Biomechanical Comparison of Fixation Stability among Various Pedicle Screw Geometries: Effects of Screw Outer/Inner Projection Shape and Thread Profile
Abstract
:1. Introduction
2. Materials and Methods
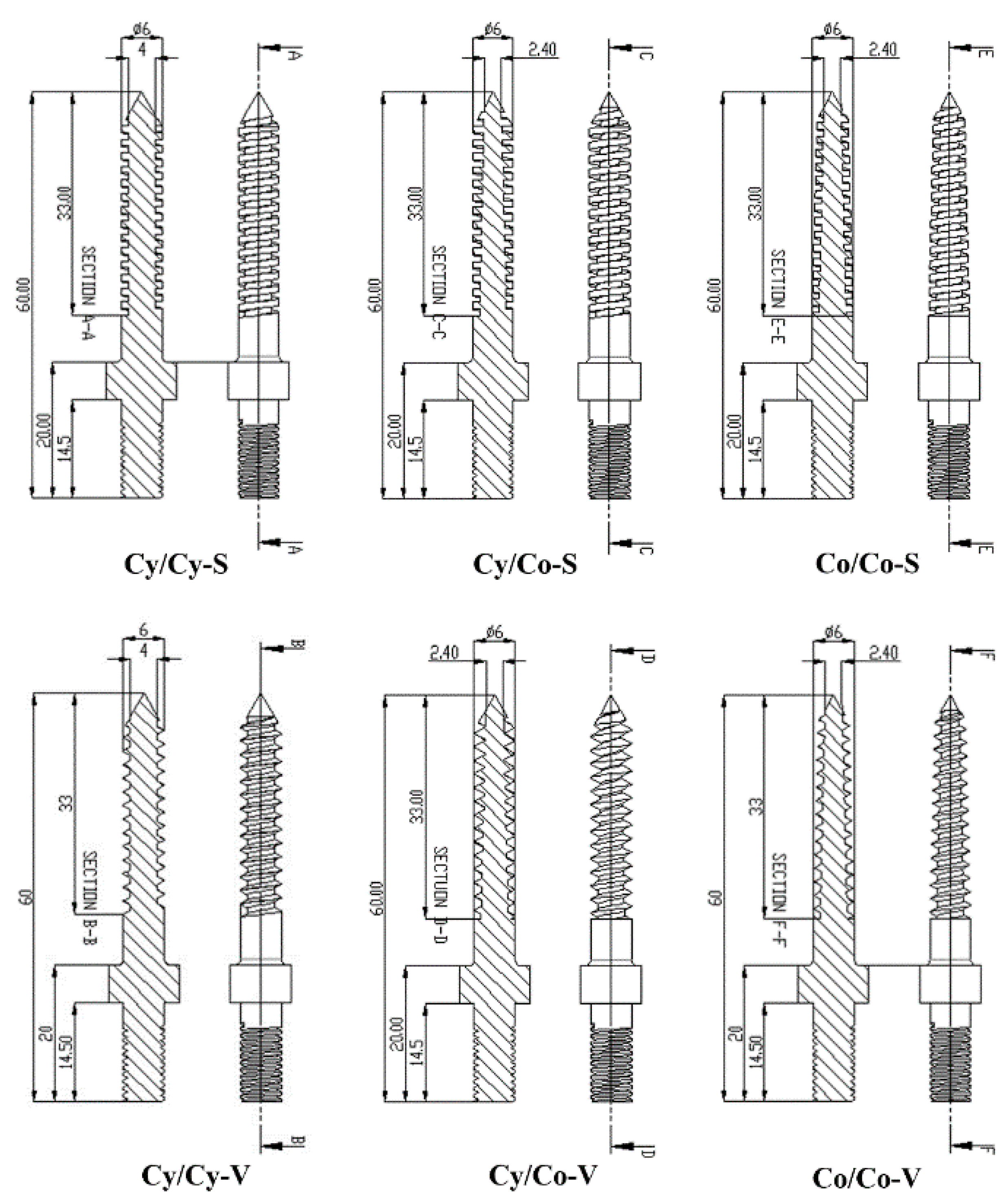
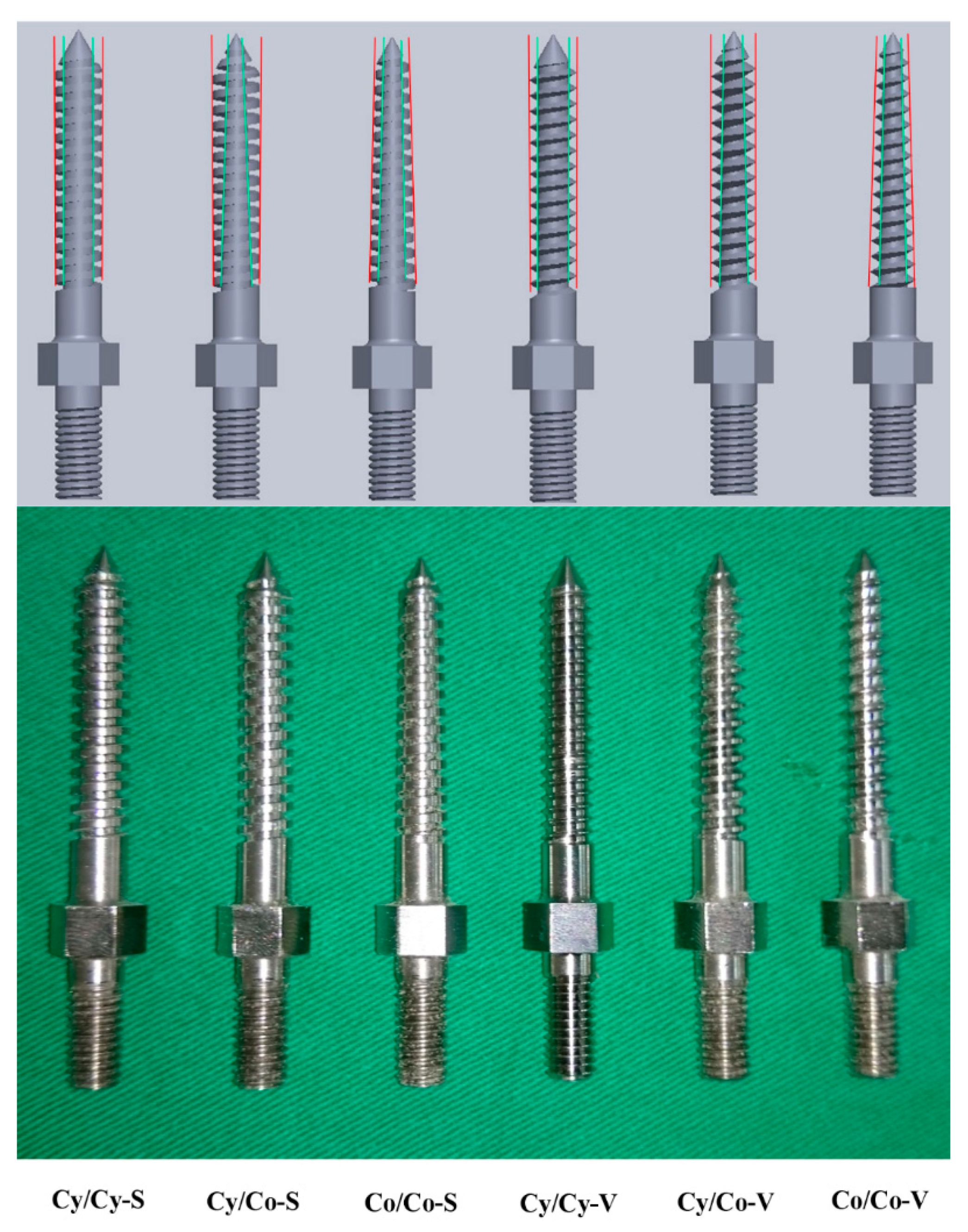
2.1. Pedicle Screw Geometries
2.2. Test Blocks
2.3. Specimen Preparation
2.3.1. Comparison of Different Bone Mineral Densities
2.3.2. Comparison of Different Pilot-Hole Sizes
2.4. Biomechanical Testing
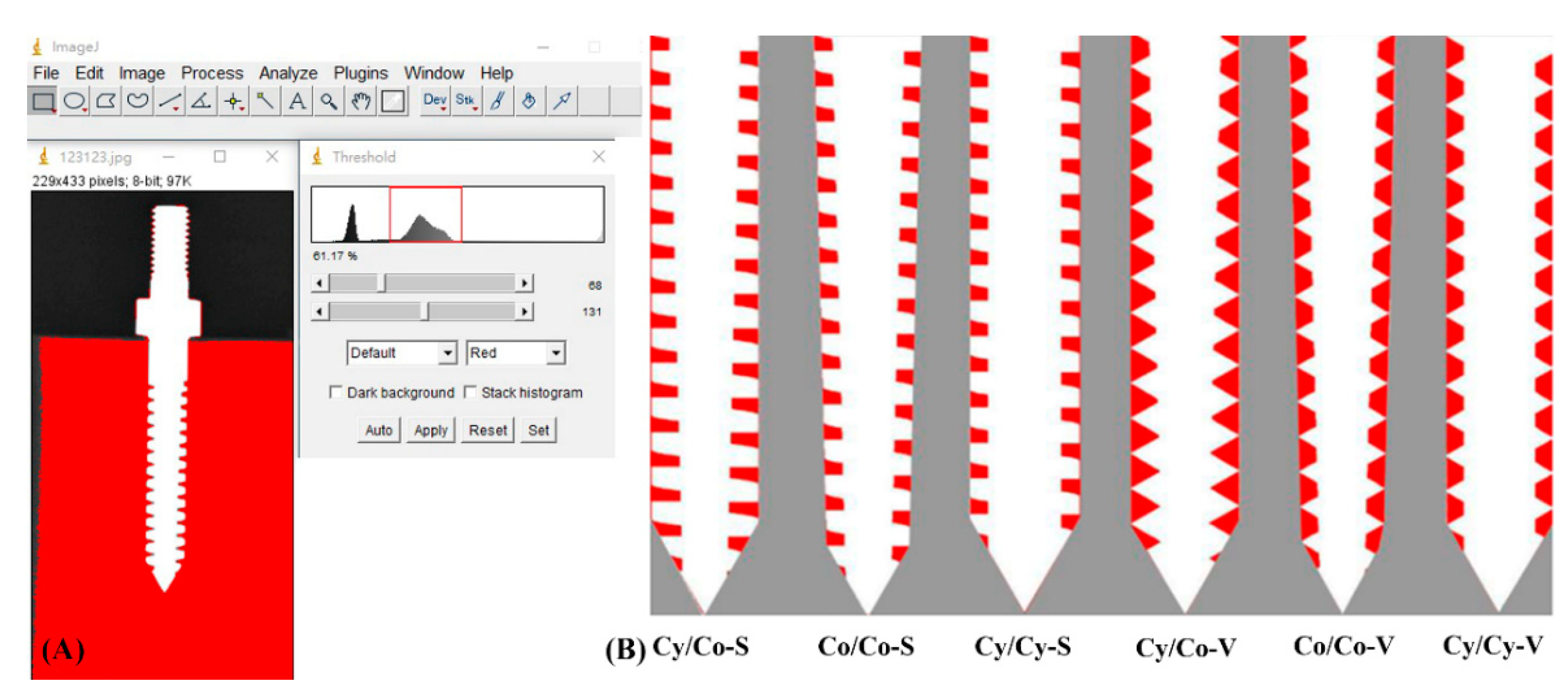
2.5. Quantification of the Embedded Bone Volume (EBV)
2.6. Statistical Analysis
3. Results
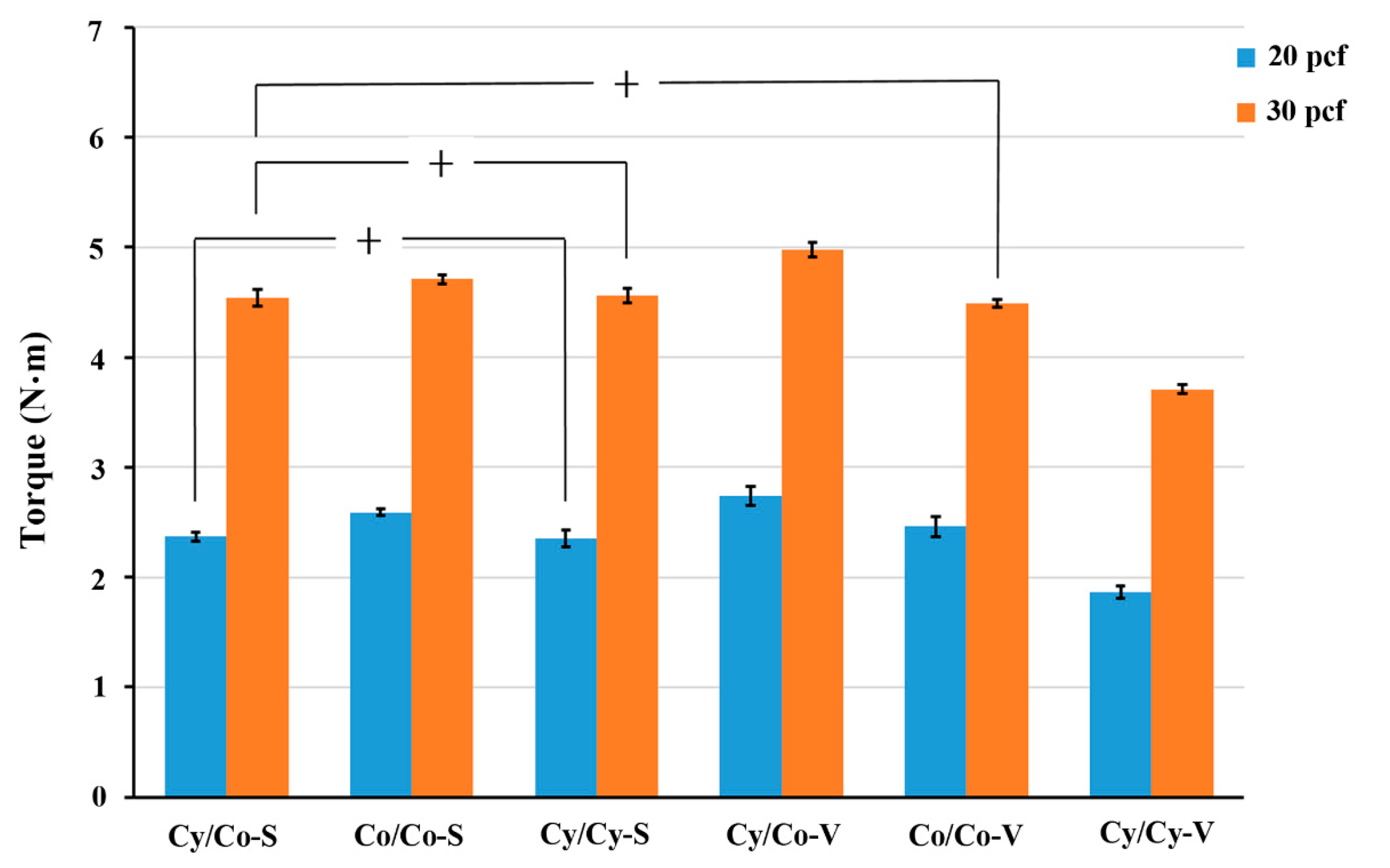
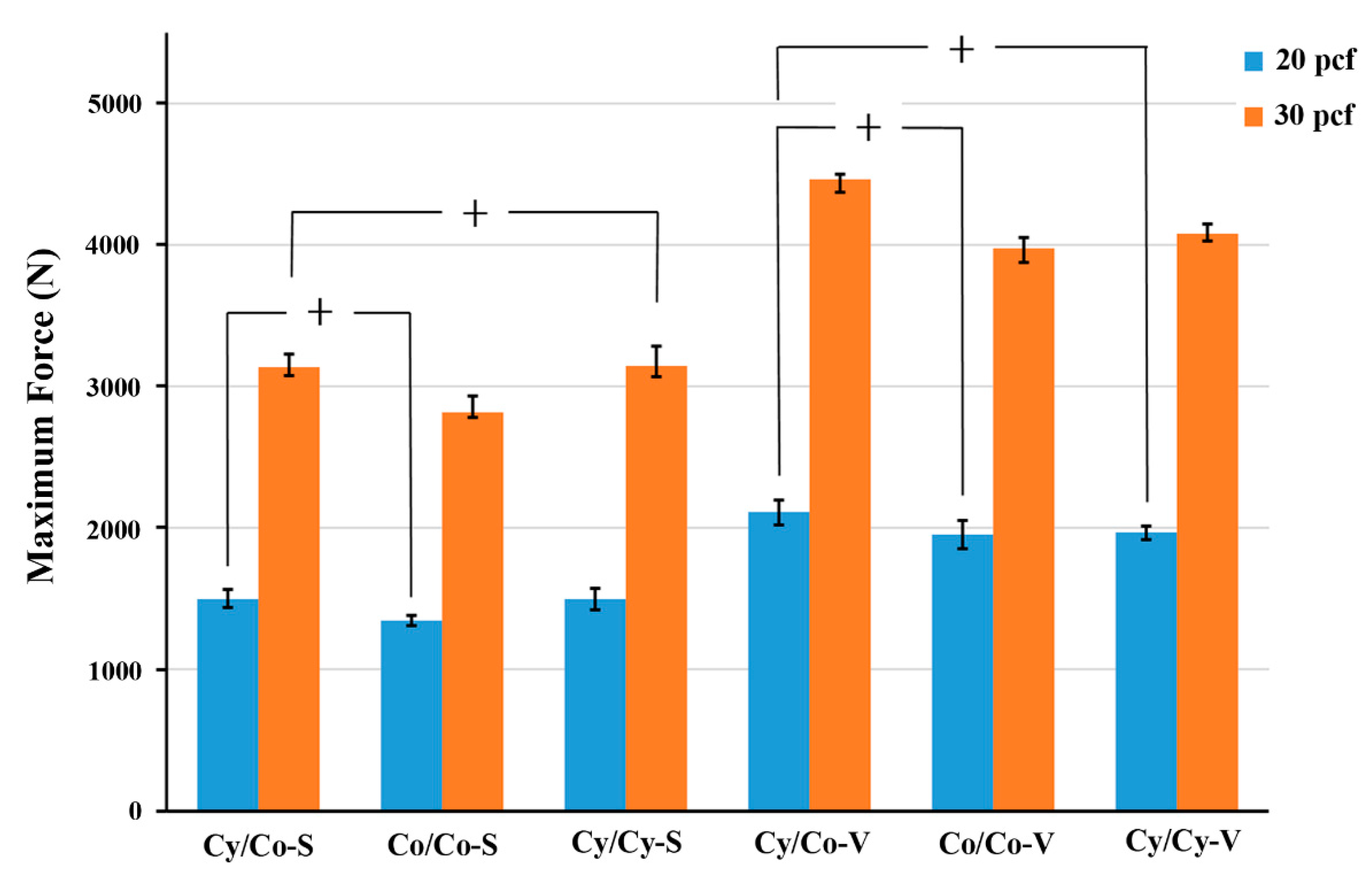
3.1. Effect of Bone Density (Using 3.7-mm Pilot Holes)
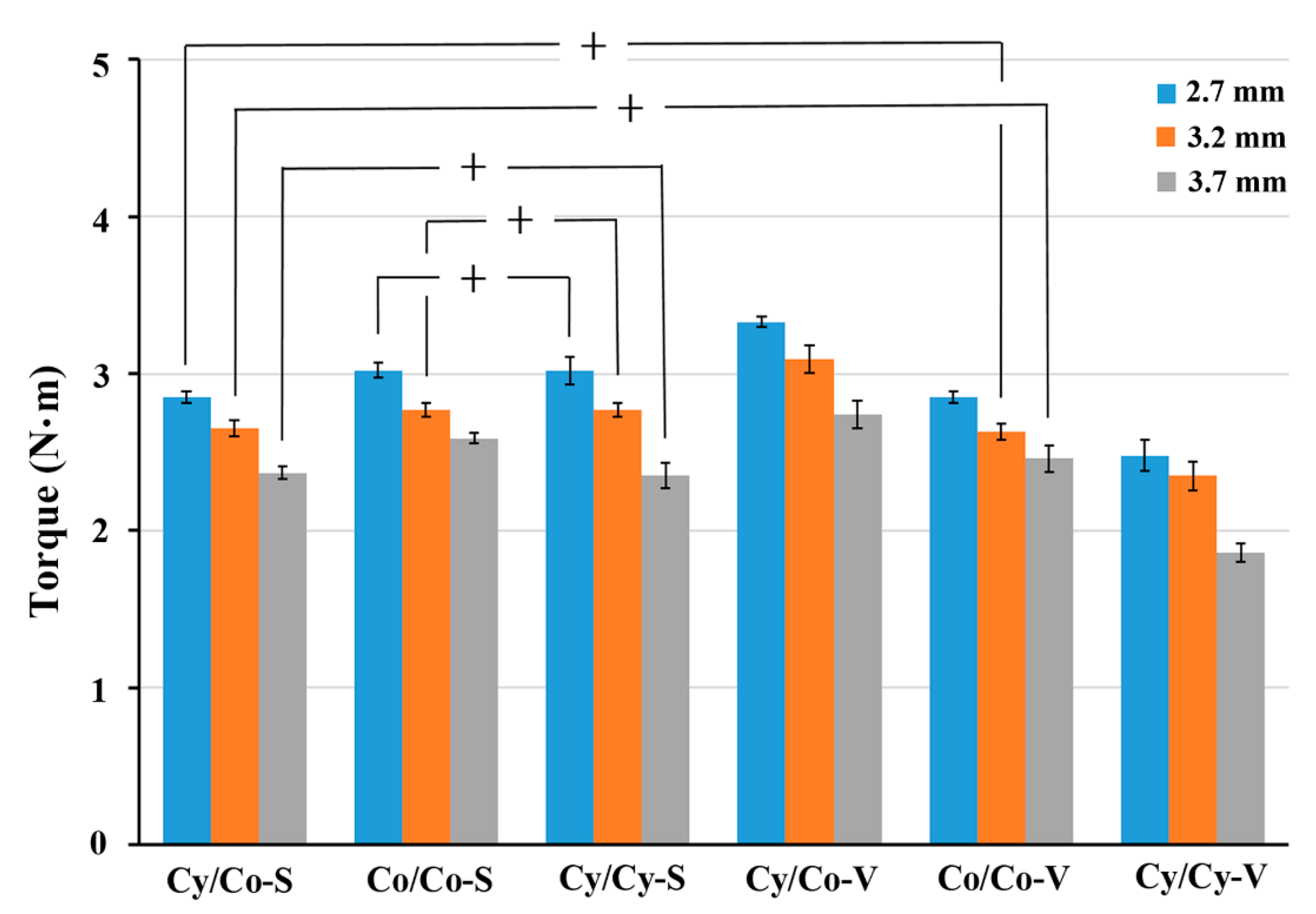
3.2. Effect of Pilot-Hole Size (Using 20-Pcf Test Blocks)
3.3. Embedded Bone Volume (EBV)
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ohrt-Nissen, S.; Dahl, B.; Gehrchen, M. Choice of rods in surgical treatment of adolescent idiopathic scoliosis: What are the clinical implications of biomechanical properties?—A review of the literature. Neurospine 2018, 15, 123–130. [Google Scholar] [CrossRef] [Green Version]
- Tsirikos, A.I. Correction of Adolescent Idiopathic Scoliosis Using a Convex Pedicle Screw Technique: A Novel Technique for Deformity Correction. JBJS Essent. Surg. Tech. 2019, 9, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Suk, S.I.L.; Kim, J.H.; Kim, S.S.; Lim, D.J. Pedicle screw instrumentation in adolescent idiopathic scoliosis (AIS). Eur. Spine J. 2012, 21, 13–22. [Google Scholar] [CrossRef] [Green Version]
- Nouh, M.R. Spinal fusion-hardware construct: Basic concepts and imaging review. World J. Radiol. 2012, 4, 193–207. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Frost, B.A.; Camarero-Espinosa, S.; Johan-Foster, E. Materials for the spine: Anatomy, problems, and solutions. Materials 2019, 12, 253. [Google Scholar] [CrossRef] [Green Version]
- Obid, P.; Danyali, R.; Kueny, R.; Huber, G.; Reichl, M.; Richter, A.; Niemeyer, T.; Morlock, M.; Püschel, K.; Übeyli, H. Hybrid Instrumentation in Lumbar Spinal Fusion: A Biomechanical Evaluation of Three Different Instrumentation Techniques. Glob. Spine J. 2017, 7, 47–53. [Google Scholar] [CrossRef] [Green Version]
- Reichl, M.; Kueny, R.A.; Danyali, R.; Obid, P. Biomechanical Effects of a Dynamic Topping off Instrumentation in a Long Rigid Pedicle Screw Construct. Clin. Spine Surg. 2017, 30, E440–E447. [Google Scholar] [CrossRef] [PubMed]
- Lamerain, M.; Bachy, M.; Delpont, M.; Kabbaj, R.; Mary, P.; Vialle, R. CoCr rods provide better frontal correction of adolescent idiopathic scoliosis treated by all-pedicle screw fixation. Eur. Spine J. 2014, 23, 1190–1196. [Google Scholar] [CrossRef]
- Murphy, M.E.; Gilder, H.; Maloney, P.R.; McCutcheon, B.A.; Rinaldo, L.; Shepherd, D.; Kerezoudis, P.; Ubl, D.S.; Crowson, C.S.; Krauss, W.E.; et al. Lumbar decompression in the elderly: Increased age as a risk factor for complications and nonhome discharge. J. Neurosurg. Spine. 2017, 26, 353–362. [Google Scholar] [CrossRef] [Green Version]
- Turcotte, J.J.; Patton, C.M. Predictors of Postoperative Complications After Surgery for Lumbar Spinal Stenosis and Degenerative Lumbar Spondylolisthesis. J. Am. Acad. Orthop. Surg. Glob. Res. Rev. 2018, 2, e085. [Google Scholar] [CrossRef]
- Reid, J.J.; Johnson, J.S.; Wang, J.C. Challenges to bone formation in spinal fusion. J. Biomech. 2011, 44, 213–220. [Google Scholar] [CrossRef]
- Gruskay, J.A.; Webb, M.L.; Grauer, J.N. Methods of evaluating lumbar and cervical fusion. Spine J. 2014, 14, 531–539. [Google Scholar] [CrossRef]
- Chun, D.S.; Baker, K.C.; Hsu, W.K. Lumbar pseudarthrosis: A review of current diagnosis and treatment. Neurosurg. Focus 2015, 39, E10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Meng, B.; Bunch, J.; Burton, D.; Wang, J. Lumbar interbody fusion: Recent advances in surgical techniques and bone healing strategies. Eur. Spine J. 2021, 30, 22–33. [Google Scholar] [CrossRef] [PubMed]
- Pfeiffer, F.M.; Abernathie, D.L. A comparison of pullout strength for pedicle screws of different designs: A study using tapped and untapped pilot holes. Spine 2006, 31, E867–E870. [Google Scholar] [CrossRef] [PubMed]
- Ricci, W.M.; Tornetta, P.; Petteys, T.; Gerlach, D. A comparison of screw insertion torque and pullout strength. J. Orthop. Trauma 2010, 24, 374–378. [Google Scholar] [CrossRef] [Green Version]
- Addevico, F.; Morandi, M.; Scaglione, M.; Solitro, G.F. Screw insertion torque as parameter to judge the fixation. Assessment of torque and pull-out strength in different bone densities and screw-pitches. Clin. Biomech. 2020, 72, 130–135. [Google Scholar] [CrossRef] [PubMed]
- Amirouche, F.; Solitro, G.F.; Magnan, B.P. Stability and Spine Pedicle Screws Fixation Strength—A Comparative Study of Bone Density and Insertion Angle. Spine Deform. 2016, 4, 261–267. [Google Scholar] [CrossRef]
- Shah, A.H.; Behrents, R.G.; Kim, K.B.; Kyung, H.-M.; Buschang, P.H. Effects of screw and host factors on insertion torque and pullout strength. Angle Orthod. 2012, 82, 603–610. [Google Scholar] [CrossRef]
- Battula, S.; Schoenfeld, A.J.; Sahai, V.; Vrabec, G.A.; Tank, J.; Njus, G.O. The effect of pilot hole size on the insertion torque and pullout strength of self-tapping cortical bone screws in osteoporotic bone. J. Trauma 2008, 64, 990–995. [Google Scholar] [CrossRef] [Green Version]
- Kim, Y.Y.; Choi, W.S.; Rhyu, K.W. Assessment of pedicle screw pullout strength based on various screw designs and bone densities—An ex vivo biomechanical study. Spine J. 2012, 12, 164–168. [Google Scholar] [CrossRef]
- Defino, H.L.A.; Miranda, R.F.; Pinheiro, R.P.; Shimano, A. Influence of diameter and geometry in the tapping of the pilot hole in pedicle screws. Coluna/Columna 2019, 18, 51–54. [Google Scholar] [CrossRef] [Green Version]
- Zdero, R.; Olsen, M.; Bougherara, H.; Schemitsch, E.H. Cancellous bone screw purchase: A comparison of synthetic femurs, human femurs, and finite element analysis. Proc. Inst. Mech. Eng. Part H J. Eng. Mech. 2008, 222, 1175–1183. [Google Scholar] [CrossRef] [PubMed]
- Shea, T.M.; Laun, J.; Gonzalez-Blohm, S.A.; Doulgeris, J.J.; Lee, W.E.; Aghayev, K.; Vrionis, F.D. Designs and Techniques That Improve the Pullout Strength of Pedicle Screws in Osteoporotic Vertebrae: Current Status. BioMed Res. Int. 2014, 2014. [Google Scholar] [CrossRef] [PubMed]
- Varghese, V.; Saravana Kumar, G.; Krishnan, V. Effect of various factors on pull out strength of pedicle screw in normal and osteoporotic cancellous bone models. Med. Eng. Phys. 2017, 40, 28–38. [Google Scholar] [CrossRef]
- ASTM F1839-08 (2016) Standard Specification for Rigid Polyurethane Foam for Use as a Standard Material for Testing Orthopaedic Devices and Instruments. Available online: https://www.astm.org/Standards/F1839.htm (accessed on 2 April 2020).
- Chen, L.H.; Tai, C.L.; Lee, D.M.; Lai, P.L.; Lee, Y.C.; Niu, C.C.; Chen, W.J. Pullout strength of pedicle screws with cement augmentation in severe osteoporosis: A comparative study between cannulated screws with cement injection and solid screws with cement pre-filling. BMC Musculoskelet. Disord. 2011, 12, 33. [Google Scholar] [CrossRef] [Green Version]
- Liu, M.Y.; Tsai, T.T.; Lai, P.L.; Hsieh, M.K.; Chen, L.H.; Tai, C.L. Biomechanical comparison of pedicle screw fixation strength in synthetic bones: Effects of screw shape, core/thread profile and cement augmentation. PLoS ONE 2020, 15, e0229328. [Google Scholar] [CrossRef]
- Hsieh, M.K.; Liu, M.Y.; Chen, J.K.; Tsai, T.T.; Lai, P.L.; Niu, C.C.; Tai, C.L. Biomechanical study of the fixation stability of broken pedicle screws and subsequent strategies. PLoS ONE 2019, 14, e0219189. [Google Scholar] [CrossRef]
- Cho, W.; Cho, S.K.; Wu, C. The biomechanics of pedicle screw-based instrumentation. J. Bone Jt. Surg-Ser. B. 2010, 92, 1061–1065. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ono, A.; Brown, M.D.; Latta, L.L.; Milne, E.L.; Holmes, D.C. Triangulated pedicle screw construct technique and pull-out strength of conical and cylindrical screws. J. Spinal Disord. 2001, 14, 323–329. [Google Scholar] [CrossRef]
- Abshire, B.B.; McLain, R.F.; Valdevit, A.; Kambic, H.E. Characteristics of pullout failure in conical and cylindrical pedicle screws after full insertion and back-out. Spine J. 2001, 1, 408–414. [Google Scholar] [CrossRef]
- Chao, C.K.; Hsu, C.C.; Wang, J.L.; Lin, J. Increasing Bending Strength and Pullout Strength in Conical Pedicle Screws: Biomechanical Tests and Finite Element Analyses. J. Spinal Disord. Tech. 2008, 21, 130–138. [Google Scholar] [CrossRef] [Green Version]
- Hsu, C.C.; Chao, C.K.; Wang, J.L.; Hou, S.M.; Tsai, Y.T.; Lin, J. Increase of pullout strength of spinal pedicle screws with conical core: Biomechanical tests and finite element analyses. J. Orthop. Res. 2005, 23, 788–794. [Google Scholar] [CrossRef] [PubMed]
- Krenn, M.H.; Piotrowski, W.P.; Penzkofer, R.; Augat, P. Influence of thread design on pedicle screw fixation. Laboratory investigation. J. Neurosurg. Spine 2008, 9, 90–95. [Google Scholar] [CrossRef]
- Kimura, H.; Shikata, J.; Odate, S.; Soeda, T.; Yamamura, S. Risk factors for cage retropulsion after posterior lumbar interbody fusion: Analysis of 1070 cases. Spine 2012, 37, 1164–1169. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, D.Y.; Park, Y.J.; Song, S.Y.; Jeong, S.T.; Kim, D.H. Risk Factors for Posterior Cage Migration after Lumbar Interbody Fusion Surgery. Asian Spine J. 2018, 12, 59–68. [Google Scholar] [CrossRef] [Green Version]



Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hsieh, M.-K.; Li, Y.-D.; Liu, M.-Y.; Lin, C.-X.; Tsai, T.-T.; Lai, P.-L.; Tai, C.-L. Biomechanical Comparison of Fixation Stability among Various Pedicle Screw Geometries: Effects of Screw Outer/Inner Projection Shape and Thread Profile. Appl. Sci. 2021, 11, 9901. https://doi.org/10.3390/app11219901
Hsieh M-K, Li Y-D, Liu M-Y, Lin C-X, Tsai T-T, Lai P-L, Tai C-L. Biomechanical Comparison of Fixation Stability among Various Pedicle Screw Geometries: Effects of Screw Outer/Inner Projection Shape and Thread Profile. Applied Sciences. 2021; 11(21):9901. https://doi.org/10.3390/app11219901
Chicago/Turabian StyleHsieh, Ming-Kai, Yun-Da Li, Mu-Yi Liu, Chen-Xue Lin, Tsung-Ting Tsai, Po-Liang Lai, and Ching-Lung Tai. 2021. "Biomechanical Comparison of Fixation Stability among Various Pedicle Screw Geometries: Effects of Screw Outer/Inner Projection Shape and Thread Profile" Applied Sciences 11, no. 21: 9901. https://doi.org/10.3390/app11219901





