Modified Endoscopic-Assisted Approach for Removal of Ectopic Third Molar in the Maxillary Sinus
Abstract
:1. Introduction
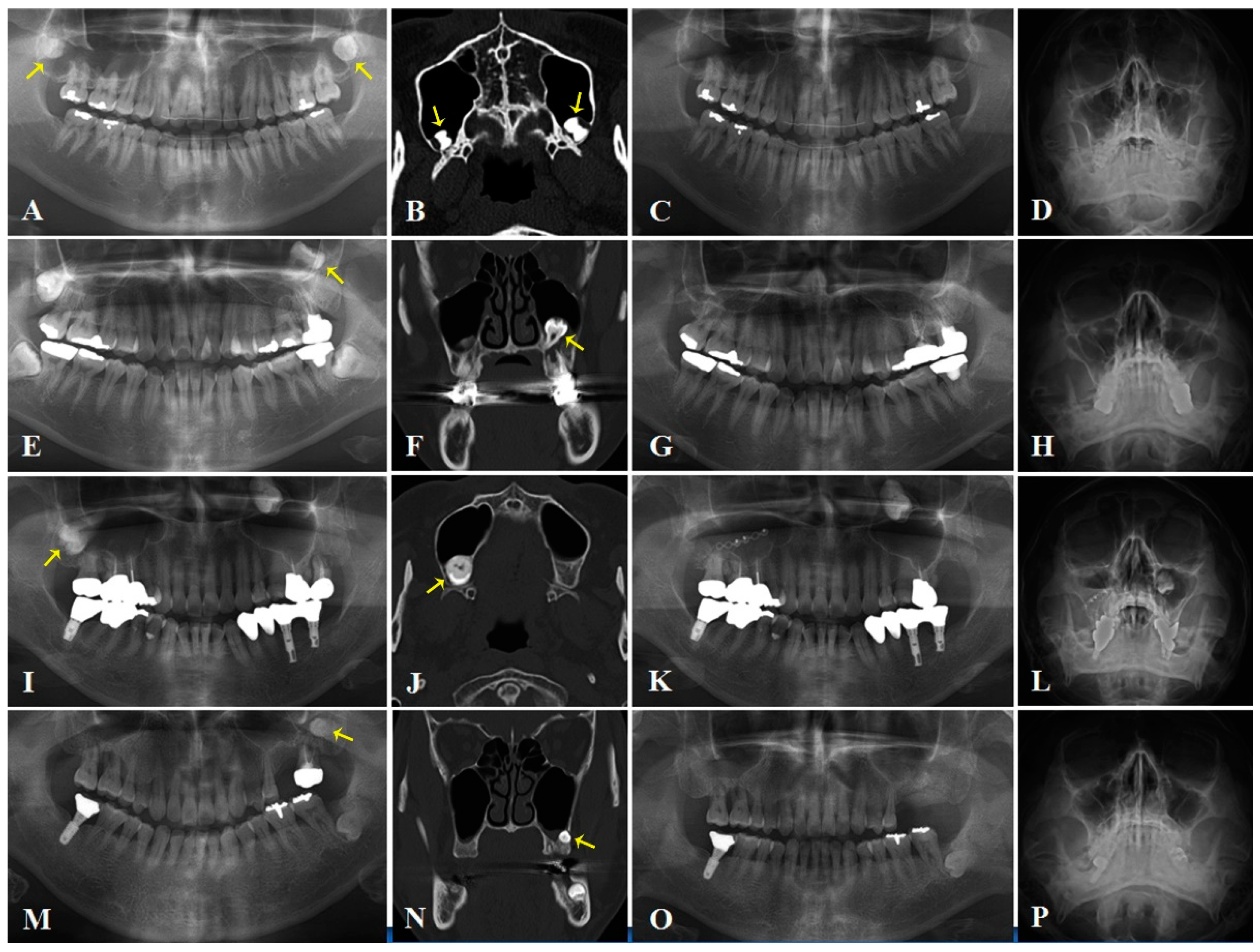
2. Case Series
2.1. Case 1
2.2. Case 2
2.3. Case 3
2.4. Case 4
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Buyukkurt, M.C.; Omezli, M.M.; Miloglu, O. Dentigerous cyst associated with an ectopic tooth in the maxillary sinus: A report of 3 cases and review of the literature. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2010, 109, 67–71. [Google Scholar] [CrossRef] [PubMed]
- Lombroni, L.G.; Farronato, G.; Santamaria, G.; Lombroni, D.M.; Gatti, P.; Capelli, M. Ectopic teeth in the maxillary sinus: A case report and literature review. Indian J. Dent. Res. 2018, 29, 667–671. [Google Scholar]
- Ramanojam, S.; Halli, R.; Hebbale, M.; Bhardwaj, S. Ectopic tooth in maxillary sinus: Case series. Ann. Maxillofac. Surg. 2013, 3, 89–92. [Google Scholar] [CrossRef]
- Huang, I.Y.; Chen, C.M.; Chuang, F.H. Caldwell-Luc procedure for retrieval of displaced root in the maxillary sinus. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2011, 112, e59–e63. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.M. The removal of an implant beneath the optic canal by modified endoscopic-assisted sinus surgery. Eur. Arch. Otorhinolaryngol. 2017, 274, 1167–1171. [Google Scholar] [PubMed]
- Sharma, S.; Chauhan, J.S. Bilateral ectopic third molars in maxillary sinus associated with dentigerous cyst—A rare case report. Int. J. Surg. Case Rep. 2019, 61, 298–301. [Google Scholar] [CrossRef] [PubMed]
- Yang, P.; Liang, H.; Zou, B.; Liu, J.; Yuan, D.; Meng, Z.; Xu, K. Ectopic tooth in maxillary sinus compressing the nasolacrimal canal: A case report. Medicine 2021, 200, e25514. [Google Scholar] [CrossRef] [PubMed]
- Bressan, E.; Ferroni, L.; Gardin, C.; Bellin, G.; Sbricoli, L.; Sivolella, S.; Brunello, G.; Schwartz-Arad, D.; Mijiritsky, E.; Penarrocha, M.; et al. Metal Nanoparticles Released from Dental Implant Surfaces: Potential Contribution to Chronic Inflammation and Peri-Implant Bone Loss. Materials 2019, 12, 2036. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vassallo, P.; Tranfa, F.; Forte, R.; D’Aponte, A.; Strianese, D.; Bonavolontà, G. Ophthalmic complications after surgery for nasal and sinus polyposis. Eur. J. Ophthalmol. 2001, 11, 218–222. [Google Scholar] [CrossRef] [PubMed]
- DeFreitas, J.; Lucente, F.E. The Caldwell-Luc procedure: Institutional review of 670 cases: 1975–1985. Laryngoscope 1998, 98, 1297–1300. [Google Scholar]
- Park, M.W.; Kim, S.M.; Amponsah, E.K.; Lee, S.K. Simple repair of a blow-out fracture by the modified Caldwell-Luc approach. J. Craniofac. Surg. 2015, 26, e306–e307. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.M.; Eo, M.Y.; Cho, Y.J.; Kim, Y.S.; Lee, S.K. Differential protein expression in the secretory fluids of maxillary sinusitis and maxillary retention cyst. Eur. Arch. Otorhinolaryngol. 2017, 274, 215–222. [Google Scholar] [CrossRef] [PubMed]
- Inchingolo, F.; Tatullo, M.; Marrelli, M.; Inchingolo, A.M.; Picciariello, V.; Inchingolo, A.D.; Dipalma, G.; Vermesan, D.; Cagiano, R. Clinical trial with bromelain in third molar exodontia. Eur. Rev. Med. Pharmacol. Sci. 2010, 14, 771–774. [Google Scholar] [PubMed]
- Diachkova, E.; Morozova, E.; Blagushina, N.; Tarasenko, S. The modified Caldwell-Luc approach with the use of collagen material for treatment of a chronic perforated maxillary sinusitis. Case Rep. Dent. 2020, 27, 8874227. [Google Scholar] [CrossRef] [PubMed]
- Juzikis, E.; Gaubys, A.; Rusilas, H. Uses of maxillary sinus lateral wall bony window in an open window sinus lift procedure: Literature review. Stomatologija 2018, 20, 14–21. [Google Scholar] [PubMed]
- Dimitriou, R.; Mataliotakis, G.I.; Calori, G.M.; Giannoudis, P.V. The role of barrier membranes for guided bone regeneration and restoration of large bone defects: Current experimental and clinical evidence. BMC Med. 2012, 10, 81. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Perniconi, B.; Coletti, D.; Aulino, P.; Costa, A.; Aprile, P.; Santacroce, L.; Chiaravalloti, E.; Coquelin, L.; Chevallier, N.; Teodori, L.; et al. Muscle acellular scaffold as a biomaterial: Effects on C2C12 cell differentiation and interaction with the murine host environment. Front. Physiol. 2014, 5, 354. [Google Scholar] [CrossRef] [PubMed] [Green Version]


Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Seo, M.-H.; Lee, J.-Y.; Frimpong, P.; Eo, M.-Y.; Kim, S.-M. Modified Endoscopic-Assisted Approach for Removal of Ectopic Third Molar in the Maxillary Sinus. Appl. Sci. 2021, 11, 8446. https://doi.org/10.3390/app11188446
Seo M-H, Lee J-Y, Frimpong P, Eo M-Y, Kim S-M. Modified Endoscopic-Assisted Approach for Removal of Ectopic Third Molar in the Maxillary Sinus. Applied Sciences. 2021; 11(18):8446. https://doi.org/10.3390/app11188446
Chicago/Turabian StyleSeo, Mi-Hyun, Ju-Young Lee, Paul Frimpong, Mi-Young Eo, and Soung-Min Kim. 2021. "Modified Endoscopic-Assisted Approach for Removal of Ectopic Third Molar in the Maxillary Sinus" Applied Sciences 11, no. 18: 8446. https://doi.org/10.3390/app11188446





