ||||
|---|---|---|---|---|---|---|
| SPAC Tubular | SPAC Molded | Conventional | SPAC Tubular | SPAC Molded | Conventional | |
| t1 | 6.42 | 6.81 | 6.92 | 12.86 | 22.23 | 20.34 |
| t2 | 6.54 | 7.01 | 6.89 | 12.14 | 16.03 | 12.54 |
| t3 | 37.93 | 36.88 | 37.01 | 77.83 | 76.48 | 75.49 |
| t4 | 63.25 | 60.15 | 58.59 | 139.56 | 135.53 | 131.13 |
| t5 | 28.90 | 27.83 | 27.65 | 58.98 | 56.54 | 54.14 |
| Time Point | SAWSS (Pa) | Low WSS Areas (cm2) | ||||
|---|---|---|---|---|---|---|
| SPAC Tubular | SPAC Molded | Conventional | SPAC Tubular | SPAC Molded | Conventional | |
| t1 | 0.18 | 0.19 | 0.19 | 102.57 | 101.08 | 100.8 |
| t2 | 0.20 | 0.20 | 0.25 | 100.31 | 100.11 | 98.35 |
| t3 | 0.52 | 0.50 | 0.50 | 48.90 | 68.49 | 61.49 |
| t4 | 5.03 | 4.82 | 4.74 | 0.85 | 1.99 | 2.38 |
| t5 | 0.35 | 0.34 | 0.31 | 65.22 | 84.12 | 73.81 |
| Segment | SAWSS (Pa) | ||
|---|---|---|---|
| SPAC Tubular | SPAC Molded | Conventional | |
| AAo | 3.55 | 2.95 | 2.74 |
| Aortic arch | 7.03 | 6.67 | 6.37 |
| DAo | 5.49 | 5.44 | 5.53 |
| Slice | Averaged Secondary Flow Velocity (cm/s) | Maximum Secondary Flow Velocity (cm/s) | ||||
|---|---|---|---|---|---|---|
| SPAC Tubular | SPAC Molded | Conventional | SPAC Tubular | SPAC Molded | Conventional | |
| 1 | 5.34 | 4.09 | 4.18 | 39.13 | 16.08 | 15.21 |
| 3 | 30.56 | 28.69 | 26.93 | 75.54 | 78.86 | 87.16 |
| 5 | 14.62 | 17.30 | 17.29 | 37.46 | 42.52 | 50.91 |
| Slice | Percentage Difference in Averaged Secondary Flow Velocity (%) | Percentage Difference in Maximum Secondary Flow Velocity (%) | ||||
|---|---|---|---|---|---|---|
| SPAC Tubular | SPAC Molded | Conventional | SPAC Tubular | SPAC Molded | Conventional | |
| 1 | 27.75 | −0.21 | 0 | 157.26 | 0.57 | 0 |
| 3 | 13.48 | 0.65 | 0 | −13.33 | −0.95 | 0 |
| 5 | −15.44 | 0.01 | 0 | −26.42 | −1.65 | 0 |
| Slice | Mean Secondary Velocity | Percentage Change (%) | |||
|---|---|---|---|---|---|
| SPAC Tubular | SPAC Molded | Conventional | SPAC Tubular | SPAC Molded | |
| slice 1 | 0.08 | 0.07 | 0.07 | 14.29 | 0.00 |
| slice 2 | 0.55 | 0.63 | 0.65 | 15.38 | 3.08 |
| slice 3 | 0.70 | 0.71 | 0.64 | 9.37 | 10.94 |
| slice 4 | 0.60 | 0.36 | 0.37 | 62.16 | 2.70 |
| slice 5 | 0.27 | 0.32 | 0.31 | 12.90 | 3.23 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhu, G.-Y.; Huang, H.; Su, Y.-L.; Yeo, J.-H.; Shen, X.-Q.; Yang, C.-F. Numerical Investigation of the Effects of Prosthetic Aortic Valve Design on Aortic Hemodynamic Characteristics. Appl. Sci. 2020, 10, 1396. https://doi.org/10.3390/app10041396
Zhu G-Y, Huang H, Su Y-L, Yeo J-H, Shen X-Q, Yang C-F. Numerical Investigation of the Effects of Prosthetic Aortic Valve Design on Aortic Hemodynamic Characteristics. Applied Sciences. 2020; 10(4):1396. https://doi.org/10.3390/app10041396
Chicago/Turabian StyleZhu, Guang-Yu, Hai Huang, Ya-Li Su, Joon-Hock Yeo, Xiao-Qin Shen, and Cheng-Fu Yang. 2020. "Numerical Investigation of the Effects of Prosthetic Aortic Valve Design on Aortic Hemodynamic Characteristics" Applied Sciences 10, no. 4: 1396. https://doi.org/10.3390/app10041396
APA StyleZhu, G.-Y., Huang, H., Su, Y.-L., Yeo, J.-H., Shen, X.-Q., & Yang, C.-F. (2020). Numerical Investigation of the Effects of Prosthetic Aortic Valve Design on Aortic Hemodynamic Characteristics. Applied Sciences, 10(4), 1396. https://doi.org/10.3390/app10041396






