1. Introduction
Due to the loss of sensory and motor functions of the lower extremities, paraplegic patients often suffer from various complications, such as a decrease in various organs’ functions, including the bladder, nerve and muscle atrophy, cardiovascular, and musculoskeletal diseases. As a rehabilitation treatment for such patients, muscular contractures are minimized, and secondary medical conditions caused by prolonged sitting such as osteoporosis, bedsores, and organ function decline can be improved through standing or regular gait training using a hip–knee–ankle–foot orthosis (HKAFO) or reciprocating-gait-orthosis (RGO) [
1,
2,
3,
4].
However, the frequency and duration of training are very important for recovering gait ability in paraplegic patients. Training using a traditional mechanical orthosis requires high energy, making it difficult to train for long periods. As a result, improving the chronic effects of spinal cord injury (SCI) becomes harder [
1].
A new treatment strategy that uses an exoskeleton system assisting each joint with electric motors has made promising developments. In particular, walk training was possible for approximately 20–50 min with the HKAFO or RGO, increasing up to 2 h by wearing the powered exoskeleton system [
1].
It is also known that the trunk muscle plays an important role in maintaining a sitting or standing position [
5]. To increase the activity of these muscles, overground gait training using an exoskeleton robot system appeared more efficient than Lokomat, which repeatedly trains a pre-defined joint trajectory on a treadmill [
6].
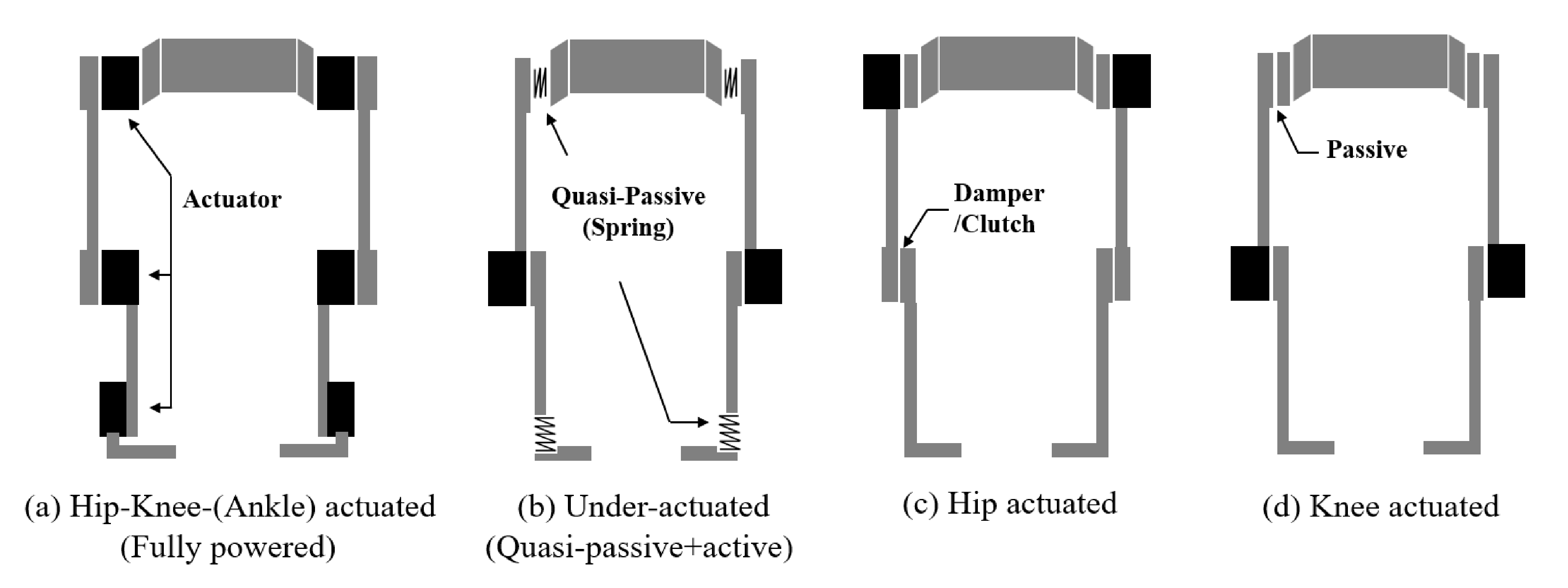
Figure 1a shows fully powered exoskeleton robots such as the Exso, Rewalk, and HAL, which have been developed to assist daily life activities such as standing, walking, and climbing stairs in paralyzed patients. They are also classified as Class II medical devices by the U.S. Food and Drug Administration (FDA). However, in real-life environments, these robots are very unstable for climbing stairs and have limitations in their wearability because they are heavy and bulky [
7]. Additionally, more than 60% of SCI patients are neurologically incomplete [
8]. For such incomplete paraplegic patients with some residual muscles, the AAN (assist as needed) [
9] approach may be useful. In particular, as the number of residual muscles increases, the functions to be assisted by the orthosis decreases, reducing the size of the exoskeletal gait orthosis (EGO) system [
8].
Figure 1b shows an under-actuated exoskeleton system that supports loads and assists in walking using a kinetic energy storage function, and is mainly used to aid the user’s power in industrial sites [
9,
10].
Figure 1c shows the phoenix developed by Suitx [
11] for gait rehabilitation. It has a hip-actuated-exoskeletal-gait orthosis (HAEGO), in which a motor assists only the hip joint, and a mechanical clutch is applied to the knee joint. It does not support higher functions such as climbing stairs, but basic movements, including sitting/standing/walking, are possible. Weighing 12.25 kg, it is lightweight and modular, with the advantage that the patients can wear it by themselves in a wheelchair.
The human knee joint plays an important role in performing most daily activities, such as sitting, standing, and walking. In particular, when the range of the knee’s motion is limited during walking, the patient’s metabolic cost increases because unnatural movements such as hip elevation are accompanied by compensation [
12]. Yu et al. have reported that the foot swing acceleration of the active knee joint system is larger than that of the active hip joint system in the swing section after toe-off [
13]. Based on these findings, the following two hypotheses were established. Firstly, by assisting the force that accelerates the body forward while walking through knee joint actuation, the user’s metabolic cost can be reduced, and the walking speed can be improved. Secondly, in general, a crutch is an assistive weight-bearing device for propulsion by patients using their arms when walking, but it causes pain in the arms and shoulders with a large energy expenditure [
14,
15]. Therefore, if the propulsion force is assisted by knee actuation, it is expected that the shoulder and hand pain will be reduced by lowering the dependence on the crutches.
In this study, based on the above hypotheses, a lightweight knee-actuated-exoskeletal-gait orthosis (KAEGO) was developed, as shown in
Figure 1d, and applied to an SCI patient with incomplete paraplegia. In addition, to verify the proposed hypotheses, a six minute walking test was performed using the KAEGO system. The metabolic cost, walking speed, and travel distance using the KAEGO were compared with those using a non-powered EGO.
Compared to a non-powered EGO, the use of the KAEGO system improved the overall gait performance, including walking speed, distance, and metabolic cost, with increasing assist torque applied to the knee joint. Based on these results, we are confident that the lightweight and inexpensive partial assistive exoskeleton system can be effectively utilized for gait rehabilitation in incomplete paraplegic patients. In the future, we plan to verify the effectiveness of the proposed system in different injury levels and a larger number of patients.
The remainder of this paper is structured as follows.
Section 2 describes the configuration of the KAEGO system, sensor structure, classification of the gait mode, control model, and experimental protocol.
Section 3 analyzes the results of the walking experiment, and
Section 4 reviews the validity of the proposed hypotheses based on the experimental results.
2. Materials & Methods
2.1. System Configuration of KAEGO
The system configuration of KAEGO developed in this study is shown in
Figure 2. It consists of a high-level controller that manages the left and right gait phases from sensor information and a low-level controller that is mounted on each knee actuator module for torque control of the knee. The main controller, sensor, and knee actuator can be easily separated into modules; therefore it is designed to be converted into a non-powered exoskeleton orthosis if necessary. The hip joint is coupled to the waist brace by a bearing with low friction. The adduction/abduction and intra/extra rotation of the hip joint is limited, allowing the patient to move the hip joint forward stably or backward by the upper body motion using an elbow crutch. The waist brace was made of urethane foam to match the patient’s body shape, and its weight was minimized using a carbon composite material. The pelvic link was designed to be detachable from the hip joint. If the pelvic link is connected to the hip joint, the exoskeleton system can be used like an RGO.
2.2. Knee Actuator Module Design
Based on a normal person’s clinical gait analysis, the torque required for the knee joint in one gait cycle is approximately 40 Nm and 15 Nm in the stance and swing sections, respectively [
12]. In a paraplegic patient wearing an EGO, crutches are used to walk, which distribute the load on the knee joint during walking. Therefore, the load on the knee joint in this patient will be lower than in a normal person. In this study, to minimize the system’s volume and weight, the actuator output was designed to cover the swing section at a maximum of 20 Nm, and an electric brake was also built in to prevent falls in cases of emergency.
Figure 3 shows the developed knee actuation module, and the design specifications are shown in
Table 1.
The low-level motion controller is an integrated control module that includes a motor driver and various sensor interfaces and performs torque control of the knee actuation module. In addition, it acts as a sensor interface that transmits the knee and hip joint angle measured from the potentiometer and the inertial measurement unit (IMU), the ground reaction force (GRF) sensor signal, and the motion status parameters of the actuator to the high-level controller through the controller area network (CAN) interface.
2.3. Human Machine Synchronization
In exoskeleton system research, the technology used for motion synchronization with the wearer is very important in terms of the gait training effect and metabolic cost. For accurate motion synchronization, it is necessary to accurately and quickly recognize the wearer’s motion and force, but the generalized human–robot interfacing technology has not yet been developed [
13]. For the exoskeleton system to respond more flexibly and rapidly, predicting the joint’s movement in advance is necessary. Among several studies, methods using electromyogram (EMG) [
7] or electroencephalography (EEG) [
16] signals are representative. However, the muscular EMG signal detector is inconvenient to wear because the sensor is attached to the skin surface, and the method using EEG is still in the research stage and is being developed by various sensor combinations [
13].
In this study, motion synchronization between the exoskeleton system and the user was achieved, as shown in
Figure 4. While the exoskeleton system detects the user’s intention of walking by using complex sensors such as the ground reaction force (GRF) and IMU sensors, the wearer recognizes the operation state of the exoskeleton system by a buzzer sound and visual feedback. Using this synchronization technique, users can more easily adapt to the motion of the exoskeleton system.
2.4. GRF Sensor Design
In the exoskeleton system, the GRF sensor is related to the wearer’s gait pattern and is widely used because it can directly detect the presence or absence of contact between the foot and the ground [
12]. As shown in
Figure 5, we developed a GRF sensor module with three load cells attached to the rear foot, mid-foot, and forefoot areas to detect changes in heel contact, mid-stance, and toe-off. The toe and heel signals were designed to have a temporal deviation according to the ground condition around the mid-sensor. For example, on flat ground, the heel signal was temporally ahead of the mid, but when going up a slope, the toe signal was temporally ahead of the mid. The load-cell sensor applied to measure GRF was a half-bridge type low-cost sensor that could measure up to 50 kg each and had repeatability of 0.05 FS.
2.5. Gait Mode Estimation and Finite State Machine Design
In general, walking can be divided into stance and swing sections. In a normal person, walking is clinically divided into several stages, as needed [
12]. In this study, to develop a simple and predictable gait control protocol, as shown in
Figure 6, the gait mode was classified into four functional modes (SWF: swing flexion, SWE: swing extension, STF: stance flexion, and STE: stance extension).
The patient wearing the EGO first moves the center of gravity to the opposite leg for walking and then uses the trunk muscles to create a hip movement to move the leg. Therefore, the patient’s walking intention can be predicted by the movement of the center of gravity and the hip’s motion.
As shown in Equation (1), the differential values (
) of the left and right GRF sensors were extracted to detect the movement of the center of gravity, and the average values (
) of the mid-sensor (
) and heel-sensor (
) were applied as differential data.
Figure 7 shows the KAEGO’s finite state machine for gait control developed in this study. The initial state was set to the STE mode, and the knee actuator was driven with high impedance to keep the patient in a standing position.
SWF (mode 1) is the first step in a gait cycle, and when the gait controller detects the patient’s gait intention, it generates a patient-specific knee flexion torque, and a buzzer notifies the patient that the gait mode is switched to swing mode. In addition, the knee angle () is controlled in real-time so as to not exceed the reference value, and when the change in knee angular velocity () decreases below the reference value, it is switched to the SWE (mode 2). In this mode, a patient-specific extension torque is applied to the knee actuator to extend the flexed knee.
STF (mode 3) is a preparatory step for the impact when the foot touches the ground and is switched when the knee is fully extended or heel contact () is detected. At this time, the knee actuator acts as a mechanical spring or damper and is driven to minimize the impact applied to the knee joint when contacting the heel.
STE (mode 4) is a mid-stance section, as shown in
Figure 5b, where the knee is fully extended, and the sole is parallel to the ground. In this mode, one gait cycle is completed, and if the controller detects the patient’s intention to walk again, the state is switched to SWF, and a new gait cycle is started.
2.6. Control Model
General position-based control is a method that forces the system to follow a specified trajectory. However, a high output torque is required for the system to track motion without dynamic interaction with the user [
17]. In contrast, impedance control is a suitable control method for systems that require interaction with the wearer and is widely applied to the development of various rehabilitation assistance systems such as powered knee prostheses and exoskeleton systems [
10,
13,
17]. The more residual muscles the wearer has, the less the load that the exoskeleton system needs to assist, allowing the selection of a low-power actuator, thereby reducing the volume and weight of the system.
Based on previous studies, the output torque required for the knee joint can be expressed as a simple piecewise passive impedance function of linear spring (
k) and damping (
d) terms (
Figure 8) [
17,
18]. In this study, the output torque
was defined as a simple passive impedance model composed of user-customized torque
and passive impedance terms, as shown in Equation (2) below, to generate a negative torque in the stance mode and active torque in the swing mode. The user customized load torque changes according to the patient’s body condition and the degree of gait training; mathematical modeling was practically impossible. Therefore, the knee torque profiles for flexion and extension of each gait phase were experimentally set. The user customized torque profile is shown in
Figure 8b.
Table 2 shows the maximum user-customized load torque and impedance coefficients for each gait mode applied to the 6 min walk test. The mechanical friction of the knee joint was simplified by the Coulomb friction coefficient (
), and the variation in the friction torque according to the angular velocity was ignored.
where
is the knee angle and
is the equilibrium knee angle at each gait mode.
2.7. Experimental Protocol
To verify the effectiveness of the KAEGO system for gait rehabilitation, a 6 min walking test was conducted on one paraplegic patient with incomplete SCI. For the subject’s safety, the experiment was conducted based on guidelines (RERI-IRB-200318-2), pre-approved by the Rehabilitation Engineering Research Institute ethics committee. The patient consented to participate in the study, which was conducted under the guidance of a professional therapist.
The patient who participated in the experiment had been training with the non-powered EGO (RGO) for many years, so he adapted quickly to the new KAEGO system. He was, therefore, a suitable subject for the comparative evaluation of KAEGO with the non-powered orthosis. The characteristics of the subject have been summarized in
Table 3.
KAEGO was manufactured by installing two knee actuation modules and a control module with a battery in the non-powered EGO that the subject had been using for training. Accordingly, the weight of KAEGO was 13.85 kg, which was approximately 5.5 kg higher than that of the non-powered orthosis.
The 6 min walking test is widely used to evaluate the physical activity in patients by comparing their metabolic consumption [
1,
19]. In this study, a walking test was conducted under three conditions: (i) wearing non-powered EGO vs. KAEGO; (ii) setting the knee-assisting torque to approximately 25% (5 Nm); and (iii) approximately 100% (20 Nm) of the rated torque. The detailed user customized torque data for the gait experiment are defined in
Table 4. The changes in metabolic cost, walking speed, and the distance traveled in patients with these three EGOs were compared. Before the experiment, the participant trained for 60 min per session, three sessions a week, and for at least 10 sessions to adapt to each system. In addition, a preliminary test was conducted once on the day of the experiment so that the participant could fully understand the protocol. The equipment used in the experiment was K4b
2 (Cosmed, Roma Italy) [
20], which was used to calculate the metabolic cost by measuring the subject’s oxygen consumption (VO
2) and heart rate (HR), as shown in
Figure 9a.
Figure 9b shows the 60 m track around which the patient walked at a comfortable speed for 6 min and measured the walking energy efficiency. Each experiment was conducted three times.
The metabolic cost of transport (COT) while walking has been applied to quantitatively evaluate the walking efficiency of patients with incomplete SCI and wearing the proposed exoskeleton system [
10]. This metabolic COT quantifies the energy required to move an individual or object from one place to another and is widely used as a method for evaluating human walking efficiency [
21]. It is calculated by normalizing the total energy to the distance traveled and the total weight. The total energy consumed in the 6 min walking experiment was calculated by measuring the calorie consumption and converting it to energy for 3 min after the stabilization period. The total weight was 81.95 kg, including the patient’s weight, laboratory equipment, and the exoskeleton system. The distance walked was calculated using the average walking speed for 3 min to measure the total energy.
4. Discussion
In this study, we hypothesized that the metabolic cost associated with walking would decrease and walking speed would increase based on the knee joint activation. To verify this hypothesis, a modular knee actuator installed in a non-powered EGO was developed. A walking metabolic cost test demonstrated the effectiveness of the proposed system in one SCI patient with incomplete paraplegia.
We found that when the KAEGO was worn, VO
2 and HR showed a small increase, but the distance traveled and walking speed increased significantly. The COT, which indicates the overall energy consumption, decreased by up to 24.5% as the knee assist torque increased. As compare
Table 5 and
Table 7, despite an increase in weight of 5.5 kg compared to the non-powered EGO, the user’s COT decreased by up to 24%, and the travel distance increased by up to 37%. These findings confirm that the proposed KAEGO system improves the walking energy efficiency in patients with incomplete paraplegia.
The increase in the patient’s HR is presumed to be due to the increase in the weight of the exoskeleton system and the limited freedom of the knee joint due to incomplete synchronization [
10]. In addition, because the knee assist torque generates a large motion, a higher level of concentration is required to maintain gait balance, which could be the cause for the increase in the patient’s HR.
The study participant was a 40-year-old man who could walk with a non-powered EGO but was only able to train for less than 20 min per session due to muscle pain in the wrist and shoulder caused by the use of an elbow crutch. However, when using the KAEGO, he felt his dependence on the elbow crutch was reduced due to the knee motion assist, reducing the wrist and shoulder pain. This met the second hypothesis we proposed. As a result, he could train for double the time or more, without much difficulty. In particular, when wearing the non-powered EGO, the patient had to maintain the tension of the residual muscles at all times to prevent sudden flexion of the knee joint in the stance section. However, because KAEGO prevents sudden flexion, the patient felt more stable in the standing position.
In conclusion, the KAEGO is a lightweight and efficient exoskeleton system that is effective in improving gait and rehabilitation of incomplete SCI patients, but has limitations that can only be applied to patients with high trunk muscle activity and voluntary hip motion. In this case, the application of a pelvic-link like RGO can also be considered as a way to supplement the limitations of KAEGO. Additionally, the developed exoskeleton system is not for daily life, but only for gait rehabilitation training, and the training has to be performed under the guidance of at least one professional therapist.
In the follow-up study, an objective evaluation of the changes in the overall gait balance, upper trunk muscle activity, and the elbow crutch’s influence is necessary through 3D gait analysis. In addition, the effectiveness of the proposed system should be further verified in multiple patients with various injury levels.