Estimation of Distances in 3D by Orthodontists Using Digital Models
Abstract
1. Introduction
1.1. VR (Virtual Reality) and Medical Applications
1.2. VR in Orthopedic Dentofacial Orthodontics
- −
- −
- Deploy, thanks to the practitioner’s diagnosis and therapeutic projection, a cognitive activity in space created digitally by 3D models (which is another key element of VR) [2].
1.3. VR and the Evaluation of Distances
1.4. Objective of the Study
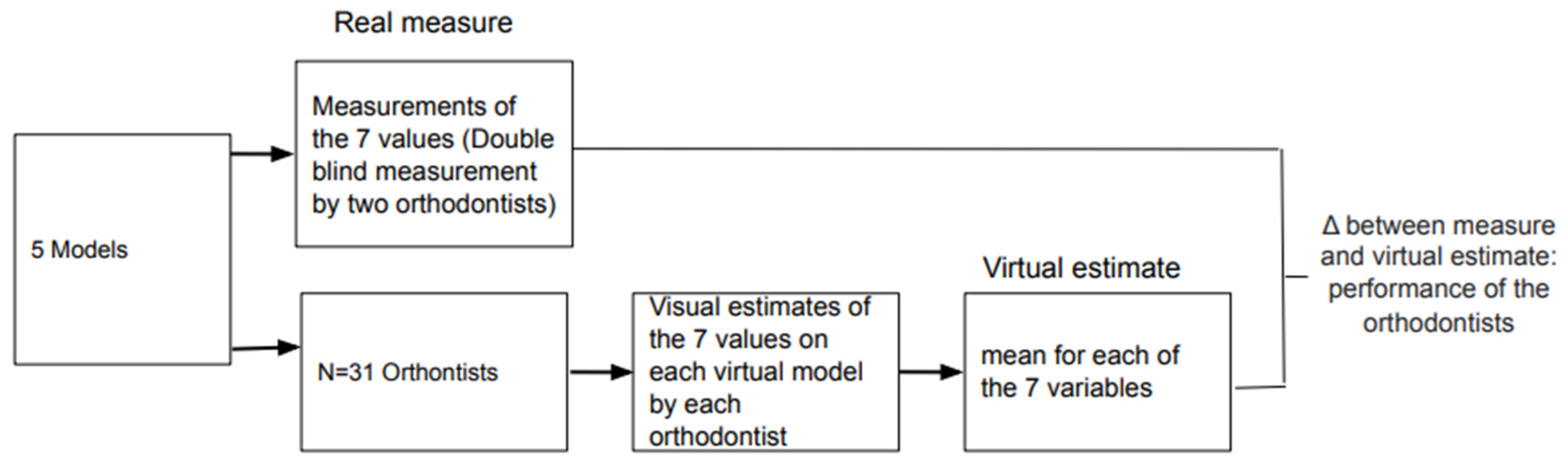
2. Method
2.1. Participants
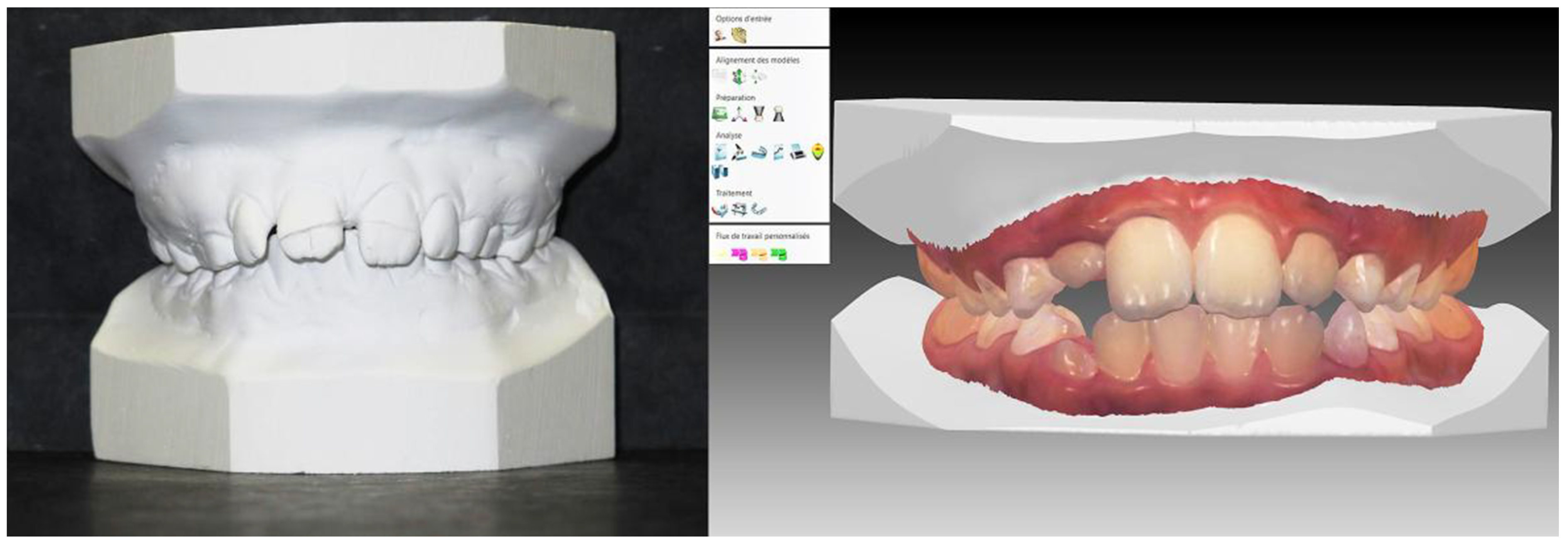
2.2. Materials
- −
- Crowding of the mandibular arch: the amount of space required for proper alignment of the teeth in the arch (volumetric reconstitution, intra-arch measurement);
- −
- Spee’s curve—the curve formed by the projection in a sagittal plane of the buccal cusps of the mandibular teeth (vertical dimension, intra-arch measurement);
- −
- Antero-posterior symmetry of the first permanent maxillary molars (teeth 16 and 26) while taking their mesial side as a reference (sagittal dimension, intra-arch measurement);
- −
- Inter-molar distance of 16/26 (horizontal dimension, intra-arch measurement): distance separating the mesiobuccal cusp of the first permanent maxillary molars (teeth 16 and 26);
- −
- Right canine class according to Angle’s classification [47] based on the mesiodistal relationship of the teeth (sagittal dimension, inter-arch measurement);
- −
- Overjet of 11/41—the gap as assessed on to the occlusal plane between the buccal side of the mandibular incisors and the occlusal edges of the central maxillary incisors (sagittal dimension, inter-arch measurement);
- −
- Alignment of 11/41—Alignment of the mandibular incisors by their opposing maxillaries (vertical dimension, inter-arch measurement).
2.3. Statistical Analyses
3. Results
- −
- Variables for which the estimates were not significantly different from the real values. This was the case for the following 3 variables:The overjet (t (30) = −1.60; p = 0.11);The curve of Spee (t (30) = −1.33; p = 0.19);The inter-molar distance (t (29) = 0.39; p = 0.69).
- −
- Variables for which the estimates were significantly different from the actual value 0 but not from the value 1. This was the case for the following 3 variables:The 16/26 symmetry: value = 0 (t (30) = −9.65; p ≤ 0.01), but with a test value = 1 (t (30) = −0.66; p = 0.51);The over bite: test value = 0 (t (30) = −5.40; p ≤ 0.01), but with a test value = 1 (t (30) = 0.64; p = 0.52);The right canine class: test value = 0 (t (30) = 3.19; p = ≤ 0.01), but with a test value = 1 (t (30) = −0.51; p = 0.61).
- −
- Variables for which the estimation error was significantly different from the value 1. This was the case only for the mandibular discrepancy variable: test value = 0 (t (30) = −10.74; p ≤ 0.01), test value = 1 (t (30) = 6.23; p ≤ 0.01).
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Stephen, R.E. What are virtual environments? IEEE Comput. Graph. Appl. 1994, 1, 17–22. [Google Scholar]
- Ouramdane, N.; Otmane, S.; Mallem, M. Interaction 3D en Réalité Virtuelle-Etat de l’art. Tech. Sci. Inform. 2009, 28, 1017–1049. [Google Scholar] [CrossRef]
- Engler, C.E. Affordable VR by 1994. Comput. Gaming World 1992, 1, 80–82. [Google Scholar]
- Li, L.; Yu, F.; Shi, D.; Shi, J.; Tian, Z.; Yang, J.; Wang, X.; Jiang, Q. Application of virtual reality technology in clinical medicine. Am. J. Transl. Res. 2017, 9, 3867–3880. [Google Scholar] [PubMed]
- Baldominos, A.; Saez, Y.; del Pozo, C.G. An approach to physical rehabilitation using state-of-the-art virtual reality and motion tracking technologies. Procedia Comput. Sci. 2015, 64, 10–16. [Google Scholar] [CrossRef]
- Li, A.; Montaño, Z.; Chen, V.J.; Gold, J.I. Virtual reality and pain management: Current trends and future directions. Pain Manag. 2011, 1, 147–157. [Google Scholar] [CrossRef] [PubMed]
- Satava, R.M.; Jones, S.B. Virtual environments for medical training and education. Presence Teleoperators Virtual Environ. 1997, 6, 139–146. [Google Scholar] [CrossRef]
- Ackerman, M.J. The visible human project. Proc. IEEE 1998, 86, 504–511. [Google Scholar] [CrossRef]
- Ayoub, A.; Pulijala, Y. The application of virtual reality and augmented reality in Oral & Maxillofacial Surgery. BMC Oral. Health 2019, 19, 1–8. [Google Scholar]
- Medellín-Castillo, H.I.; Govea-Valladares, E.H.; Pérez-Guerrero, C.N.; Gil-Valladares, J.; Lim, T.; Ritchie, J.M. The evaluation of a novel haptic-enabled virtual reality approach for computer-aided cephalometry. Comput. Methods Programs Biomed. 2016, 130, 46–53. [Google Scholar] [CrossRef]
- Wu, F.; Chen, X.; Lin, Y.; Wang, C.; Wang, X.; Shen, G.; Qin, J.; Heng, P.-A. A virtual training system for maxillofacial surgery using advanced haptic feedback and immersive workbench. Int. J. Med Robot. Comput. Assist. Surg. 2014, 10, 78–87. [Google Scholar] [CrossRef]
- Kwon, H.B.; Park, Y.S.; Han, J.S. Augmented reality in dentistry: A current perspective. Acta Odontol. Scand. 2018, 76, 497–503. [Google Scholar] [CrossRef] [PubMed]
- Ayoub, A.F.; Xiao, Y.; Khambay, B.; Siebert, J.P.; Hadley, D. Towards building a photo-realistic virtual human face for craniomaxillofacial diagnosis and treatment planning. Int. J. Oral Maxillofac. Surg. 2007, 36, 423–428. [Google Scholar] [CrossRef] [PubMed]
- Marcel, T.J. Three-dimensional on-screen virtual models. Am. J. Orthod. Dentofac. Orthop. 2001, 119, 666–668. [Google Scholar] [CrossRef] [PubMed]
- Kravitz, N.D.; Groth, C.; Jones, P.E.; Graham, J.W.; Redmond, W.R. Intraoral digital scanners. J. Clin. Orthod. 2014, 48, 337–347. [Google Scholar]
- Lanier, J. A Vintage Virtual Reality Interview, 1988. In Interview by Adam Heilbrun of Jaron Lanier, Published; 1988; Available online: https://philpapers.org/rec/LANAVV (accessed on 1 September 2021).
- TootyVR—Application de VR Dentaire. 2020. Available online: https://www.tootyvr.com/ (accessed on 1 September 2021).
- Siegel, Z.D.; Kelly, J.W. Walking through a virtual environment improves perceived size within and beyond the walked space. Atten. Percept. Psychophys. 2017, 79, 39–44. [Google Scholar] [CrossRef]
- El Jamiy, F.; Marsh, R. Distance estimation in virtual reality and augmented reality: A survey. In Proceedings of the 2019 IEEE International Conference on Electro Information Technology (EIT), Brookings, SD, USA, 20–22 May 2019; IEEE: New York, NY, USA, 2019; pp. 063–068. [Google Scholar]
- Swan, J.E.; Kuparinen, L.; Rapson, S.; Sandor, C. Visually perceived distance judgments: Tablet-based augmented reality versus the real world. Int. J. Hum.-Comput. Interact. 2017, 33, 576–591. [Google Scholar] [CrossRef]
- Bodenheimer, B.; Meng, J.; Wu, H.; Narasimham, G.; Rump, B.; McNamara, T.P.; Carr, T.H.; Rieser, J.J. Distance estimation in virtual and real environments using bisection. In Proceedings of the 4th Symposium on Applied Perception in Graphics and Visualization, Tubingen, Germany, 25–27 July 2007; pp. 35–40. [Google Scholar]
- Kuhl, S.A.; Thompson, W.B.; Creem-Regehr, S.H. HMD calibration and its effects on distance judgments. ACM Trans. Appl. Percept. 2009, 6, 1–20. [Google Scholar] [CrossRef]
- Messing, R.; Durgin, F.H. Distance perception and the visual horizon in head-mounted displays. ACM Trans. Appl. Percept. 2005, 2, 234–250. [Google Scholar] [CrossRef]
- Steinicke, F.; Bruder, G.; Hinrichs, K.; Lappe, M.; Ries, B.; Interrante, V. Transitional environments enhance distance perception in immersive virtual reality systems. In Proceedings of the 6th Symposium on Applied Perception in Graphics and Visualization, Chania, Greece, 30 September–2 October 2009; pp. 19–26. [Google Scholar]
- Ziemer, C.J.; Plumert, J.M.; Cremer, J.F.; Kearney, J.K. Estimating distance in real and virtual environments: Does order make a difference? Atten. Percept. Psychophys. 2009, 71, 1095–1106. [Google Scholar] [CrossRef] [PubMed]
- Kelly, J.W.; Donaldson, L.S.; Sjolund, L.A.; Freiberg, J.B. More than just perception-action recalibration: Walking through a virtual environment causes rescaling of perceived space. Atten. Percept. Psychophys. 2013, 75, 1473–1485. [Google Scholar] [CrossRef] [PubMed]
- Kunz, B.R.; Creem-Regehr, S.H.; Thompson, W.B. Does perceptual-motor calibration generalize across two different forms of locomotion? Investigations of walking and wheelchairs. PLoS ONE 2013, 8, e54446. [Google Scholar] [CrossRef]
- Stefanucci, J.K.; Creem-Regehr, S.H.; Thompson, W.B.; Lessard, D.A.; Geuss, M.N. Evaluating the accuracy of size perception on screen-based displays: Displayed objects appear smaller than real objects. J. Exp. Psychol. Appl. 2015, 21, 215. [Google Scholar] [CrossRef] [PubMed]
- Waller, D.; Richardson, A.R. Correcting distance estimates by interacting with immersive virtual environments: Effects of task and available sensory information. J. Exp. Psychol. Appl. 2008, 14, 61. [Google Scholar] [CrossRef] [PubMed]
- Durgin, F.H.; Gigone, K.; Scott, R. Perception of visual speed while moving. J. Exp. Psychol. Hum. Percept. Perform. 2005, 31, 339. [Google Scholar] [CrossRef] [PubMed]
- Henry, D.; Furness, T. Spatial perception in virtual environments: Evaluating an architectural application. In Proceedings of the IEEE Virtual Reality Annual International Symposium, Seattle, WA, USA, 18–22 September 1993; pp. 33–40. [Google Scholar]
- Interrante, V.; Ries, B.; Anderson, L. Distance perception in immersive virtual environments, revisited. In Proceedings of the IEEE Virtual Reality Conference (VR 2006), Alexandria, VA, USA, 25–29 March 2006; pp. 3–10. [Google Scholar]
- Knapp, J.M.; Loomis, J.M. Limited field of view of head-mounted displays is not the cause of distance underestimation in virtual environments. Presence Teleoperators Virtual Environ. 2004, 13, 572–577. [Google Scholar] [CrossRef]
- Mohler, B.J.; Creem-Regehr, S.H.; Thompson, W.B. The influence of feedback on egocentric distance judgments in real and virtual environments. In Proceedings of the 3rd Symposium on Applied Perception in Graphics and Visualization, Boston, MA, USA, 28–29 July 2006; pp. 9–14. [Google Scholar]
- Plumert, J.M.; Kearney, J.K.; Cremer, J.F.; Recker, K. Distance perception in real and virtual environments. ACM Trans. Appl. Percept. 2005, 2, 216–233. [Google Scholar] [CrossRef]
- Richardson, A.R.; Waller, D. The effect of feedback training on distance estimation in virtual environments. Appl. Cogn. Psychol. 2005, 19, 1089–1108. [Google Scholar] [CrossRef]
- Sahm, C.S.; Creem-Regehr, S.H.; Thompson, W.B.; Willemsen, P. Throwing versus walking as indicators of distance perception in similar real and virtual environments. ACM Trans. Appl. Percept. 2005, 2, 35–45. [Google Scholar] [CrossRef]
- Sinai, M.J.; Krebs, W.K.; Darken, R.P.; Rowland, J.H.; McCarley, J.S. Egocentric distance perception in a virutal environment using a perceptual matching task. In Proceedings of the Human Factors and Ergonomics Society Annual Meeting, Los Angeles, CA, USA, 1 September 1999; SAGE Publications: Los Angeles, CA, USA, 1999; Volume 43, pp. 1256–1260. [Google Scholar]
- Thompson, W.B.; Willemsen, P.; Gooch, A.A.; Creem-Regehr, S.H.; Loomis, J.M.; Beall, A.C. Does the quality of the computer graphics matter when judging distances in visually immersive environments? Presence 2004, 13, 560–571. [Google Scholar] [CrossRef]
- Willemsen, P.; Gooch, A.A. Perceived egocentric distances in real, image-based, and traditional virtual environments. In Proceedings of the IEEE Virtual Reality 2002, Orlando, FL, USA, 24–28 March 2002; pp. 275–276. [Google Scholar]
- Witmer, B.G.; Sadowski, W.J., Jr. Nonvisually guided locomotion to a previously viewed target in real and virtual environments. Hum. Factors 1998, 40, 478–488. [Google Scholar] [CrossRef]
- Loomis, J.M.; Knapp, J.M. Visual perception of egocentric distance in real and virtual environments. Virtual Adapt. Environ. 2003, 11, 21–46. [Google Scholar]
- Richardson, A.R.; Waller, D. Interaction with an immersive virtual environment corrects users’ distance estimates. Hum. Factors 2007, 49, 507–517. [Google Scholar] [CrossRef]
- Geuss, M.; Stefanucci, J.; Creem-Regehr, S.; Thompson, W.B. Can I pass? Using affordances to measure perceived size in virtual environments. In Proceedings of the 7th Symposium on Applied Perception in Graphics and Visualization, Los Angeles, CA, USA, 23–24 July 2010; pp. 61–64. [Google Scholar]
- Murgia, A.; Sharkey, P.M. Estimation of distances in virtual environments using size constancy. Int. J. Virtual Real. 2009, 8, 67–74. [Google Scholar] [CrossRef]
- Song, G.Y.; Jiang, R.P.; Zhang, X.Y.; Liu, S.Q.; Yu, X.N.; Chen, Q.; Weng, X.R.; Wu, W.Z.; Su, H.; Ren, C.; et al. Validation of subjective and objective evaluation methods for orthodontic treatment outcome. J. Peking Univ. Health Sci. 2015, 47, 90–97. [Google Scholar]
- Campbell, S.; Goldstein, G. Angle’s Classification—A Prosthodontic Consideration: Best Evidence Consensus Statement. J. Prosthodont. 2021, 30 (Suppl. 1), 67–71. [Google Scholar] [CrossRef]
- Rossini, G.; Parrini, S.; Castroflorio, T.; Deregibus, A.; Debernardi, C.L. Diagnostic accuracy and measurement sensitivity of digital models for orthodontic purposes: A systematic review. Am. J. Orthod. Dentofac. Orthop. 2016, 149, 161–170. [Google Scholar] [CrossRef]
- Kumar, A.A.; Phillip, A.; Kumar, S.; Rawat, A.; Priya, S.; Kumaran, V. Digital model as an alternative to plaster model in assessment of space analysis. J. Pharm. Bioallied Sci. 2015, 7 (Suppl. 2), S465. [Google Scholar] [CrossRef] [PubMed]
- Reuschl, R.P.; Heuer, W.; Stiesch, M.; Wenzel, D.; Dittmer, M.P. Reliability and validity of measurements on digital study models and plaster models. Eur. J. Orthod. 2016, 38, 22–26. [Google Scholar] [CrossRef]
- Priot, A.E.; Charbonneau, M.; Paillé, D. Spatial constraints for 3D perception in Helmet-Mounted Displays. In Head-and Helmet-Mounted Displays XIII: Design and Applications; International Society for Optics and Photonics: Bellingham, WA, USA, 2008; Volume 6955, p. 69550G. [Google Scholar]
- Aglioti, S.; DeSouza, J.F.; Goodale, M.A. Size-contrast illusions deceive the eye but not the hand. Curr. Biol. 1995, 5, 679–685. [Google Scholar] [CrossRef]
- Pavani, F.; Boscagli, I.; Benvenuti, F.; Rabuffetti, M.; Farnè, A. Are perception and action affected differently by the Titchener circles illusion? Exp. Brain Res. 1999, 127, 95–101. [Google Scholar] [CrossRef]
- Kenyon, R.V.; Phenany, M.; Sandin, D.; Defanti, T. Accommodation and size-constancy of virtual objects. Ann. Biomed. Eng. 2008, 36, 342–348. [Google Scholar] [CrossRef]
- Frey, J.; Hachet, M.; Lotte, F. EEG-based neuroergonomics for 3D user interfaces: Opportunities and challenges. Trav. Hum. 2017, 80, 73–92. [Google Scholar] [CrossRef]
- Kelly, J.W.; Hammel, W.W.; Siegel, Z.D.; Sjolund, L.A. Recalibration of perceived distance in virtual environments occurs rapidly and transfers asymmetrically across scale. IEEE Trans. Vis. Comput. Graph. 2014, 20, 588–595. [Google Scholar] [CrossRef]
- Ebrahimi, E.; Altenhoff, B.M.; Pagano, C.C.; Babu, S.V. Carryover effects of calibration to visual and proprioceptive information on near field distance judgments in 3d user interaction. In Proceedings of the 2015 IEEE Symposium on 3D User Interfaces (3DUI), Arles, France, 23–24 March 2015; pp. 97–104. [Google Scholar]
- Trabucco, J.T.; Rottigni, A.; Cavallo, M.; Bailey, D.; Patton, J.; Marai, G.E. User perspective and higher cognitive task-loads influence movement and performance in immersive training environments. BMC Biomed. Eng. 2019, 1, 21. [Google Scholar] [CrossRef]
- Goodale, M.A.; Milner, A.D.; Jakobson, L.S.; Carey, D.P. A neurological dissociation between perceiving objects and grasping them. Nature 1991, 349, 154–156. [Google Scholar] [CrossRef]
- Goodale, M.A.; Westwood, D.A. An evolving view of duplex vision: Separate but interacting cortical pathways for perception and action. Curr. Opin. Neurobiol. 2004, 14, 203–211. [Google Scholar] [CrossRef]
- Goodale, M.A.; Meenan, J.P.; Bülthoff, H.H.; Nicolle, D.A.; Murphy, K.J.; Racicot, C.I. Separate neural pathways for the visual analysis of object shape in perception and prehension. Curr. Biol. 1994, 4, 604–610. [Google Scholar] [CrossRef]
- Makaremi, M. The role of cognitive sciences in orthodontic treatments: Optimizing the interface between practitioners and new technologies. J. Dentofac. Anom. Orthod. 2016, 19, 410. [Google Scholar] [CrossRef]
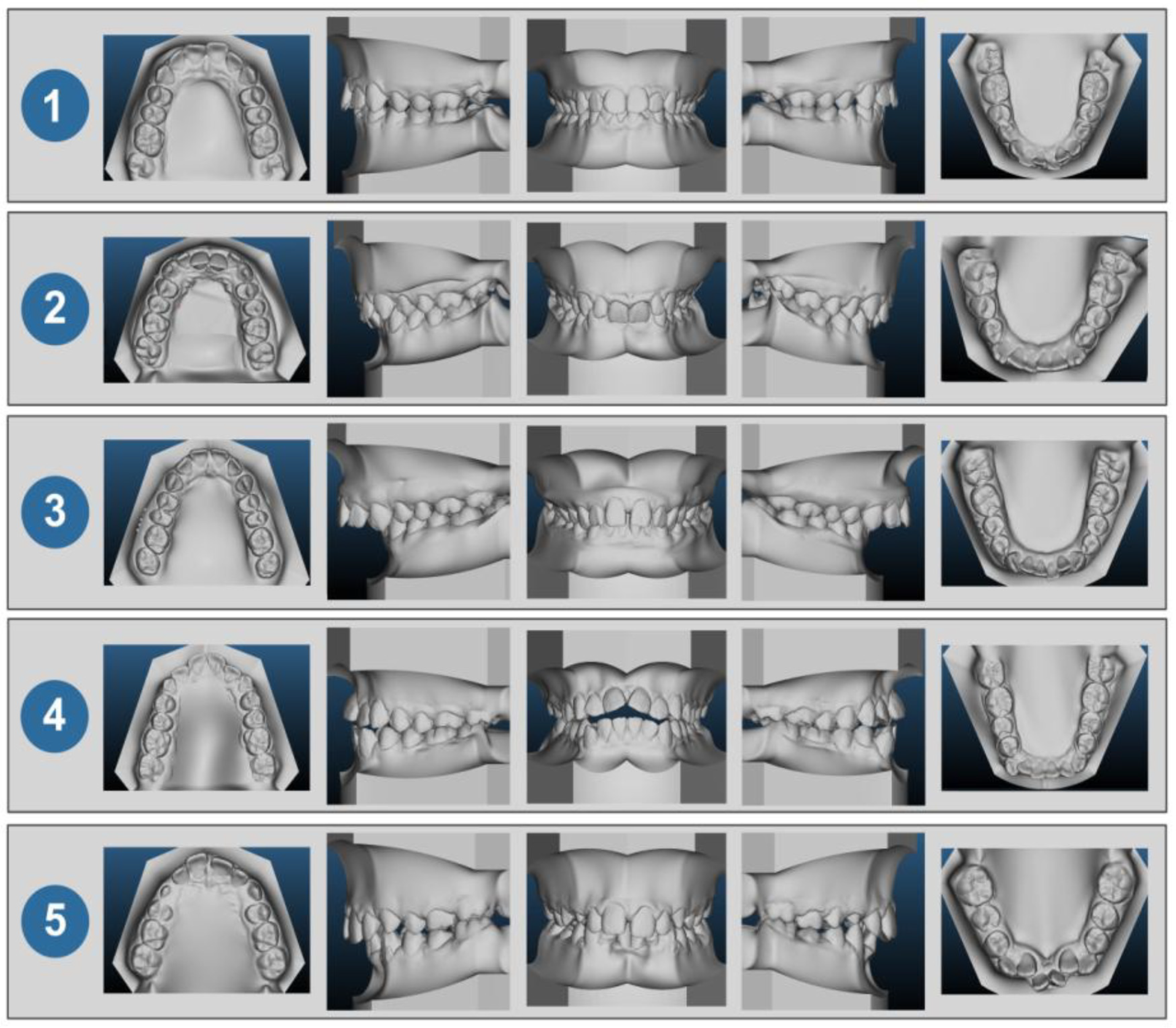

| Case no. 1 | Class I with moderate crowding of the arch |
| Case no. 2 | Class II with pronounced incisor supraclusion |
| Case no. 3 | Class II with a significantly increased overjet |
| Case no. 4 | Class II incisor infraclusion |
| Case no. 5 | Class II with malposition of the mandibular incisors |
| Case No. 1 | Case No. 2 | Case No. 3 | Case No. 4 | Case No. 5 | |
|---|---|---|---|---|---|
| Mandibular Discrepancy | ×1: −3 | ×1: 0.5 | ×1: −3 | ×1: −3.5 | ×1: 2.5 |
| ×2: −2.73 | ×2: −2.35 | ×2: −3.55 | ×2: −4.44 | ×2: −4.60 | |
| σ: 1.43 | σ: 3.21 | ×1: −3 | ×1: −3.5 | ×1: 2.5 | |
| Intermolar Distance | ×1: 36 | ×1: 37 | ×1: 36.5 | ×1: 40 | ×1: 40 |
| ×2: 38.10 | ×2: 38.6 | ×2: 38 | ×2: 36.6 | ×2: 41 | |
| σ: 7.82 | σ: 8.22 | σ: 8.73 | σ: 8.11 | σ: 8.36 | |
| Spee Curve | ×1: 2 | ×1: 1.5 | ×1: 2.5 | ×1: 2 | ×1: 2.5 |
| ×2: 2.42 | ×2: 1.66 | ×2: 2.47 | ×2: 1.03 | ×2: 2.2 | |
| σ: 0.81 | σ: 0.90 | σ: 0.86 | σ: 1.07 | σ: 0.87 | |
| 16/26 Symetric | ×1: 3 | ×1: 1 | ×1: 1 | ×1: 0 | ×1: 1.5 |
| ×2: 1.52 | ×2: 0.32 | ×2: 0.11 | ×2: −0.32 | ×2: 0.19 | |
| σ: 1.80 | σ: 0.97 | σ: 1.19 | σ: 0.77 | σ: 1.60 | |
| Right Canine Class | ×1: 6 | ×1: 1 | ×1: 8 | ×1: −4 | ×1: 2 |
| ×2: 5.45 | ×2: 3.24 | ×2: 7.34 | ×2: −2.75 | ×2: 2.95 | |
| σ: 1.47 | σ: 2.57 | σ: 2.19 | σ: 3.08 | σ: 1.36 | |
| Over Jet | ×1: 1.5 | ×1: 3.5 | ×1: 14 | ×1: 3 | ×1: 4.5 |
| ×2: 1.45 | ×2: 4.32 | ×2: 10.94 | ×2: 2.97 | ×2: 5.08 | |
| σ: 1.23 | σ: 1.81 | σ: 4.47 | σ: 1.04 | σ: 1.96 | |
| Over Bite | ×1: 7 | ×1: 5 | ×1: 5 | ×1: −5 | ×1: 4 |
| ×2: 6.27 | ×2: 3.52 | ×2: 9.55 | ×2: 4.18 | ×2: 3.63 | |
| σ: 1.60 | σ: 1.80 | σ: 1.11 | σ: 2.05 | σ: 0.97 |
| t = 0 | Mean | Standard Deviation | t | Sig. | Power (0.8) |
|---|---|---|---|---|---|
| Mandibular Discrepancy | −2.23 | 1.15 | −10.74 | ≤0.01 | 5 |
| Right Canine Class | 0.62 | 1.08 | 3.19 | ≤0.01 | 48 |
| Spee Curve | −0.13 | 0.58 | −1.33 | 0.19 | 313 |
| Intermolar Distance | 0.56 | 7.79 | 0.39 | 0.69 | 3049 |
| Over Bite | −0.65 | 0.66 | −5.40 | ≤0.01 | 17 |
| Over Jet | −0.34 | 1.20 | −1.60 | 0.11 | 197 |
| 16/26 Symetric | −0.93 | 0.53 | −9.65 | ≤0.01 | 6 |
| t = 1 | Mean | Standard Deviation | t | Sig. | Power (0.8) |
| Mandibular Discrepancy | 2.25 | 1.11 | 6.23 | ≤0.01 | 4 |
| Right Canine Class | 0.92 | 0.84 | −0.51 | 0.61 | 14 |
| Over Bite | 0.80 | 0.44 | 0.64 | 0.52 | 5 |
| 16/26 Symetric | 0.93 | 0.53 | −0.66 | 0.51 | 6 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Makaremi, M.; N’Kaoua, B. Estimation of Distances in 3D by Orthodontists Using Digital Models. Appl. Sci. 2021, 11, 8285. https://doi.org/10.3390/app11188285
Makaremi M, N’Kaoua B. Estimation of Distances in 3D by Orthodontists Using Digital Models. Applied Sciences. 2021; 11(18):8285. https://doi.org/10.3390/app11188285
Chicago/Turabian StyleMakaremi, Masrour, and Bernard N’Kaoua. 2021. "Estimation of Distances in 3D by Orthodontists Using Digital Models" Applied Sciences 11, no. 18: 8285. https://doi.org/10.3390/app11188285
APA StyleMakaremi, M., & N’Kaoua, B. (2021). Estimation of Distances in 3D by Orthodontists Using Digital Models. Applied Sciences, 11(18), 8285. https://doi.org/10.3390/app11188285





