Analysis of Process Costing for the Use of Navigation Systems in Functional Endoscopic Sinus Surgery
Abstract
:Featured Application
Abstract
1. Introduction
Process Cost Accounting
2. Materials and Methods
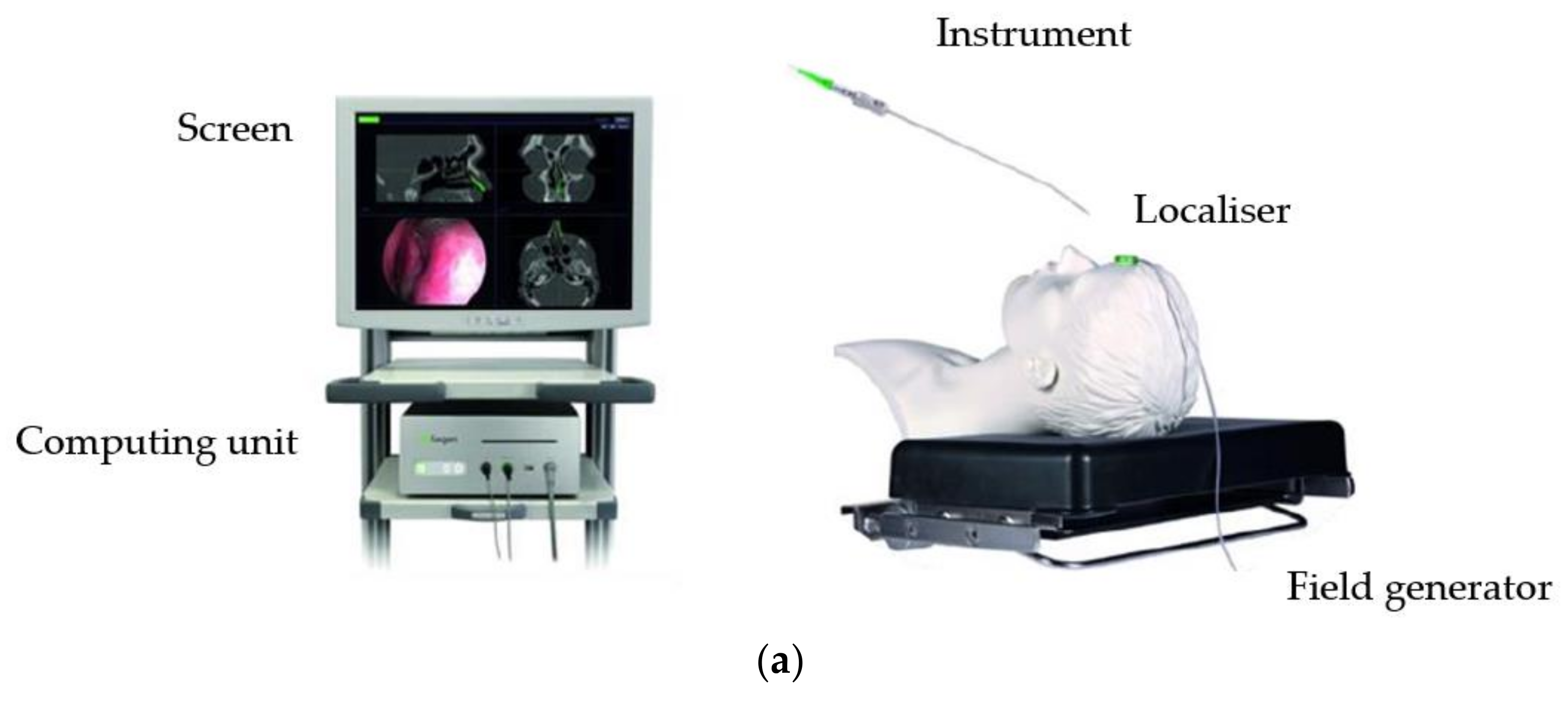
2.1. Navigation Device Usage Time
- Documentation of a complete and successful registration process.
- Matching date and operating time, from the log file to a navigated operation from the MCC.
2.2. Approach to Determining Process Costs
3. Results
3.1. Mean Navigation Device Usage Time
3.2. Frequency Distributions of Incision–Suture Times
3.3. Results—Operating Times
3.4. Cost Analysis
4. Discussion
Critical Examination of the Methodology
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Oeken, J.; Törpel, J. Der Einfluss der Navigation auf die endoskopische NNH-Chirurgie. HNO 2007, 56, 151–157. [Google Scholar] [CrossRef] [PubMed]
- Strauß, G.; Koulechov, K.; Röttger, S.; Bahner, J.; Trantakis, C.; Hofer, M.; Korb, W.; Burgert, O.; Meixensberger, J.; Manzey, D.; et al. Ist der Vorteil eines Navigationssystems in der HNO-Chirurgie messbar? Ein Konzept zur Evaluation ergonomischer und chirurgischer Erfolgsparameter. HNO 2006, 54, 947–957. [Google Scholar] [CrossRef] [PubMed]
- Grevers, G.; Menauer, F.; Leunig, A.; Caversaccio, M.; Kastenbauer, E. Navigationschirurgie bei Nasennebenhöhlenerkrankungen. Laryngorhinootologie 1999, 78, 41–46. [Google Scholar] [CrossRef]
- Reardon, E.J. Navigational risks associated with sinus surgery and the clinical effects of implementing a navigational system for sinus surgery. Laryngoscope 2002, 112 (Suppl. 99), 1–19. [Google Scholar] [CrossRef]
- Caversaccio, M.; Zheng, G.; Nolte, L.-P. Computerassistierte Chirurgie der Nasennebenhöhlen und er vorderen Schädelbasis. HNO 2008, 56, 376–378. [Google Scholar] [CrossRef]
- Schlöndorff, G.; Mosges, R.; Meyer-Ebrecht, D.; Krybus, W.; Adams, L. CAS (computer assisted surgery). A new procedure in head and neck surgery. HNO 1989, 37, 187–190. [Google Scholar] [PubMed]
- Hedermann, R. New Manufacturing Concepts for Electromagnetically Navigated Instruments. Master’s Thesis, Mechanical Engeneering, Technical University, Munich, Germany, 2013. [Google Scholar]
- Fiagon AG Medical Technologies. Available online: https://www.fiagon.com/ous/de/ (accessed on 6 August 2021).
- Zapp, W. Kosten-, Leistungs-, Erlös- und Ergebnisrechnung im Krankenhaus. (1. Auflage Ausg.); Baumann Fachverlage GmbH & Co. KG: Kulmbach, Germany, 2009. [Google Scholar]
- Hedderich, J. Angewandte Statistik: Methodensammlung mit R, 15. Auflage Hrsg.; Springer Spektrum: Berlin, Germany, 2016. [Google Scholar]
- Greiling, M. Pfade durch das klinische Prozessmanagement. (1. Auflage Ausg.); Kohlhammer GmbH: Stuttgart, Germany, 2004. [Google Scholar]
- Greiling, M. Prozesskostenrechnung im Krankenhaus-Instrument und praktische Umsetzung zur Steuerung der DRGs. In Leistungsmanagement im Krankenhaus: G-DRGS; Vetter, U., Hofmann, L., Eds.; Springer: Berlin/Heidelberg, Germany, 2005; pp. 117–129. [Google Scholar]
- Schöffski, O.; Graf von der Schulenburg, J.-M. Gesundheitsökonomische Evaluationen (4. Auflage Ausg.); Springer: Berlin/Heidelberg, Germany, 2012. [Google Scholar]
- Attigah, N.; Demirel, S.; Hakimi, M.; Bruijnen, H.; Schöffski, O.; Müller, A.; Geis, U.; Böckler, D. Hybridoperationssaal vs. konventioneller Operationssaal: Betriebswirtschaftliche Gegenüberstellung in der Gefäßchirurgie am Beispiel der endovaskulären Aneurysmachirugie. Chirurg 2017, 88, 587–594. [Google Scholar] [CrossRef] [PubMed]
- Kothe-Zimmermann, H. Prozesskostenrechnung und Prozessoptimierung im Krankenhaus (1. Auflage Ausg.); W. Kohlhammer: Stuttart, Germany, 2006. [Google Scholar]
- Cerha, O.; Kirschner, S.; Günther, K.-P.; Lützner, J.J.D.O. Kostenanalyse zu Navigation in der Knieendoprothetik. Orthopädie 2009, 38, 1235–1240. [Google Scholar] [CrossRef]
- Strauß, G.; Limpert, E.; Strauss, M.; Hofer, M.; Dittrich, E.; Nowatschin, S.; Lüth, T. Untersuchung zur Effizienz eines Navigationssystems für die HNO-Chirurgie. Laryngorhinootologie 2009, 88, 776–781. [Google Scholar] [CrossRef]
- Mueller, S.; Caversaccio, M. Outcome of computer-assisted surgery in patients with chronic rhinosinusitis. J. Laryngol. Otol. 2010, 124, 500–504. [Google Scholar] [CrossRef] [Green Version]
- Giotakis, A.; Kral, F.; Freysinger, W.; Markart, S.; Riechelmann, H. Missed paranasal sinus compartments in sinus surgery with and without image-guidance systems: A pilot feasibility study. Int. J. Comput. Assist. Radiol. Surg. 2019, 14, 895–902. [Google Scholar] [CrossRef] [PubMed]
- Hepworth, E.; Bucknor, M.; Patel, A.; Vaughan, W.C. Nationwide survey on the use of image-guided functional endoscopic sinus surgery. Otolaryngol. Head Neck. Surg. 2006, 135, 68–73. [Google Scholar] [CrossRef]
- Rosen, M.; Saigal, K.; Evans, J.; Keane, W.M. A review of the endoscopic approach to the pituitary through the sphenoid sinus. Curr. Opin. Otolaryngol. Head Neck Surg. 2006, 14, 6–13. [Google Scholar] [CrossRef] [PubMed]
- Weber, R. Aktueller Stand der endonasalen Nasennebenhöhlenchirurgie. Laryngorhinootologie 2015, 94 (Suppl. 1), S64–S142. [Google Scholar] [CrossRef] [PubMed]
- Gibbons, M.; Gunn, M.; Niwas, S.; Sillers, M.J. Cost analysis of computer-aided endoscopic sinus surgery. Am. J. Rhinol. Mar.-Apr. 2001, 15, 71–75. [Google Scholar] [CrossRef] [PubMed]
- Metson, R.; Consenza, M.; Cunningham, M.; Randolph, G.W. Physician experience with an optical image guidance system for sinus surgery. Laryngoscope. 2000, 110, 972–976. [Google Scholar] [CrossRef] [PubMed]
- Caversaccio, M.; Bächler, R.; Lädrach, K.; Schroth, G.; Nolte, L.P.; Häusler, R. Frameless computer-aided surgery system for revision endoscopic sinus surgery. Otolaryngol. Head Neck Surg. 2000, 122, 808–813. [Google Scholar] [CrossRef]
- Sedlmaier, B.; Schleich, A.; Ohnesorge, B. Das NEN-HNO-Navigationsystem-erste klinische Anwendung. HNO 2001, 49, 523–529. [Google Scholar] [CrossRef]
- Kahn, M.; Ecke, U.; Mann, W. Der Einsatz eines optischen Navigationssystems in der Nasennebenhöhlenchirurgie. HNO 2003, 51, 209–215. [Google Scholar] [CrossRef]
- Sunkaraneni, V.; Yeh, D.; Qian, H.; Javer, A.R. Computer or not? Use of image guidance during endoscopic sinus surgery for chronic rhinosinusitis at St Paul’s Hospital, Vancouver, and meta-analysis. J. Laryngol. Otol. 2013, 127, 368–377. [Google Scholar] [CrossRef]
- Casiano, R.; Numa, W. Efficacy of computed tomographic image-guided endoscopic sinus surgery in residency training programs. Laryngoscope 2000, 110, 1277–1282. [Google Scholar] [CrossRef]
- Sugino, T.; Nakamura, R.; Kuboki, A.; Honda, O.; Yamamoto, M.; Ohtori, N. Comparative analysis of surgical processes for image-guided endoscopic sinus surgery. Int. J. Comput. Assist. Radiol. Surg. 2019, 1, 93–104. [Google Scholar] [CrossRef] [PubMed]
- Fried, M.; Moahrir, V.; Shin, J.; Taylor-Becker, M.; Morrison, P. Comparison of endoscopic sinus surgery with and without image guidance. Am. J. Rhinol. Jul.-Aug. 2002, 16, 193–197. [Google Scholar] [CrossRef]
- Dalgorf, D.; Sacks, R.; Wormald, P.-J.; Naidoo, Y.; Panizza, B.; Uren, B.; Brown, C.; Curotta, J.; Snidvongs, K.; Harvey, R.J. Image-guided surgery influences perioperative morbidity from endoscopic sinus surgery: A systematic review and meta-analysis. Otolaryngol. Head Neck Surg. 2013, 149, 17–29. [Google Scholar] [CrossRef] [PubMed]







| Period | 01.01.2012–31.12.2016 | ||
|---|---|---|---|
| Total | Group without Navigation | Group with Navigation | |
| Number of cases (n) | 1158 | 829 | 329 |
| female (n) | 448 | 339 | 109 |
| female (%) | 38.69% | 40.89% | 33.13% |
| male (n) | 710 | 490 | 220 |
| male (%) | 61.31% | 59.11% | 66.87% |
| Mean age (a) | 48.97 | 48.55 | 50.04 |
| Age: min/max | 8/89 | 8/87 | 8/89 |
| 2012 | 2013 | 2014 | 2015 | 2016 | Total | Mean (n/Year) | |
|---|---|---|---|---|---|---|---|
| With navigation | 15 | 38 | 76 | 111 | 89 | 329 | |
| Without navigation | 217 | 174 | 157 | 137 | 144 | 829 | |
| Total | 232 | 212 | 233 | 248 | 208 | 1158 | 227 |
| Position | Number of Physicians | Number of Operations with Navigation | Number of Operations without Navigation | Total |
|---|---|---|---|---|
| Junior Doctors | 22 | 34 | 136 | 170 |
| Specialists | 8 | 33 | 179 | 212 |
| Consultants | 15 | 79 | 363 | 442 |
| Head of Department | 1 | 183 | 151 | 334 |
| Total | 46 | 329 | 829 | 1158 |
| CC grp | CT grp | Cost-Type Group Long Name | ActType | AvgTariff | Comments | |
|---|---|---|---|---|---|---|
| ENT Surgery | 4 | 1 | Personnel costs: medical activity | SNZ_GW_AD | EUR 1.19/min | Weighted incision–suture time incl. set-up time physician |
| 4 | 3 | Personnel costs: med. tech. activity/functional activity | SNZ_GW_FD | EUR 0.83/min | Weighted incision–suture time incl. set-up time functional activity | |
| 4 | 7 | Personnel and material costs: med. infrastructure | SNZ_RZ | EUR 1.37/min | Incision–suture time incl. set-up time | |
| 4 | 8 | Personnel and material costs: non-med. infrastructure | SNZ_RZ | EUR 1.31/min | Incision–suture time incl. set-up time | |
| 4 | 4a | Material costs: medication (indirect costs) | SNZ_RZ | EUR 0.05/min | Incision–suture time incl. set-up time | |
| 4 | 6a | Material costs: other med. needs (indirect costs) | SNZ_RZ | EUR 0.83/min | Incision–suture time incl. set-up time | |
| Anesthesia | 5 | 1 | Personnel costs: medical activity | NRK_AD | EUR 0.98/min | Weighted anesthesia time incl. set-up time physician |
| 5 | 3 | Personnel costs: med. tech. activity/functional activity | NRK_FD | EUR 0.74/min | Weighted anesthesia time incl. set-up time functional activity | |
| 5 | 4a | Material costs: medication (indirect costs) | NRK | EUR 0.12/min | Anesthesia time | |
| 5 | 6a | Material costs: other med. need (indirect costs) | NRK | EUR 0.58/min | Anesthesia time | |
| 5 | 7 | Personnel and material costs: med. infrastructure | NRK | EUR 0.32/min | Anesthesia time | |
| 5 | 8 | Personnel and material costs: non-med. infrastructure | NRK | EUR 0.47/min | Anesthesia time |
| Mean | Median | SD | Interquartile Range | Minimum | Maximum | |
|---|---|---|---|---|---|---|
| Time (min) | 7.50 | 6.44 | 5.03 | 6.57 | 0.60 | 29.67 |
| Without Navigation | With Navigation | |||||||
|---|---|---|---|---|---|---|---|---|
| Number | Mean Operating Time (Min) | Median (Min) | SD | Number | Mean Operating Time (Min) | Median (Min) | SD | |
| Junior Doctors | 136 | 92.96 | 87.00 | 40.81 | 34 | 121.21 | 110.00 | 49.20 |
| JNR1 | 8 | 84.25 | 87 | 18.58 | 3 | 89.33 | 94 | 9.87 |
| JNR2 | 4 | 80.75 | 102 | 45.19 | ||||
| JNR3 | 8 | 78.75 | 72 | 31.52 | 6 | 162.17 | 141 | 69.36 |
| JNR4 | 2 | 76.00 | 76 | 46.67 | ||||
| JNR5 | 19 | 101.05 | 96 | 37.20 | 1 | 110.00 | 100 | |
| JNR6 | 4 | 84.25 | 91.5 | 37.99 | 1 | 57.00 | 57 | |
| JNR7 | 3 | 94.67 | 90 | 8.08 | ||||
| JNR8 | 1 | 67.00 | 67 | |||||
| JNR9 | 5 | 86.40 | 76 | 49.23 | ||||
| JNR10 | 6 | 118.67 | 111 | 61.05 | ||||
| JNR11 | 7 | 78.86 | 78 | 44.08 | 2 | 88.50 | 88.5 | 38.89 |
| JNR12 | 4 | 82.50 | 104 | 33.04 | 2 | 100.50 | 100.5 | 4.95 |
| JNR13 | 3 | 99.33 | 80 | 38.80 | ||||
| JNR14 | 5 | 72.80 | 61 | 35.44 | 1 | 206.00 | 206 | |
| JNR15 | 9 | 95.00 | 87.5 | 38.88 | ||||
| JNR16 | 1 | 46.00 | 46 | |||||
| JNR17 | 13 | 102.92 | 116 | 46.65 | 14 | 129.64 | 117.5 | 34.49 |
| JNR18 | 15 | 98.00 | 93.5 | 43.04 | 2 | 83.00 | 83 | 11.31 |
| JNR19 | 4 | 144.00 | 125 | 62.42 | ||||
| JNR20 | 2 | 117.00 | 117 | 38.18 | 1 | 38.00 | 38 | |
| JNR21 | 8 | 70.38 | 58 | 33.33 | 1 | 110.00 | 110 | |
| JNR22 | 5 | 97.20 | 97 | 44.72 | ||||
| Specialists | 179 | 99.05 | 93.00 | 50.52 | 33 | 113.12 | 114.00 | 42.40 |
| SP1 | 26 | 101.46 | 107 | 46.54 | 5 | 132.60 | 168 | 60.64 |
| SP2 | 34 | 114.32 | 105 | 56.49 | 7 | 127.71 | 122 | 36.07 |
| SP3 | 28 | 111.86 | 113 | 60.05 | 14 | 106.07 | 112 | 34.10 |
| SP4 | 18 | 65.78 | 77 | 21.96 | ||||
| SP5 | 18 | 123.11 | 131 | 43.53 | 1 | 175.00 | 161.5 | |
| SP6 | 39 | 77.44 | 74 | 43.43 | 2 | 59.50 | 59.5 | 38.89 |
| SP7 | 16 | 103.31 | 101.5 | 39.87 | 4 | 99.25 | 102 | 36.34 |
| Consultants | 363 | 76.01 | 67.00 | 42.52 | 79 | 75.37 | 72.00 | 34.70 |
| CON1 | 11 | 84.55 | 77 | 28.57 | 1 | 40.00 | 40 | |
| CON2 | 34 | 68.76 | 59.5 | 36.40 | 2 | 75.00 | 75 | 22.63 |
| CON3 | 28 | 103.61 | 103 | 45.19 | 1 | 81.00 | 81 | |
| CON4 | 1 | 48.00 | 48 | |||||
| CON5 | 6 | 116.67 | 118 | 52.37 | ||||
| CON6 | 17 | 106.41 | 104.5 | 53.71 | 1 | 50.00 | 50 | |
| CON7 | 59 | 83.22 | 81.5 | 38.66 | 23 | 92.87 | 104 | 33.65 |
| CON8 | 14 | 83.57 | 74 | 23.44 | ||||
| CON9 | 17 | 52.24 | 45.5 | 27.38 | 28 | 70.18 | 69 | 33.46 |
| CON10 | 64 | 67.81 | 61.5 | 37.09 | 3 | 68.00 | 32 | 72.99 |
| CON11 | 26 | 51.27 | 50 | 25.68 | 8 | 62.25 | 80 | 29.79 |
| CON12 | 23 | 71.96 | 81 | 45.41 | 1 | 58.00 | 58 | |
| CON13 | 21 | 61.81 | 63 | 28.56 | 6 | 59.33 | 54.5 | 26.69 |
| CON14 | 42 | 77.86 | 67 | 55.92 | 5 | 83.20 | 59 | 33.17 |
| Head of Department | 151 | 55.32 | 49.00 | 29.10 | 183 | 60.29 | 57.00 | 28.52 |
| Overall result | 829 | 80.00 | 72.00 | 44.59 | 329 | 75.50 | 69.00 | 40.55 |
| Without Navigation | With Navigation | |||||||
|---|---|---|---|---|---|---|---|---|
| Number | Mean Operating Time | Median | SD | Number | Mean Operating Time | Median | SD | |
| Junior Doctors | 21 | 93.71 | 80.00 | 42.41 | 20 | 139.40 | 117.00 | 48.10 |
| JNR3 | 8 | 78.75 | 72 | 31.52 | 6 | 162.17 | 141 | 69.36 |
| JNR17 | 13 | 102.92 | 116 | 46.65 | 14 | 129.64 | 117.5 | 34.49 |
| Specialists | 62 | 113.21 | 109.00 | 57.65 | 21 | 113.29 | 114.00 | 35.43 |
| SP2 | 34 | 114.32 | 105 | 56.49 | 7 | 127.71 | 122.00 | 36.07 |
| SP3 | 28 | 111.86 | 113 | 60.05 | 14 | 106.07 | 112 | 34.10 |
| Consultants | 76 | 76.29 | 67.50 | 38.53 | 51 | 80.41 | 80.00 | 35.11 |
| CON7 | 59 | 83.22 | 81.5 | 38.66 | 23 | 92.87 | 104 | 33.65 |
| CON9 | 17 | 52.24 | 45.5 | 27.38 | 28 | 70.18 | 69 | 33.46 |
| Head of Department | 151 | 55.32 | 49.00 | 29.10 | 183 | 60.29 | 57.00 | 28.52 |
| Overall result | 310 | 74.64 | 59.00 | 45.28 | 275 | 73.82 | 69.00 | 39.76 |
| Tariff (EUR/Min) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ENT Surgery | CCGrp | CTGrp | CTGrp Long Name | 2012 | 2013 | 2014 | 2015 | 2016 | Mean | SD | Mean Weighting | Calculated Tariff (EUR/Min) |
| 4 | 1 | Personnel costs: medical activity | 1.21 | 1.01 | 1.22 | 1.12 | 1.19 | 1.15 | 0.071 | 1.7 | 1.91 | |
| 4 | 3 | Personnel costs: med. tech. activity/functional activity | 0.86 | 0.91 | 0.89 | 0.95 | 0.83 | 0.89 | 0.039 | 2.4 | 2.15 | |
| 4 | 7 | Personnel and material costs: med. infrastructure | 1.01 | 1.12 | 1.07 | 1.09 | 1.37 | 1.13 | 0.113 | 1.0 | 1.13 | |
| 4 | 8 | Personnel and material costs: non-med. infrastructure | 1.15 | 1.18 | 1.27 | 1.16 | 1.30 | 1.21 | 0.057 | 1.0 | 1.21 | |
| 4 | 4a | Material costs: medication (indirect costs) | 0.07 | 0.06 | 0.06 | 0.05 | 0.05 | 0.06 | 0.006 | 1.0 | 0.06 | |
| 4 | 6a | Material costs: other med. need (indirect costs) | 0.87 | 0.81 | 1.09 | 0.60 | 0.83 | 0.84 | 0.143 | 1.0 | 0.84 | |
| Anesthesia | 5 | 1 | Personnel costs: medical activity | 1.18 | 1.13 | 1.11 | 1.12 | 0.98 | 1.10 | 0.062 | 1.3 | 1.44 |
| 5 | 3 | Personnel costs: med. tech. activity/functional activity | 0.79 | 0.81 | 0.84 | 0.85 | 0.74 | 0.81 | 0.036 | 1.8 | 1.45 | |
| 5 | 7 | Personnel and material costs: med. infrastructure | 0.38 | 0.38 | 0.37 | 0.39 | 0.32 | 0.37 | 0.025 | 1.0 | 0.37 | |
| 5 | 8 | Personnel and material costs: non-med. infrastructure | 0.56 | 0.56 | 0.51 | 0.42 | 0.47 | 0.51 | 0.048 | 1.0 | 0.51 | |
| 5 | 4a | Material costs: medication (indirect costs) | 0.13 | 0.12 | 0.12 | 0.13 | 0.12 | 0.12 | 0.006 | 1.0 | 0.12 | |
| 5 | 6a | Material costs: other med. need (indirect costs) | 0.59 | 0.60 | 0.60 | 0.64 | 0.58 | 0.60 | 0.019 | 1.0 | 0.60 | |
| Total: | 11.79 | |||||||||||
| Number of Operations/Year: | 227 | |||||
|---|---|---|---|---|---|---|
| Navigated (Min) | Non-Navigated (Min) | Difference (Min) | Cost Rate (EUR/Min) | Per Operation (EUR) | Per Year (EUR) | |
| Case 1 | 69 | 72 | −3 | 11.79 | −5.4 | −8029.0 |
| Case 2 | 69 | 59 | 10 | 117.9 | 26,763.3 | |
| Case 3 | 57 | 49 | 8 | 94.3 | 21,410.6 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schwan, F.E.; Traxdorf, M.; Seebauer, C.T.; Sekita, A.; Habekost, C.; Iro, H.; Bohr, C. Analysis of Process Costing for the Use of Navigation Systems in Functional Endoscopic Sinus Surgery. Appl. Sci. 2021, 11, 8616. https://doi.org/10.3390/app11188616
Schwan FE, Traxdorf M, Seebauer CT, Sekita A, Habekost C, Iro H, Bohr C. Analysis of Process Costing for the Use of Navigation Systems in Functional Endoscopic Sinus Surgery. Applied Sciences. 2021; 11(18):8616. https://doi.org/10.3390/app11188616
Chicago/Turabian StyleSchwan, Franziska Eva, Maximilian Traxdorf, Caroline Theresa Seebauer, Andrzej Sekita, Cornelia Habekost, Heinrich Iro, and Christopher Bohr. 2021. "Analysis of Process Costing for the Use of Navigation Systems in Functional Endoscopic Sinus Surgery" Applied Sciences 11, no. 18: 8616. https://doi.org/10.3390/app11188616






