Effects of a Single Session of Floss Band Intervention on Flexibility of Thigh, Knee Joint Proprioception, Muscle Force Output, and Dynamic Balance in Young Adults
Abstract
:1. Introduction
2. Materials and Methods
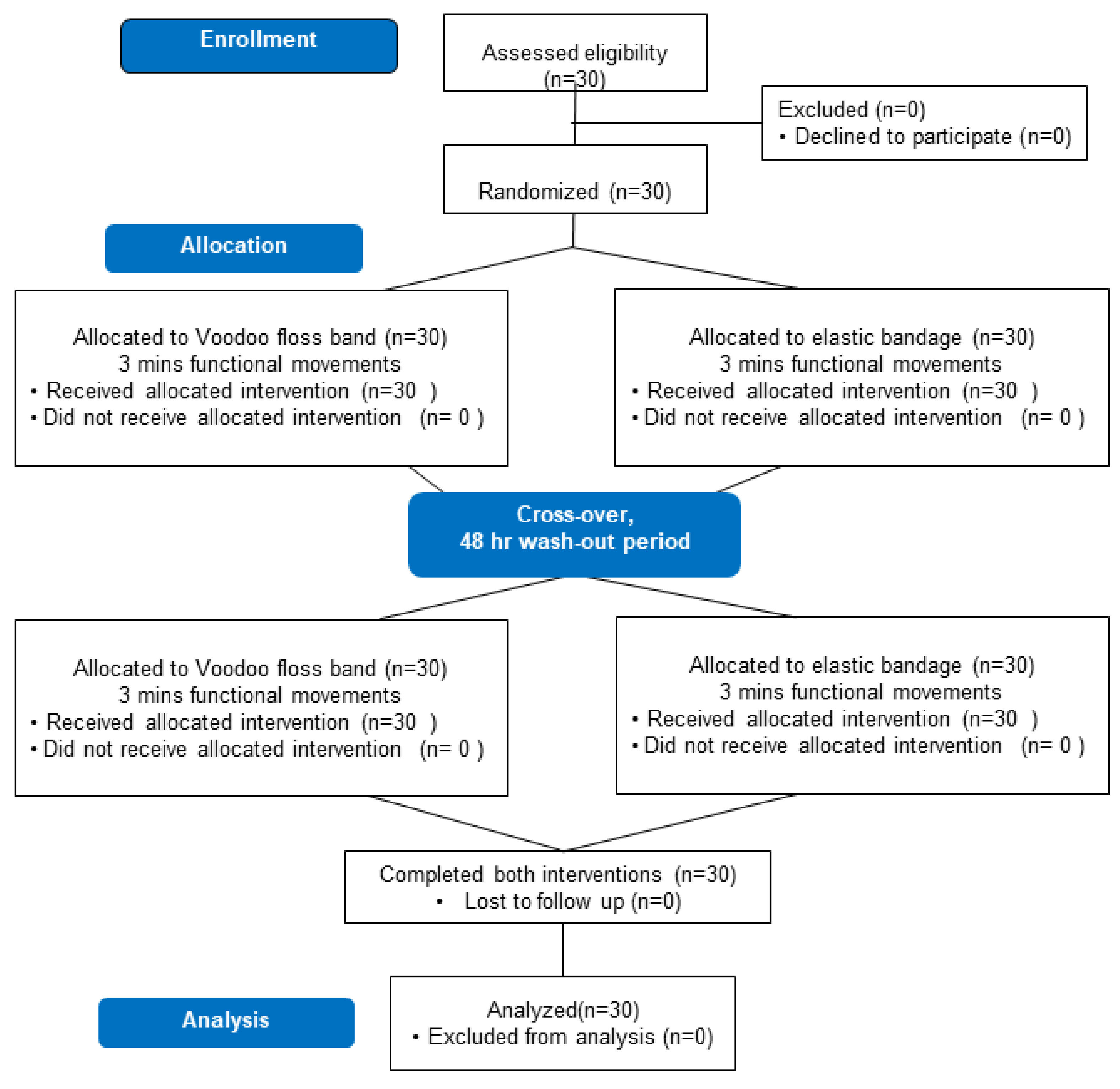
2.1. Participants
2.2. Study Procedures
2.3. Outcome Measures
2.3.1. Primary Outcome
2.3.2. Secondary Outcomes
2.4. Intervention Protocols
2.4.1. Elastic Bandage Intervention
2.4.2. Floss Band Intervention
2.5. Statistical Analyses
3. Results
3.1. Primary Outcomes
3.2. Secondary Outcomes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Opplert, J.; Babault, N. Acute Effects of Dynamic Stretching on Muscle Flexibility and Performance: An Analysis of the Current Literature. Sports Med. 2018, 48, 299–325. [Google Scholar] [CrossRef] [PubMed]
- Kiefer, B.; Lemarr, K.; Enriquez, C.; Tivener, K. A Pilot Study: Psychological Effects of the Voodoo Floss Band on Glenohumeral Flexibility. Int. J. Athl. Ther. Train. 2017, 22, 1–16. [Google Scholar]
- Starrett, K.; Cordoza, G. Becoming a Supple Leopard: The Ultimate Guide to Resolving Pain, Preventing Injury, and Optimizing Athletic Performance, 2nd ed.; Victory Belt Publishing: Las Vegas, NV, USA, 2013. [Google Scholar]
- Vogrin, M.; Kalc, M.; Licen, T. Acute Effects of Tissue Flossing around the Upper Thigh on Neuromuscular Performance: A Study Using Different Degrees of Wrapping Pressure. J. Sport Rehabil. 2020, 30, 601–608. [Google Scholar] [CrossRef]
- Kaneda, H.; Takahira, N.; Tsuda, K.; Tozaki, K.; Kudo, S.; Takahashi, Y.; Sasaki, S.; Kenmoku, T. Effects of Tissue Flossing and Dynamic Stretching on Hamstring Muscles Function. J. Sports Sci. Med. 2020, 19, 681–689. [Google Scholar] [PubMed]
- Reeves, G.V.; Kraemer, R.R.; Hollander, D.B.; Clavier, J.; Thomas, C.; Francois, M.; Castracane, V.D. Comparison of hormone responses following light resistance exercise with partial vascular occlusion and moderately difficult resistance exercise without occlusion. J. Appl. Physiol. 2006, 101, 1616–1622. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Takarada, Y.; Nakamura, Y.; Aruga, S.; Onda, T.; Miyazaki, S.; Ishii, N. Rapid increase in plasma growth hormone after low-intensity resistance exercise with vascular occlusion. J. Appl. Physiol. 2000, 88, 61–65. [Google Scholar] [CrossRef] [Green Version]
- Loenneke, J.P.; Wilson, J.M.; Marín, P.J.; Zourdos, M.C.; Bemben, M.G. Low intensity blood flow restriction training: A meta-analysis. Eur. J. Appl. Physiol. 2012, 112, 1849–1859. [Google Scholar] [CrossRef]
- Pope, Z.K.; Willardson, J.M.; Schoenfeld, B.J. Exercise and blood flow restriction. J. Strength Cond. Res. 2013, 27, 2914–2926. [Google Scholar] [CrossRef] [Green Version]
- Lawson, C.S.; Downey, J.M. Preconditioning: State of the art myocardial protection. Cardiovasc. Res. 1993, 27, 542–550. [Google Scholar] [CrossRef]
- Pang, C.Y.; Yang, R.Z.; Zhong, A.; Xu, N.; Boyd, B.; Forrest, C.R. Acute ischaemic preconditioning protects against skeletal muscle infarction in the pig. Cardiovasc. Res. 1995, 29, 782–788. [Google Scholar] [CrossRef]
- Konrad, A.; Mocnik, R.; Nakamura, M. Effects of Tissue Flossing on the Healthy and Impaired Musculoskeletal System: A Scoping Review. Front. Physiol. 2021, 12, 666129. [Google Scholar] [CrossRef]
- Pavlů, D.; Pánek, D.; Kuncová, E.; Thung, J.S. Effect of Blood Circulation in the Upper Limb after Flossing Strategy. Appl. Sci. 2021, 11, 1634. [Google Scholar] [CrossRef]
- Wortman, R.J.; Brown, S.M.; Savage-Elliott, I.; Finley, Z.J.; Mulcahey, M.K. Blood Flow Restriction Training for Athletes: A Systematic Review. Am. J. Sports Med. 2021, 49, 1938–1944. [Google Scholar] [CrossRef] [PubMed]
- Driller, M.W.; Overmayer, R.G. The effects of tissue flossing on ankle range of motion and jump performance. Phys. Ther. Sport 2017, 25, 20–24. [Google Scholar] [CrossRef] [PubMed]
- Vogrin, M.; Novak, F.; Licen, T.; Greiner, N.; Mikl, S.; Kalc, M. Acute Effects of Tissue Flossing on Ankle Range of Motion and Tensiomyography Parameters. J. Sport Rehabil. 2020, 30, 129–135. [Google Scholar] [CrossRef] [PubMed]
- Kielur, D.S.; Powden, C.J. Changes of Ankle Dorsiflexion Using Compression Tissue Flossing: A Systematic Review and Meta-Analysis. J. Sport Rehabil. 2020, 30, 306–314. [Google Scholar] [CrossRef] [PubMed]
- Kruse, S. Easy Flossing, 1st ed.; Georg Thieme Verlag KG: Stuttgart, Germany, 2018. [Google Scholar]
- Kumar, B.; Das, A.; Alagirusamy, R. Effect of material and structure of compression bandage on interface pressure variation over time. Phlebology 2014, 29, 376–385. [Google Scholar] [CrossRef] [PubMed]
- Ahlhorn, A.; Krämer, D. Flossing in Therapie und Training; Riva: Munich, Germany, 2016. [Google Scholar]
- Suresh, K. An overview of randomization techniques: An unbiased assessment of outcome in clinical research. J. Hum. Reprod. Sci. 2011, 4, 8–11. [Google Scholar] [CrossRef] [PubMed]
- Youdas, J.W.; Krause, D.A.; Hollman, J.H.; Harmsen, W.S.; Laskowski, E. The influence of gender and age on hamstring muscle length in healthy adults. J. Orthop. Sports Phys. Ther. 2005, 35, 246–252. [Google Scholar] [CrossRef] [PubMed]
- Butler, R.J.; Southers, C.; Gorman, P.P.; Kiesel, K.B.; Plisky, P.J. Differences in soccer players’ dynamic balance across levels of competition. J. Athl. Train. 2012, 47, 616–620. [Google Scholar] [CrossRef] [Green Version]
- Lee, C.L.; Chu, I.H.; Lyu, B.J.; Chang, W.D.; Chang, N.J. Comparison of vibration rolling, nonvibration rolling, and static stretching as a warm-up exercise on flexibility, joint proprioception, muscle strength, and balance in young adults. J. Sports Sci. 2018, 36, 2575–2582. [Google Scholar] [CrossRef]
- Callaghan, M.J.; Selfe, J.; Bagley, P.J.; Oldham, J.A. The Effects of Patellar Taping on Knee Joint Proprioception. J. Athl. Train. 2002, 37, 19–24. [Google Scholar] [CrossRef] [Green Version]
- Drouin, J.M.; Valovich-mcLeod, T.C.; Shultz, S.J.; Gansneder, B.M.; Perrin, D.H. Reliability and validity of the Biodex system 3 pro isokinetic dynamometer velocity, torque and position measurements. Eur. J. Appl. Physiol. 2004, 91, 22–29. [Google Scholar] [PubMed]
- Charlier, R.; Mertens, E.; Lefevre, J.; Thomis, M. Muscle mass and muscle function over the adult life span: A cross-sectional study in Flemish adults. Arch. Gerontol. Geriatr. 2015, 61, 161–167. [Google Scholar] [CrossRef]
- Linek, P.; Sikora, D.; Wolny, T.; Saulicz, E. Reliability and number of trials of Y Balance Test in adolescent athletes. Musculoskelet. Sci. Pract. 2017, 31, 72–75. [Google Scholar] [CrossRef] [PubMed]
- Cheatham, S.W.; Baker, R. Technical Report: Quantification of the Rockfloss® Floss Band Stretch Force at Different Elongation Lengths. J. Sport Rehabil. 2019, 29, 377–380. [Google Scholar] [CrossRef] [PubMed]
- Haff, G.G.; Triplett, N.T. Essentials of Strength Training and Conditioning, 4th ed.; Human Kinetics: Champaign, IL, USA, 2015. [Google Scholar]
- Faul, F.; Erdfelder, E.; Lang, A.G.; Buchner, A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef]
- Lyu, B.J.; Lee, C.L.; Chang, W.D.; Chang, N.J. Effects of Vibration Rolling with and without Dynamic Muscle Contraction on Ankle Range of Motion, Proprioception, Muscle Strength and Agility in Young Adults: A Crossover Study. Int. J. Environ. Res. Public Health 2020, 17, 354. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, S.; Lee, D.K. What is the proper way to apply the multiple comparison test? Korean J. Anesthesiol. 2020, 73, 572. [Google Scholar] [CrossRef]
- Lakens, D. Calculating and reporting effect sizes to facilitate cumulative science: A practical primer for t-tests and ANOVAs. Front. Psychol. 2013, 4, 863. [Google Scholar] [CrossRef] [Green Version]
- Behm, D.G.; Wilke, J. Do Self-Myofascial Release Devices Release Myofascia? Rolling Mechanisms: A Narrative Review. Sports Med. 2019, 49, 1173–1181. [Google Scholar] [CrossRef] [PubMed]
- Plocker, D.; Wahlquist, B.; Dittrich, B. Effects of tissue flossing on upper extremity range of motion and power. Int. J. Exerc. Sci. Conf. Proc. 2015, 12, 37. [Google Scholar]
- Hodeaux, K. The Effect of Floss Bands on Elbow Range of Motion in Tennis Players. Bachelor’s Thesis, University of Arkansas, Fayetteville, NC, USA, 2017. [Google Scholar]
- Mills, B.; Mayo, B.; Tavares, F.; Driller, M. The Effect of Tissue Flossing on Ankle Range of Motion, Jump, and Sprint Performance in Elite Rugby Union Athletes. J. Sport Rehabil. 2019, 29, 282–286. [Google Scholar] [CrossRef] [Green Version]
- Konrad, A.; Bernsteiner, D.; Budini, F.; Reiner, M.M.; Glashuttner, C.; Berger, C.; Tilp, M. Tissue flossing of the thigh increases isometric strength acutely but has no effects on flexibility or jump height. Eur. J. Sport Sci. 2020, 21, 1648–1658. [Google Scholar] [CrossRef]
- Driller, M.; Mackay, K.; Mills, B.; Tavares, F. Tissue flossing on ankle range of motion, jump and sprint performance: A follow-up study. Phys. Ther. Sport 2017, 28, 29–33. [Google Scholar] [CrossRef] [PubMed]
- Hjortskov, N.; Skotte, J.; Hye-Knudsen, C.; Fallentin, N. Sympathetic outflow enhances the stretch reflex response in the relaxed soleus muscle in humans. J. Appl. Physiol. 2005, 98, 1366–1370. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hodgson, M.; Docherty, D.; Robbins, D. Post-activation potentiation: Underlying physiology and implications for motor performance. Sports Med. 2005, 35, 585–595. [Google Scholar] [CrossRef]
- Mitchell, C.J.; Sale, D.G. Enhancement of jump performance after a 5-RM squat is associated with postactivation potentiation. Eur. J. Appl. Physiol. 2011, 111, 1957–1963. [Google Scholar] [CrossRef]
- Ager, A.L.; Borms, D.; Deschepper, L.; Dhooghe, R.; Dijkhuis, J.; Roy, J.S.; Cools, A. Proprioception: How is it affected by shoulder pain? A systematic review. J. Hand Ther. 2020, 33, 507–516. [Google Scholar] [CrossRef]
- Roijezon, U.; Clark, N.C.; Treleaven, J. Proprioception in musculoskeletal rehabilitation. Part 1: Basic science and principles of assessment and clinical interventions. Man. Ther. 2015, 20, 368–377. [Google Scholar] [CrossRef]
- Aslan, H.; Buddhadev, H.H.; Suprak, D.N.; San Juan, J.G. Acute effects of two hip flexor stretching techniques on knee joint position sense and balance. Int. J. Sports Phys. Ther. 2018, 13, 846–859. [Google Scholar] [CrossRef] [PubMed]
- Galis, J.; Cooper, D.J. Application of a Floss Band at Differing Pressure Levels: Effects at the Ankle Joint. J. Strength Cond. Res. 2020. [Google Scholar] [CrossRef]



| Parameter | Intervention | Pre | Post Immediately | Post 20 min | p Immediately | p Post 20 min | Effect Size Immediately | Effect Size 20 min | |
|---|---|---|---|---|---|---|---|---|---|
| Flexibility | Hamstring (degrees) | FB | 147 ± 10.69 | 155.06 ± 9.36 *# | 154.7 ± 10.8 *# | <0.001 | <0.001 | 0.8 | 0.72 |
| EB | 149.06 ± 12.58 | 147.06 ± 11.17 | 147.58 ± 11.03 | 0.079 | 0.689 | 0.17 | 0.13 | ||
| Quadriceps (degrees) | FB | 129.81 ± 10.69 | 132.67 ± 6.74 *# | 132.77 ± 6.92 *# | <0.001 | <0.001 | 0.32 | 0.33 | |
| EB | 129.4 ± 7.9 | 129.39 ± 8.19 | 129.52 ± 8.6 | 1 | 1 | 0 | 0.01 | ||
| Joint Proprioception | Joint reposition error (degrees) | FB | 4.42 ± 2.17 | 3.88 ± 2.13 | 4.97 ± 4.19 | 0.39 | 0.76 | 0.25 | 0.16 |
| EB | 3.69 ± 2.34 | 4.29 ± 2.61 | 4.25 ± 2.31 | 0.47 | 0.42 | 0.24 | 0.24 | ||
| Muscle Strength | Quadriceps (N-m/Kg) | FB | 1.22 ± 0.43 | 2.19 ± 0.56 * | 1.38 ± 0.47 * | 0.007 | <0.001 | 1.94 | 0.36 |
| EB | 1.25 ± 0.37 | 2.13 ± 0.58 * | 1.35 ± 0.43 * | 0.007 | <0.001 | 1.8 | 0.25 | ||
| Hamstrings (N-m/Kg) | FB | 2.12 ± 0.52 | 1.37 ± 0.31 * | 2.12 ± 0.46 # | <0.001 | 1 | 1.75 | 0 | |
| EB | 2.12 ± 0.49 | 1.34 ± 0.34 * | 1.95 ± 0.56 * | <0.001 | <0.001 | 1.83 | 0.32 | ||
| Dynamic Balance | Y-balance test | FB | 0.93 ± 0.07 | 0.97 ± 0.07 *# | 0.99 ± 0.07 *# | <0.001 | <0.001 | 0.57 | 0.86 |
| EB | 0.94 ± 0.07 | 0.95 ± 0.07 * | 0.96 ± 0.08 | 0.25 | 0.208 | 0.14 | 0.27 | ||
| Post Immediately ΔFB-ΔEB (Effect Size) | 20 min Later ΔFB-ΔEB (Effect Size) | |
|---|---|---|
| Hamstring flexibility (degree) | 10.06 ± 5.3 | 9.18 ± 8.81 |
| (2.09) | (1.58) | |
| Quadriceps flexibility (degree) | 2.87 ± 5.31 | 2.83 ± 4.22 |
| (0.76) | (0.84) | |
| Joint proprioception (degree) | −0.96 ± 4.06 | 0.17 ± 5.52 |
| (−0.24) | (0.04) | |
| Quadriceps Muscle Force Output (N-m/Kg) | 0.07 ± 0.53 | 0.07 ± 0.36 |
| Effect size | (0.17) | (0.21) |
| Hamstrings Muscle Force Output (N-m/Kg) | 0.02 ± 0.35 | 0.15 ± 0.34 |
| (0.08) | (0.65) | |
| Y-balance test | 0.02 ± 0.04 | 0.03 ± 0.05 |
| (0.85) | (0.66) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chang, N.-J.; Hung, W.-C.; Lee, C.-L.; Chang, W.-D.; Wu, B.-H. Effects of a Single Session of Floss Band Intervention on Flexibility of Thigh, Knee Joint Proprioception, Muscle Force Output, and Dynamic Balance in Young Adults. Appl. Sci. 2021, 11, 12052. https://doi.org/10.3390/app112412052
Chang N-J, Hung W-C, Lee C-L, Chang W-D, Wu B-H. Effects of a Single Session of Floss Band Intervention on Flexibility of Thigh, Knee Joint Proprioception, Muscle Force Output, and Dynamic Balance in Young Adults. Applied Sciences. 2021; 11(24):12052. https://doi.org/10.3390/app112412052
Chicago/Turabian StyleChang, Nai-Jen, Wei-Chun Hung, Chia-Lun Lee, Wen-Dien Chang, and Bo-Han Wu. 2021. "Effects of a Single Session of Floss Band Intervention on Flexibility of Thigh, Knee Joint Proprioception, Muscle Force Output, and Dynamic Balance in Young Adults" Applied Sciences 11, no. 24: 12052. https://doi.org/10.3390/app112412052
APA StyleChang, N. -J., Hung, W. -C., Lee, C. -L., Chang, W. -D., & Wu, B. -H. (2021). Effects of a Single Session of Floss Band Intervention on Flexibility of Thigh, Knee Joint Proprioception, Muscle Force Output, and Dynamic Balance in Young Adults. Applied Sciences, 11(24), 12052. https://doi.org/10.3390/app112412052








