Cortisol Reactivity to a Digital Version of Trier Social Stress Test and Eating Behavior in Non-Overweight and Overweight Adolescents: A Pilot Study
Abstract
1. Introduction
2. Design and Methods
2.1. Study Population
2.2. Study Design
2.3. Trier Social Stress Test (TSST)
2.3.1. Pre-Experimental Stage (10 min)
2.3.2. Experimental Stage
2.3.3. The Recovery Stage (25 min)
2.4. Collection and Analysis of Salivary Cortisol Samples
2.5. Anthropometric Measurements
2.6. Statistical Analysis
3. Results
3.1. Sociodemographics, Anthropometric, Perceived Stress, and Cortisol Response to Induced-Social Stress in Adolescents
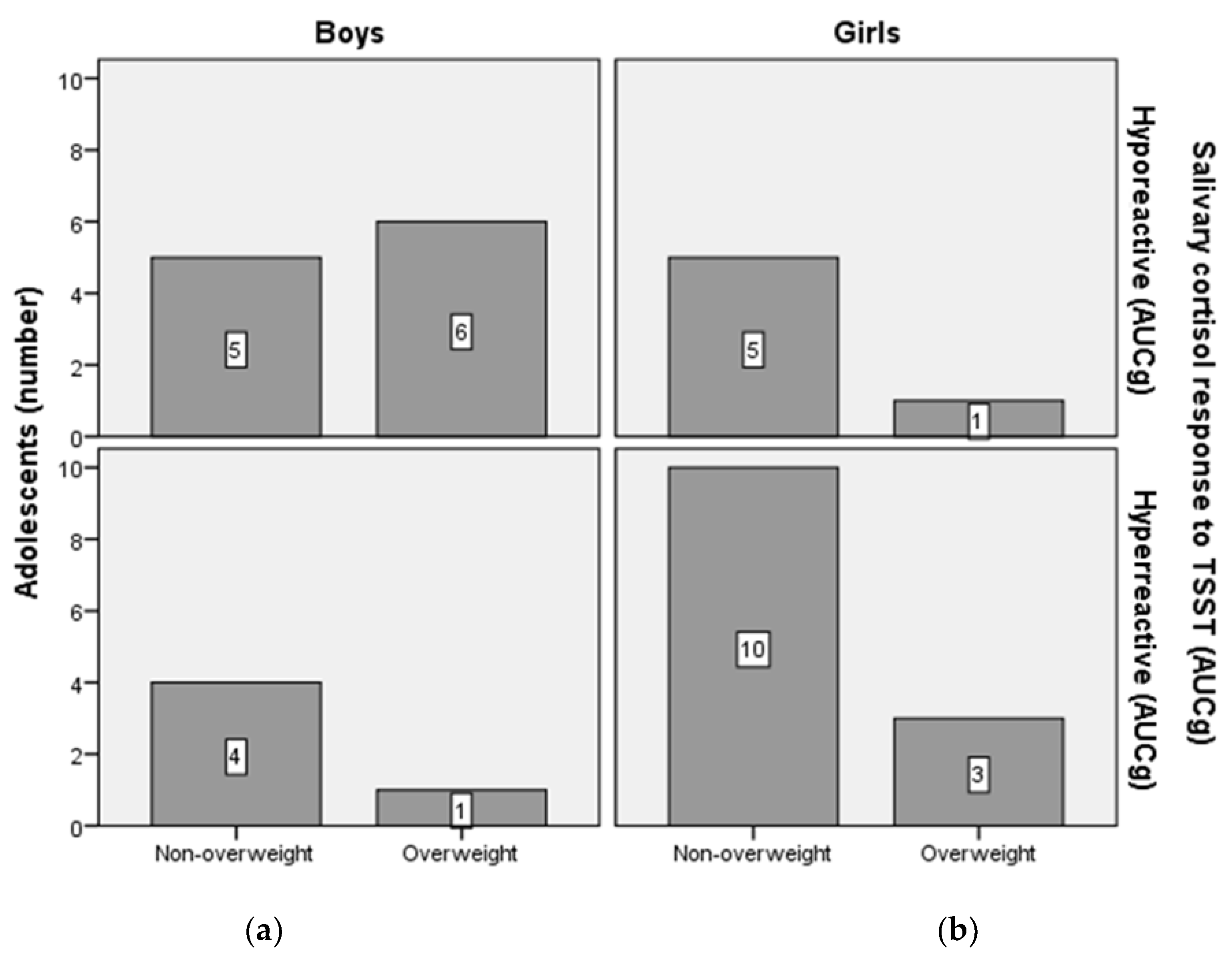
3.2. Cortisol Reactivity and Adiposity in Adolescents
3.3. Cortisol Reactivity and Eating Behavior in Adolescents
3.4. Correlations between Cortisol Response to TSST and PSS Scores
3.5. Correlations between Stress Parameters and Eating Behavior
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Therrien, F.; Drapeau, V.; Lalonde, J.; Lupien, S.J.; Beaulieu, S.; Tremblay, A.; Richard, D. Awakening cortisol response in lean, obese, and reduced obese individuals: Effect of gender and fat distribution. Obesity 2007, 15, 377–385. [Google Scholar] [CrossRef]
- Epel, E.; Lapidus, R.; McEwen, B.; Brownell, K. Stress may add bite to appetite in women: A laboratory study of stress-induced cortisol and eating behavior. Psychoneuroendocrinology 2001, 26, 37–49. [Google Scholar] [CrossRef]
- Dickerson, S.S.; Kemeny, M.E. Acute stressors and cortisol responses: A theoretical integration and synthesis of laboratory research. Psychol. Bull. 2004, 130, 355–391. [Google Scholar] [CrossRef]
- Gluck, M.E.; Geliebter, A.; Hung, J.; Yahav, E. Cortisol, hunger, and desire to binge eat following a cold stress test in obese women with binge eating disorder. Psychosom. Med. 2004, 66, 876–881. [Google Scholar] [CrossRef] [PubMed]
- Herhaus, B.; Ullmann, E.; Chrousos, G.; Petrowski, K. High/low cortisol reactivity and food intake in people with obesity and healthy weight. Transl. Psychiatry 2020, 10, 40. [Google Scholar] [CrossRef]
- Rosenberg, N.; Bloch, M.; Ben Avi, I.; Rouach, V.; Schreiber, S.; Stern, N.; Greenman, Y. Cortisol response and desire to binge following psychological stress: Comparison between obese subjects with and without binge eating disorder. Psychiatry Res. 2013, 208, 156–161. [Google Scholar] [CrossRef] [PubMed]
- Kirschbaum, C.; Pirke, K.M.; Hellhammer, D.H. The ’Trier Social Stress Test’—A tool for investigating psychobiological stress responses in a laboratory setting. Neuropsychobiology 1993, 28, 76–81. [Google Scholar] [CrossRef]
- Schulz, S.; Laessle, R.G. Stress-induced laboratory eating behavior in obese women with binge eating disorder. Appetite 2012, 58, 457–461. [Google Scholar] [CrossRef]
- Herhaus, B.; Passler, S.; Petrowski, K. Stress-related laboratory eating behavior in adults with obesity and healthy weight. Physiol. Behav. 2018, 196, 150–157. [Google Scholar] [CrossRef] [PubMed]
- Liang, J.; Matheson, B.E.; Kaye, W.H.; Boutelle, K.N. Neurocognitive correlates of obesity and obesity-related behaviors in children and adolescents. Int. J. Obes. 2014, 38, 494–506. [Google Scholar] [CrossRef]
- Verdejo-Garcia, A.; Moreno-Padilla, M.; Garcia-Rios, M.C.; Lopez-Torrecillas, F.; Delgado-Rico, E.; Schmidt-Rio-Valle, J.; Fernandez-Serrano, M.J. Social stress increases cortisol and hampers attention in adolescents with excess weight. PLoS ONE 2015, 10, e0123565. [Google Scholar] [CrossRef]
- Lu, Q.; Tao, F.; Hou, F.; Zhang, Z.; Sun, Y.; Xu, Y.; Xu, S.; Zhao, Y. Cortisol reactivity, delay discounting and percent body fat in Chinese urban young adolescents. Appetite 2014, 72, 13–20. [Google Scholar] [CrossRef]
- Messerli-Burgy, N.; Horsch, A.; Schindler, C.; Boichat, A.; Kriemler, S.; Munsch, S.; Crottet, B.; Marquez-Vidal, P.M.; Borghini, A.; Puder, J.J. Influence of Acute Physical Activity on Stress Reactivity in Obese and Normal Weight Children: A Randomized Controlled Trial. Obes. Facts 2019, 12, 115–130. [Google Scholar] [CrossRef]
- Moss, R.H.; Conner, M.; O’Connor, D.B. Exploring the effects of daily hassles on eating behaviour in children: The role of cortisol reactivity. Psychoneuroendocrinology 2020, 117, 104692. [Google Scholar] [CrossRef]
- World Health Organization. Growth Reference 5–19 Years—BMI-for-Age (5-19 Years). 2007. Available online: https://www.who.int/tools/growth-reference-data-for-5to19-years/indicators/bmi-for-age (accessed on 22 August 2021).
- Currie, C.; Nic Gabhainn, S.; Godeau, E.; International, H.N.C.C. The Health Behaviour in School-aged Children: WHO Collaborative Cross-National (HBSC) study: Origins, concept, history and development 1982–2008. Int. J. Public Health 2009, 54 (Suppl. 2), 131–139. [Google Scholar] [CrossRef]
- Cohen, S.; Kamarck, T.; Mermelstein, R. A global measure of perceived stress. J. Health Soc. Behav. 1983, 24, 385–396. [Google Scholar] [CrossRef]
- Khoury, J.E.; Gonzalez, A.; Levitan, R.D.; Pruessner, J.C.; Chopra, K.; Basile, V.S.; Masellis, M.; Goodwill, A.; Atkinson, L. Summary cortisol reactivity indicators: Interrelations and meaning. Neurobiol. Stress 2015, 2, 34–43. [Google Scholar] [CrossRef] [PubMed]
- George, S.A.; Khan, S.; Briggs, H.; Abelson, J.L. CRH-stimulated cortisol release and food intake in healthy, non-obese adults. Psychoneuroendocrinology 2010, 35, 607–612. [Google Scholar] [CrossRef]
- Newman, E.; O’Connor, D.B.; Conner, M. Daily hassles and eating behaviour: The role of cortisol reactivity status. Psychoneuroendocrinology 2007, 32, 125–132. [Google Scholar] [CrossRef] [PubMed]
- Appelhans, B.M.; Pagoto, S.L.; Peters, E.N.; Spring, B.J. HPA axis response to stress predicts short-term snack intake in obese women. Appetite 2010, 54, 217–220. [Google Scholar] [CrossRef] [PubMed]
- Cunningham, S.; Mazurka, R.; Wynne-Edwards, K.E.; Milev, R.V.; Pizzagalli, D.A.; Kennedy, S.; Harkness, K.L. Cortisol reactivity to stress predicts behavioral responsivity to reward moderation by sex, depression, and anhedonia. J. Affect. Disord. 2021, 293, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Mazurka, R.; Wynne-Edwards, K.E.; Harkness, K.L. Stressful Life Events Prior to Depression Onset and the Cortisol Response to Stress in Youth with First Onset Versus Recurrent Depression. J. Abnorm. Child Psychol. 2016, 44, 1173–1184. [Google Scholar] [CrossRef] [PubMed]
- Krishnaveni, G.V.; Jones, A.; Veena, S.R.; Somashekara, R.; Karat, S.C.; CH, D.F. Adiposity and Cortisol Response to Stress in Indian Adolescents. Indian Pediatr. 2018, 55, 125–130. [Google Scholar] [CrossRef] [PubMed]
- Dockray, S.; Susman, E.J.; Dorn, L.D. Depression, cortisol reactivity, and obesity in childhood and adolescence. J. Adolesc. Health 2009, 45, 344–350. [Google Scholar] [CrossRef]
- Campbell, J.; Ehlert, U. Acute psychosocial stress: Does the emotional stress response correspond with physiological responses? Psychoneuroendocrinology 2012, 37, 1111–1134. [Google Scholar] [CrossRef]

| Characteristics | Boys (N = 16) | Girls (N = 19) | p-Value |
|---|---|---|---|
| Sociodemographic parameters | |||
| Age | 15.6 ± 0.7 | 15.5 ± 0.6 | 0.739 |
| Mother’s education (high scool or less, %) | 50 | 57.1 | 0.606 |
| Father’s education (high scool or less, %) | 33.4 | 42.9 | 0.732 |
| How many people live in your house? (≥4, %) | 50 | 57.2 | 0.878 |
| Perceived family wealth (very well off and well off, %) | 87.5 | 94.7 | 0.453 |
| Anthropometric parameters | |||
| BMI (kg/m2) | 21.8 ± 3.6 | 21.52 ± 2.7 | 0.855 |
| Excess weight 1 (%/N) | 43.8 (7) | 21.1 (4) | 0.286 |
| Physical activity | |||
| Vigorous exercise 1 h (≥3 days/week, %) | 37.5 | 47.4 | 0.562 |
| Playing computer games (≥2 h/school day, %) | 14.3 | 58.3 | 0.106 |
| Watching TV (≥2 h/school day, %) | 60 | 68.4 | 0.071 |
| General health and well-being | |||
| Self-rated health (excellent and good, %) | 50 | 26,3 | 0.155 |
| Multiple complaints (≥2 complaints/week, %) | 100 | 94.7 | 0.359 |
| Perceived stress | |||
| Pre-test score (mean ± SD, median) | 21.09 ± 7.37 (23) | 24,81 ± 6,19 | 0.167 |
| Post-test score (mean ± SD, median) | 29.97 ± 7.34(31) | 31,76 ± 5,49 | 0.231 |
| Cortisol reactivity to TSST Salivary cortisol (nmol/L) | |||
| T0 (before experiment) | 4.3 ± 2.9 | 5.8 ± 3.3 | 0.145 |
| T5 (after the 1st digital test) | 10.4 ± 10.6 | 10.5 ± 9.3 | 0.655 |
| T10 (after the 2nd digital test) | 27.1 ± 28.0 | 26.1 ± 23.7 | 0.947 |
| T15 (after the 3rd digital test) | 25.1 ± 27.5 | 36.3 ± 31.4 | 0.246 |
| T40 (after 25 min of recovery) | 12.6 ± 9.7 | 25.5 ± 20.1 | 0.020 * |
| Area under the curve, AUGg | 690.1 ± 658.2 | 1087.8 ± 813.6 | 0.091 |
| Food Consumption | Hyporeactive (N = 17) | Hyperreactive (N = 18) | p-Value |
|---|---|---|---|
| Snack frequency (>3 daily) (%) | 5.9 | 22.2 | 0.174 |
| Snack frequency (>6 daily) (%) | 11.8 | 5.6 | 0.303 |
| Fruit consumption (daily) (%) | 35.3 | 16.7 | 0.214 |
| Vegetable consumption (daily) (%) | 29.4 | 44.4 | 0.365 |
| Consumption of sweets (daily) (%) | 5.9 | 16.7 | 0.323 |
| Soft drink consumption (daily) (%) | 0 | 27.8 | 0.021 * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gotca, I.; Druica, A.; Timofte, D.V.; Preda, C.; Anton-Paduraru, D.-T.; Ghiciuc, C.M.; Ungureanu, M.C.; Leustean, L.; Mocanu, V. Cortisol Reactivity to a Digital Version of Trier Social Stress Test and Eating Behavior in Non-Overweight and Overweight Adolescents: A Pilot Study. Appl. Sci. 2021, 11, 9683. https://doi.org/10.3390/app11209683
Gotca I, Druica A, Timofte DV, Preda C, Anton-Paduraru D-T, Ghiciuc CM, Ungureanu MC, Leustean L, Mocanu V. Cortisol Reactivity to a Digital Version of Trier Social Stress Test and Eating Behavior in Non-Overweight and Overweight Adolescents: A Pilot Study. Applied Sciences. 2021; 11(20):9683. https://doi.org/10.3390/app11209683
Chicago/Turabian StyleGotca, Ioan, Andrada Druica, Daniel V. Timofte, Cristina Preda, Dana-Teodora Anton-Paduraru, Cristina Mihaela Ghiciuc, Maria Christina Ungureanu, Letitia Leustean, and Veronica Mocanu. 2021. "Cortisol Reactivity to a Digital Version of Trier Social Stress Test and Eating Behavior in Non-Overweight and Overweight Adolescents: A Pilot Study" Applied Sciences 11, no. 20: 9683. https://doi.org/10.3390/app11209683
APA StyleGotca, I., Druica, A., Timofte, D. V., Preda, C., Anton-Paduraru, D.-T., Ghiciuc, C. M., Ungureanu, M. C., Leustean, L., & Mocanu, V. (2021). Cortisol Reactivity to a Digital Version of Trier Social Stress Test and Eating Behavior in Non-Overweight and Overweight Adolescents: A Pilot Study. Applied Sciences, 11(20), 9683. https://doi.org/10.3390/app11209683










