Comparison Method of Biomechanical Analysis of Trans-Tibial Amputee Gait with a Mechanical Test Machine Simulation
Abstract
:Featured Application
Abstract
1. Introduction
2. Materials and Methods
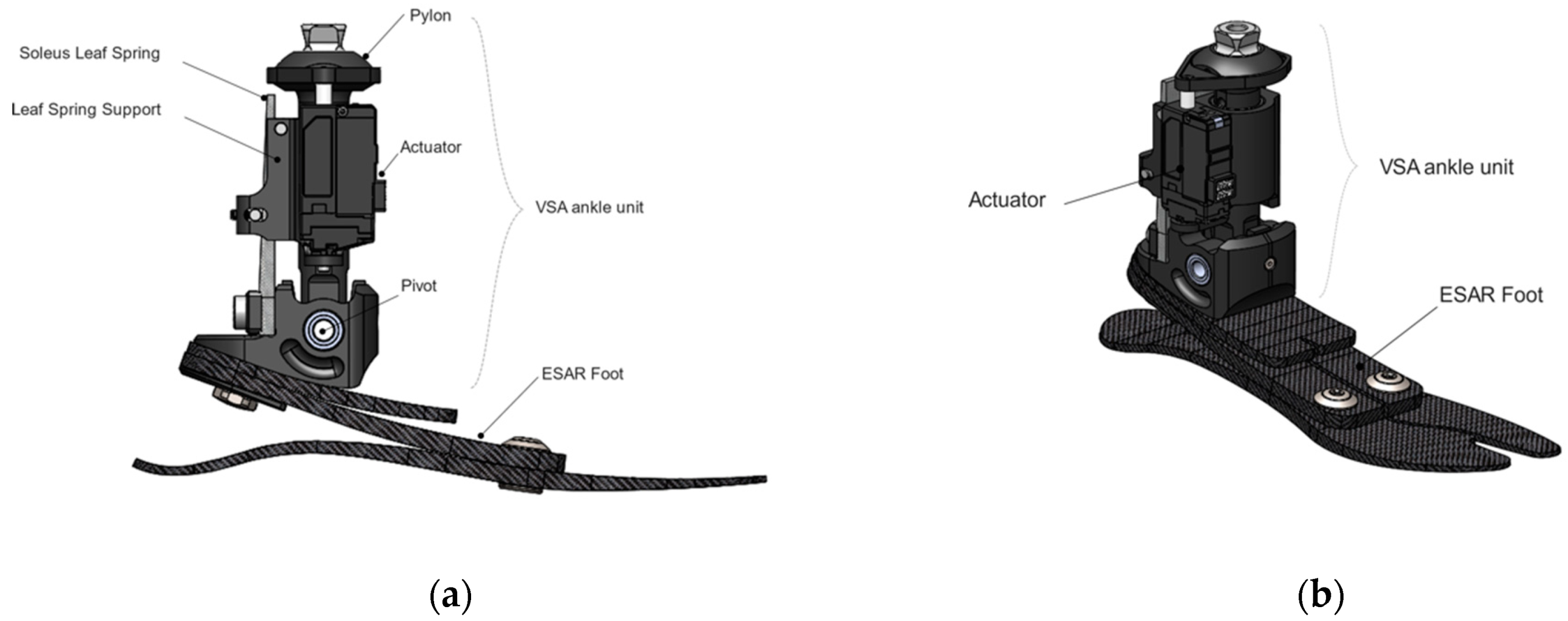
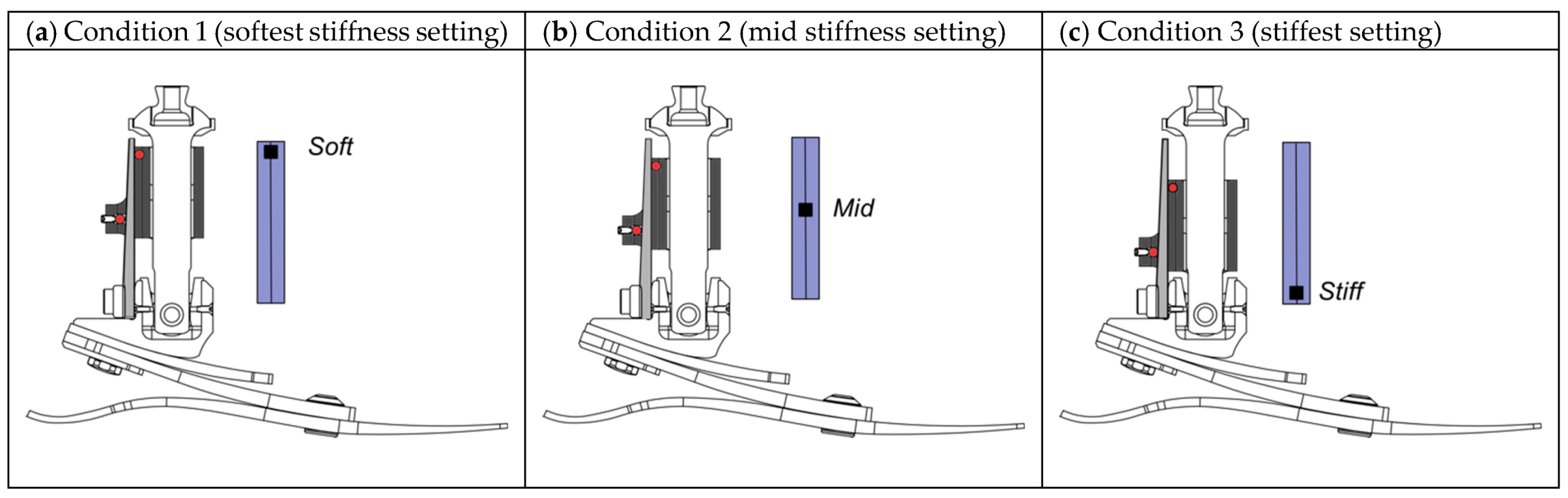
2.1. Prosthetic Foot Assessed
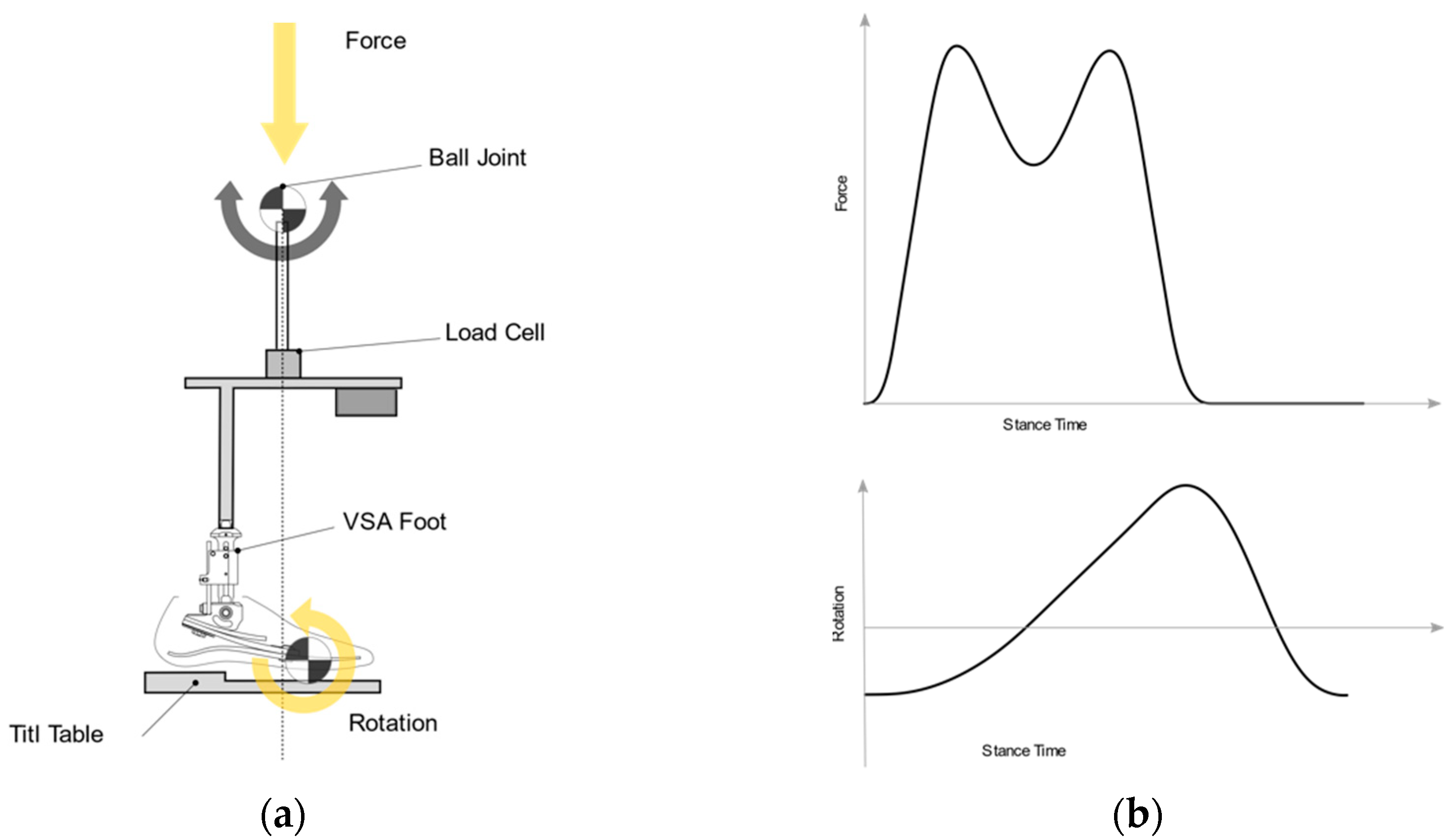
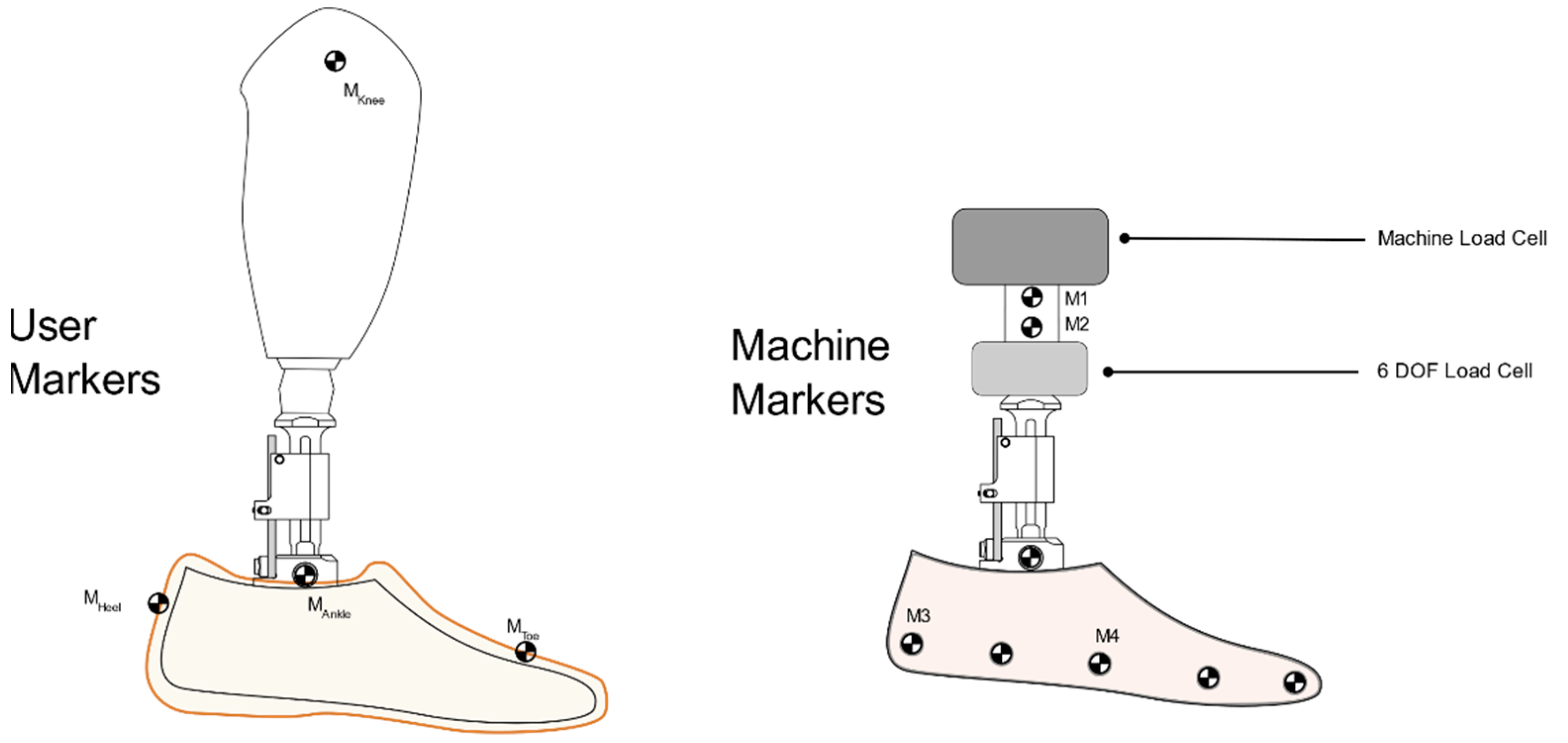
2.2. Mechanical Testing
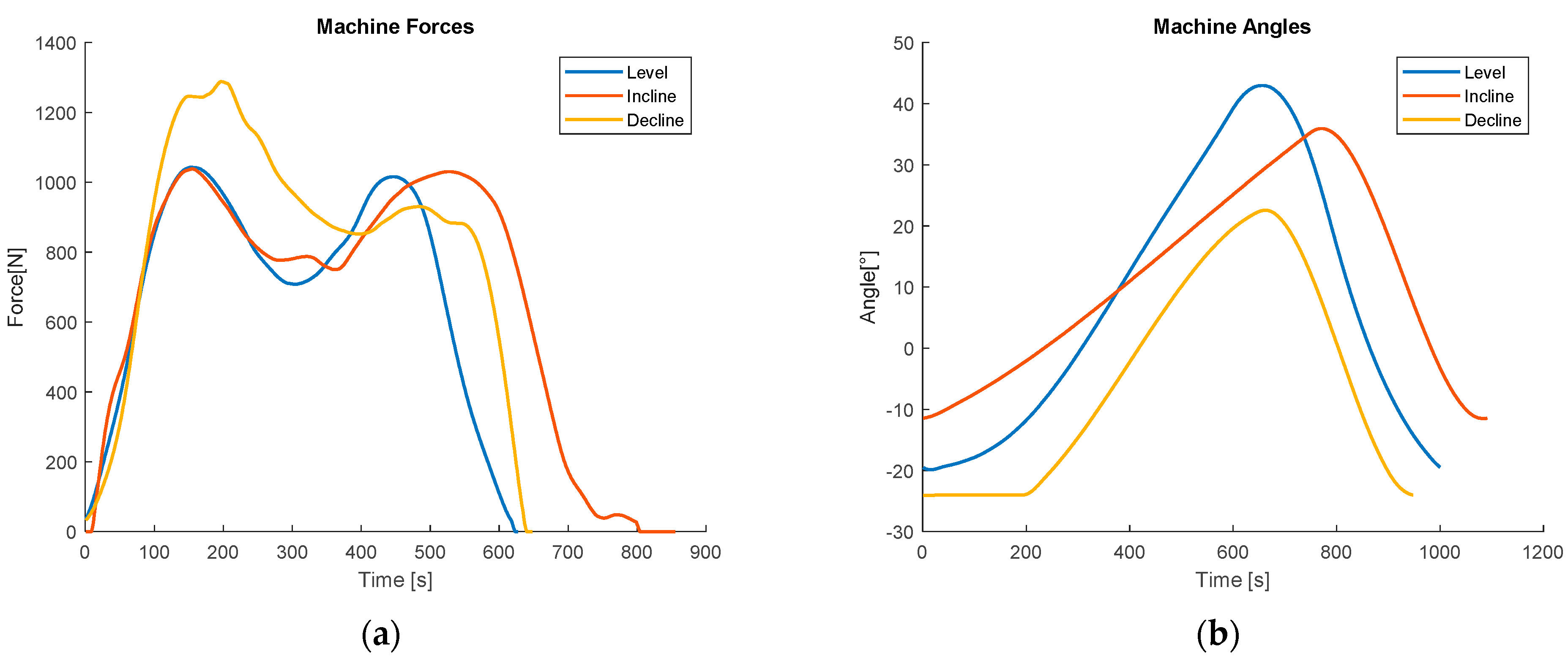
2.2.1. Level Ground
2.2.2. Ramp Input
2.3. User Testing
2.3.1. Users
2.3.2. User Data Collection and Processing
2.3.3. Functional Joint Center Calculation
2.4. Statistics
3. Results
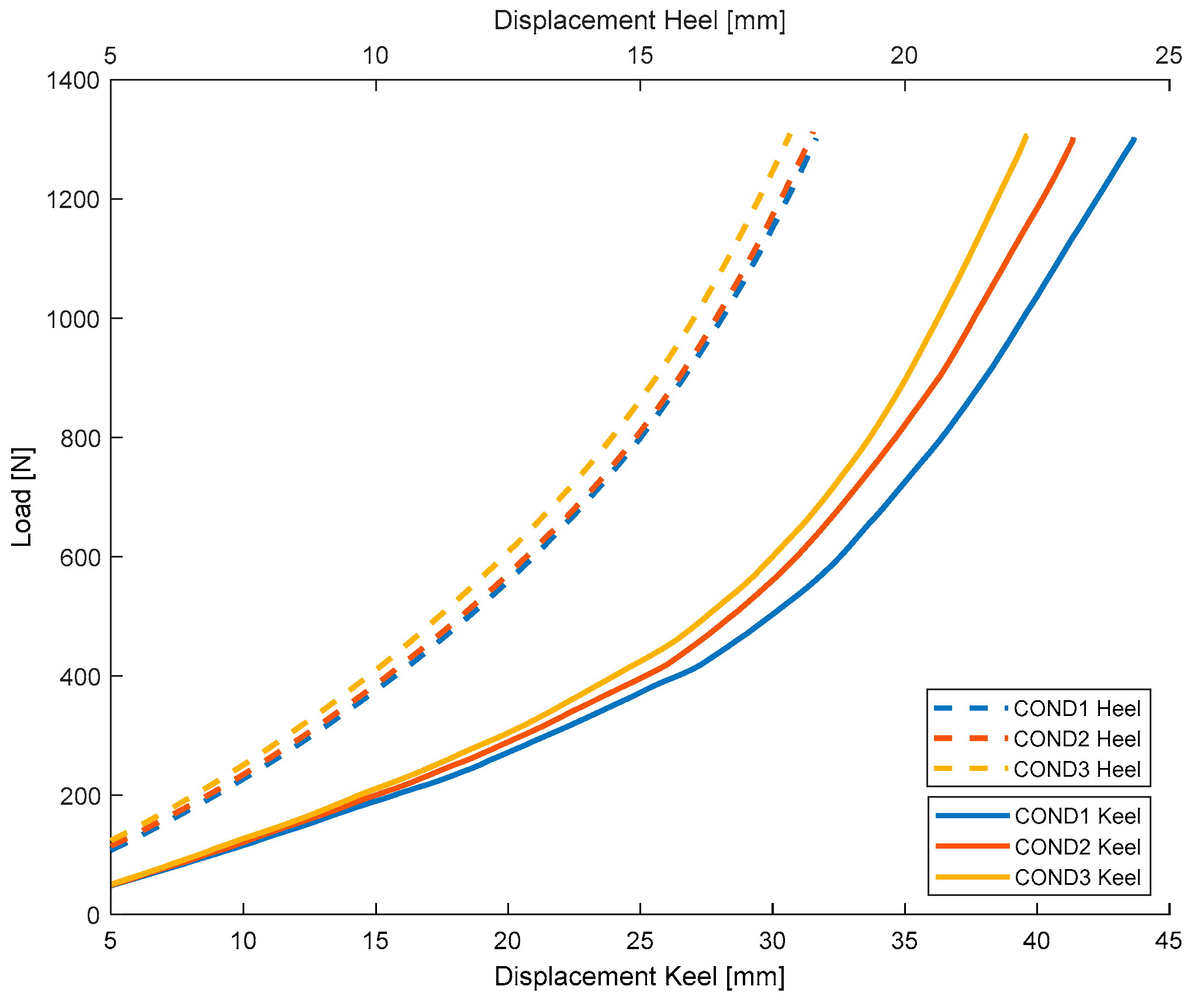
3.1. Force Displacement–Static
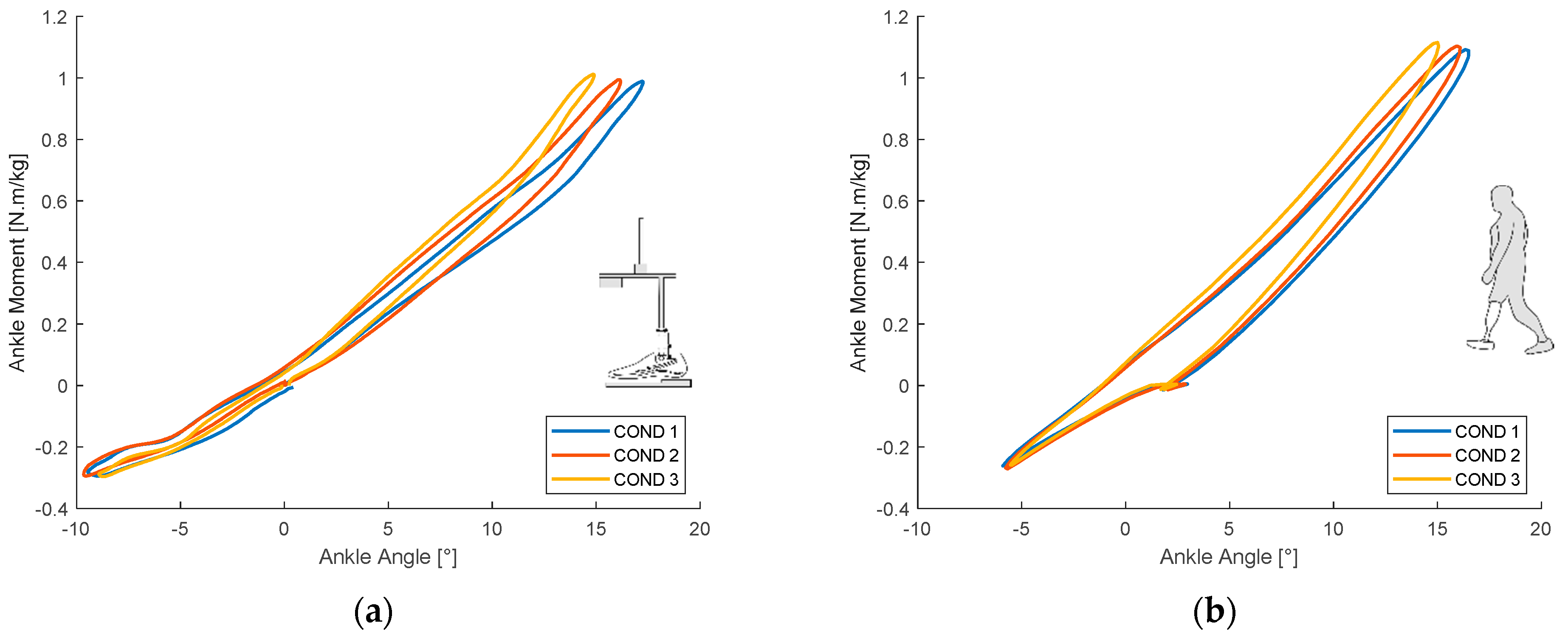
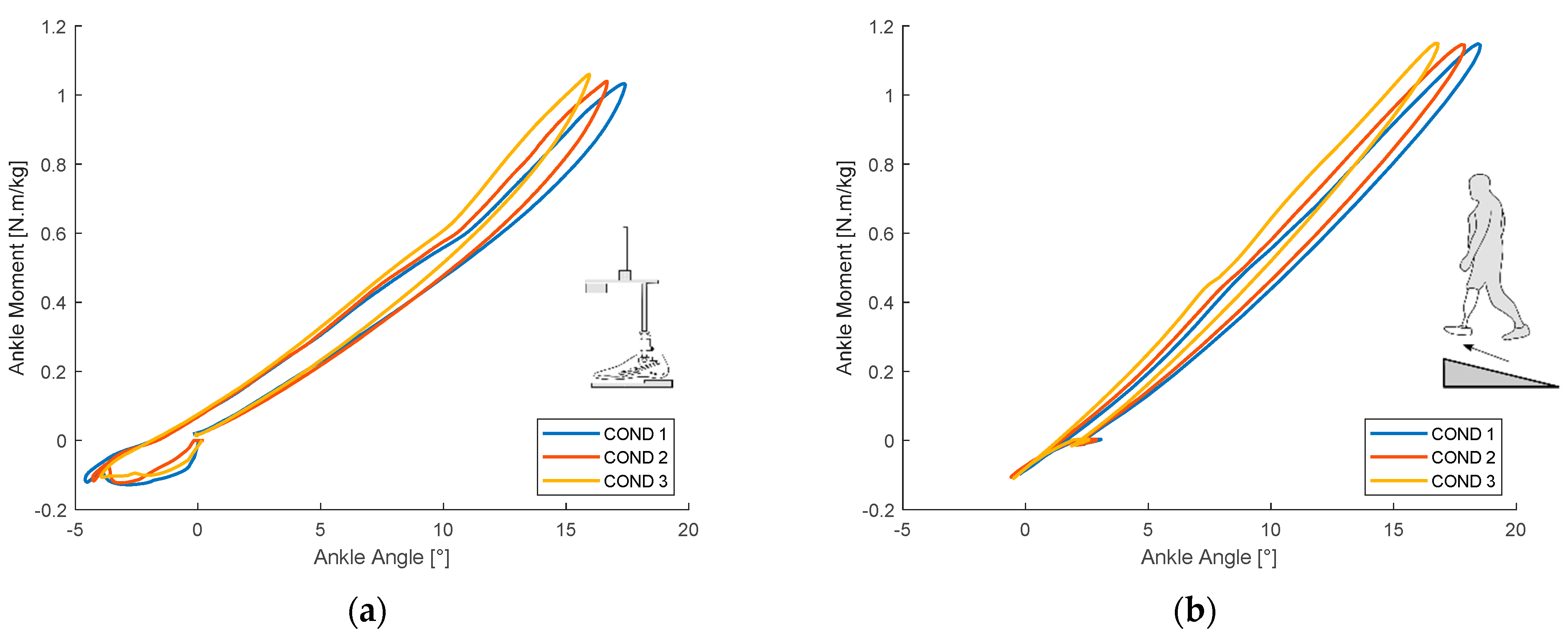
3.2. Ankle Sagittal Moment-Test Machine & Biomechanical Results
3.2.1. Level Ground
3.2.2. Ramp
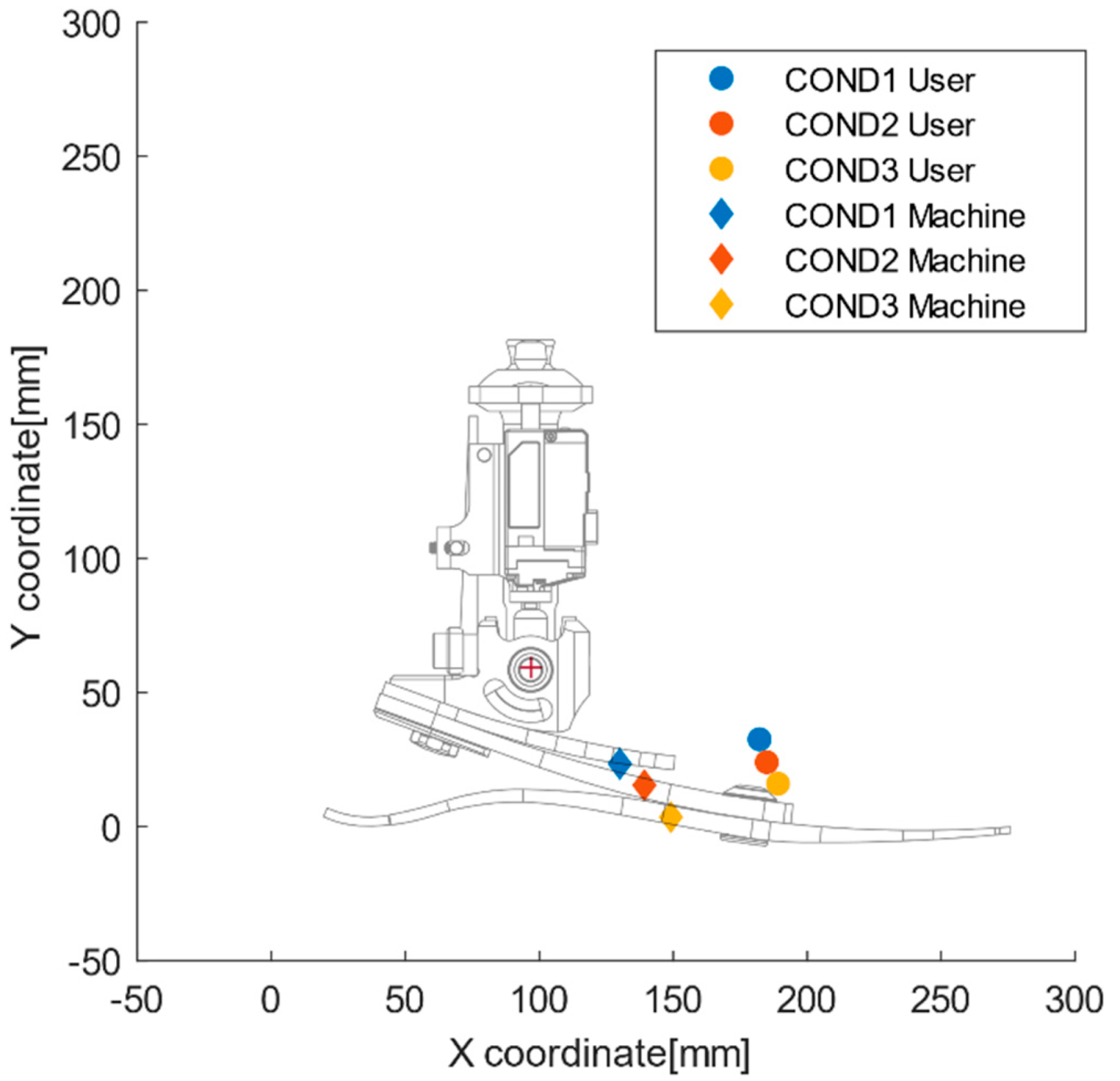
3.2.3. Functional Joint Center
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Riegger, C.L. Anatomy of the Ankle and Foot general osteology and foot shape. Phys. Ther. J. 1988, 68, 1802–1814. [Google Scholar] [CrossRef]
- Heitzmann, D.; Putz, C.; Wolf, S.I. Benefits of an increased prosthetic ankle range of motion for individuals with a trans- tibial amputation walking with a new prosthetic foot Daniel. Gait Posture 2018. [Google Scholar] [CrossRef]
- Childers, W.L.; Takahashi, K.Z. Increasing prosthetic foot energy return affects whole-body mechanics during walking on level ground and slopes. Sci. Rep. 2018, 8, 5354. [Google Scholar] [CrossRef]
- Versluys, R.; Beyl, P.; Van Damme, M.; Desomer, A.; Van Ham, R.; Lefeber, D. Prosthetic feet: State-of-the-art review and the importance of mimicking human anklefoot biomechanics. Disabil. Rehabil. Assist. Technol. 2009, 4, 65–75. [Google Scholar] [CrossRef]
- Andrysek, J. Lower-limb prosthetic technologies in the developing world: A review of literature from 1994–2010. Prosthet. Orthot. Int. 2010, 34, 378–398. [Google Scholar] [CrossRef]
- Kobayashi, T.; Orendurff, M.S.; Arabian, A.K.; Rosenbaum-Chou, T.G.; Boone, D.A. Effect of prosthetic alignment changes on socket reaction moment impulse during walking in transtibial amputees. J. Biomech. 2014, 47, 1315–1323. [Google Scholar] [CrossRef] [PubMed]
- Bellmann, M.; Blumentritt, S.; Pusch, M.; Schmalz, T.; Schönemeier, M. Measuring Technology The 3D L.A.S.A.R.—A New Generation of Static Analysis for Optimising Prosthetic and Orthotic Alignment. Orthopädie Tech. 2017, 12, 18–25. [Google Scholar]
- Macfarlane, P.A.; Nielsen, D.H.; Shurr, D.G.; Meier, K.G.; Clark, R.; Kerns, J.; Moreno, M.; Ryan, B. Transfemoral amputee physiological requirements:Comparison Between SACH Foot Walking and Flex-Foot Walking. J. Prosthet. Orthot. 1997, 9, 138–143. [Google Scholar] [CrossRef]
- Underwood, H.A.; Tokuno, C.D.; Eng, J.J. A comparison of two prosthetic feet on the multi-joint and multi-plane kinetic gait compensations in individuals with a unilateral trans-tibial amputation. Clin. Biomech. 2004, 19, 609–616. [Google Scholar] [CrossRef] [Green Version]
- Womac, N.D.; Neptune, R.R.; Klute, G.K. Stiffness and energy storage characteristics of energy storage and return prosthetic feet. Prosthet. Orthot. Int. 2019, 43, 266–275. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sawers, A.; Hahn, M.E. Trajectory of the center of rotation in non-articulated energy storage and return prosthetic feet. J. Biomech. 2011, 44, 1673–1677. [Google Scholar] [CrossRef]
- Rusaw, D.; Ramstrand, N. Sagittal plane position of the functional joint centre of prosthetic foot/ankle mechanisms. Clin. Biomech. 2010, 25, 713–720. [Google Scholar] [CrossRef] [Green Version]
- Lecomte, C.; Armannsdottir, A.L.; Starker, F.; Tryggvason, H.; Briem, K.; Brynjólfsson, S. Variable Stiffness Foot Design and Validation. J. Biomech. 2021, 122, 110440. [Google Scholar] [CrossRef]
- ISO. ISO/DIS 16955 Prosthetics—Quantification of Physical Parameters of Ankle/Foot Devices and Foot Units. 2012. Available online: https://www.iso.org/standard/69821.html (accessed on 31 May 2021).
- Technical Committee ISO/TC 168 “Prosthetics and Orthotics” ISO 10328:2016 Prosthetics—Structural Testing. 2016. Available online: https://www.iso.org/standard/70205.html (accessed on 31 May 2021).
- ISO. ISO 22675:2016 Foot Devices and Foot Units. 2016. Available online: https://www.iso.org/standard/70203.html (accessed on 31 May 2021).
- Starker, F.; Blab, F.; Dennerlein, F.; Schneider, U. A Method for Sports Shoe Machinery Endurance Testing: Modification of ISO 22675 Prosthetic Foot Test Machine for Heel-to-toe Running Movement. Procedia Eng. 2014, 72, 405–410. [Google Scholar] [CrossRef]
- Lai, H.J.; Yu, C.H.; Kao, H.C.; Chen, W.C.; Chou, C.W.; Cheng, C.K. Ankle-foot simulator development for testing ankle-foot orthoses. Med. Eng. Phys. 2010, 32, 623–629. [Google Scholar] [CrossRef]
- Robertson, D.G.E.; Dowling, J.J. Design and responses of Butterworth and critically damped digital filters. J. Electromyogr. Kinesiol. 2003, 13, 569–573. [Google Scholar] [CrossRef]
- American Orthotic and Prosthetic Association AOPA Prosthetic Foot Project Report. Available online: https://www.aopanet.org/wp-content/uploads/2013/12/Prosthetic_Foot_Project.pdf (accessed on 17 June 2020).
- Halsne, E.G.; Czerniecki, J.M.; Shofer, J.B.; Morgenroth, D.C. The effect of prosthetic foot stiffness on foot-ankle biomechanics and relative foot stiffness perception in people with transtibial amputation. Clin. Biomech. 2020, 80. [Google Scholar] [CrossRef] [PubMed]
- Major, M.J.; Howard, D.; Jones, R.; Twiste, M. The effects of transverse rotation angle on compression and effective lever arm of prosthetic feet during simulated stance. Prosthet. Orthot. Int. 2012, 36, 231–235. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Webber, C.M.; Kaufman, K. Instantaneous stiffness and hysteresis of dynamic elastic response prosthetic feet. Prosthet. Orthot. Int. 2017, 41, 463–468. [Google Scholar] [CrossRef] [PubMed]
- Rigney, S.; Simmons, A.; Kark, L. Energy Storage and Return Prostheses: A Review of Mechanical Models. Crit. Rev. Biomed. Eng. 2016, 44, 269–292. [Google Scholar] [CrossRef]
- Curtze, C.; Hof, A.L.; van Keeken, H.G.; Halbertsma, J.P.K.; Postema, K.; Otten, B. Comparative roll-over analysis of prosthetic feet. J. Biomech. 2009, 42, 1746–1753. [Google Scholar] [CrossRef] [PubMed]
- Schnall, B.L.; Dearth, C.L.; Elrod, J.M.; Golyski, P.R.; Koehler-McNicholas, S.R.; Ray, S.F.; Hansen, A.H.; Hendershot, B.D. A more compliant prosthetic foot better accommodates added load while walking among Servicemembers with transtibial limb loss. J. Biomech. 2019, 109395. [Google Scholar] [CrossRef] [PubMed]
- Klodd, E.; Hansen, A.; Fatone, S.; Edwards, M. Effects of prosthetic foot forefoot flexibility on oxygen cost and subjective preference rankings of unilateral transtibial prosthesis users. J. Rehabil. Res. Dev. 2010, 47, 543–552. [Google Scholar] [CrossRef]
- Fradet, L.; Alimusaj, M.; Braatz, F.; Wolf, S.I. Biomechanical analysis of ramp ambulation of transtibial amputees with an adaptive ankle foot system. Gait Posture 2010, 32, 191–198. [Google Scholar] [CrossRef]
- Michelini, A.; Eshraghi, A.; Andrysek, J. Two-dimensional video gait analysis: A systematic review of reliability, validity, and best practice considerations. Prosthet. Orthot. Int. 2020, 44, 245–262. [Google Scholar] [CrossRef] [PubMed]
- Fogelberg, D.J.; Allyn, K.J.; Smersh, M.; Maitland, M.E. What People Want in a Prosthetic Foot: A Focus Group Study. J. Prosthet. Orthot. 2016. [Google Scholar] [CrossRef] [PubMed]
- Shepherd, M.K.; Rouse, E.J. Comparing Preference of Ankle-Foot Stiffness in Below-Knee Amputees and Prosthetists. Press. Nat. Sci. Reports 2020. [Google Scholar] [CrossRef] [PubMed]
- Zelik, K.E.; Huang, T.W.P.; Adamczyk, P.G.; Kuo, A.D. The role of series ankle elasticity in bipedal walking. J. Theor. Biol. 2014, 346, 75–85. [Google Scholar] [CrossRef] [Green Version]
- Lamers, E.P.; Eveld, M.E.; Zelik, K.E. Subject-specific responses to an adaptive ankle prosthesis during incline walking. J. Biomech. 2019, 95, 109273. [Google Scholar] [CrossRef]
- Safaeepour, Z.; Esteki, A.; Ghomshe, F.T.; Azuan, N.; Osman, A. Quantitative analysis of human ankle characteristics at different gait phases and speeds for utilizing in ankle-foot prosthetic design. Biomed. Eng. Online 2014, 13, 1–8. [Google Scholar] [CrossRef] [Green Version]

| User | A | B | C | D | E |
|---|---|---|---|---|---|
| Gender | Male | Male | Male | Male | Male |
| Age (years) | 53 | 60 | 42 | 59 | 72 |
| Height (cm) | 179 | 187 | 177 | 180 | 182 |
| Mass (kg) | 103 | 82 | 100 | 100 | 102 |
| Foot size (cm) | 27 | 27 | 26 | 27 | 27 |
| BMI (kg/m2) | 32.1 | 24 | 31.9 | 30.9 | 30.8 |
| Amputated side | Right | Right | Right | Left | Left |
| Time since amputation (years) | 16 | 43 | 9 | 4 | 8 |
| Prescribed prosthetic foot | Pro-Flex Pivot | Vari-Flex XC | Pro-Flex XC | Pro-Flex XC | Vari-Flex with Quick Align |
| Prosthetic foot stiffness category | Cat. 5 | Cat. 5 | Cat. 6 | Cat. 6 | Cat. 6 |
| Cause of amputation | Trauma | Trauma | Trauma | Trauma | Trauma |
| Condition | Maximum Ankle Plantarflexion (°) | Maximum Ankle Dorsiflexion (°) | ||||||
|---|---|---|---|---|---|---|---|---|
| Machine Test | Biomechanical Test | Correlation Coefficient | p | Machine Test | Biomechanical Test | Correlation Coefficient | p | |
| COND 1: Level | −9.6 | −5.9 | 0.961 | 0.179 | 17.2 | 16.5 | 0.998 | 0.043 |
| COND 2: Level | −9.4 | −5.7 | 16.1 | 15.9 | ||||
| COND 3: Level | −8.8 | −5.5 | 14.8 | 15.0 | ||||
| COND 1: Incline | −4.6 | −0.2 | −0.564 | 0.619 | 17.4 | 18,4 | 0.995 | 0.065 |
| COND 2: Incline | −4.2 | −0.5 | 16.6 | 17.7 | ||||
| COND 3: Incline | −3.6 | −0.4 | 15.8 | 16,7 | ||||
| COND 1: Decline | −14.8 | −8.0 | 0.963 | 0.173 | 13.5 | 15.7 | 0.986 | 0.106 |
| COND 2: Decline | −14.5 | −7.8 | 12.6 | 15.1 | ||||
| COND 3: Decline | −14.1 | −7.7 | 12.2 | 14.6 | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lecomte, C.; Ármannsdóttir, A.L.; Starker, F.; Briem, K.; Brynjólfsson, S. Comparison Method of Biomechanical Analysis of Trans-Tibial Amputee Gait with a Mechanical Test Machine Simulation. Appl. Sci. 2021, 11, 5318. https://doi.org/10.3390/app11125318
Lecomte C, Ármannsdóttir AL, Starker F, Briem K, Brynjólfsson S. Comparison Method of Biomechanical Analysis of Trans-Tibial Amputee Gait with a Mechanical Test Machine Simulation. Applied Sciences. 2021; 11(12):5318. https://doi.org/10.3390/app11125318
Chicago/Turabian StyleLecomte, Christophe, Anna Lára Ármannsdóttir, Felix Starker, Kristin Briem, and Sigurður Brynjólfsson. 2021. "Comparison Method of Biomechanical Analysis of Trans-Tibial Amputee Gait with a Mechanical Test Machine Simulation" Applied Sciences 11, no. 12: 5318. https://doi.org/10.3390/app11125318
APA StyleLecomte, C., Ármannsdóttir, A. L., Starker, F., Briem, K., & Brynjólfsson, S. (2021). Comparison Method of Biomechanical Analysis of Trans-Tibial Amputee Gait with a Mechanical Test Machine Simulation. Applied Sciences, 11(12), 5318. https://doi.org/10.3390/app11125318






