Reducing the Heart Failure Burden in Romania by Predicting Congestive Heart Failure Using Artificial Intelligence: Proof of Concept
Abstract
:1. Introduction
1.1. Pathopyshiology of Acute Heart Failure
1.2. Artificial Intelligence in Cardiology
1.3. Main Contributions
2. Materials and Methods
2.1. Study Population
2.2. Intervention
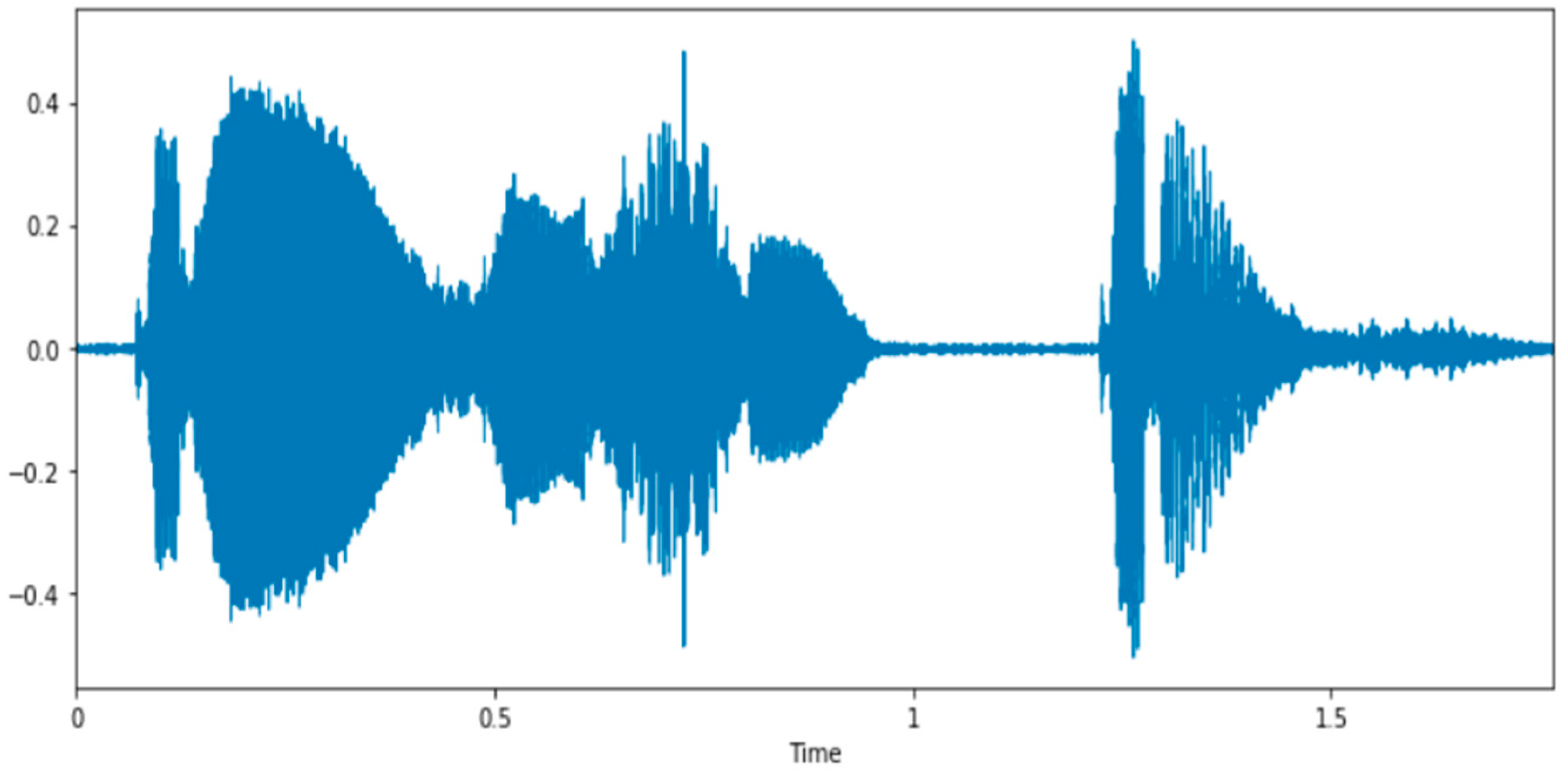
2.3. Feature Extraction
2.4. Machine-Learning Approaches
2.4.1. Support Vector Machine (SVM)
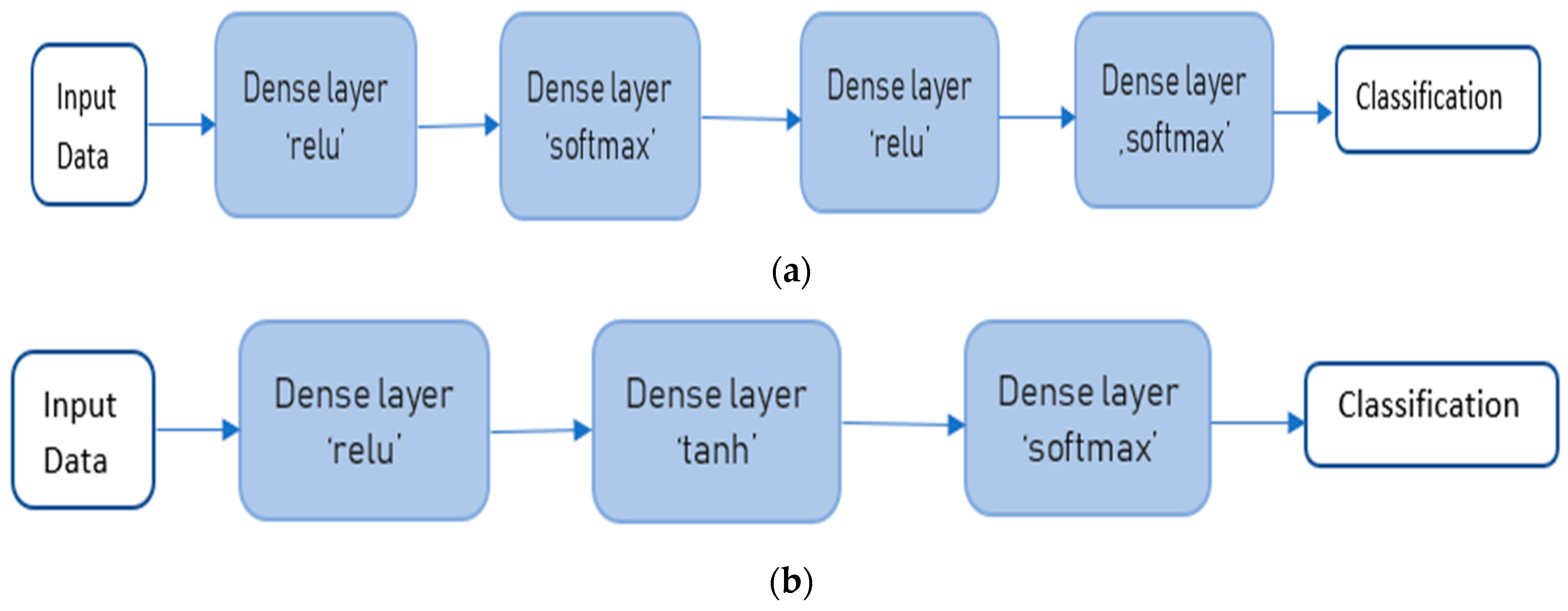
2.4.2. Artificial Neural Networks (ANN)
2.4.3. K-Nearest Neighbors (KNN)
3. Results
4. Discussion
5. Conclusions
6. Limitations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Naylor, M.D.; Brooten, D.A.; Campbell, R.L.; Maislin, G.; McCauley, K.M.; Schwartz, J.S. Transitional care of older adults hospitalized with heart failure: A randomized controlled trial. J. Am. Geriatr. Soc. 2004, 52, 675–684. [Google Scholar] [CrossRef]
- Ziaeian, B.; Fonarow, G.C. Epidemiology and aetiology of heart failure. Nat. Rev. Cardiol. 2016, 13, 368–378. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Andrei, C.A.; Oancea, B.; Nedelcu, M.; Sinescu, R.D. Predicting Cardiovascular Diseases Prevalence Using Neural Networks. Econ. Comput. Econ. Cybern. Stud. Res. 2015, 49, 73–84. [Google Scholar]
- Lee, H.; Oh, S.H.; Cho, H.; Cho, H.J.; Kang, H.Y. Prevalence and socio-economic burden of heart failure in an aging society of South Kirea. BMC Cardiovasc. Disord. 2016, 16, 215. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bui, A.L.; Horwich, T.B.; Fonarow, G.C. Epidemiology and risk profile of heart failure. Nat. Rev. Cardiol. 2011, 1, 30–41. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Roger, V.L. Epidemiology of heart failure. Circ. Res. 2013, 113, 646–659. [Google Scholar] [CrossRef]
- Brennan, E.J. Chronic heart failure nursing: Integrated multidisciplinary care. Br. J. Nurs. 2018, 27, 681–688. [Google Scholar] [CrossRef] [PubMed]
- Porcel, J.M. Pleural effusions from congestive heart failure. Semin. Respir. Crit. Care Med. 2010, 31, 689–697. [Google Scholar] [CrossRef]
- Natanzon, A.; Kronzon, I. Pericardial and pleural effusions in congestive heart failure- anatomical, pathophysiologic and clinical considerations. Am. J. Med. Sci. 2009, 338, 211–216. [Google Scholar] [CrossRef]
- Lesyuk, W.; Kriza, C.; Kolominsky-Rabas, P. Cost-of-illness studies in heart failure: A systematic review 2004–2016. BMC Cardiovasc. Disord. 2018, 18, 74. [Google Scholar] [CrossRef] [Green Version]
- Heidenreich, P.A.; Albert, N.M.; Allen, L.A.; Bluemke, D.A.; Butler, J.; Fonarow, G.C.; Ikonomidis, J.S.; Khavjou, O.; Konstam, M.A.; Maddox, T.M.; et al. Forecasting the impact of heart failure in the United States: A policy statement from the American Heart Association. Circ. Heart Fail. 2013, 6, 606–609. [Google Scholar] [CrossRef] [Green Version]
- Chioncel, O.; Tatu-Chitoiu, G.; Christodorescu, R.; Coman, I.M.; Deleanu, D.; Vinereanu, D.; Macarie, C.; Crespo, M.; Laroche, C.; Fereirra, T.; et al. Characteristic of patients with heart failure from Romania enrolled in—ESC-HF Long-term (ESC-HF-LT) Registry. Rom. J. Cardiol. 2015, 25, 1–8. [Google Scholar]
- Van Nuys, K.E.; Xie, Z.; Tysinger, B.; Hlatky, M.A.; Goldman, D.P. Innovation in Heart Failure Treatment: Life expectancy, Disability and Healt Disparities. JACC Heart Fail. 2018, 6, 401–409. [Google Scholar] [CrossRef] [PubMed]
- Bytyci, I.; Bajraktari, G. Mortality in heart failure patients. Anatol. J. Cardiol. 2015, 15, 63–68. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ni, H.; Xu, J. Recent trends in heart failure-related Mortality: United States 2000–2014. In NCHS Data Brief; National Center for Health Statistics: Hyattsville, MD, USA, 2015; Volume 231, pp. 1–8. [Google Scholar]
- King, M.; Kingery, J.; Casey, B. Diagnosis and evaluation of heart failure. Am. Fam. Physician 2012, 85, 1161–1168. [Google Scholar]
- Kurmani, S.; Squire, I. Acute Heart Failure: Definition, Classification and Epidemiology. Curr. Heart Fail. Rep. 2017, 14, 385–392. [Google Scholar] [CrossRef] [Green Version]
- Gheorghiade, M.; Zannad, F.; Sopko, G.; Klein, L.; Piña, I.L.; Konstam, M.A.; Massie, B.M.; Roland, E.; Targum, S.; Collins, S.P.; et al. Acute heart failure syndromes: Current state and framework for future research. Circulation 2005, 112, 3958–3968. [Google Scholar] [CrossRef] [Green Version]
- Dobbe, L.; Rahman, R.; Elmassry, M.; Paz, P.; Nugent, K. Cardiogenic Pulmonary Edema. Am. J. Med. Sci. 2019, 358, 389–397. [Google Scholar] [CrossRef]
- Tsuchiya, N.; Griffin, L.; Yabuuchi, H.; Kawanami, S.; Shinzato, J.; Murayama, S. Imaging findings of pulmonary edema: Part 1. Cardiogenic pulmonary edema and acute respiratory distress syndrome. Acta Radiol. 2020, 61, 184–194. [Google Scholar] [CrossRef]
- Vergani, G.; Cressoni, M.; Crimella, F.; L’Acqua, C.; Sisillo, E.; Gurgitano, M.; Liguori, A.; Annoni, A.; Carrafiello, G.; Chiumello, D. A Morphological and Quantitative Analysis of Lung CT Scan in Patients with Acute Respiratory Distress Syndrome and in Cardiogenic Pulmonary Edema. J. Intensive Care Med. 2020, 35, 284–292. [Google Scholar] [CrossRef] [PubMed]
- Sacchetti, A.D.; Harris, R.H. Acute cardiogenic pulmonary edema. What’s the latest in emergency treatment? Postgrad Med. 1998, 103, 145–166. [Google Scholar] [CrossRef]
- Trayes, K.P.; Studdiford, J.S.; Pickle, S.; Tully, A.S. Edema: Diagnosis and management. Am. Fam. Physician 2013, 88, 102–110. [Google Scholar] [PubMed]
- Verdolini, K.; Min, Y.; Titze, I.R.; Lemke, J.; Brown, K.; van Mersbergen, M.; Jiang, J.J.; Fisher, K. Biological Mechanisms Underlying Voice Changes Due to Dehydration. J. Speech Lang. Heart Res. 2002, 45, 268–281. [Google Scholar] [CrossRef]
- Murton, O.M.; Hillman, R.E.; Mehta, D.D. Acoustic speech analysis of patients with decompensated heart failure: A pilot study. J. Acoust. Soc. Am. 2017, 142, EL401–EL407. [Google Scholar] [CrossRef] [Green Version]
- Toback, M.; Clark, N. Strategies to improve self-management in heart failure patients. Contemp. Nurse 2017, 53, 105–120. [Google Scholar] [CrossRef] [PubMed]
- Andrews, A.M.; Russell, C.L.; Cheng, A.L. Medication Adherence Interventions for Older Adults with Heart Failure: A systematic Review. J. Gerontol. Nurs. 2017, 43, 37–45. [Google Scholar] [CrossRef] [Green Version]
- Savarese, G.; Lund, L.H. Global Public Health Burden of Heart Failure. Card. Fail. Rev. 2017, 3, 7–11. [Google Scholar] [CrossRef]
- Johnson, K.; Soto, J.T.; Glicksberg, B.; Shameer, K.; Miotto, R.; Ali, M.; Ashley, E.; Dudley, J.T. Artificial Intelligence in Cardiology. J. Am. Coll. Cardiol. 2018, 71, 2668–2679. [Google Scholar] [CrossRef]
- Bonderman, D. Artificial intelligence in cardiology. Wien. Klin. Wochenschr. 2017, 129, 866–868. [Google Scholar] [CrossRef] [PubMed]
- Ramesh, A.N.; Kambhampati, C.; Monson, R.T., Jr.; Drew, P.J. Artificial intelligence in medicine. Ann. R. Coll. Surg. Engl. 2004, 86, 334–338. [Google Scholar] [CrossRef] [Green Version]
- Dawes, T.J.W.; de Marvao, A.; Shi, W.; Fletcher, T.; Watson, G.M.J.; Wharton, J.; Rhodes, C.J.; Howard, L.S.G.E.; Gibbs, J.S.R.; Rueckert, D.; et al. Machine Learning of Three-dimensional Right Ventricular Motion Enables Outcome Prediction in Pulmonary Hypertension: A Cardiac MR Imaging Study. Radiology 2017, 283, 381–390. [Google Scholar] [CrossRef] [Green Version]
- Choi, D.-J.; Park, J.J.; Ali, T.; Lee, S. Artificial intelligence for the diagnosis of heart failure. npj Digit. Med. 2020, 3, 1–6. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Guo, A.; Pasque, M.; Loh, F.; Mann, D.L.; Payne, P.R.O. Heart Failure Diagnosis, Readmission, and Mortality Prediction Using Machine Learning and Artificial Intelligence Models. Curr. Epidemiol. Rep. 2020, 7, 212–219. [Google Scholar] [CrossRef]
- Khader, S.; Johnson, K.W.; Yahi, A.; Miotto, R.; Li, L.; Ricks, D.; Jebakaran, J.; Kovatch, P.; Sengupta, P.P.; Gelijns, S.; et al. Predictive modeling of hospital readmission rates using electronic medical record-wide machine learning: A case-study using Mount Sinai Heart Failure Cohort. Pac. Symp. Biocomput. 2017, 22, 276–287. [Google Scholar]
- Dolgin, M.; New York Heart Association; Criteria Committee. Nomenclature and Criteria for Diagnosis of Diseases of the Heart and Great Vessels, 9th ed.; Little Brown & Co.: Boston, MA, USA, 1994; pp. 253–256. [Google Scholar]
- Magre, S.B.; Janse, P.V.; Desmukh, R.R. A review on Feature Extraction and Noise Reduction Technique. Int. J. Adv. Res. Comput. Sci. Softw. Eng. 2014, 4, 352–356. [Google Scholar]
- Sidey-Gibbons, J.A.M.; Sidey-Gibbons, C.J. Machine learning in medicine: A practical introduction. BMC Med. Res. Methodol. 2019, 19, 1–18. [Google Scholar] [CrossRef] [Green Version]
- Cortes, C.; Vapnik, V.N. Support-vector networks. Mach. Learn. 1995, 20, 273–297. [Google Scholar] [CrossRef]
- Zhang, R.; Li, B.; Peng, T. Audio classification based on SVM-UBM. In Proceedings of the 9th International Conference on Signal Processing Beijing, Beijing, China, 26–29 October 2008; pp. 1586–1589. [Google Scholar]
- Hofmann, T.; Schölkopf, B.; Smola, A.J. Kernel methods in machine learning. Ann. Stat. 2008, 36, 1171–1220. [Google Scholar] [CrossRef] [Green Version]
- Schmidhuber, J. Deep Learning in Neural Networks: An Overview. Neural Netw. 2015, 61, 85–117. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hastie, T.; Tibshirani, R.; Friedman, J. The Elements of Statistical Learning: Data Mining, Inference, and Prediction: With 200 Full-Color Illustrations; Springer: New York, NY, USA, 2001. [Google Scholar]
- Lin, Y.; Wang, J. Research on the Text Classification Based on SVM-KNN. In Proceedings of the 2014 IEEE 5th International Conference on Software Engineering and Service Science, Beijing, China, 27–29 June 2014. [Google Scholar]
- Groenewegen, A.; Rutten, F.H.; Mosterd, A.; Hoes, A.W. Epidemiologyand of heart failure. Eur. J. Heart Fail. 2020, 22, 1342–1356. [Google Scholar] [CrossRef] [PubMed]
- Jones, N.R.; Roalfe, A.K.; Adoki, I.; Hobbs, F.D.R.; Taylor, C.J. Survival of patients with chronic heart failure in the community: A systematic review and meta-analysis. Eur. J. Heart Fail. 2019, 21, 1306–1325. [Google Scholar] [CrossRef]
- Dharmarajan, K.; Rich, M.W. Epidemiology, Pathophysiology and Prognosis of Heart Failure in Older Adults. Heart Fail. Clin. 2017, 13, 417–426. [Google Scholar] [CrossRef] [Green Version]
- Cook, C.; Cole, G.; Asaria, P.; Jabbour, R.; Francis, D.P. The annual global economic burden of heart failure. Int. J. Cardiol. 2014, 171, 368–376. [Google Scholar] [CrossRef]
- Zugck, C.; Muller, A.; Helms, T.M.; Wildau, H.J.; Becks, T.; Hacker, J.; Haag, S.; Goldhagen, K.; Schwab, J.O. Health economic impact of heart failure: An analysis of the nationwide German database. Dtsch. Med. Wochenschr. 2010, 135, 633–638. [Google Scholar] [CrossRef]
- Delgado, J.F.; Oliva, J.; Llano, M.; Pascual-Figal, D.; Grillo, J.J.; Comín-Colet, J.; Díaz, B.; de la Concha, L.M.; Martí, B.; Peña, L.M. Health care and non-health care costs in the treatment of patients with symptomatic chronic heart failure in Spain. Rev. Esp. Cardiol. 2014, 67, 643–650. [Google Scholar] [CrossRef]
- Dunlay, S.M.; Shah, N.D.; Shi, Q.; Morlan, B.; VanHouten, H.; Long, K.H.; Roger, V.L. Lifetime costs of medical care after heart failure diagnosis. Circ. Cardiovasc. Qual. Outcomes 2011, 4, 68–75. [Google Scholar] [CrossRef] [Green Version]
- Jadczyk, T.; Wojakowski, W.; Tendera, M.; Henry, T.D.; Egnaczyk, G.; Shreenivas, S. Artificial Intelligence Can Improve Patient Management at the Time of a Pandemic: The Role of Voice Technology. J. Med. Internet Res. 2021, 23, e22959. [Google Scholar] [CrossRef] [PubMed]



| Class | Patient Symptoms |
|---|---|
| I | No limitation of physical activity. Ordinary physical activity does not cause undue fatigue, palpitation, dyspnea (shortness of breath) |
| II | Slight limitation of physical activity. Comfortable at rest. Ordinary physical activity results in fatigue, palpitation, dyspnea (shortness of breath). |
| III | Marked limitation of physical activity. Comfortable at rest. Less than ordinary activity causes fatigue, palpitations or dyspnea. |
| IV | Unable to carry on any physical activity without discomfort. Symptoms of heart failure at rest. If any physical activity is undertaken, discomfort increases. |
| Patient No. | Age | Sex | Smoker Status | Body mass Index | Arterial Hypertension | Diabetes Mellitus Type 2 | Dyslipidemia |
|---|---|---|---|---|---|---|---|
| 1 | 75 | F | No | 24.21 kg/m2 | Yes (grade 2) | Yes | Yes |
| 2 | 71 | F | Yes | 34.66 kg/m2 | Yes (grade 3) | No | Yes |
| 3 | 73 | M | No | 38.06 kg/m2 | Yes (grade 3) | Yes | Yes |
| 4 | 76 | M | No | 24.8 kg/m2 | Yes (grade 3) | No | No |
| 5 | 70 | M | Yes | 27.65 kg/m2 | Yes (grade 3) | No | Yes |
| 6 | 65 | M | No | 27.7 kg/m2 | Yes (grade 3) | Yes | Yes |
| 7 | 91 | M | No | 24.68 kg/m2 | Yes (grade 3) | Yes | Yes |
| 8 | 70 | M | No | 31.04 kg/m2 | No | No | Yes |
| 9 | 66 | F | Yes | 44.17 kg/m2 | Yes (grade 2) | Yes | No |
| 10 | 79 | F | No | 23.43 kg/m2 | Yes (grade 3) | Yes | No |
| 11 | 75 | M | Yes | 26.23 kg/m2 | No | No | No |
| 12 | 78 | M | Yes | 26.89 kg/m2 | Yes (grade 2) | No | Yes |
| 13 | 67 | M | Yes | 30.86 kg/m2 | Yes (grade 3) | Yes | Yes |
| 14 | 74 | F | No | 44.92 kg/m2 | No | Yes | Yes |
| 15 | 67 | F | Yes | 33.58 kg/m2 | Yes (grade 2) | Yes | Yes |
| 16 | 66 | F | Yes | 46.88 kg/m2 | No | Yes | Yes |
| Patient NO. | Left Ventricular Ejection Fraction | IHD | IHD Type | Atrial Fibrillation | Aortic Valve Disease | Mitral Valve Disease | Tricuspid Valve Disease |
|---|---|---|---|---|---|---|---|
| 1 | 15% | Yes | PCI | Yes | Metal prosthesis | Metal prosthesis | Tricuspid annuloplasty |
| 2 | 50% | Yes | PCI | No | No | Easy mitral regurgitation | No |
| 3 | 19% | Yes | CABG | No | No | Severe mitral regurgitation | Severe tricuspid regurgitation |
| 4 | 35% | Yes | MTh. | No | Easy aortic regurgitation | Moderate mitral regurgitation | Moderate tricuspid regurgitation |
| 5 | 30% | Yes | PCI | Yes | No | Moderate mitral regurgitation | Moderate tricuspid regurgitation |
| 6 | 20% | Yes | PCI | No | No | Moderate mitral regurgitation | Moderate tricuspid regurgitation |
| 7 | 40% | Yes | CABG | No | Moderate aortic stenosis | Severe mitral regurgitation | Easy tricuspid regurgitation |
| 8 | 25% | Yes | MTh | No | No | Easy mitral regurgitation | No |
| 9 | 40% | Yes | MTh | No | No | Moderate mitral regurgitation | Moderate tricuspid regurgitation |
| 10 | 30% | Yes | MTh | Yes | No | Moderate mitral regurgitation | Easy tricuspid regurgitation |
| 11 | 25% | Yes | CABG | Yes | Severe aortic stenosis | Metal prosthesis | Severe tricuspid regurgitation |
| 12 | 50% | Yes | PCI | Yes | Moderate aortic regurgitation | Moderate mitral regurgitation | Moderate tricuspid regurgitation |
| 13 | 45% | Yes | PCI | No | No | Easy mitral regurgitation | Easy tricuspid regurgitation |
| 14 | 20% | Yes | MTh | Yes | No | Moderate mitral regurgitation | Moderate tricuspid regurgitation |
| 15 | 40% | Yes | CABG | No | No | Moderate mitral regurgitation | Easy tricuspid regurgitation |
| 16 | 10% | Yes | PCI | No | No | Moderate mitral regurgitation | Moderate tricuspid regurgitation |
| Method | Results |
|---|---|
| SVM | Accuracy obtained using radial basis function (rbf) kernel = 0.709 Accuracy obtained using linear kernel = 0.618 Accuracy obtained using polynomial kernel = 0.527 |
| ANN | Model 1: Maximum value of the loss function obtained during testing: 1.1447 Maximum accuracy obtained during testing: 0.418 Model 2: Maximum value of the loss function obtained during testing: 1.3237 Maximum accuracy obtained during testing: 0.436 |
| KNN | Model score obtained for KNN: 0.945 Confusion Matrix: [[20 0 2] [0 13 0] [1 0 19]] |
| Patient No. | Admission Weight | Discharge Weight | Mean Value of Daily Diuresis | Daily Water Supply | Ntprobnp Admission | Ntprobnp Discharge |
|---|---|---|---|---|---|---|
| 1 | 62 kg | 58 kg | 2500 mL/24 h | 2000 mL/day | 3480 pg/mL | 1200 pg/mL |
| 2 | 78 kg | 73 kg | 3500 mL/24 h | 1000 mL/day | 4638 pg/mL | 900 pg/mL |
| 3 | 110 kg | 102 kg | 2600 mL/24 h | 750mL/day | 17,545 pg/mL | 500 pg/mL |
| 4 | 70 kg | 65 kg | 3000mL/24 h | 2000 mL/day | 3131 pg/mL | 1000 pg/mL |
| 5 | 78 kg | 74 kg | 3000 mL/24 h | 1500 mL/day | >30.000 pg/mL | 1200 pg/mL |
| 6 | 96 kg | 90 kg | 3500 mL/24 h | 1000 mL/day | 1207 pg/mL | 400 pg/mL |
| 7 | 78 kg | 71 kg | 2700 mL/24 h | 1000 mL/day | 8987 pg/mL | 700 pg/mL |
| 8 | 95 kg | 90 kg | 3100 mL/24 h | 1000 mL/day | 4277 pg/mL | 800 pg/mL |
| 9 | 110 kg | 103 kg | 4000 mL/24 h | 1500 mL/day | 3664 pg/mL | 650 pg/mL |
| 10 | 60 kg | 55g | 3800 mL/24 h | 1500 mL/day | 5200 pg/mL | 1105 pg/mL |
| 11 | 85 kg | 79 kg | 3400 mL/24 h | 1000 mL/day | 15.300 pg/mL | 940 pg/mL |
| 12 | 85 kg | 80 kg | 3500 mL/24 h | 1500 mL/day | 4325 pg/mL | 456 pg/mL |
| 13 | 100 kg | 94 kg | 4000 mL/24 h | 2000 mL/day | 6800 pg/mL | 670 pg/mL |
| 14 | 115 kg | 109 kg | 4500 mL/24 h | 1500 mL/day | 2262 pg/mL | 370 pg/mL |
| 15 | 90 kg | 82 kg | 3800 mL/24 h | 1000 mL/day | 3797 pg/mL | 800 pg/mL |
| 16 | 120 kg | 110 kg | 4300 mL/24 h | 1000 mL/day | 10.939 pg/mL | 589 pg/mL |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pană, M.-A.; Busnatu, Ș.-S.; Serbanoiu, L.-I.; Vasilescu, E.; Popescu, N.; Andrei, C.; Sinescu, C.-J. Reducing the Heart Failure Burden in Romania by Predicting Congestive Heart Failure Using Artificial Intelligence: Proof of Concept. Appl. Sci. 2021, 11, 11728. https://doi.org/10.3390/app112411728
Pană M-A, Busnatu Ș-S, Serbanoiu L-I, Vasilescu E, Popescu N, Andrei C, Sinescu C-J. Reducing the Heart Failure Burden in Romania by Predicting Congestive Heart Failure Using Artificial Intelligence: Proof of Concept. Applied Sciences. 2021; 11(24):11728. https://doi.org/10.3390/app112411728
Chicago/Turabian StylePană, Maria-Alexandra, Ștefan-Sebastian Busnatu, Liviu-Ionut Serbanoiu, Electra Vasilescu, Nirvana Popescu, Cătălina Andrei, and Crina-Julieta Sinescu. 2021. "Reducing the Heart Failure Burden in Romania by Predicting Congestive Heart Failure Using Artificial Intelligence: Proof of Concept" Applied Sciences 11, no. 24: 11728. https://doi.org/10.3390/app112411728
APA StylePană, M.-A., Busnatu, Ș.-S., Serbanoiu, L.-I., Vasilescu, E., Popescu, N., Andrei, C., & Sinescu, C.-J. (2021). Reducing the Heart Failure Burden in Romania by Predicting Congestive Heart Failure Using Artificial Intelligence: Proof of Concept. Applied Sciences, 11(24), 11728. https://doi.org/10.3390/app112411728








