Figure 1.
Typical working environments and protective clothing for COVID-19 nucleic acid sampling personnel.
Figure 1.
Typical working environments and protective clothing for COVID-19 nucleic acid sampling personnel.
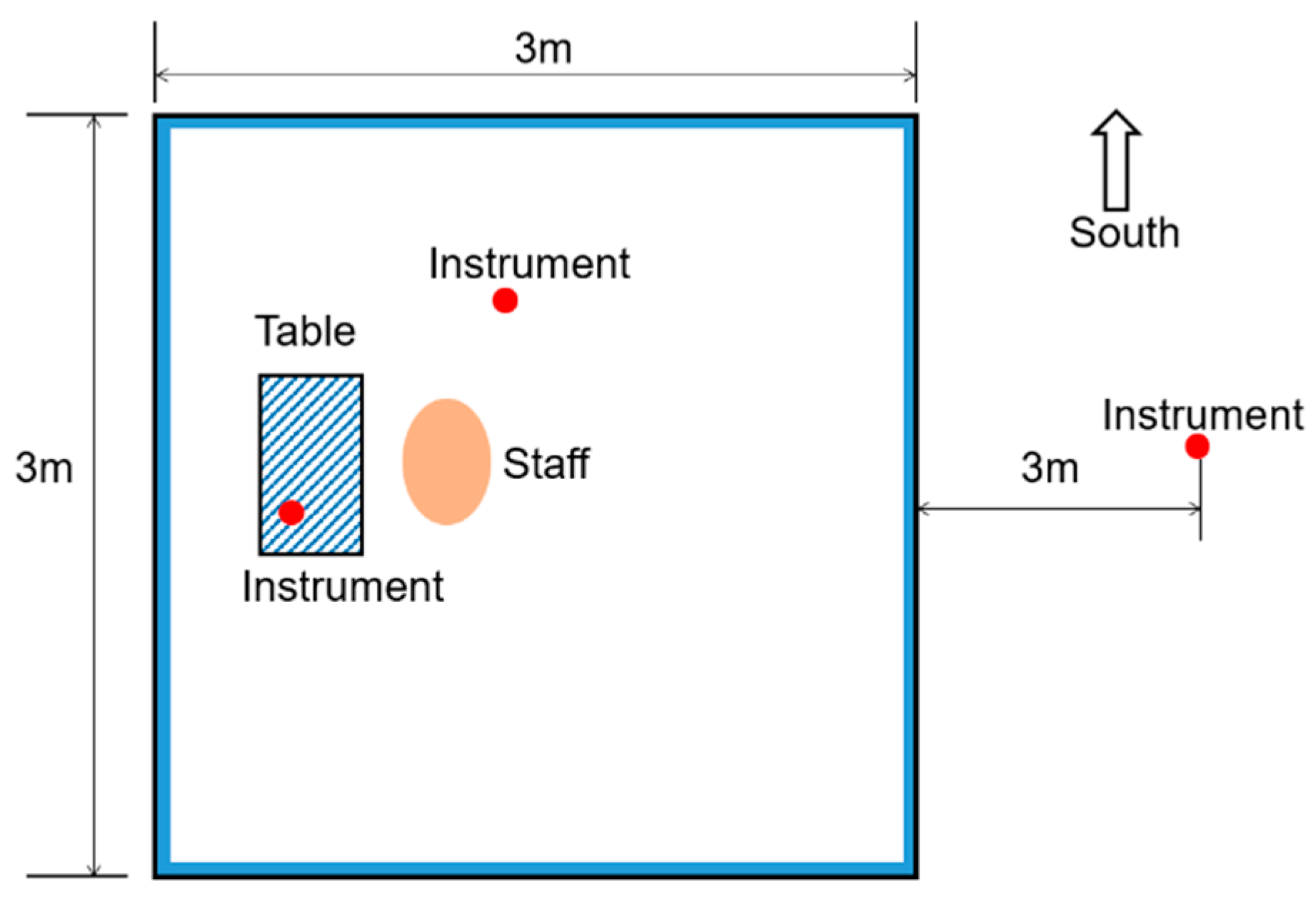
Figure 2.
The location and general arrangements of the experimental site.
Figure 2.
The location and general arrangements of the experimental site.
Figure 3.
Details of the experimental tent layout.
Figure 3.
Details of the experimental tent layout.
Figure 4.
Participants wearing the experimental clothes: (a) full-body nonwoven disposable protective clothing, face mask, goggles and gloves; (b) surgical gown.
Figure 4.
Participants wearing the experimental clothes: (a) full-body nonwoven disposable protective clothing, face mask, goggles and gloves; (b) surgical gown.
Figure 5.
Details of the basis for the division of the sampled working conditions into four thermal categories. (Note: The colored ovals represent the sample range selected under different working conditions).
Figure 5.
Details of the basis for the division of the sampled working conditions into four thermal categories. (Note: The colored ovals represent the sample range selected under different working conditions).
Figure 6.
The subjective feeling voting scales.
Figure 6.
The subjective feeling voting scales.
Figure 7.
Schematic diagram of the experimental procedures.
Figure 7.
Schematic diagram of the experimental procedures.
Figure 8.
Variation of Tsk and HR with time under four different working conditions (i.e., 21–23 °C, 23–25 °C, 25–27 °C and 27–29 °C). (a) Mean skin temperature, (b) Heart Rate. Note: * and ** represent the correlation between WBGT and various parameters; * p < 0.05, ** p < 0.01.
Figure 8.
Variation of Tsk and HR with time under four different working conditions (i.e., 21–23 °C, 23–25 °C, 25–27 °C and 27–29 °C). (a) Mean skin temperature, (b) Heart Rate. Note: * and ** represent the correlation between WBGT and various parameters; * p < 0.05, ** p < 0.01.
Figure 9.
Average skin temperatures for eight different locations on the body of test participants under four different working conditions (i.e., 21–23 °C, 23–25 °C, 25–27 °C and 27–29 °C).
Figure 9.
Average skin temperatures for eight different locations on the body of test participants under four different working conditions (i.e., 21–23 °C, 23–25 °C, 25–27 °C and 27–29 °C).
Figure 10.
The amount of sweat production and metabolic rate under four different working conditions (i.e., 21–23 °C, 23–25 °C, 25–27 °C and 27–29 °C). (a) Sweat production, (b) Metabolic weight-loss.
Figure 10.
The amount of sweat production and metabolic rate under four different working conditions (i.e., 21–23 °C, 23–25 °C, 25–27 °C and 27–29 °C). (a) Sweat production, (b) Metabolic weight-loss.
Figure 11.
Typical sweating patterns of test participants.
Figure 11.
Typical sweating patterns of test participants.
Figure 12.
Changes of physiological strain index with time under four different working conditions (i.e., 21–23 °C, 23–25 °C, 25–27 °C and 27–29 °C).
Figure 12.
Changes of physiological strain index with time under four different working conditions (i.e., 21–23 °C, 23–25 °C, 25–27 °C and 27–29 °C).
Figure 13.
Comprehensive subjective evaluation voting (thermal sensation votes, humid sensation votes, thermal comfort votes, thermal acceptance votes) under four different working conditions (i.e., 21–23 °C, 23–25 °C, 25–27 °C and 27–29 °C). (a) TSV, (b) HSV, (c) TCV, (d) Thermal acceptability.
Figure 13.
Comprehensive subjective evaluation voting (thermal sensation votes, humid sensation votes, thermal comfort votes, thermal acceptance votes) under four different working conditions (i.e., 21–23 °C, 23–25 °C, 25–27 °C and 27–29 °C). (a) TSV, (b) HSV, (c) TCV, (d) Thermal acceptability.
Figure 14.
Voting of participants’ sweating and uncomfortable position under four different working conditions (i.e., 21–23 °C, 23–25 °C, 25–27 °C and 27–29 °C). (a) Sweating position voting, (b) Uncomfortable position voting.
Figure 14.
Voting of participants’ sweating and uncomfortable position under four different working conditions (i.e., 21–23 °C, 23–25 °C, 25–27 °C and 27–29 °C). (a) Sweating position voting, (b) Uncomfortable position voting.
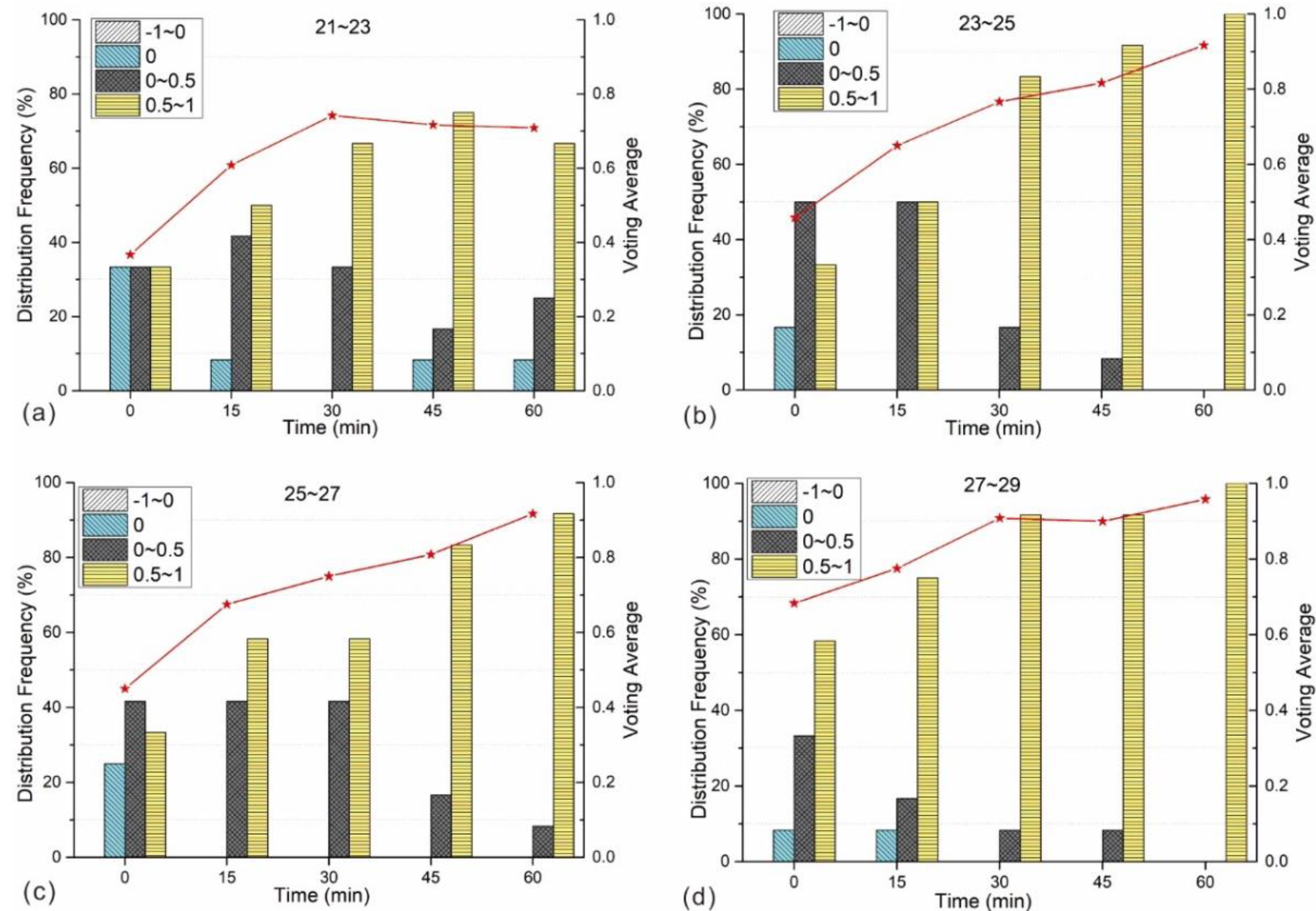
Figure 15.
The variation of the temperature expectation vote with time under four different working conditions (i.e., 21–23 °C, 23–25 °C, 25–27 °C and 27–29 °C). (a) Working condition: 21–23 °C, (b) Working condition: 23–25 °C, (c) Working condition: 25–27 °C, (d) Working condition: 27–29 °C.
Figure 15.
The variation of the temperature expectation vote with time under four different working conditions (i.e., 21–23 °C, 23–25 °C, 25–27 °C and 27–29 °C). (a) Working condition: 21–23 °C, (b) Working condition: 23–25 °C, (c) Working condition: 25–27 °C, (d) Working condition: 27–29 °C.
Figure 16.
The variation of the humidity expectation vote with time under four different working conditions (i.e., 21–23 °C, 23–25 °C, 25–27 °C and 27–29 °C). (a) Working condition: 21–23 °C, (b) Working condition: 23–25 °C, (c) Working condition: 25–27 °C, (d) Working condition: 27–29 °C.
Figure 16.
The variation of the humidity expectation vote with time under four different working conditions (i.e., 21–23 °C, 23–25 °C, 25–27 °C and 27–29 °C). (a) Working condition: 21–23 °C, (b) Working condition: 23–25 °C, (c) Working condition: 25–27 °C, (d) Working condition: 27–29 °C.
Table 1.
Environmental conditions experienced during the test period.
Table 1.
Environmental conditions experienced during the test period.
| Date | Temperature (°C) | Weather Condition | Humidity (%) | Solar Radiation (W/m2) |
|---|
| 30 June | 24.0–29.5 | Cloudy | 52–74 | 165–1096 |
| 1 July | 27.1–35.1 | Cloudy | 30–55 | 221–1053 |
| 2 July | 26.6–29.8 | Overcast | 49–58 | 248–819 |
| 3 July | 24.8–28.2 | Overcast | 59–66 | 50–418 |
| 4 July | 25.6–30.8 | Sunny | 51–66 | 126–980 |
| 5 July | 25.5–33.3 | Sunny | 47–69 | 117–1080 |
| 6 July | 26.0–29.4 | Cloudy | 59–70 | 279–829 |
| 7 July | 27.5–37.1 | Sunny | 34–64 | 115–965 |
| 8 July | 28.5–36.7 | Cloudy | 30–63 | 131–993 |
| 9 July | 21.9–27.7 | Cloudy | 54–80 | 30–296 |
| 10 July | 25.2–31.8 | Cloudy | 50–65 | 104–814 |
| 11 July | 27.1–31.4 | Drizzly | 52–67 | 43–735 |
| 20 July | 25.7–38.0 | Sunny | 36–74 | 250–978 |
| 27 July | 25.3–29.0 | Cloudy | 54–77 | 101–1081 |
Table 2.
The details of the physiological and environmental testing instrumentation used in the experiment.
Table 3.
Average environmental parameters for each of the four working conditions.
Table 3.
Average environmental parameters for each of the four working conditions.
| Working Condition | WBGT (°C) | ta (°C) | RH (%) |
|---|
| 21–23 | 23.04 | 24.78 | 77.02 |
| 23–25 | 24.79 | 28.22 | 60.35 |
| 25–27 | 26.45 | 29.85 | 57.83 |
| 27–29 | 28.60 | 35.12 | 39.30 |
Table 4.
Basic information for the experimental participants.
Table 4.
Basic information for the experimental participants.
| | | Age (Years) | Height (cm) | Weight (kg) | BMI |
|---|
| All | AVE | 23.73 | 171.00 | 62.69 | 21.24 |
| STDEVP | 0.75 | 7.87 | 13.42 | 3.28 |
| Male | AVE | 23.50 | 176.33 | 72.67 | 23.35 |
| STDEVP | 0.76 | 3.30 | 9.04 | 3.05 |
| Female | AVE | 24.00 | 164.60 | 50.80 | 18.70 |
| STDEVP | 0.63 | 6.95 | 5.27 | 0.77 |
Table 5.
Correlation between WBGT index and various physiological parameters.
Table 5.
Correlation between WBGT index and various physiological parameters.
| | | Tsk | HR | SWp | M |
|---|
| WBGT | Pearson | 0.854 ** | 0.739 ** | 0.670 ** | 0.623 ** |
| p(sig.) | 0.000 | 0.000 | 0.000 | 0.000 |
Table 6.
Results of t-test analyses of the physiological parameters of male and female test participants.
Table 6.
Results of t-test analyses of the physiological parameters of male and female test participants.
| | | F | Significance | t | p(Sig.) | Mean Difference |
|---|
| Tsk | Equal variances assumed | 0.110 | 0.741 | −0.547 | 0.587 | 0.248 |
| Equal variances not assumed | | | −0.547 | 0.587 | 0.248 |
| HR | Equal variances assumed | 2.758 | 0.106 | 0.870 | 0.391 | 2.464 |
| Equal variances not assumed | | | 0.906 | 0.371 | 2.464 |
| SWp | Equal variances assumed | 12.992 | 0.001 | 2.773 | 0.008 | 46.674 |
| Equal variances not assumed | | | 2.773 | 0.009 | 46.674 |
| M | Equal variances assumed | 2.313 | 0.135 | 2.374 | 0.022 | 4.713 |
| Equal variances not assumed | | | 2.374 | 0.023 | 4.713 |
Table 7.
Pearson correlation analysis between subjective evaluation and physiological parameters.
Table 7.
Pearson correlation analysis between subjective evaluation and physiological parameters.
| | | Tsk | HR | SWp | M |
|---|
| TSV | Pearson | 0.534 ** | 0.495 ** | 0.416 ** | 0.318 * |
| p(sig.) | 0.000 | 0.002 | 0.003 | 0.028 |
| HSV | Pearson | 0.494 ** | 0.375 ** | 0.509 ** | 0.407 ** |
| p(sig.) | 0.009 | 0.002 | 0.000 | 0.004 |
| TCV | Pearson | −0.510 ** | −0.335 * | −0.379 ** | −0.319 ** |
| p(sig.) | 0.001 | 0.046 | 0.008 | 0.002 |