Effectiveness of Exercise and Manual Therapy as Treatment for Patients with Migraine, Tension-Type Headache or Cervicogenic Headache: An Umbrella and Mapping Review with Meta-Meta-Analysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Review Inclusion Criteria
2.1.1. Population
2.1.2. Intervention and Control
2.1.3. Outcomes
2.1.4. Study Design
2.2. Search Strategy
2.3. Selection Criteria and Data Extraction
2.4. Methodology Quality Assessment
2.5. Risk of Bias Assessment
2.6. Evidence Map
- Number of studies (figure size): The size of each figure is directly proportional to the number of original studies included in each of the meta-analyses.
- Study Population (bubble colour) and type of intervention (symbol): The type of population evaluated in each study is represented by a colour (green: migraine; blue: TTH; yellow: CGH). The type of therapeutic intervention determined each symbol inside the bubble (x: manual therapy; −: therapeutic exercise; +: mixed intervention). In addition, in the second mapping, the plot of the figure represents the study variable.
- x-Axis: In the descriptive mapping, each of the study variables is represented on the x-axis. In the second mapping, each of the reviews was classified according to the size effect as described by Hopkins (Hopkins et al., 2009). The categorisation of the effect size is described in the section Data synthesis and analysis.
- y-Axis: The descriptive mapping represents the quality of each of the reviews on the y-axis according to the AMSTAR scale. In the second mapping, the reviews were sorted into the following 4 categories according to the Physical Activity Guidelines Advisory Committee (PAGAC): strong, moderate, limited or not assignable.
2.7. Qualitative Analysis
2.8. Data Synthesis and Analysis
3. Results
3.1. Characteristics of the Included Systematic Reviews
3.2. Results of the Methodology Quality Analysis
3.3. Results of the Risk of Bias Analysis
3.4. Evidence Map
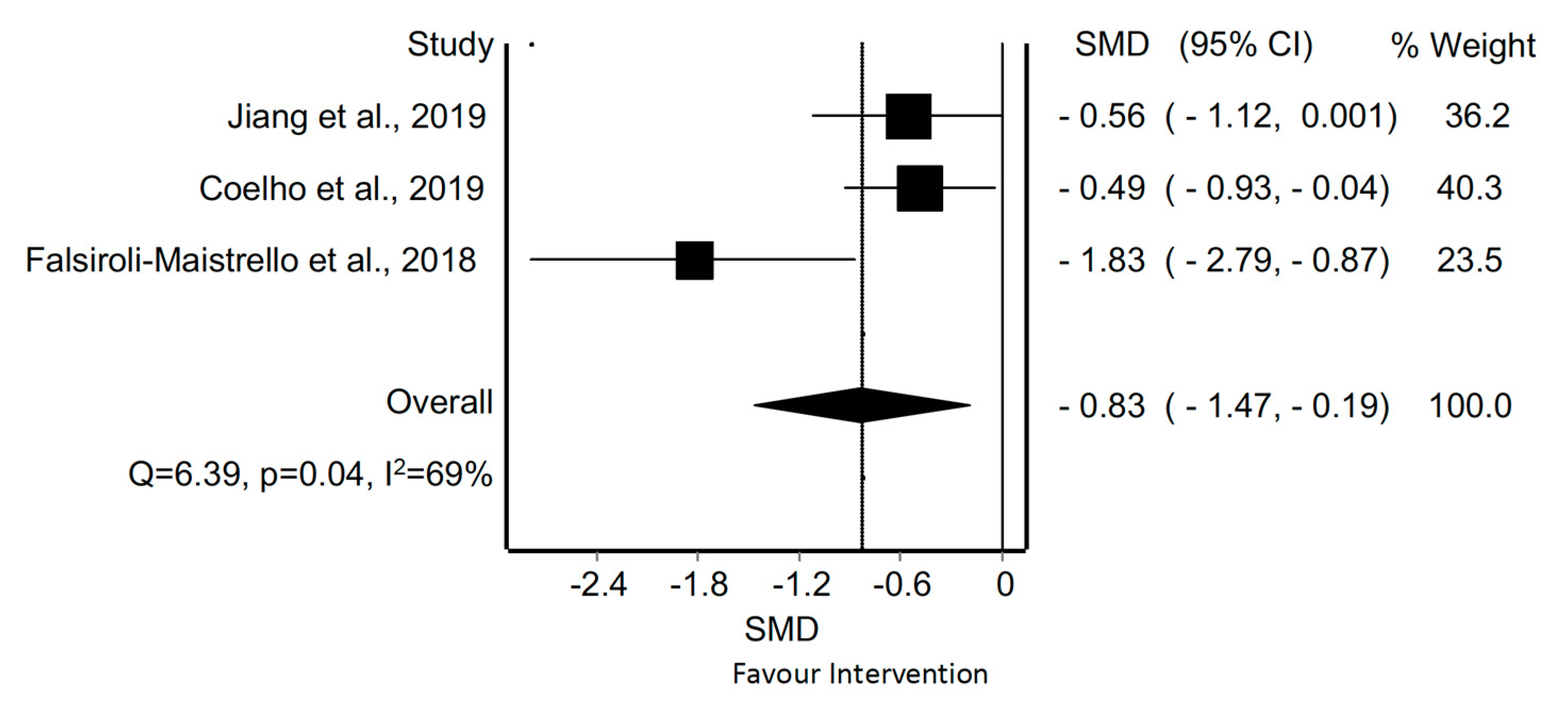
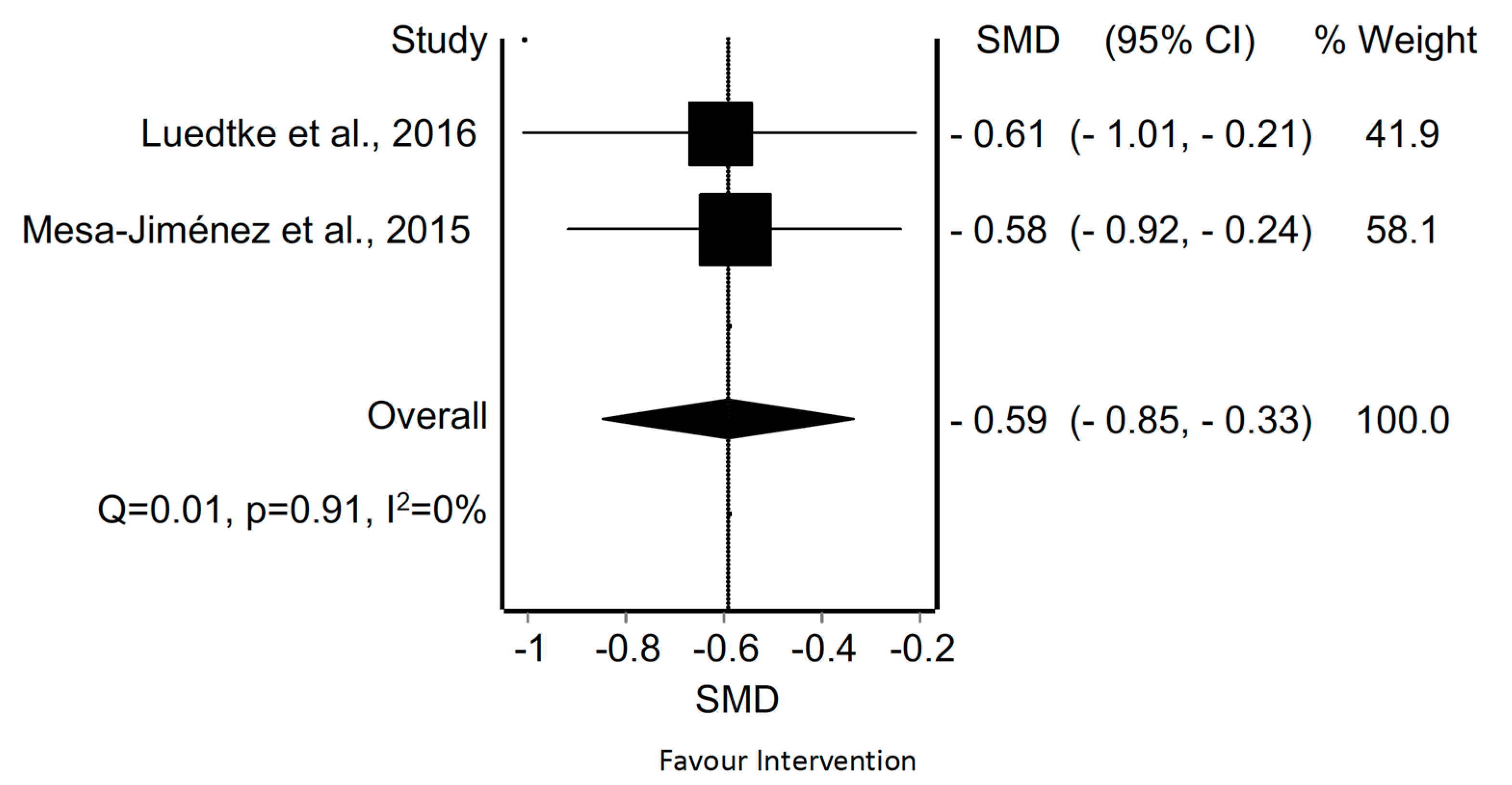
3.5. Pain Intensity
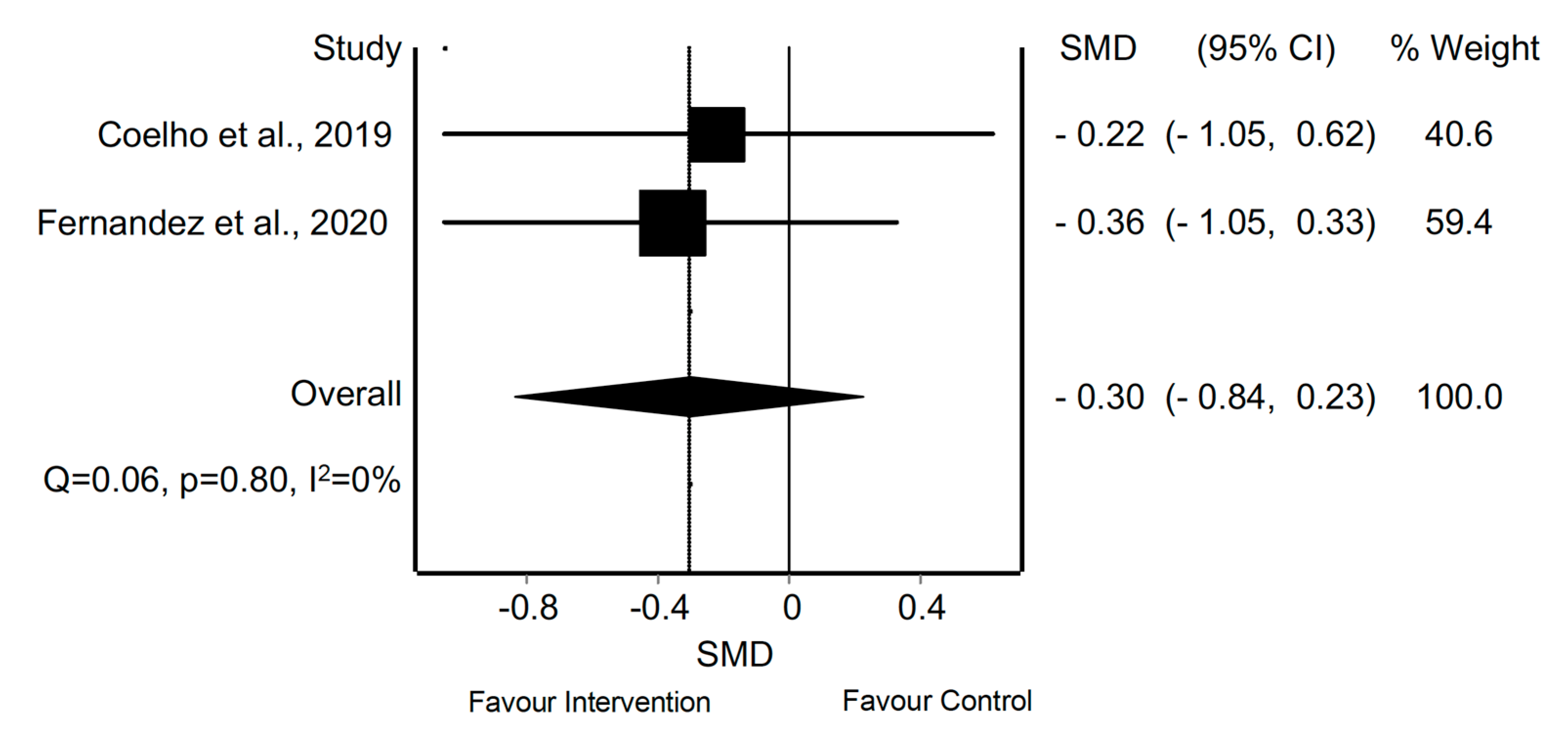
3.6. Frequency of Symptoms
3.7. Quality of Life
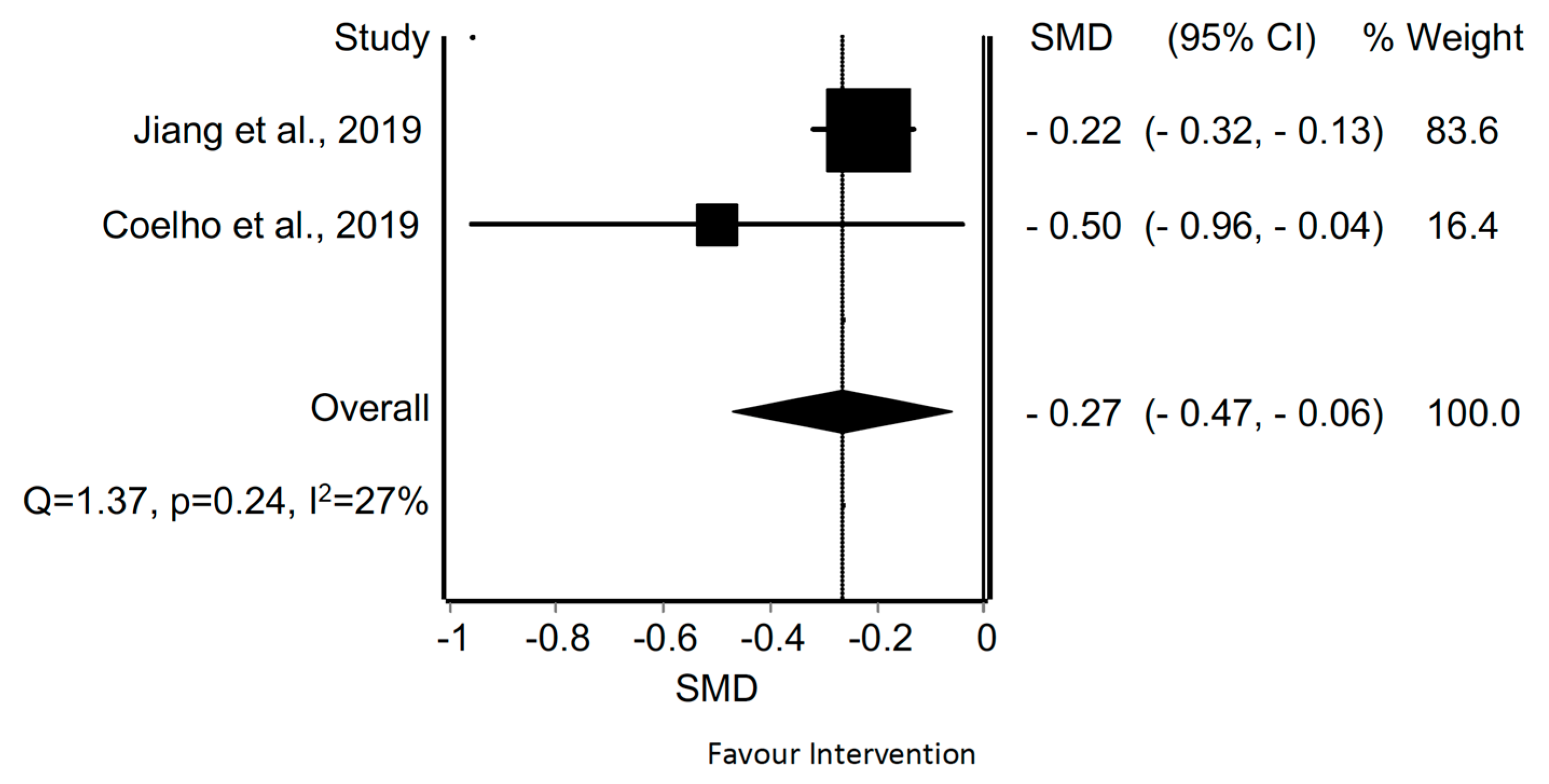
3.8. Disbility
4. Discussion
4.1. Migraine
4.2. Tension-Type Headache
4.3. Cervicogenic Headache
4.4. Clinical Implications
4.5. Research Implications
4.6. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- International Headache Society (IHS). Headache Classification Committee of the International Headache Society (IHS). The International Classification of Headache Disorders, 3rd ed. Cephalalgia 2018, 38, 285. [Google Scholar] [CrossRef]
- Stovner, L.J.; Nichols, E.; Steiner, T.J.; Abd-Allah, F.; Abdelalim, A.; Al-Raddadi, R.M.; Ansha, M.G.; Barac, A.; Bensenor, I.M.; Doan, L.P.; et al. Global, Regional, and National Burden of Migraine and Tension-Type Headache, 1990–2016: A Systematic Analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2018, 17, 954–976. [Google Scholar] [CrossRef] [Green Version]
- Bendtsen, L.; Evers, S.; Linde, M.; Mitsikostas, D.D.; Sandrini, G.; Schoenen, J. EFNS Guideline on the Treatment of Tension-Type Headache—Report of an EFNS Task Force. Eur. J. Neurol. 2010, 17, 1318–1325. [Google Scholar] [CrossRef] [PubMed]
- Kristoffersen, E.S.; Grande, R.B.; Aaseth, K.; Lundqvist, C.; Russell, M.B. Management of Primary Chronic Headache in the General Population: The Akershus Study of Chronic Headache. J. Headache Pain 2012, 13, 113–120. [Google Scholar] [CrossRef] [Green Version]
- Russell, M.B. Epidemiology and Management of Medication-Overuse Headache in the General Population. Neurol. Sci. 2019, 40, 23–26. [Google Scholar] [CrossRef]
- Volcy-Gómez, M. The Impact of Migraine and Other Primary Headaches on the Health System and in Social and Economic Terms. Rev. Neurol. 2006, 43, 228–235. [Google Scholar] [CrossRef] [PubMed]
- Gil-Martínez, A.; Kindelan-Calvo, P.; Agudo-Carmona, D.; Muñoz-Plata, R.; López-de-Uralde-Villanueva, I.; La Touche, R. Therapeutic Exercise as Treatment for Migraine and Tension-Type Headaches: A Systematic Review of Randomised Clinical Trials. Rev. Neurol. 2013, 57, 433–443. [Google Scholar] [CrossRef] [Green Version]
- La Touche, R.; Fernández Pérez, J.J.; Proy Acosta, A.; González Campodónico, L.; Martínez García, S.; Adraos Juárez, D.; Serrano García, B.; Angulo-Díaz-Parreño, S.; Cuenca-Martínez, F.; Suso-Martí, L.; et al. Is Aerobic Exercise Helpful in Patients with Migraine? A Systematic Review and Meta-analysis. Scand. J. Med. Sci. Sports 2020, 30, 965–982. [Google Scholar] [CrossRef]
- Biondi, D.M. Physical Treatments for Headeache: A Structured Review. Headache 2005, 45, 738–746. [Google Scholar] [CrossRef] [PubMed]
- Bialosky, J.E.; Beneciuk, J.M.; Bishop, M.D.; Coronado, R.A.; Penza, C.W.; Simon, C.B.; George, S.Z. Unraveling the Mechanisms of Manual Therapy: Modeling an Approach. J. Orthop. Sports Phys. Ther. 2018, 48, 8–18. [Google Scholar] [CrossRef]
- Bougioukas, K.I.; Liakos, A.; Tsapas, A.; Ntzani, E.; Haidich, A.B. Preferred Reporting Items for Overviews of Systematic Reviews Including Harms Checklist: A Pilot Tool to Be Used for Balanced Reporting of Benefits and Harms. J. Clin. Epidemiol. 2018, 93, 9–24. [Google Scholar] [CrossRef] [PubMed]
- Stone, P. Popping the (PICO) Question in Research and Evidence-Based Practice. Appl. Nurs. Res. 2002, 15, 197–198. [Google Scholar] [CrossRef]
- Moher, D.; Pham, B.; Jones, A.; Cook, D.J.; Jadad, A.R.; Moher, M.; Tugwell, P.; Klassen, T.P. Does Quality of Reports of Randomised Trials Affect Estimates of Intervention Efficacy Reported in Meta-Analyses? Lancet 1998, 352, 609–613. [Google Scholar] [CrossRef]
- Furlan, A.D.; Pennick, V.; Bombardier, C.; Van Tulder, M. Updated Method Guidelines for Systematic Reviews in the Cochrane Back Review Group. Spine 2009, 34, 1929–1941. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.; Welch, V.; Collaboration, C. Cochrane Handbook for Systematic Reviews of Interventions; Version 5.1.0; Wiley-Blackwell: Chichester, UK, 2008. [Google Scholar]
- Barton, C.J.; Webster, K.E.; Menz, H.B. Evaluation of the Scope and Quality of Systematic Reviews on Nonpharmacological Conservative Treatment for Patellofemoral Pain Syndrome. J. Orthop. Sports Phys. Ther. 2008, 38, 529–541. [Google Scholar] [CrossRef] [PubMed]
- McHugh, M.L. Interrater Reliability: The Kappa Statistic. Biochem. Med. 2012, 22, 276–282. [Google Scholar] [CrossRef]
- Whiting, P.; Savović, J.; Higgins, J.P.T.; Caldwell, D.M.; Reeves, B.C.; Shea, B.; Davies, P.; Kleijnen, J.; Churchill, R. ROBIS: A New Tool to Assess Risk of Bias in Systematic Reviews Was Developed. J. Clin. Epidemiol. 2016, 69, 225–234. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Torres, A.; Tennant, B.; Ribeiro-Lucas, I.; Vaux-Bjerke, A.; Piercy, K.; Bloodgood, B. Umbrella and Systematic Review Methodology to Support the 2018 Physical Activity Guidelines Advisory Committee. J. Phys. Act. Health 2018, 15, 805–810. [Google Scholar] [CrossRef]
- Barendregt, J.J.; Doi, S.A.; Lee, Y.Y.; Norman, R.E.; Vos, T. Meta-Analysis of Prevalence. J. Epidemiol Community Health 2013, 67, 974–978. [Google Scholar] [CrossRef]
- Barendregt, J.J.; Doi, S.A. MetaXL User Guide; Version 5.3; EpiGear International Pty Ltd.: Queensland, Australia, 2016. [Google Scholar]
- Lewis, S.; Clarke, M. Forest Plots: Trying to See the Wood and the Trees. Br. Med. J. 2001, 322, 1479–1480. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hedges, L.V. Estimation of Effect Size from a Series of Independent Experiments. Psychol. Bull. 1982, 92, 490–499. [Google Scholar] [CrossRef]
- Hopkins, W.; Marshall, S.; Batterham, A.; Hanin, J. Progressive Statistics for Studies in Sports Medicine and Exercise Science. Med. Sci. Sports Exerc. 2009, 41, 3–12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Suurmond, R.; van Rhee, H.; Hak, T. Introduction, Comparison, and Validation of Meta-Essentials: A Free and Simple Tool for Meta-Analysis. Res. Synth. Methods 2017, 8, 537–553. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Higgins, J.P.; Thompson, S.G.; Deeks, J.J.; Altman, D.G. Measuring Inconsistency in Meta-Analyses. Br. Med. J. 2003, 327, 557–560. [Google Scholar] [CrossRef] [Green Version]
- Huedo-Medina, T.B.; Sánchez-Meca, J.; Marín-Martínez, F.; Botella, J. Assessing Heterogeneity in Meta-Analysis: Q Statistic or I2 Index? Psychol. Methods 2006, 11, 193–206. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- DerSimonian, R.; Laird, N. Meta-Analysis in Clinical Trials. Control. Clin. Trials 1986, 7, 177–188. [Google Scholar] [CrossRef]
- Machado-Oliveira, L.; da Silva Gauto, Y.O.; de Santana Neto, F.J.; da Silva, M.G.; Germano-Soares, A.H.; Diniz, P.R.B. Effects of Different Exercise Intensities on Headache: A Systematic Review. Am. J. Phys. Med. Rehabil. 2020, 99, 390–396. [Google Scholar] [CrossRef]
- Chaibi, A.; Russell, M.B. Manual Therapies for Primary Chronic Headaches: A Systematic Review of Randomized Controlled Trials. J. Headache Pain 2014, 15, 67. [Google Scholar] [CrossRef] [Green Version]
- Racicki, S.; Gerwin, S.; DiClaudio, S.; Reinmann, S.; Donaldson, M. Conservative Physical Therapy Management for the Treatment of Cervicogenic Headache: A Systematic Review. J. Man. Manip. Ther. 2013, 21, 113–124. [Google Scholar] [CrossRef] [Green Version]
- Fernández-De-Las-Peñas, C.; Alonso-Blanco, C.; Cuadrado, M.L.; Miangolarra, J.C.; Barriga, F.J.; Pareja, J.A. Are Manual Therapies Effective in Reducing Pain from Tension-Type Headache?A Systematic Review. Clin. J. Pain 2006, 22, 278–285. [Google Scholar] [CrossRef]
- Bronfort, G.; Assendelft, W.J.; Evans, R.; Haas, M.; Bouter, L. Efficacy of Spinal Manipulation for Chronic Headache: A Systematic Review. J. Manip. Physiol. Ther. 2001, 24, 457–466. [Google Scholar] [CrossRef] [Green Version]
- Cumplido-Trasmonte, C.; Fernández-González, P.; Alguacil-Diego, I.M.; Molina-Rueda, F. Terapia Manual En Adultos Con Cefalea Tensional: Revisión Sistemática. Neurologia 2018. [Google Scholar] [CrossRef] [PubMed]
- Brønfort, G.; Haas, M.; Evans, R.L.; Goldsmith, C.H.; Assendelft, W.J.; Bouter, L.M. Non-Invasive Physical Treatments for Chronic/Recurrent Headache. Cochrane Database Syst. Rev. 2009, 2017. [Google Scholar] [CrossRef] [Green Version]
- Fernández-de-las-Peñas, C.; Alonso-Blanco, C.; Cuadrado, M.L.; Pareja, J.A. Spinal Manipulative Therapy in the Management of Cervicogenic Headache. Headache J. Head Face Pain 2005, 45, 1260–1263. [Google Scholar] [CrossRef] [PubMed]
- Maistrello, L.F.; Rafanelli, M.; Turolla, A. Manual Therapy and Quality of Life in People with Headache: Systematic Review and Meta-Analysis of Randomized Controlled Trials. Curr. Pain Headache Rep. 2019, 23, 1–14. [Google Scholar] [CrossRef]
- Jiang, W.; Li, Z.; Wei, N.; Chang, W.; Chen, W.; Sui, H.J. Effectiveness of Physical Therapy on the Suboccipital Area of Patients with Tension-Type Headache. Medicine 2019, 98, e15487. [Google Scholar] [CrossRef] [PubMed]
- Lemmens, J.; De Pauw, J.; Van Soom, T.; Michiels, S.; Versijpt, J.; Van Breda, E.; Castien, R.; De Hertogh, W. The Effect of Aerobic Exercise on the Number of Migraine Days, Duration and Pain Intensity in Migraine: A Systematic Literature Review and Meta-Analysis. J. Headache Pain 2019, 20, 16. [Google Scholar] [CrossRef] [PubMed]
- Falsiroli Maistrello, L.; Geri, T.; Gianola, S.; Zaninetti, M.; Testa, M. Effectiveness of Trigger Point Manual Treatment on the Frequency, Intensity, and Duration of Attacks in Primary Headaches: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Front. Neurol. 2018, 9, 254. [Google Scholar] [CrossRef] [Green Version]
- Luedtke, K.; Allers, A.; Schulte, L.H.; May, A. Efficacy of Interventions Used by Physiotherapists for Patients with Headache and Migraine—Systematic Review and Meta-Analysis. Cephalalgia 2016, 36, 474–492. [Google Scholar] [CrossRef]
- Mesa-Jiménez, J.A.; Lozano-López, C.; Angulo-Díaz-Parreño, S.; Rodríguez-Fernández, Á.L.; De-La-Hoz-Aizpurua, J.L.; Fernández-De-Las-Peñas, C. Multimodal Manual Therapy vs. Pharmacological Care for Management of Tension Type Headache: A Meta-Analysis of Randomized Trials. Cephalalgia 2015, 35, 1323–1332. [Google Scholar] [CrossRef] [PubMed]
- Coelho, M.; Ela, N.; Garvin, A.; Cox, C.; Sloan, W.; Palaima, M.; Cleland, J.A. The Effectiveness of Manipulation and Mobilization on Pain and Disability in Individuals with Cervicogenic and Tension-Type Headaches: A Systematic Review and Meta-Analysis. Phys. Ther. Rev. 2019, 24, 29–43. [Google Scholar] [CrossRef]
- Fernandez, M.; Moore, C.; Tan, J.; Lian, D.; Nguyen, J.; Bacon, A.; Christie, B.; Shen, I.; Waldie, T.; Simonet, D.; et al. Spinal Manipulation for the Management of Cervicogenic Headache: A Systematic Review and Meta-Analysis. Eur. J. Pain (UK) 2020, 24, 1687–1702. [Google Scholar] [CrossRef] [PubMed]
- González-Oria, C.; Belvís, R.; Cuadrado, M.L.; Díaz-Insa, S.; Guerrero-Peral, A.L.; Huerta, M.; Irimia, P.; Láinez, J.M.; Latorre, G.; Leira, R.; et al. Document of Revision and Updating of Medication Overuse Headache (MOH). Neurologia 2021, 36, 229–240. [Google Scholar] [CrossRef] [PubMed]
- Grazzi, L.; Toppo, C.; D’Amico, D.; Leonardi, M.; Martelletti, P.; Raggi, A.; Guastafierro, E. Non-Pharmacological Approaches to Headaches: Non-Invasive Neuromodulation, Nutraceuticals, and Behavioral Approaches. Int. J. Environ. Res. Public Health 2021, 18, 1503. [Google Scholar] [CrossRef]
- Ashina, M.; Buse, D.C.; Ashina, H.; Pozo-Rosich, P.; Peres, M.F.; Lee, M.J.; Terwindt, G.M.; Halker Singh, R.; Tassorelli, C.; Do, T.P.; et al. Migraine: Integrated Approaches to Clinical Management and Emerging Treatments. Lancet 2021. [Google Scholar] [CrossRef]
- Krøll, L.S.; Hammarlund, C.S.; Linde, M.; Gard, G.; Jensen, R.H. The Effects of Aerobic Exercise for Persons with Migraine and Co-Existing Tension-Type Headache and Neck Pain. A Randomized, Controlled, Clinical Trial. Cephalalgia 2018, 38, 1805–1816. [Google Scholar] [CrossRef]
- Song, T.J.; Chu, M.K. Exercise in Treatment of Migraine Including Chronic Migraine. Curr. Pain Headache Rep. 2021, 25, 14. [Google Scholar] [CrossRef]
- Hanssen, H.; Minghetti, A.; Magon, S.; Rossmeissl, A.; Rasenack, M.; Papadopoulou, A.; Klenk, C.; Faude, O.; Zahner, L.; Sprenger, T.; et al. Effects of Different Endurance Exercise Modalities on Migraine Days and Cerebrovascular Health in Episodic Migraineurs: A Randomized Controlled Trial. Scand. J. Med. Sci. Sports 2018, 28, 1103–1112. [Google Scholar] [CrossRef]
- Eslami, R.; Parnow, A.; Pairo, Z.; Nikolaidis, P.; Knechtle, B. The Effects of Two Different Intensities of Aerobic Training Protocols on Pain and Serum Neuro-Biomarkers in Women Migraineurs: A Randomized Controlled Trail. Eur. J. Appl. Physiol. 2021, 121, 609–620. [Google Scholar] [CrossRef] [PubMed]
- Benatto, M.T.; Bevilaqua-Grossi, D.; Carvalho, G.F.; Bragatto, M.M.; Pinheiro, C.F.; Lodovichi, S.S.; Dach, F.; Fernandez-de-Las-Penas, C.; Florencio, L.L. Kinesiophobia Is Associated with Migraine. Pain Med. 2019, 20, 846–851. [Google Scholar] [CrossRef] [PubMed]
- Amiri, M.; Jull, G.; Bullock-Saxton, J.; Darnell, R.; Lander, C. Cervical Musculoskeletal Impairment in Frequent Intermittent Headache. Part 2: Subjects with Concurrent Headache Types. Cephalalgia 2007, 27, 891–898. [Google Scholar] [CrossRef]
- Do, T.P.; Heldarskard, G.F.; Kolding, L.T.; Hvedstrup, J.; Schytz, H.W. Myofascial Trigger Points in Migraine and Tension-Type Headache. J. Headache Pain 2018, 19, 84. [Google Scholar] [CrossRef]
- Watson, D.H.; Drummond, P.D. Head Pain Referral during Examination of the Neck in Migraine and Tension-Type Headache. Headache 2012, 52, 1226–1235. [Google Scholar] [CrossRef] [PubMed]
- Pielsticker, A.; Haag, G.; Zaudig, M.; Lautenbacher, S. Impairment of Pain Inhibition in Chronic Tension-Type Headache. Pain 2005, 118, 215–223. [Google Scholar] [CrossRef]
- Varkey, E.; Hagen, K.; Zwart, J.A.; Linde, M. Physical Activity and Headache: Results from the Nord-Trøndelag Health Study (HUNT). Cephalalgia 2008, 28, 1292–1297. [Google Scholar] [CrossRef] [PubMed]
- Davenport, S.; Dickinson, A.; Minns Lowe, C. Therapy-Based Exercise from the Perspective of Adult Patients: A Qualitative Systematic Review Conducted Using an Ethnographic Approach. Clin. Rehabil. 2019, 33, 1963–1977. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Olesen, J.; Bes, A.; Kunkel, R.; Lance, J.W.; Nappi, G.; Pfaffenrath, V.; Rose, F.C.; Schoenberg, B.S.; Soyka, D.; Tfelt-Hansen, P.; et al. The International Classification of Headache Disorders, 3rd ed (Beta Version). Cephalalgia 2013, 33, 629–808. [Google Scholar] [CrossRef] [Green Version]
- Bogduk, N. Cervicogenic Headache: Anatomic Basis and Pathophysiologic Mechanisms. Curr. Pain Headache Rep. 2001, 5, 382–386. [Google Scholar] [CrossRef]
- Becker, W.J. Cervicogenic Headache: Evidence That the Neck Is a Pain Generator. Headache 2010, 50, 699–705. [Google Scholar] [CrossRef]
- Hall, T.M.; Robinson, K.W.; Fujinawa, O.; Akasaka, K.; Pyne, E.A. Intertester Reliability and Diagnostic Validity of the Cervical Flexion-Rotation Test. J. Manip. Physiol. Ther. 2008, 31, 293–300. [Google Scholar] [CrossRef]
- Zito, G.; Jull, G.; Story, I. Clinical Tests of Musculoskeletal Dysfunction in the Diagnosis of Cervicogenic Headache. Man. Ther. 2006, 11, 118–129. [Google Scholar] [CrossRef] [PubMed]
- Togha, M.; Bahrpeyma, F.; Jafari, M.; Nasiri, A. A Sonographic Comparison of the Effect of Dry Needling and Ischemic Compression on the Active Trigger Point of the Sternocleidomastoid Muscle Associated with Cervicogenic Headache: A Randomized Trial. J. Back Musculoskelet. Rehabil. 2020, 33, 749–759. [Google Scholar] [CrossRef]
- Haas, M.; Bronfort, G.; Evans, R.; Schulz, C.; Vavrek, D.; Takaki, L.; Hanson, L.; Leininger, B.; Neradilek, M.B. Dose-Response and Efficacy of Spinal Manipulation for Care of Cervicogenic Headache: A Dual-Center Randomized Controlled Trial. Spine J. 2018, 18, 1741–1754. [Google Scholar] [CrossRef] [PubMed]
- Wilhelm, M.P.; Donaldson, M.; Griswold, D.; Learman, K.E.; Garcia, A.N.; Learman, S.M.; Cleland, J.A. The Effects of Exercise Dosage on Neck-Related Pain and Disability: A Systematic Review with Meta-Analysis. J. Orthop. Sports Phys. Ther. 2020, 50, 607–621. [Google Scholar] [CrossRef] [PubMed]
- Ylinen, J.; Nikander, R.; Nykänen, M.; Kautiainen, H.; Häkkinen, A. Effect of Neck Exercises on Cervicogenic Headache: A Randomized Controlled Trial. J. Rehabil. Med. 2010, 42, 344–349. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Andersen, L.L.; Mortensen, O.S.; Zebis, M.K.; Jensen, R.H.; Poulsen, O.M. Effect of Brief Daily Exercise on Headache among Adults--Secondary Analysis of a Randomized Controlled Trial. Scand. J. Work Environ. Health 2011, 37, 547–550. [Google Scholar] [CrossRef] [PubMed] [Green Version]








| Study | No. and Type of Included Studies (Subjects) | Objectives | Population | Intervention | No. of Studies Included in Meta-Analysis (Subjects) | Outcome Measures | Results |
|---|---|---|---|---|---|---|---|
| La Touche et al., 2020 | 7 RCTs (n = 408) 3 CCTs (n = 76) | Evaluate the effects of AE on patients with MH regarding pain intensity, frequency of MH and quality of life | Population: patients older than 18 y diagnosed with MH with or without aura by the ICHD-I, II or III criteria Age (y): 19 to 50 Gender (F/M): 92.35%/7.65% Mean headache duration (y): NA | Intervention group: AE with other forms of exercise therapy and/or minimal usual care Comparison group: Maintenance of daily activity, relaxation or no treatment | Pain intensity | ||
| 5 (n = 166) | VAS | The meta-analysis showed statistically significant differences in the reduction of pain intensity by AE in patients with MH in the short-term (SMD = 1.25; 95% CI 0.47 to 2.04). | |||||
| Frequency of symptoms | |||||||
| 7 (n = 214) | Self-report headache diaries | AE intervention showed statistically significant differences in decreasing the frequency of symptoms in the short-term compared to control group (SMD = 0.76; 95% CI 0.32 to 1.20). | |||||
| Quality of life | |||||||
| 4 (n = 150) | Profil der Lebensqualitat chronisch Kranker, Well-BeingIndex, HIT-6 | The meta-analysis showed statistically significant differences in the increase in quality of life in the short-term for the Intervention group compared to the control group (SMD = 2.70; 95% CI 1.17 to 4.24). | |||||
| Machado-Oliveira et al., 2020 | 14 RCTs (n = 1988) 1 CCT (n = 16) 1 noncontrolled clinical trial (n = 52) | Investigate the effects of different exercise intensities on headache parameters | Population: adults older than 18 y diagnosed with MH or TTH by a neurologist and/or ICHD-I, II or III criteria Age (years): 18 to 55 Gender (F/M): 62%/38% Mean headache duration (y): 18.13 | Intervention group: AE or resistance exercise Comparison group: Usual care, medication, ergonomic and posture correction, health information or no treatment | Pain intensity | ||
| - | VAS, NPRS | AE or resistance exercise were effective interventions in reducing pain intensity in patients with MH, TTH or CGH. | |||||
| Frequency of symptoms | |||||||
| - | Self-report headache diaries | Interventions through AE or resistance exercise showed positive results on reduction of the frequency of headache. | |||||
| Falsiroli-Maistrello et al., 2019 | 10 RCTs (n = 728) | Evaluate the effectiveness of manual therapy on health-related quality of life in patients with TTH, MH or CGH | Population: patients older than 18 y diagnosed with MH with or without aura, TTH or CGH by the ICHD-III criteria Age (y): 18 to 65 Gender (F/M): 80%/20% Mean headache duration (y): 12.68 | Intervention group: Manual therapy Comparison group: Usual care, placebo or no treatment | Disability | ||
| 7 (n = 495) | HDI | The analysis showed a significant difference in favour of the Intervention group at the post-treatment (MD = −4.01; 95% CI −5.82 to −2.20) and at the follow-up (MD = −5.62; 95% CI −10.69 to −0.54). | |||||
| Quality of life | |||||||
| 9 (n = 721) | HIT-6 | The combined results between the subgroup of TTH and MH showed a significance difference in favour of the treatment at the post-treatment (MD = −3.67; 95% CI −5.71 to −1.63) and follow-up (MD = −2.47; 95% CI −3.27 to −1.68). | |||||
| Jiang et al., 2019 | 6 RCTs (n = 505) | Evaluate the effectiveness of physical therapy on the suboccipital area of patients with TTH | Population: patients older than 18 years with TTH diagnosed by the ICHD-II criteria Age (y): 18 to 65 Gender (F/M): 81.18%/18.82% Mean headache duration (y): 16.10 | Intervention group: Any direct manual treatment on the suboccipital area Comparison group: No treatment | Pain intensity | ||
| SIT vs. Control 3 (n = 122) OAA vs. Control 3 (n = 126) SIT + OAA vs. Control 3 (n = 122) | VAS | The meta-analysis did not show significant difference at 4 weeks post-treatment but did at 8 weeks for the SIT group (MD = 1.02; 95% CI 1.77 to 0.27). For the OAA group, the meta-analysis showed a significant difference at 4 weeks post-treatment (MD = 0.98; 95% CI 1.83 to 0.12) but no effect at 8 weeks. Finally, the SIT + OAA group showed a decrease in VAS score at 4 weeks (MD = 1.38; 95% CI 2.21 to 0.56) and 8 weeks (MD = 1.29; 95% CI 2.46 to 0.13). | |||||
| Disability | |||||||
| 2 (n = 182) | HDI | The meta-analysis showed that patients treated with SIT + OAA had positive results (MD = −2.66; 95% CI −4.58 to −0.75). | |||||
| Lemmens et al., 2019 | 5 RCTs (n = 324) 1 CCT (n = 16) | Investigate the effect of AE on frequency and pain intensity in patients with MH | Population: patients with MH with or without aura classified by the ICHD-II criteria Age (y): 18 to 65 Gender (F/M): 88%/12% Mean headache duration (y): 19.10 | Intervention group: AE Comparison group: Usual care, maintenance of daily physical activity, medication, health information or no treatment | Pain intensity | ||
| - | VAS | Studies reported a low quality of evidence for the reduction of pain intensity by an intervention based on AE in patients with MH. | |||||
| Frequency of symptoms | |||||||
| 4 (n = 176) | Self-report headache diaries | The meta-analysis showed a mean reduction in the number of MH days per month, favouring the AE group (MD = −0.61; 95% CI −1.14 to −0.09). | |||||
| Falsiroli-Maistrello et al., 2018 | 7 RCTs (n = 390) | Establish the effectiveness of manual trigger point treatment compared to minimal active or no active interventions in terms of frequency and intensity in patients with primary headache | Population: adults older than 18 y with MH or TTH diagnosed by ICHD-III criteria Age (y): 12 to 60 Gender (F/M): 76.15%/23.85% Mean headache duration (y): 9.20 | Intervention group: Any direct or indirect manual treatment targeting trigger point Comparison group: Sham treatment, medication or no treatment | Pain intensity | ||
| TTH and MH: 5 (n = 208) MH: 2 (n = 88) TTH: 4 (n = 168) | VAS, Numeric Pain Index | Combined MH and TTH results showed statistically significant difference in favouring the Intervention group (MD = −12.93; 95% CI −18.70 to −7.16). Sub-analyses presented a significant reduction of pain intensity in the Intervention group in patients with MH (MD = −13.60; 95% CI −19.54 to −7.66) and TTH (MD = −12.83; 95% CI −19.49 to −6.17). | |||||
| Frequency of symptoms | |||||||
| MH and TTH: 6 (n = 277) MH: 2 (n = 88) TTH: 4 (n = 189) | Self-report headache diaries | The analysis of the combined results indicated a statistically significant reduction after treatment, favouring the Intervention group (MD = −3.05; 95% CI −4.11 to −2.00). Sub-analyses showed a significant difference favouring the Intervention group for both MH (MD = −1.92; 95% CI −3.03 to −0.80) and TTH patients (MD = −3.50; 95% CI −4.91 to −2.09). | |||||
| Disability | |||||||
| - | HDI, HIT-6 | The results were controversial, showing significant differences in terms of reduction of disability in the Intervention group or in both groups in different studies. | |||||
| Quality of life | |||||||
| - | SF-36, McGill Pain Questionnaire | The results reported no significant differences between the intervention and Comparison group. | |||||
| Luedtke et al., 2016 | 26 RCTs (n = 3891) | Evaluate the effectiveness of manual therapy or exercise therapy on the intensity and frequency of MH, TTH and CGH | Population: adults with MH, TTH, CGH or mixed headache diagnosed by ICHD-I, II or III criteria Age (y): 18 to 70 Gender (F/M): 84.44%/15.56% Mean headache duration (y): 10.97 | Intervention group: AE, manual therapy or strength and endurance training Comparison group: Placebo, usual care, no treatment or any other active treatment | Pain intensity | ||
| MH: 5 (n = 254) TTH: 3 (n = 176) CGH: 6 (n = 388) | VAS, NPRS | The meta-analysis showed differences but not significant ones, in favour of the Intervention group in patients with MH (MD = −0.62; 95% CI −2.89 to 1.65). The differences were significant in the case of patients with TTH (MD = −1.11; 95% CI −1.64 to −0.57) or GCH (MD = −2.52; 95% CI −3.86 to −1.19). | |||||
| Frequency of symptoms | |||||||
| MH: 5 (n = 254) TTH: 2 (n = 94) CGH: 4 (n = 296) | Self-report headache diaries | The meta-analysis showed no significative differences in favour of the Intervention group in patients with MH (MD = −2.99; 95% CI −7.85 to 1.87) and TTH (MD = −7.58; 95% CI −18.13 to 2.97). There were significant differences in the case of CGH (MD = −1.34; 95% CI −1.40 to −1.28). | |||||
| Mesa-Jiménez et al., 2015 | 5 RCTs (n = 206) | Compare the efficacy of multimodal manual therapy versus pharmacological care in patients with TTH | Population: patients with TTH and chronic headache diagnosed by ICHD-II criteria Age (y): 18 to 83 Gender (F/M): 79.12%/20.88% Mean headache duration (y): 12.77 | Intervention group: Manual therapy in isolation or combined with exercises Comparison group: Medication | Pain intensity | ||
| 5 (n = 206) | VAS | The meta-analysis showed significant differences favouring manual therapy compared to medication after the intervention (WMD = −0.59; 95% CI −0.88 to −0.30). There were no significant differences in the long-term (WMD = −0.34; 95% CI −1.10 to 0.40). | |||||
| Frequency of symptoms | |||||||
| 4 (n = 178) | Self-report headache diaries | The meta-analysis showed that manual therapy was more effective than pharmacological medical care (WMD = −0.80; 95% CI –1.66 to −0.44) immediately after the intervention. | |||||
| Chaibi and Russell, 2014 | 6 RCTs (n = 288) | Assess the efficacy of manual therapy for chronic TTH | Population: patients older than 18 years with headache diagnosed by a neurologist or a physician employing ICHD-I, II or III criteria Age (y): 19 to 68 Gender (F/M): 78.82%/21.18% Mean headache duration (y): 13.26 | Intervention group: Manual therapy, ultrasound, TENS or exercises Comparison group: Usual care, detuned ultrasound, biofeedback treatment, spinal connective tissue manipulation or no treatment | Pain intensity | ||
| - | VAS, NPRS | The Intervention group had significantly more reduction in their headache intensity than the Comparison group after manual therapy intervention. | |||||
| Frequency of symptoms | |||||||
| - | Self-report headache diaries | There was a reduction of more than half in the frequency of symptoms post-treatment, and the results were maintained for more than six months.. | |||||
| Racicki et al., 2013 | 6 RCTs (n = 457) | Asses the effectiveness of conservative physical therapy management of CGH | Population: patients diagnosed with CGH by the ICHD-II criteria Age (y): 7 to 60 Gender (F/M): 67.20%/32.80% Mean headache duration (y): 6.03 | Intervention group: Manual therapy, therapeutic exercise or a combination of both Comparison group: Conservative treatment, placebo or no treatment | Pain intensity | ||
| - | VAS, MVK pain scale | The exercise intervention displayed statistically significant improvements at 7 weeks. The combination of exercise and manipulative therapy displayed statistically significant improvements. Those improvements persisted at the 12-month-follow up period. | |||||
| Frequency of symptoms | |||||||
| - | Self-report headache diaries | The exercise intervention displayed statistically significant improvements at 7 weeks. The combination of exercise and manipulative therapy displayed statistically significant improvements. Those improvements persisted at the 12-month-follow up period. | |||||
| Disability | |||||||
| - | MVK disability scale | With the exception of one study, all reported reduction in disability but there was conflicting evidence regarding the effects of manipulative therapy. | |||||
| Fernández-de-las-Peñas et al., 2006 | 5 RCTs (n = 321) 1 CCT (n = 20) | Establish whether manual therapies have specific efficacy in reducing pain from TTH | Population: patients with a diagnosis of episodic and chronic TTH employing ICDH-I or II criteria Age (y): 18 to 70 Gender (F/M): 47.50%/52.50% Mean headache duration (y): 11.71 | Intervention group: Different type of manual therapies Comparison group: Intervention plus other therapy, medication, placebo or no treatment | Pain intensity | ||
| - | VAS, NPRS, McGill Pain Questionnaire | The results were not generally consistent, as one trial reported positive results, another one reported neutral results, and the last one reported neutral results at the end of treatment and positive results at follow-up. | |||||
| Frequency of symptoms | |||||||
| - | Self-report headache diaries | The results found were controversial. While some studies found moderate effect in the reduction of this outcome, others revealed similar effects comparing the intervention and Comparison group. | |||||
| Disability | |||||||
| - | NDI, Headache index value | Only one study evaluated this outcome, showing positive results for the Intervention group with a moderate within-group effect size. | |||||
| Quality of life | |||||||
| - | SF-36 | There were no significant differences between groups at the end of the treatment. However, at 4 weeks follow up, SMT showed greater improvement than medication. | |||||
| Bronfort et al., 2001 | 9 RCTs (n = 683) | Assess the clinical efficacy of SMT for chronic headache (MH, TTH and CGH) | Population: patients diagnosed with MH, TTH or CGH by the ICHD-I criteria Age (y): 15 to 70 Gender (F/M): NA Mean headache duration (y): NA | Intervention group: SMT with or without other therapies Comparison group: Medication, other forms of manual therapy, placebo or no treatment | Pain intensity | ||
| - | VAS | In patients with TTH, it appears to be an advantage for SMT at 4 weeks post-treatment, but 6 weeks later, medication was better. In patients with MH, SMT group showed an advantage after 8 weeks of treatment. The combination of amitriptyline and SMT did not provide any advantage. Patients with CGH, who received SMT, reported approximately twice the reduction in headache intensity per episode than the massage group. | |||||
| Frequency of symptoms | |||||||
| - | Self-report headache diaries | In patients with CGH, the SMT group showed a decrease of 69% compared with a 47% decrease in the Comparison group at 8 weeks of treatment. | |||||
| Disability | |||||||
| - | HDI | There appears to be an advantage for chiropractic SMT after 8 weeks. | |||||
| Coelho et al., 2019 | 9 RCTs (n = 793) | Evaluate the effectiveness of mobilization and manipulation compared to other conservative treatments in patients with CGH and TTH | Population: adults older than 18 y diagnosed with CGH or TTH by the ICHD criteria Age (y): 18 to 70 Gender (F/M): 68.22%/31.78% Mean headache duration (y): NA | Intervention group: Different manual therapy techniques Comparison group: Conservative treatment | Pain intensity | ||
| TTH: 2 (n = 146) CGH: 3 (n = 291) | VAS, NPRS | There was significant differences favouring mobilization and manipulation over conservative care at 1–4 weeks in patients with TTH (SMD = 0.49; 95% CI 0.04 to 0.93). In the case of CGH patients, the difference was not significative at 1–3 months (SMD = 0.19; 95% CI −0.24 to 0.62). | |||||
| Frequency of symptoms | |||||||
| TTH: 2 (n = 146) CGH: 2 (n = 236) | Self-report headache diaries | There was no statistical difference between groups at 1–4 weeks in patients with TTH (SMD = 0.29; 95% CI −0.15 to 0.73) and at 1–3 months in patients with CGH (SMD = 0.22; 95% CI −0.62 to 1.05). | |||||
| Disability | |||||||
| TTH: 2 (n = 124) | NDI, SF-36, SF-12, HDI | There was a significant difference favouring the Intervention group in patients with TTH (SMD = 0.47; 95% CI 0.10 to 0.84). | |||||
| Cumplido-Trasmonte et al., 2018 | 10 RCTs (n = 731) | Determine the effectiveness of manual and non-invasive techniques in the treatment of patients with TTH | Population: patients older than 18 y diagnosed with TTH by the ICHD-II criteria Age (y): 18 to 70 Gender (F/M): 80.79%/19.21% Mean headache duration (y): NA | Intervention group: Manual therapy techniques Comparison group: Conservative treatment, usual care or sham massage or no treatment | Pain intensity | ||
| - | VAS, McGill Pain Questionnaire | After the intervention, all articles showed significant improvements over the Comparison group, and better improvements were found when the intervention combined different types of manual therapy. | |||||
| Frequency of symptoms | |||||||
| - | Self-report headache diaries | The results showed significant improvements for the Intervention group following the intervention. Regarding this group, better outcomes were found when different types of manual therapy were combined. | |||||
| Disability | |||||||
| - | HDI | All treatment groups showed significant improvements in the overall HDI count, revealing better improvements for the combination of cervical manipulation and suboccipital inhibition. | |||||
| Quality of life | |||||||
| - | SF-12, HIT-6, SF-36 | The studies that evaluated quality of life outcome showed inconclusive results. | |||||
| Gil-Martínez et al., 2013 | 10 RCTs (n = 2495) | Investigate the effectiveness of therapeutic exercise on MH and TTH | Population: patients older than 18 y diagnosed with MH or TTH by the ICHD-II criteria Age (y): 18 to 65 Gender (F/M): 83.57%/16.43% Mean headache duration (y): 19.87 | Intervention group: Therapeutic exercise in isolation or combined with other physical therapy treatments Comparison group: Conventional medical or physical therapy treatment, education or no treatment | Pain intensity | ||
| - | VAS, NPRS | There was evidence that therapeutic exercise on the craneocervical and shoulder region significantly improved, in the medium term, the intensity of pain. | |||||
| Frequency of symptoms | |||||||
| - | Self-report headache diaries | The results showed that therapeutic exercise on the craneocervical and shoulder region significantly improved the frequency of symptoms in the medium term, with a strong level of evidence. | |||||
| Disability | |||||||
| - | HDI | There was improvement in the disability outcome at medium term regarding therapeutic exercise on the craniocervical and shoulder region, with a strong level of evidence. | |||||
| Bronfort et al., 2009 | 22 RCTs (n = 2628) | Evaluate the effect of specific non-invasive physical treatments for chronic/recurrent headaches | Population: patients with chronic/recurrent headaches, including episodic and chronic TTH, CGH and MH, classified according to the ICHD-I criteria Age (y): 12 to 78 Gender (F/M): 72.77%/27.23% Mean headache duration (y): 8.75 | Intervention group: One or more types of non-invasive physical treatment Comparison group: Placebo, no treatment and any other type of active intervention | Pain intensity | ||
| - | VAS | The results showed greater reduction for the Intervention group in the short- and mid-term. | |||||
| Frequency of symptoms | |||||||
| - | Self-report headache diaries | The Intervention group performed significantly better in terms of headache frequency at 4 and 8 weeks. In addition, the results showed significantly more reduction in headache frequency at 12 months. | |||||
| Disability | |||||||
| - | HDI, NDI | Significantly fewer patients in the Intervention group experienced a 50% reduction in headache index score after 4 weeks. In addition, there was a significant difference in favor of the Intervention group after 3 weeks. | |||||
| Fernández-de-las-Peñas et al., 2005 | 2 RCTs (n = 253) | To assess the effectiveness of SMT in CGH | Population: patients older than 18 y, diagnosed with CGH based on ICHD-II criteria Age (y): 18 to 60 Gender (F/M): 67.19%/32.81% Mean headache duration (y): 6.07 | Intervention group: Exercise or manipulative therapy Comparison group: Massage and laser therapy or no treatment | Pain intensity | ||
| - | VAS | Manipulative therapy reported positive results on headache intensity compared to the control group. | |||||
| Frequency of symptoms | |||||||
| - | Self-report headache diaries | Only one study evaluated the frequency of symptoms, obtaining positive results for the Intervention group. | |||||
| Fernandez et al., 2020 | 6 RCTs (n = 549) | Review the evidence on SMT and manual therapy in the treatment of CGH | Population: Patients older than 18 y with CGH diagnosis based on ICHD-III criteria Age (y): 18 to 70 Gender (F/M): 58.83%/41.17% Mean headache duration (y): 7.3 | Intervention group: SMT Comparison group: Sham massage, exercise placebo or no treatment | Pain intensity | ||
| Short term: 6 (n = 364) Mid term: 3 (n = 157) Long term: 2 (n = 120) | VAS | Analysis revealed a significant small effect favouring SMT over other manual therapies for pain intensity in the short term (MD = −10.88; 95% CI −17.94 to −3.82). However, there was a non-significant difference between groups in the mid- and long-term (MD = −9.77; 95% CI −24.21 to 4.68 and MD = −0.76; 95% CI −5.89 to 4.37, respectively). | |||||
| Frequency of symptoms | |||||||
| Short term: 3 (n = 163) Mid term: 3 (n = 157) Long term: 2 (n = 120) | Self-report headache diaries | There was a significant small effect favouring SMT for frequency of symptoms in short- and mid-term (SMD = −0.35, 95% CI −0.66 to −0.04 and SMD = −0.32; 95% CI −0.63 to −0.00, respectively) but not in long term follow up (SMD = −0.378; 95% CI −0.84 to 0.10). | |||||
| Disability | |||||||
| Short term: 2 (n = 142) | MVK, NDI | There was a significant small effect favouring SMT for disability in the short term (MD = −13.31; 95% CI −18.07 to −8.56). It was not possible to assess disability in the mid- and long-term. | |||||
| Study | Group | Type of Intervention | Frequency and Intervention Time, Follow-Up | Session Duration | Intensity |
|---|---|---|---|---|---|
| La Touche et al., 2020 | Intervention group |
| 2 to 5 times/week 6 to 12 weeks | 40 to 60 min HIIT: Intervals of 4 min followed by an active rest period of 3 min | 70 to 95% of HRmax RPE (14–16) 45–60% VO2max |
| Comparison group |
| ||||
| Machado-Oliveira et al., 2020 | Intervention group | AE training:
| 2 to 5 times/week 6 to 20 weeks | 40 to 60 min HIIT: NA | 70 to 95% of HRmax RPE (13–16) 60 to 75% of VO2max |
Resistance training:
| 1 to 5 times/week 10 to 52 weeks | 2 to 30 min | 10 to 80% of maximal repetition load | ||
| Comparison group |
| ||||
| Falsiroli-Maistrello et al., 2019 | Intervention group |
| 4 to 14 times/week 4 weeks to 6 months Follow-up: 2 weeks to 9 months | 15 to 50 min | NR |
| Comparison group |
| ||||
| Jiang et al., 2019 | Intervention group |
| 1 time/week 4 weeks Follow up: 8 weeks | 20 min | NR |
| Comparison group |
| ||||
| Lemmens et al., 2019 | Intervention group |
| 2 to 5 times/week 10 to 16 weeks | 28 to 50 min | RPE (14–16) 70 to 95% of HRmax 60–75% VO2max |
| Comparison group |
| ||||
| Falsiroli-Maistrello et al., 2018 | Intervention group |
| 2 to 5 times/week 2 to 12 weeks Follow up: 2 weeks to 4 months | 15 to 100 min | NR |
| Comparison group |
| ||||
| Luedtke et al., 2016 | Intervention group |
| 1 to 12 times/week 1 week to 8 months | 2 to 50 min | NR |
| Comparison group |
| ||||
| Mesa-Jiménez et al., 2015 | Intervention group |
| 1 to 12 times/week 2 to 8 weeks | 10 to 60 min | NR |
| Comparison group |
| ||||
| Chaibi and Russell, 2014 | Intervention group |
| 2 to 12.8 times/week 8 days to 9 months | 30 to 40 min | NR |
| Comparison group |
| ||||
| Racicki et al., 2013 | Intervention group |
| 1 to 12 times/week 6 to 12 weeks Follow up: 4 weeks to 12 months | 10 to 30 min | NR |
| Comparison group |
| ||||
| Fernández-de-las-Peñas et al., 2006 | Intervention group |
| 2 to 5 times/week 4 to 6 weeks Follow-up: 4 weeks to 6 months | 10 to 30 min | NR |
| Comparison group |
| ||||
| Bronfort et al., 2001 | Intervention group |
| 1 to 12 times/week 1 to 8 weeks | 15 to 20 min | NR |
| Comparison group |
| ||||
| Coelho et al., 2019 | Intervention group |
| 2 to 4 times/week 4 to 6 weeks Follow-up: Immediately post-treatment to 12 months | 5 to 20 min | NR |
| Comparison group |
| ||||
| Cumplido-Trasmonte et al., 2018 | Intervention group |
| 1 to 5 times/week 4 to 6 weeks | 10 to 30 min | NR |
| Comparison group |
| ||||
| Gil-Martinez et al., 2013 | Intervention group |
| 1 to 12 times/week 6 to 12 weeks Follow up: Immediately post-treatment to 26 weeks | 15–60 min | RPE (14–16) |
| Comparison group |
| ||||
| Bronfort et al., 2009 | Intervention group |
| 2 to 5 times/week 1 to 12 weeks Follow up: Immediately post-treatment to 36 months | 5 min to 1 h | NR |
| Comparison group |
| ||||
| Fernández-de-las-Peñas et al., 2005 | Intervention group |
| 2 times/week 3 to 6 weeks Follow up: 1 week to 12 months | 30 min | NR |
| Comparison group |
| ||||
| Fernandez et al., 2020 | Intervention group |
| 1 to 3 times/week 3 to 12 weeks Follow up: 1 week to 12 months | 10 min | NR |
| Comparison group |
|
| Study | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | Score |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| La Touche et al., 2020 | 2 | 2 | 1 | 2 | 2 | 2 | 1 | 2 | 2 | 2 | 2 | 2 | 2 | 24 |
| Machado-Oliveira et al., 2020 | 2 | 2 | 1 | 1 | 0 | 1 | 2 | 2 | 1 | 0 | 0 | 0 | 0 | 12 |
| Falsiroli-Maistrello et al., 2019 | 2 | 0 | 1 | 2 | 1 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 22 |
| Jiang et al., 2019 | 2 | 2 | 1 | 1 | 1 | 2 | 0 | 2 | 1 | 2 | 2 | 2 | 0 | 18 |
| Lemmens et al., 2019 | 2 | 1 | 1 | 1 | 1 | 1 | 2 | 2 | 1 | 2 | 0 | 0 | 2 | 16 |
| Falsiroli-Maistrello et al., 2018 | 2 | 1 | 2 | 2 | 1 | 2 | 2 | 2 | 2 | 1 | 2 | 2 | 2 | 23 |
| Luedtke et al., 2016 | 2 | 2 | 1 | 2 | 1 | 2 | 2 | 2 | 2 | 1 | 2 | 2 | 2 | 23 |
| Mesa-Jiménez et al., 2015 | 1 | 2 | 1 | 1 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 0 | 21 |
| Chaibi and Russell, 2014 | 1 | 2 | 1 | 1 | 0 | 1 | 2 | 0 | 2 | 0 | 0 | 0 | 0 | 10 |
| Racicki et al., 2013 | 2 | 2 | 1 | 1 | 0 | 1 | 2 | 2 | 2 | 2 | 1 | 1 | 0 | 17 |
| Fernández-de-las-Peñas et al., 2006 | 1 | 2 | 1 | 1 | 0 | 1 | 2 | 2 | 2 | 2 | 0 | 0 | 1 | 15 |
| Bronfort et al., 2001 | 1 | 1 | 2 | 1 | 1 | 1 | 1 | 2 | 1 | 2 | 1 | 1 | 1 | 16 |
| Coelho et al., 2019 | 2 | 1 | 2 | 2 | 0 | 1 | 2 | 2 | 2 | 1 | 2 | 2 | 0 | 19 |
| Cumplido-Trasmonte et al., 2018 | 1 | 2 | 2 | 1 | 1 | 2 | 2 | 1 | 1 | 0 | 0 | 0 | 1 | 14 |
| Gil-Martínez et al., 2013 | 0 | 2 | 0 | 2 | 1 | 2 | 0 | 2 | 2 | 2 | 0 | 0 | 1 | 14 |
| Bronfort et al., 2009 | 1 | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 2 | 2 | 0 | 0 | 2 | 19 |
| Fernández-de-las-Peñas et al., 2005 | 0 | 2 | 0 | 0 | 2 | 0 | 0 | 0 | 1 | 0 | 0 | 1 | 1 | 7 |
| Fernandez et al., 2020 | 2 | 1 | 2 | 1 | 0 | 2 | 2 | 2 | 1 | 2 | 2 | 2 | 2 | 21 |
| Study | Phase 2 | Phase 3 | |||
|---|---|---|---|---|---|
| Study Eligibility Criteria | Identification and Selection of Studies | Data Collection and Study Appraisal | Synthesis and Findings | Risk of Bias in the Review | |
| La Touche et al., 2020 | L | L | L | L | L |
| Machado-Oliveira et al., 2020 | H | L | H | H | H |
| Falsiroli-Maistrello et al., 2019 | L | L | L | L | L |
| Jiang et al., 2019 | H | L | H | L | H |
| Lemmens et al., 2019 | H | H | L | H | H |
| Falsiroli-Maistrello et al., 2018 | L | L | L | L | L |
| Luedtke et al., 2016 | L | L | L | L | L |
| Mesa-Jiménez et al., 2015 | L | L | H | H | H |
| Chaibi and Russell, 2014 | H | H | H | H | H |
| Racicki et al., 2013 | H | H | H | H | H |
| Fernández-de-las-Peñas et al., 2006 | H | H | L | H | H |
| Bronfort et al., 2001 | H | H | H | H | H |
| Coelho et al., 2019 | H | H | L | L | H |
| Cumplido-Trasmonte et al., 2018 | L | H | H | H | H |
| Gil-Martínez et al., 2013 | L | H | H | H | H |
| Bronfort et al., 2009 | L | L | L | L | L |
| Fernández-de-las-Peñas et al., 2005 | H | H | H | H | H |
| Fernandez et al., 2020 | L | L | L | L | L |
| Criteria | Effect | Evidence | |||||
|---|---|---|---|---|---|---|---|
| Outcome Headache and Intervention Type (No. of Meta-Analyses) | Applicability | Generalizability | Risk of Bias or Study Limitations | Quantity and Consistency | Magnitude and Precision of Effect | SMD (95% CI) | |
| Pain intensity | |||||||
| Strong | Moderate | Strong | Limited | Moderate | −1.16 (−1.90, −0.41) | Moderate |
| Strong | Moderate | Limited | Limited | Moderate | −0.83 (−1.47, −0.19) | Limited |
| Strong | Moderate | Strong | Limited | Limited | −0.59 (−0.85, −0.33) | Moderate |
| Strong | Limited | Moderate | Limited | Limited | −0.49 (−0.86, −0.12) | Limited |
| Frequency of symptoms | |||||||
| Strong | Moderate | Limited | Limited | Moderate | −0.75 (−1.08, −0.43) | Limited |
| Strong | Moderate | Limited | Limited | Moderate | −0.91 (−2.18, 0.36) | Limited |
| Strong | Moderate | Limited | Limited | Limited | −0.30 (−0.84, 0.23) | Limited |
| Disability | |||||||
| Strong | Moderate | Limited | Limited | Limited | −0.27 (−0.47, −0.06) | Limited |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Herranz-Gómez, A.; García-Pascual, I.; Montero-Iniesta, P.; Touche, R.L.; Paris-Alemany, A. Effectiveness of Exercise and Manual Therapy as Treatment for Patients with Migraine, Tension-Type Headache or Cervicogenic Headache: An Umbrella and Mapping Review with Meta-Meta-Analysis. Appl. Sci. 2021, 11, 6856. https://doi.org/10.3390/app11156856
Herranz-Gómez A, García-Pascual I, Montero-Iniesta P, Touche RL, Paris-Alemany A. Effectiveness of Exercise and Manual Therapy as Treatment for Patients with Migraine, Tension-Type Headache or Cervicogenic Headache: An Umbrella and Mapping Review with Meta-Meta-Analysis. Applied Sciences. 2021; 11(15):6856. https://doi.org/10.3390/app11156856
Chicago/Turabian StyleHerranz-Gómez, Aida, Irene García-Pascual, Pablo Montero-Iniesta, Roy La Touche, and Alba Paris-Alemany. 2021. "Effectiveness of Exercise and Manual Therapy as Treatment for Patients with Migraine, Tension-Type Headache or Cervicogenic Headache: An Umbrella and Mapping Review with Meta-Meta-Analysis" Applied Sciences 11, no. 15: 6856. https://doi.org/10.3390/app11156856
APA StyleHerranz-Gómez, A., García-Pascual, I., Montero-Iniesta, P., Touche, R. L., & Paris-Alemany, A. (2021). Effectiveness of Exercise and Manual Therapy as Treatment for Patients with Migraine, Tension-Type Headache or Cervicogenic Headache: An Umbrella and Mapping Review with Meta-Meta-Analysis. Applied Sciences, 11(15), 6856. https://doi.org/10.3390/app11156856








