Removal of Inflammatory Tissue/Product by Sinus Membrane Puncturing during Lateral Sinus Augmentation in Asymptomatic Patients with Severely Opacified Sinuses: A Case Series
Abstract
:1. Introduction
2. Case Report
2.1. Surgical and Clinical Procedures
2.2. Patients
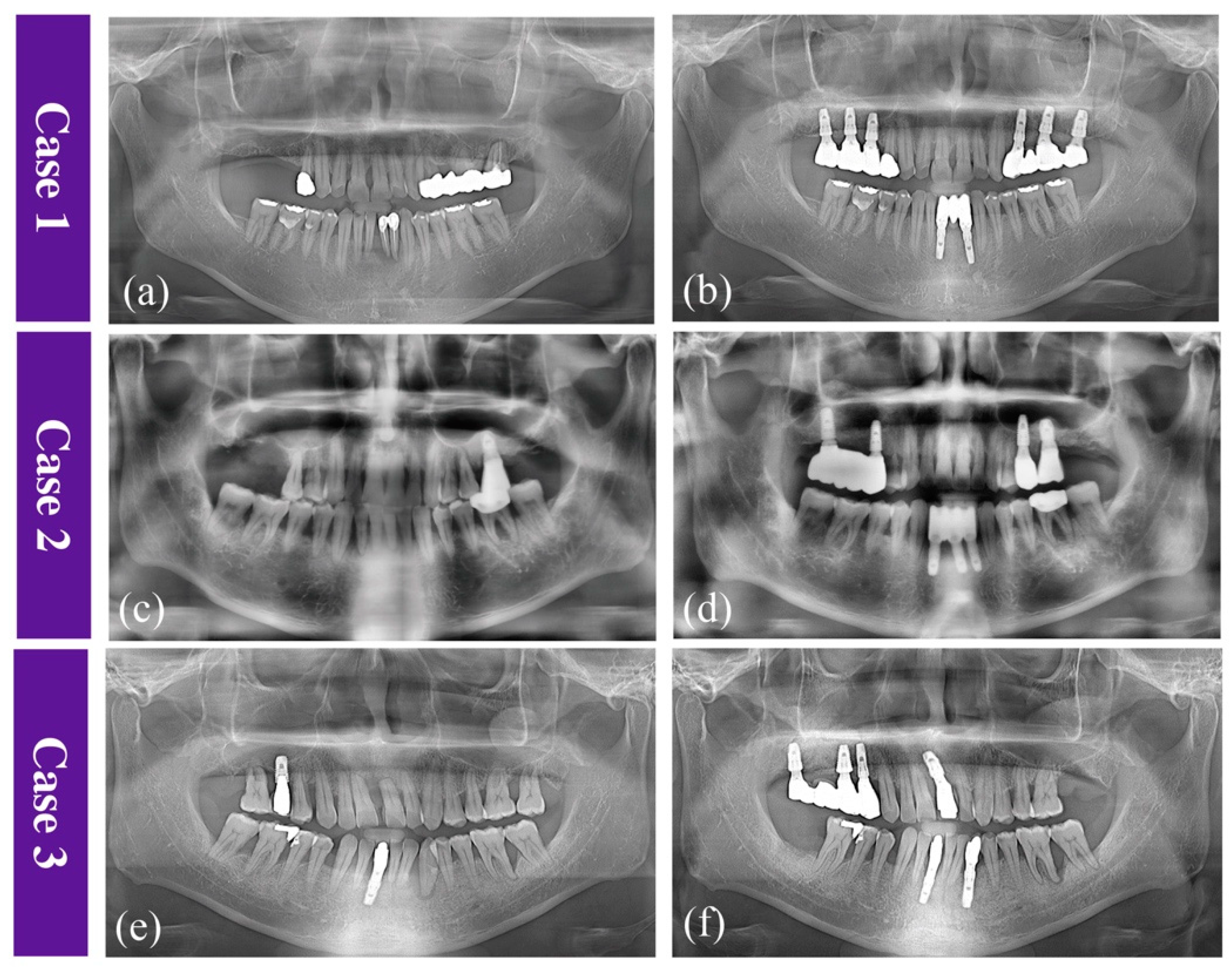
2.2.1. Case 1
2.2.2. Case 2
2.2.3. Case 3
2.3. Clinical Findings
2.4. Histological Findings
2.5. Radiological Findings
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Pjetursson, B.E.; Tan, W.C.; Zwahlen, M.; Lang, N.P. A systematic review of the success of sinus floor elevation and survival of implants inserted in combination with sinus floor elevation: Part I: Lateral approach. J. Clin. Periodontol. 2008, 35, 216–240. [Google Scholar] [CrossRef]
- Raghoebar, G.M.; Onclin, P.; Boven, G.C.; Vissink, A.; Meijer, H.J.A. Long-term effectiveness of maxillary sinus floor augmentation: A systematic review and meta-analysis. J. Clin. Periodontol. 2019, 46 (Suppl. S21), 307–318. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tan, W.C.; Lang, N.P.; Zwahlen, M.; Pjetursson, B.E. A systematic review of the success of sinus floor elevation and survival of implants inserted in combination with sinus floor elevation. Part II: Transalveolar technique. J. Clin. Periodontol. 2008, 35, 241–254. [Google Scholar] [CrossRef]
- Carmeli, G.; Artzi, Z.; Kozlovsky, A.; Segev, Y.; Landsberg, R. Antral computerized tomography pre-operative evaluation: Relationship between mucosal thickening and maxillary sinus function. Clin. Oral Implant. Res. 2011, 22, 78–82. [Google Scholar] [CrossRef] [PubMed]
- Lin, Y.H.; Yang, Y.C.; Wen, S.C.; Wang, H.L. The influence of sinus membrane thickness upon membrane perforation during lateral window sinus augmentation. Clin. Oral Implant. Res. 2016, 27, 612–617. [Google Scholar] [CrossRef]
- Wen, S.C.; Lin, Y.H.; Yang, Y.C.; Wang, H.L. The influence of sinus membrane thickness upon membrane perforation during transcrestal sinus lift procedure. Clin. Oral Implant. Res. 2015, 26, 1158–1164. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shanbhag, S.; Karnik, P.; Shirke, P.; Shanbhag, V. Cone-beam computed tomographic analysis of sinus membrane thickness, ostium patency, and residual ridge heights in the posterior maxilla: Implications for sinus floor elevation. Clin. Oral Implant. Res. 2014, 25, 755–760. [Google Scholar] [CrossRef]
- Wang, J.H.; Jang, Y.J.; Lee, B.J. Natural course of retention cysts of the maxillary sinus: Long-term follow-up results. Laryngoscope 2007, 117, 341–344. [Google Scholar] [CrossRef] [PubMed]
- Bertrand, B.; Eloy, P. Relationship of chronic ethmoidal sinusitis, maxillary sinusitis, and ostial permeability controlled by sinusomanometry: Statistical study. Laryngoscope 1992, 102, 1281–1284. [Google Scholar] [CrossRef]
- Timmenga, N.M.; Raghoebar, G.M.; Liem, R.S.; van Weissenbruch, R.; Manson, W.L.; Vissink, A. Effects of maxillary sinus floor elevation surgery on maxillary sinus physiology. Eur. J. Oral Sci. 2003, 111, 189–197. [Google Scholar] [CrossRef]
- Schwartz-Arad, D.; Herzberg, R.; Dolev, E. The prevalence of surgical complications of the sinus graft procedure and their impact on implant survival. J. Periodontol. 2004, 75, 511–516. [Google Scholar] [CrossRef]
- Nolan, P.J.; Freeman, K.; Kraut, R.A. Correlation between Schneiderian membrane perforation and sinus lift graft outcome: A retrospective evaluation of 359 augmented sinus. J. Oral Maxillofac. Surg. 2014, 72, 47–52. [Google Scholar] [CrossRef]
- Park, W.B.; Han, J.Y.; Kang, P.; Momen-Heravi, F. The clinical and radiographic outcomes of Schneiderian membrane perforation without repair in sinus elevation surgery. Clin. Implant. Dent. Relat. Res. 2019, 21, 931–937. [Google Scholar] [CrossRef]
- Silver, A.J.; Baredes, S.; Bello, J.A.; Blitzer, A.; Hilal, S.K. The opacified maxillary sinus: CT findings in chronic sinusitis and malignant tumors. Radiology 1987, 163, 205–210. [Google Scholar] [CrossRef]
- Rege, I.C.; Sousa, T.O.; Leles, C.R.; Mendonca, E.F. Occurrence of maxillary sinus abnormalities detected by cone beam CT in asymptomatic patients. BMC Oral Health 2012, 12, 30. [Google Scholar] [CrossRef] [Green Version]
- Felisati, G.; Borloni, R.; Chiapasco, M.; Lozza, P.; Casentini, P.; Pipolo, C. Maxillary sinus elevation in conjunction with transnasal endoscopic treatment of rhino-sinusal pathoses: Preliminary results on 10 consecutively treated patients. Acta Otorhinolaryngol. Ital. 2010, 30, 289–293. [Google Scholar]
- Abu-Ghanem, S.; Kleinman, S.; Horowitz, G.; Balaban, S.; Reiser, V.; Koren, I. Combined maxillary sinus floor elevation and endonasal endoscopic sinus surgery for coexisting inflammatory sinonasal pathologies: A one-stage double-team procedure. Clin. Oral Implant. Res. 2015, 26, 1476–1481. [Google Scholar] [CrossRef] [PubMed]
- Falco, A.; Amoroso, C.; Berardini, M.; D’Archivio, L. A retrospective study of clinical and radiologic outcomes of 69 consecutive maxillary sinus augmentations associated with functional endoscopic sinus surgery. Int. J. Oral Maxillofac. Implant. 2015, 30, 633–638. [Google Scholar] [CrossRef] [PubMed]
- Seiberling, K.A.; McHugh, R.K.; Aruni, W.; Church, C.A. The impact of intraoperative saline irrigations on bacterial load within the maxillary sinus. Int. Forum Allergy Rhinol. 2011, 1, 351–355. [Google Scholar] [CrossRef] [Green Version]
- Makary, C.; Rebaudi, A.; Menhall, A.; Naaman, N. Changes in Sinus Membrane Thickness After Lateral Sinus Floor Elevation: A Radiographic Study. Int. J. Oral Maxillofac. Implant. 2016, 31, 331–337. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Oh, J.H.; An, X.; Jeong, S.M.; Choi, B.H. Crestal Sinus Augmentation in the Presence of an Antral Pseudocyst. Implant. Dent. 2017, 26, 951–955. [Google Scholar] [CrossRef]
- Yu, H.; Qiu, L. Histological and clinical outcomes of lateral sinus floor elevation with simultaneous removal of a maxillary sinus pseudocyst. Clin. Implant. Dent. Relat. Res. 2019, 21, 94–100. [Google Scholar] [CrossRef] [Green Version]
- Kara, I.M.; Kucuk, D.; Polat, S. Experience of maxillary sinus floor augmentation in the presence of antral pseudocysts. J. Oral Maxillofac. Surg. 2010, 68, 1646–1650. [Google Scholar] [CrossRef]
- Lin, Y.; Hu, X.; Metzmacher, A.R.; Luo, H.; Heberer, S.; Nelson, K. Maxillary sinus augmentation following removal of a maxillary sinus pseudocyst after a shortened healing period. J. Oral Maxillofac. Surg. 2010, 68, 2856–2860. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.; Chung, J.H.; Shin, S.Y.; Shin, S.I.; Hong, J.Y.; Lim, H.C. Collagenated Synthetic Bone Substitute Material for Sinus Floor Elevation at Sites with a Perforated Schneiderian Membrane. J. Clin. Med. 2020, 9, 764. [Google Scholar] [CrossRef]
- Lim, H.C.; Son, Y.; Hong, J.Y.; Shin, S.I.; Jung, U.W.; Chung, J.H. Sinus floor elevation in sites with a perforated schneiderian membrane: What is the effect of placing a collagen membrane in a rabbit model? Clin. Oral Implant. Res. 2018, 29, 1202–1211. [Google Scholar] [CrossRef] [PubMed]
- Paik, J.W.; Cha, J.K.; Paeng, K.W.; Kim, M.J.; Thoma, D.S.; Jung, R.E.; Jung, U.W. Volume stability of the augmented sinus using a collagenated bovine bone mineral grafted in case of a perforated Schneiderian membrane: An experimental study in rabbits. J. Clin. Periodontol. 2020, 47, 649–656. [Google Scholar] [CrossRef] [PubMed]
- Paik, J.W.; Cha, J.K.; Song, Y.W.; Thoma, D.S.; Jung, R.E.; Jung, U.W. Effect of Schneiderian membrane integrity on bone formation in sinus augmentation: An experimental study in rabbits. J. Clin. Periodontol. 2021. Online ahead of print. [Google Scholar] [CrossRef] [PubMed]



| Patient No. | Sex/Age (years) | Smoking | Residual Bone Height (mm) | Implant Sites * | Implant Diameter and Length (mm) | Follow-Up after Final Prosthesis Insertion (Months) | Postoperative Sequelae | Sinus Membrane Thickening (Pre-Operative/at the Time of Final Prosthesis Insertion [mm]) |
|---|---|---|---|---|---|---|---|---|
| 1 | Male/39 | Yes | 4.0 | 24 | 3.8 × 12.0 | 23 | Pain, nasal bleeding, and wound dehiscence | 41.7/9.1 |
| 4.0 | 26 | 4.8 × 10.0 | ||||||
| 3.5 | 27 | 4.8 × 10.0 | ||||||
| 2 | Male/47 | Yes | 2.0 | 17 | 5.0 × 10.0 | 12 | Pain, nasal bleeding, and wound dehiscence | 32.5/8.5 |
| 1.5 | 15 | 4.5 × 10.0 | ||||||
| 3 | Male/49 | Yes | 4.0 | 17 | 4.8 × 10.0 | 36 | Pain, nasal bleeding | 38.3/5.8 |
| 0.8 | 16 | 6.0 × 10.0 | ||||||
| 3.1 | 14 | 3.8 × 10.0 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Park, W.-B.; Park, J.S.; Han, J.-Y.; Shin, S.-I.; Lim, H.-C. Removal of Inflammatory Tissue/Product by Sinus Membrane Puncturing during Lateral Sinus Augmentation in Asymptomatic Patients with Severely Opacified Sinuses: A Case Series. Appl. Sci. 2021, 11, 11831. https://doi.org/10.3390/app112411831
Park W-B, Park JS, Han J-Y, Shin S-I, Lim H-C. Removal of Inflammatory Tissue/Product by Sinus Membrane Puncturing during Lateral Sinus Augmentation in Asymptomatic Patients with Severely Opacified Sinuses: A Case Series. Applied Sciences. 2021; 11(24):11831. https://doi.org/10.3390/app112411831
Chicago/Turabian StylePark, Won-Bae, Jung Soo Park, Ji-Young Han, Seung-Il Shin, and Hyun-Chang Lim. 2021. "Removal of Inflammatory Tissue/Product by Sinus Membrane Puncturing during Lateral Sinus Augmentation in Asymptomatic Patients with Severely Opacified Sinuses: A Case Series" Applied Sciences 11, no. 24: 11831. https://doi.org/10.3390/app112411831
APA StylePark, W.-B., Park, J. S., Han, J.-Y., Shin, S.-I., & Lim, H.-C. (2021). Removal of Inflammatory Tissue/Product by Sinus Membrane Puncturing during Lateral Sinus Augmentation in Asymptomatic Patients with Severely Opacified Sinuses: A Case Series. Applied Sciences, 11(24), 11831. https://doi.org/10.3390/app112411831






