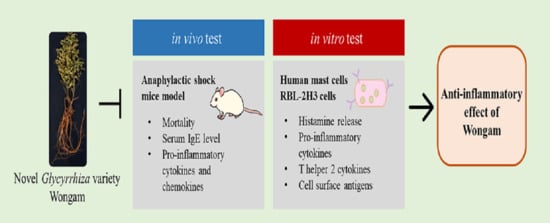
Anti-Inflammatory Effects of Novel Glycyrrhiza Variety Wongam In Vivo and In Vitro
Abstract
:1. Introduction
2. Materials and Methods
2.1. Chemicals and Reagents
2.2. Sample Preparation
2.3. Compound-48/80-Induced Anaphylactic Shock Model
2.4. IgE and Cytokine Assays
2.5. Reverse Transcription–Quantitative Polymerase Chain Reaction Analysis
2.6. HMC-1 Cell Culture and WG Treatment
2.7. RBL-2H3 Cell Sensitization and Stimulation
2.8. Cell Viability Assay
2.9. Histamine Assay
2.10. Western Blot Analysis
2.11. Statistical Analysis
3. Results
3.1. WG Protects against Mortality and Decreases IgE Levels in Compound-48/80-Induced Anaphylactic Shock Mice Model
3.2. WG Inhibits the Production of ProInflammatory Cytokines and Chemokines in the Mouse Model of Anaphylaxis
3.3. WG Inhibits ERK Activation in Mouse Model of Anaphylaxis
3.4. WG Suppresses Mast Cell Degranulation from HMC-1 and RBL-2H3 Cells
3.5. WG Inhibits the Expression Levels of ProInflammatory Cytokines from HMC-1 and RBL-2H3 Cells
3.6. WG Downregulates the Expression Levels of Chemokines, Cell Surface Antigens, and Th2 Cytokines in PMACI-Stimulated HMC-1 Cells
3.7. WG Inhibits the Activation of MAPKs and NF-κB Signaling Pathway in PMACI-Stimulated HMC-1 Cells
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
References
- Kim, D.-G.; Lee, J.; Kim, W.; An, H.-J.; Lee, J.-H.; Chang, J.; Kang, S.-H.; Song, Y.-J.; Jeon, Y.-D.; Jin, J.-S. Assessment of General Toxicity of the Glycyrrhiza New Variety Extract in Rats. Plants 2021, 10, 1126. [Google Scholar] [CrossRef] [PubMed]
- Song, Y.-J.; Kim, D.-G.; Lee, J.; Kim, W.; An, H.-J.; Lee, J.-H.; Jeon, Y.-D.; Chang, J.; Kang, S.-H.; Soh, J.-R.; et al. In Vitro Genotoxicity Assessment from the Glycyrrhiza New Variety Extract. Appl. Sci. 2021, 11, 10257. [Google Scholar] [CrossRef]
- Kang, S.-H.; Song, Y.-J.; Jeon, Y.-D.; Kim, D.-K.; Park, J.-H.; Soh, J.-R.; Lee, J.-H.; Kitalong, C.; Kim, W.; An, H.-J.; et al. Comparative Study of Anti-Inflammatory Effect on DSS-Induced Ulcerative Colitis Between Novel Glycyrrhiza Variety and Official Compendia. Appl. Sci. 2021, 11, 1545. [Google Scholar] [CrossRef]
- Pastorino, G.; Cornara, L.; Soares, S.; Rodrigues, F.; Oliveira, M.B.P. Liquorice (Glycyrrhiza glabra): A phytochemical and pharmacological review. Phytother. Res. 2018, 32, 2323–2339. [Google Scholar] [CrossRef] [PubMed]
- Shin, Y.-W.; Bae, E.-A.; Lee, B.; Lee, S.H.; Kim, J.A.; Kim, Y.-S.; Kim, D.-H. In Vitro and In Vivo Antiallergic Effects of Glycyrrhiza glabra and Its Components. Planta Med. 2007, 73, 257–261. [Google Scholar] [CrossRef]
- Yang, R.; Yuan, B.-C.; Ma, Y.-S.; Zhou, S.; Liu, Y. The anti-inflammatory activity of licorice, a widely used Chinese herb. Pharm. Biol. 2016, 55, 5–18. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, S.-H.; Hong, J.-H.; Lee, J.-E.; Lee, Y.-C. 18β-Glycyrrhetinic acid, the major bioactive component of Glycyrrhizae Radix, attenuates airway inflammation by modulating Th2 cytokines, GATA-3, STAT6, and Foxp3 transcription factors in an asthmatic mouse model. Environ. Toxicol. Pharmacol. 2017, 52, 99–113. [Google Scholar] [CrossRef] [PubMed]
- Fiore, C.; Eisenhut, M.; Krausse, R.; Ragazzi, E.; Pellati, D.; Armanini, D.; Bielenberg, J. Antiviral effects of Glycyrrhiza species. Phytother. Res. 2008, 22, 141–148. [Google Scholar] [CrossRef]
- Dong, S.; Inoue, A.; Zhu, Y.; Tanji, M.; Kiyama, R. Activation of rapid signaling pathways and the subsequent transcriptional regulation for the proliferation of breast cancer MCF-7 cells by the treatment with an extract of Glycyrrhiza glabra root. Food Chem. Toxicol. 2007, 45, 2470–2478. [Google Scholar] [CrossRef]
- Wang, W.; Hu, X.; Zhao, Z.; Liu, P.; Hu, Y.; Zhou, J.; Zhou, D.; Wang, Z.; Guo, D.; Guo, H. Antidepressant-like effects of liquiritin and isoliquiritin from Glycyrrhiza uralensis in the forced swimming test and tail suspension test in mice. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2008, 32, 1179–1184. [Google Scholar] [CrossRef]
- Pawankar, R. Allergic diseases and asthma: A global public health concern and a call to action. World Allergy Organ. J. 2014, 7, 1–12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Altrichter, S.; Kriehuber, E.; Moser, J.; Valenta, R.; Kopp, T.; Stingl, G. Serum IgE Autoantibodies Target Keratinocytes in Patients with Atopic Dermatitis. J. Investig. Dermatol. 2008, 128, 2232–2239. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, Q.; Lepus, C.M.; Raghu, H.; Reber, L.L.; Tsai, M.M.; Wong, H.H.; von Kaeppler, E.; Lingampalli, N.; Bloom, M.S.; Hu, N.; et al. IgE-mediated mast cell activation promotes inflammation and cartilage destruction in osteoarthritis. Elife 2019, 8, e39905. [Google Scholar] [CrossRef]
- Corry, D.B.; Kheradmand, F. Induction and regulation of the IgE response. Nature 1999, 402, 18–23. [Google Scholar] [CrossRef]
- Kraft, S.; Jouvin, M.H.; Kulkarni, N.; Kissing, S.; Morgan, E.S.; Dvorak, A.M.; Schroder, B.; Saftig, P.; Kinet, J.P. The tetraspanin CD63 is required for efficient IgE-mediated mast cell degranulation and anaphylaxis. J. Immunol. 2013, 191, 2871–2878. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Metcalfe, D.D.; Pawankar, R.; Ackerman, S.J.; Akin, C.; Clayton, F.; Falcone, F.H.; Gleich, G.J.; Irani, A.-M.; Johansson, M.W.; Klion, A.D.; et al. Biomarkers of the involvement of mast cells, basophils and eosinophils in asthma and allergic diseases. World Allergy Organ. J. 2016, 9, 7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vantur, R.; Rihar, M.; Koren, A.; Rijavec, M.; Kopac, P.; Bidovec-Stojkovic, U.; Erzen, R.; Korosec, P. Chemokines during anaphylaxis: The importance of CCL2 and CCL2-dependent chemotactic activity for basophils. Clin. Transl. Allergy 2020, 10, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Song, E.-H.; Chung, K.-S.; Kang, Y.-M.; Lee, J.-H.; Lee, M.; An, H.-J. Eupatilin suppresses the allergic inflammatory response in vitro and in vivo. Phytomedicine 2018, 42, 1–8. [Google Scholar] [CrossRef]
- Yang, E.-J.; Song, I.-S.; Song, K.-S. Ethanol extract of Glycyrrhizae Radix modulates the responses of antigen-specific splenocytes in experimental autoimmune encephalomyelitis. Phytomedicine 2019, 54, 56–65. [Google Scholar] [CrossRef]
- Yamamura, Y.; Santa, T.; Kotaki, H.; Uchino, K.; Sawada, Y.; Iga, T. Administration-Route Dependency of Absorption of Glycyrrhizin in Rats: Intraperitoneal Administration Dramatically Enhanced Bioavailability. Biol. Pharm. Bull. 1995, 18, 337–341. [Google Scholar] [CrossRef] [Green Version]
- Lloyd, C. Chemokines in allergic lung inflammation. Immunology 2002, 105, 144–154. [Google Scholar] [CrossRef] [PubMed]
- Castan, L.; Magnan, A.; Bouchaud, G. Chemokine receptors in allergic diseases. Allergy 2016, 72, 682–690. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- MacGlashan, D. Expression of CD203c and CD63 in human basophils: Relationship to differential regulation of piecemeal and anaphylactic degranulation processes. Clin. Exp. Allergy 2010, 40, 1365–1377. [Google Scholar] [CrossRef] [Green Version]
- Han, S.; Sun, L.; He, F.; Che, H. Anti-allergic activity of glycyrrhizic acid on IgE-mediated allergic reaction by regulation of allergy-related immune cells. Sci. Rep. 2017, 7, 7222. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shin, E.M.; Zhou, H.Y.; Guo, L.Y.; Kim, J.A.; Lee, S.H.; Merfort, I.; Kang, S.S.; Kim, H.S.; Kim, S.; Kim, Y.S. Anti-inflammatory effects of glycyrol isolated from Glycyrrhiza uralensis in LPS-stimulated RAW264.7 macrophages. Int. Immunopharmacol. 2008, 8, 1524–1532. [Google Scholar] [CrossRef]
- Krystel-Whittemore, M.; Dileepan, K.N.; Wood, J.G. Mast Cell: A Multi-Functional Master Cell. Front. Immunol. 2016, 6, 620. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Matsui, N.; Ito, D.; Takabatake, Y.; Nashioka, E.; Tada, S.; Kanagawa, M.; Fukuishi, N.; Akagi, M. Compound 48/80, a Mast Cell Stimulator, Enhances Synthesis of IgE and IgG Induced by Intranasal Application of Ovalbumin in Mice. Biol. Pharm. Bull. 2015, 38, 1954–1959. [Google Scholar] [CrossRef] [PubMed]
- Rothschild, A.M. Mechanisms of histamine release by compound 48/80. Br. J. Pharmacol. 1970, 38, 253–262. [Google Scholar] [CrossRef] [Green Version]
- Amin, K. The role of mast cells in allergic inflammation. Respir. Med. 2012, 106, 9–14. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Galli, S.J.; Tsai, M. IgE and mast cells in allergic disease. Nat. Med. 2012, 18, 693–704. [Google Scholar] [CrossRef] [Green Version]
- Norris, A.A. Pharmacology of sodium cromoglycate. Clin. Exp. Allergy 1996, 26, 5–7. [Google Scholar] [CrossRef] [PubMed]
- Kimata, H.; Yoshida, A.; Ishioka, C.; Mikawa, H. Disodium cromoglycate (DSCG) selectively inhibits IgE production and enhances IgG4 production by human B cell in vitro. Clin. Exp. Immunol. 1991, 84, 395–399. [Google Scholar] [PubMed]
- Kang, J.A.; Song, H.-Y.; Byun, E.-H.; Ahn, N.-G.; Kim, H.-M.; Nam, Y.R.; Lee, G.H.; Jang, B.-S.; Choi, D.S.; Lee, D.-E. Gamma-irradiated black ginseng extract inhibits mast cell degranulation and suppresses atopic dermatitis-like skin lesions in mice. Food Chem. Toxicol. 2018, 111, 133–143. [Google Scholar] [CrossRef] [PubMed]
- Liu, Z.; Zhong, J.-Y.; Gao, E.-N.; Yang, H. Effects of glycyrrhizin acid and licorice flavonoids on LPS-induced cytokines expression in macrophage. China J. Chin. Mater. Med. 2014, 39, 3841–3845. [Google Scholar]
- Panahi, Y.; Fakhari, S.; Mohammadi, M.; Rahmani, M.R.; Hakhamaneshi, M.S.; Jalili, A. Glycyrrhizin down-regulates CCL2 and CXCL2 expression in cerulein-stimulated pancreatic acinar cells. Am. J. Clin. Exp. Immunol. 2015, 4, 1–6. [Google Scholar] [PubMed]
- Hemmings, O.; Kwok, M.; McKendry, R.; Santos, A.F. Basophil Activation Test: Old and New Applications in Allergy. Curr. Allergy Asthma Rep. 2018, 18, 1–12. [Google Scholar] [CrossRef] [Green Version]
- Lee, M.; Lee, N.Y.; Chung, K.S.; Cheon, S.Y.; Lee, K.T.; An, H.J. Roxatidine attenuates mast cell-mediated allergic inflammation via inhibition of NF-kappaB and p38 MAPK activation. Sci. Rep. 2017, 7, 41721. [Google Scholar] [CrossRef] [Green Version]
- Kim, D.-H.; Hong, S.-W.; Kim, B.-T.; Bae, E.-A.; Park, H.-Y.; Han, M.J. Biotransformation of glycyrrhizin by human intestinal bacteria and its relation to biological activities. Arch. Pharmacal Res. 2000, 23, 172–177. [Google Scholar] [CrossRef]
- National Institute of Horticultural and Herbal Science, Rural Development Administration. Available online: https://www.nihhs.go.kr/viewer/sn_skin/doc.html?fn=42CD191439E9A9C32A42FDA1361266&rs=/viewer/result/ (accessed on 16 November 2021).






Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kang, Y.-M.; Lee, J.; Kim, W.; Jin, J.-S.; Lee, J.-H.; An, H.-J. Anti-Inflammatory Effects of Novel Glycyrrhiza Variety Wongam In Vivo and In Vitro. Appl. Sci. 2021, 11, 10822. https://doi.org/10.3390/app112210822
Kang Y-M, Lee J, Kim W, Jin J-S, Lee J-H, An H-J. Anti-Inflammatory Effects of Novel Glycyrrhiza Variety Wongam In Vivo and In Vitro. Applied Sciences. 2021; 11(22):10822. https://doi.org/10.3390/app112210822
Chicago/Turabian StyleKang, Yun-Mi, Jeonghoon Lee, Wonnam Kim, Jong-Sik Jin, Jong-Hyun Lee, and Hyo-Jin An. 2021. "Anti-Inflammatory Effects of Novel Glycyrrhiza Variety Wongam In Vivo and In Vitro" Applied Sciences 11, no. 22: 10822. https://doi.org/10.3390/app112210822