Applicability of Semi-Quantitative Evaluation of the Intercondylar Notch
Abstract
:Featured Application
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Patient Cohort
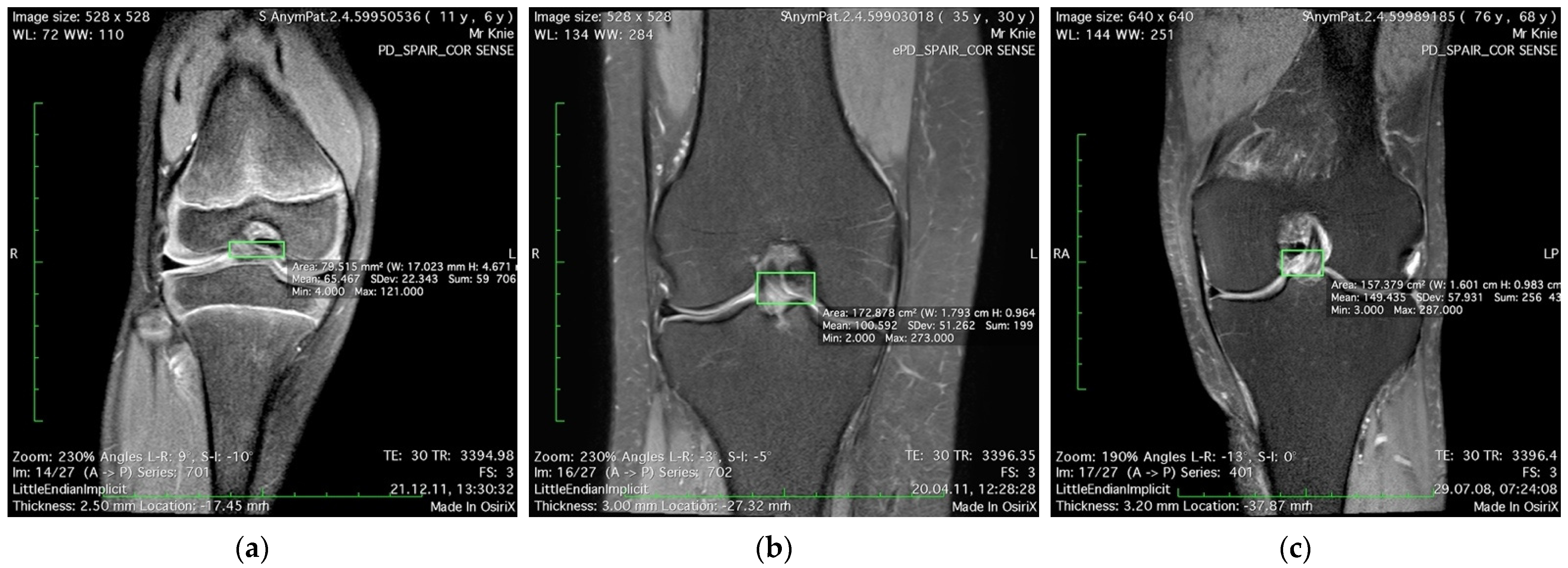
2.2. MRI Evaluation
2.3. Statistics
3. Results
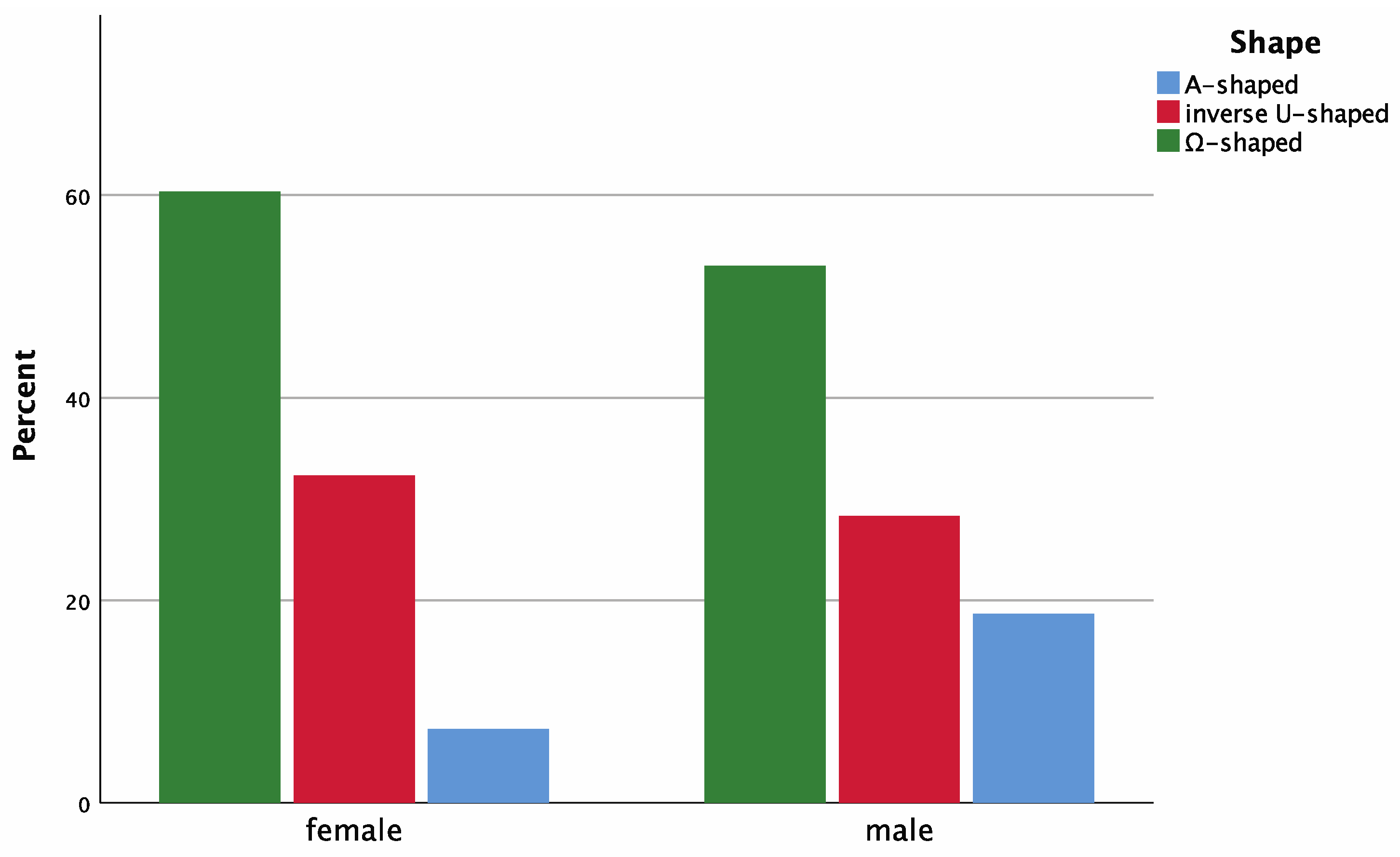
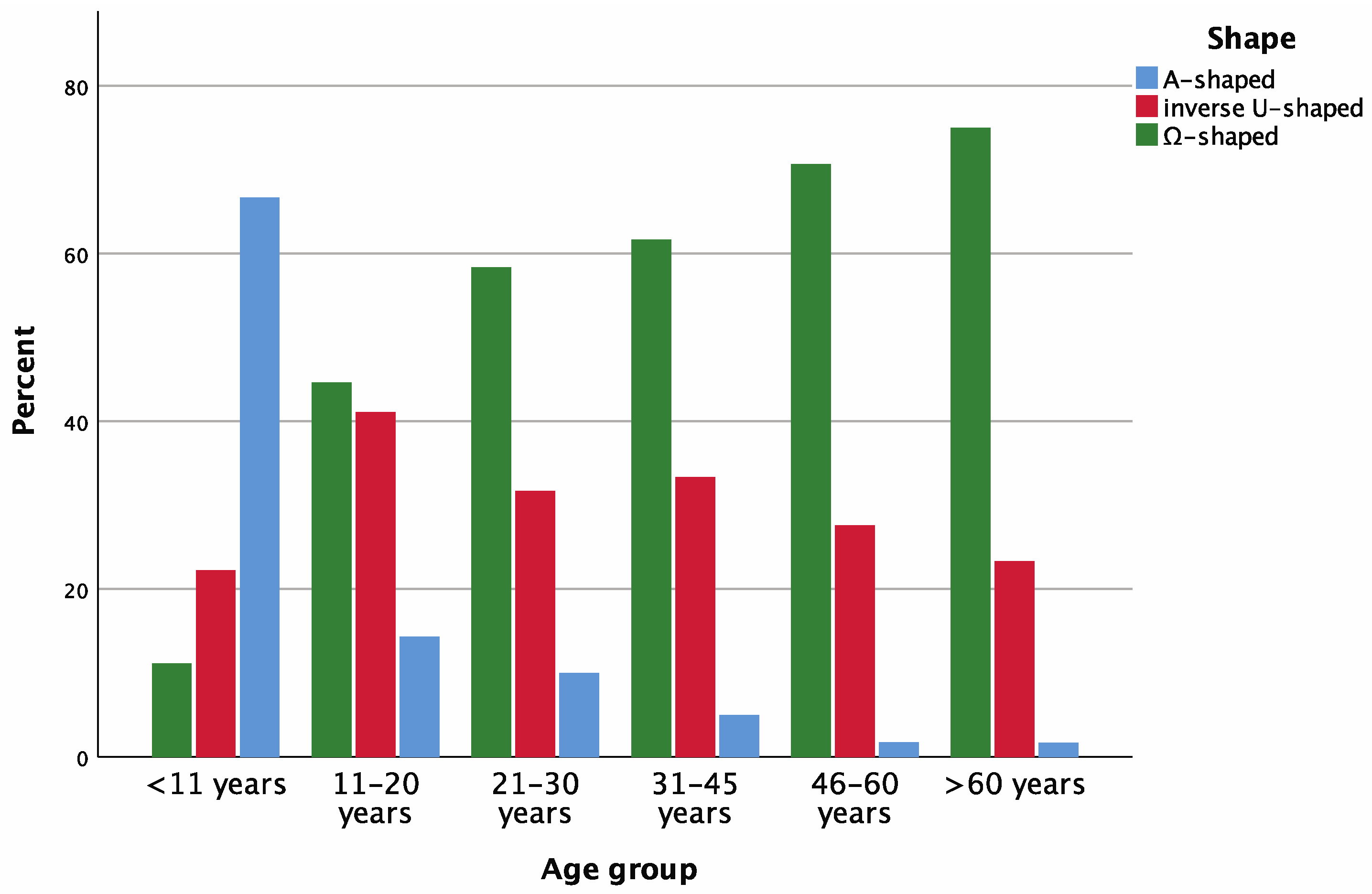
3.1. Semi-quantitative Evaluation (SqE)
3.2. Assisted Semi-Quantitative Evaluation (aSqE)
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Shelbourne, K.D.; Facibene, W.A.; Hunt, J.J. Radiographic and intraoperative intercondylar notch width measurements in men and women with unilateral and bilateral anterior cruciate ligament tears. Knee Surg. Sports Traumatol. Arthrosc. 1997, 5, 229–233. [Google Scholar] [CrossRef] [PubMed]
- Hoteya, K.; Kato, Y.; Motojima, S.; Ingham, S.J.; Horaguchi, T.; Saito, A.; Tokuhashi, Y. Association between intercondylar notch narrowing and bilateral anterior cruciate ligament injuries in athletes. Arch. Orthop. Trauma. Surg. 2011, 131, 371–376. [Google Scholar] [CrossRef] [PubMed]
- Ireland, M.L.; Ballantyne, B.T.; Little, K.; McClay, I.S. A radiographic analysis of the relationship between the size and shape of the intercondylar notch and anterior cruciate ligament injury. Knee Surg. Sports Traumatol. Arthrosc. 2001, 9, 200–205. [Google Scholar] [CrossRef] [PubMed]
- Bouras, T.; Fennema, P.; Burke, S.; Bosman, H. Stenotic intercondylar notch type is correlated with anterior cruciate ligament injury in female patients using magnetic resonance imaging. Knee Surg. Sports Traumatol. Arthrosc. 2018, 26, 1252–1257. [Google Scholar] [CrossRef] [PubMed]
- Cha, J.H.; Lee, S.H.; Shin, M.J.; Choi, B.K.; Bin, S.I. Relationship between mucoid hypertrophy of the anterior cruciate ligament (ACL) and morphologic change of the intercondylar notch: MRI and arthroscopy correlation. Skelet. Radiol. 2008, 37, 821–826. [Google Scholar] [CrossRef] [PubMed]
- Hernigou, P.; Garabedian, J. Intercondylar notch width and the risk for anterior cruciate ligament rupture in the osteoarthritic knee: Evaluation by plain radiography and CT scan. Knee 2002, 9, 313–316. [Google Scholar] [CrossRef]
- Levins, J.G.; Argentieri, E.C.; Sturnick, D.R.; Gardner-Morse, M.; Vacek, P.M.; Tourville, T.W.; Johnson, R.J.; Slauterbeck, J.R.; Beynnon, B.D. Geometric Characteristics of the Knee Are Associated With a Noncontact ACL Injury to the Contralateral Knee After Unilateral ACL Injury in Young Female Athletes. Am. J. Sports Med. 2017, 45, 3223–3232. [Google Scholar] [CrossRef]
- LaPrade, R.F.; Burnett, Q.M. Femoral intercondylar notch stenosis and correlation to anterior cruciate ligament injuries. A prospective study. Am. J. Sports Med. 1994, 22, 198–203. [Google Scholar] [CrossRef] [PubMed]
- Sonnery-Cottet, B.; Archbold, P.; Cucurulo, T.; Fayard, J.M.; Bortolletto, J.; Thaunat, M.; Prost, T.; Chambat, P. The influence of the tibial slope and the size of the intercondylar notch on rupture of the anterior cruciate ligament. J. Bone Joint Surg. Br. 2011, 93, 1475–1478. [Google Scholar] [CrossRef] [PubMed]
- Whitney, D.C.; Sturnick, D.; Vacek, P.M.; DeSarno, M.J.; Gardner-Morse, M.; Tourville, T.W.; Smith, H.C.; Slauterbeck, J.R.; Johnson, R.J.; Shultz, S.J.; et al. Relationship Between the Risk of Suffering a First-Time Noncontact ACL Injury and Geometry of the Femoral Notch and ACL: A Prospective Cohort Study With a Nested Case-Control. Analysis. Am. J. Sports Med. 2014, 42, 1796–1805. [Google Scholar] [CrossRef] [PubMed]
- Oshima, T.; Putnis, S.; Grasso, S.; Parker, D.A. The space available for the anterior cruciate ligament in the intercondylar notch is less in patients with ACL injury. Knee Surg. Sports Traumatol. Arthrosc. 2020, 28, 2105–2115. [Google Scholar] [CrossRef] [PubMed]
- Hirtler, L.; Röhrich, S.; Kainberger, F. The Femoral Intercondylar Notch During Life: An Anatomic Redefinition With Patterns Predisposing to Cruciate Ligament Impingement. AJR Am. J. Roentgenol. 2016, 207, 836–845. [Google Scholar] [CrossRef] [PubMed]
- Souryal, T.O.; Freeman, T.R. Intercondylar notch size and anterior cruciate ligament injuries in athletes. A prospective study. Am. J. Sports Med. 1993, 21, 535–539. [Google Scholar] [CrossRef] [PubMed]
- Al-Saeed, O.; Brown, M.; Athyal, R.; Sheikh, M. Association of femoral intercondylar notch morphology, width index and the risk of anterior cruciate ligament injury. Knee Surg. Sports Traumatol. Arthrosc. 2013, 21, 678–682. [Google Scholar] [CrossRef] [PubMed]
- Anderson, A.F.; Lipscomb, A.B.; Liudahl, K.J.; Addlestone, R.B. Analysis of the intercondylar notch by computed tomography. Am. J. Sports Med. 1987, 15, 547–552. [Google Scholar] [CrossRef] [PubMed]
- Keays, S.L.; Keays, R.; Newcombe, P.A. Femoral intercondylar notch width size: A comparison between siblings with and without anterior cruciate ligament injuries. Knee Surg. Sports Traumatol. Arthrosc. 2016, 24, 672–679. [Google Scholar] [CrossRef] [PubMed]
- Van Eck, C.F.; Martins, C.A.Q.; Vyas, S.M.; Celentano, U.; Van Dijk, C.N.; Fu, F.H. Femoral intercondylar notch shape and dimensions in ACL-injured patients. Knee Surg. Sports Traumatol. Arthrosc. 2010, 18, 1257–1262. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Eggerding, V.; Van Kuijk, K.S.R.; Van Meer, B.L.; Bierma-Zeinstra, S.M.A.; Van Arkel, E.R.A.; Reijman, M.; Waarsing, J.H.; Meuffels, D.E. Knee shape might predict clinical outcome after an anterior cruciate ligament rupture. Bone Joint J. 2014, 96, 737–742. [Google Scholar] [CrossRef] [PubMed]
- Everhart, J.S.; Flanigan, D.C.; Chaudhari, A.M.W. Anteromedial ridging of the femoral intercondylar notch: An anatomic study of 170 archival skeletal specimens. Knee Surg. Sports Traumatol. Arthrosc. 2014, 22, 80–87. [Google Scholar] [CrossRef] [PubMed]
- Everhart, J.; Flanigan, D.C.; Simon, R.A.; Chaudhari, A.M. Association of noncontact anterior cruciate ligament injury with presence and thickness of a bony ridge on the anteromedial aspect of the femoral intercondylar notch. Am. J. Sports Med. 2010, 38, 1667–1673. [Google Scholar] [CrossRef]
- Zoetis, T.; Tassinari, M.S.; Bagi, C.; Walthall, K.; Hurtt, M.E. Species comparison of postnatal bone growth and development. Birth Defects Res. B Dev. Reprod. Toxicol. 2003, 68, 86–110. [Google Scholar] [CrossRef] [PubMed]
- Juul, A.; Teilmann, G.; Scheike, T.; Hertel, N.T.; Holm, K.; Laursen, E.M.; Main, K.M.; Skakkebaek, N.E. Pubertal development in Danish children: Comparison of recent European and US data. Int. J. Androl. 2006, 29, 247–255; discussion 286–290. [Google Scholar] [CrossRef] [PubMed]
- Ong, K.K.; Ahmed, M.L.; Dunger, D.B. Lessons from large population studies on timing and tempo of puberty (secular trends and relation to body size): The European trend. Mol. Cell Endocrinol. 2006, 254–255, 8–12. [Google Scholar] [CrossRef] [PubMed]
- Vandervoort, A.A. Aging of the human neuromuscular system. Muscle Nerve 2002, 25, 17–25. [Google Scholar] [CrossRef] [PubMed]
- Frost, H.M. On our age-related bone loss: Insights from a new paradigm. J. Bone Miner. Res. 1997, 12, 1539–1546. [Google Scholar] [CrossRef] [PubMed]
- Cline, M.G.; Meredith, E.K.; Boyer, J.T.; Burrows, B. Decline of height with age in adults in a general population sample: Estimating maximum height and distinguishing birth cohort effects from actual loss of stature with aging. Hum. Biol. 1989, 61, 415–425. [Google Scholar] [PubMed]
- Domzalski, M.; Grzelak, P.; Gabos, P. Risk factors for Anterior Cruciate Ligament injury in skeletally immature patients: Analysis of intercondylar notch width using Magnetic Resonance Imaging. Int. Ortho. 2010, 34, 703–707. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Davis, T.J.; Shelbourne, K.D.; Klootwyk, T.E. Correlation of the intercondylar notch width of the femur to the width of the anterior and posterior cruciate ligaments. Knee Surg. Sports Traumatol. Arthrosc. 1999, 7, 209–214. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.; Ma, Y.; Geng, B.; Tan, X.; Zhang, B.; Jayswal, C.K.; Khan, S.; Meng, H.; Ding, N.; Jiang, J.; et al. Intercondylar Notch Stenosis of Knee Osteoarthritis and Relationship between Stenosis and Osteoarthritis Complicated with Anterior Cruciate Ligament Injury: A Study in MRI. Medicine 2016, 95, e3439. [Google Scholar] [CrossRef] [PubMed]
- Swami, V.G.; Mabee, M.; Hui, C.; Jaremko, J.L. Three-dimensional intercondylar notch volumes in a skeletally immature pediatric population: A magnetic resonance imaging-based anatomic comparison of knees with torn and intact anterior cruciate ligaments. Arthroscopy 2013, 29, 1954–1962. [Google Scholar] [CrossRef]
- Cohen, J. A Coefficient of Agreement for Nominal Scales. Educ. Psychol. Meas. 2016, 20, 37–46. [Google Scholar] [CrossRef]
- Altman, D.G. Practical Statistics for Medical Research, 1st ed.; Chapman and Hall: London, UK, 1991; Volume 12, p. 611. [Google Scholar]
- Tanzer, M.; Lenczner, E. The relationship of intercondylar notch size and content to notchplasty requirement in anterior cruciate ligament surgery. Arthroscopy 1990, 6, 89–93. [Google Scholar] [CrossRef]
- Tillman, M.D.; Smith, K.R.; Bauer, A.J.; Cauraugh, J.H.; Falsetti, A.B.; Pattishall, J.L. Differences in three intercondylar notch geometry indices between males and females: A cadaver study. Knee 2002, 9, 41–46. [Google Scholar] [CrossRef]
- Shepstone, L. Shape of the intercondylar notch of the human femur: A comparison of osteoarthritic and non-osteoarthritic bones from a skeletal sample. Ann. Rheum. Dis. 2001, 60, 968–973. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kamei, G.; Adachi, N.; Nakamae, A.; Nakasa, T.; Shibuya, H.; Okuhara, A.; Niimoto, T.; Kazusa, H.; Ohkawa, S.; Takazawa, K.; et al. Characteristic shape of the lateral femoral condyle in patients with osteochondritis dissecans accompanied by a discoid lateral meniscus. J. Orthop. Sci. 2012, 17, 124–128. [Google Scholar] [CrossRef]
- Fung, D.T.; Hendrix, R.W.; Koh, J.; Zhang, L.-Q. ACL impingement prediction based on MRI scans of individual knees. Clin. Orthop. Relat. Res. 2007, 460, 210–218. [Google Scholar] [CrossRef] [PubMed]
- Fung, D.T.; Zhang, L.-Q. Modeling of ACL impingement against the intercondylar notch. Clin. Biomech. 2003, 18, 933–941. [Google Scholar] [CrossRef]
- Park, H.-S.; Ahn, C.; Fung, D.T.; Ren, Y.; Zhang, L.-Q. A knee-specific finite element analysis of the human anterior cruciate ligament impingement against the femoral intercondylar notch. J. Biomech. 2010, 43, 2039–2042. [Google Scholar] [CrossRef] [Green Version]
| Age Group (Years) | Side | Total | Notch Width (mm) | Shape | ||||
|---|---|---|---|---|---|---|---|---|
| Left | Right | NWp | NWj | A-Shape | Inverse U-Shape | Ω-Shape | ||
| <11 | 19 (52.8%) | 17 (47.2%) | 36 | 16.13 ± 2.68 | 17.70 ± 3.19 | 24 (66.7%) | 8 (22.2%) | 4 (11.1%) |
| 11–20 | 24 (42.9%) | 32 (57.1%) | 56 | 18.01 ± 2.55 | 17.17 ± 3.16 | 8 (14.3%) | 22 (41.1%) | 25 (44.6%) |
| 21–30 | 29 (48.3%) | 31 (51.7%) | 60 | 18.63 ± 2.69 | 17.43 ± 3.27 | 6 (10.0%) | 19 (31.7%) | 35 (58.3%) |
| 31–45 | 31 (51.7%) | 29 (48.3%) | 60 | 18.96 ± 3.10 | 17.15 ± 2.98 | 3 (5.0%) | 20 (33.3%) | 37 (61.7%) |
| 46–60 | 33 (56.9%) | 25 (43.1%) | 58 | 19.38 ± 2.90 | 17.36 ± 3.37 | 1 (1.7%) | 16 (27.6%) | 41 (70.7%) |
| >60 | 30 (50.0%) | 30 (50.0%) | 60 | 18.60 ± 2.36 | 16.61 ± 3.08 | 1 (1.7%) | 14 (23.3%) | 45 (75.0%) |
| Total | 166 | 164 | 330 | 18.45 ± 2.85 | 17.21 ± 3.17 | 43 (13.0%) | 100 (30.3%) | 187 (56.7%) |
| Shape | Control | SqE | aSqE | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | Correct | Mistaken As | Total | Correct | Mistaken As | ||||||
| A-Shape | Inverse U-Shape | Ω-Shape | A-Shape | Inverse U-Shape | Ω-Shape | ||||||
| A-shape | 43 | 44 | 25 | - | 6 | 12 | 44 | 41 | 0 | 3 | 0 |
| Inverse U-shape | 100 | 37 | 19 | 12 | - | 69 | 103 | 94 | 4 | 0 | 5 |
| Ω-shape | 187 | 249 | 165 | 6 | 12 | - | 183 | 180 | 0 | 3 | 0 |
| Total | 330 | 330 | 209 * | 18 | 18 | 81 | 330 | 315 * | 4 | 6 | 3 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hirtler, L.; Tschematschar, K.; Kainberger, F.; Röhrich, S. Applicability of Semi-Quantitative Evaluation of the Intercondylar Notch. Appl. Sci. 2021, 11, 5921. https://doi.org/10.3390/app11135921
Hirtler L, Tschematschar K, Kainberger F, Röhrich S. Applicability of Semi-Quantitative Evaluation of the Intercondylar Notch. Applied Sciences. 2021; 11(13):5921. https://doi.org/10.3390/app11135921
Chicago/Turabian StyleHirtler, Lena, Katrin Tschematschar, Franz Kainberger, and Sebastian Röhrich. 2021. "Applicability of Semi-Quantitative Evaluation of the Intercondylar Notch" Applied Sciences 11, no. 13: 5921. https://doi.org/10.3390/app11135921






