Effects of Increased Extracellular Potassium Concentration Induced by Ischemia on the Vulnerability of Ventricular Arrhythmias and the Regularity of Related Ventricular Tachycardia
Abstract
:1. Introduction
2. Materials and Methods
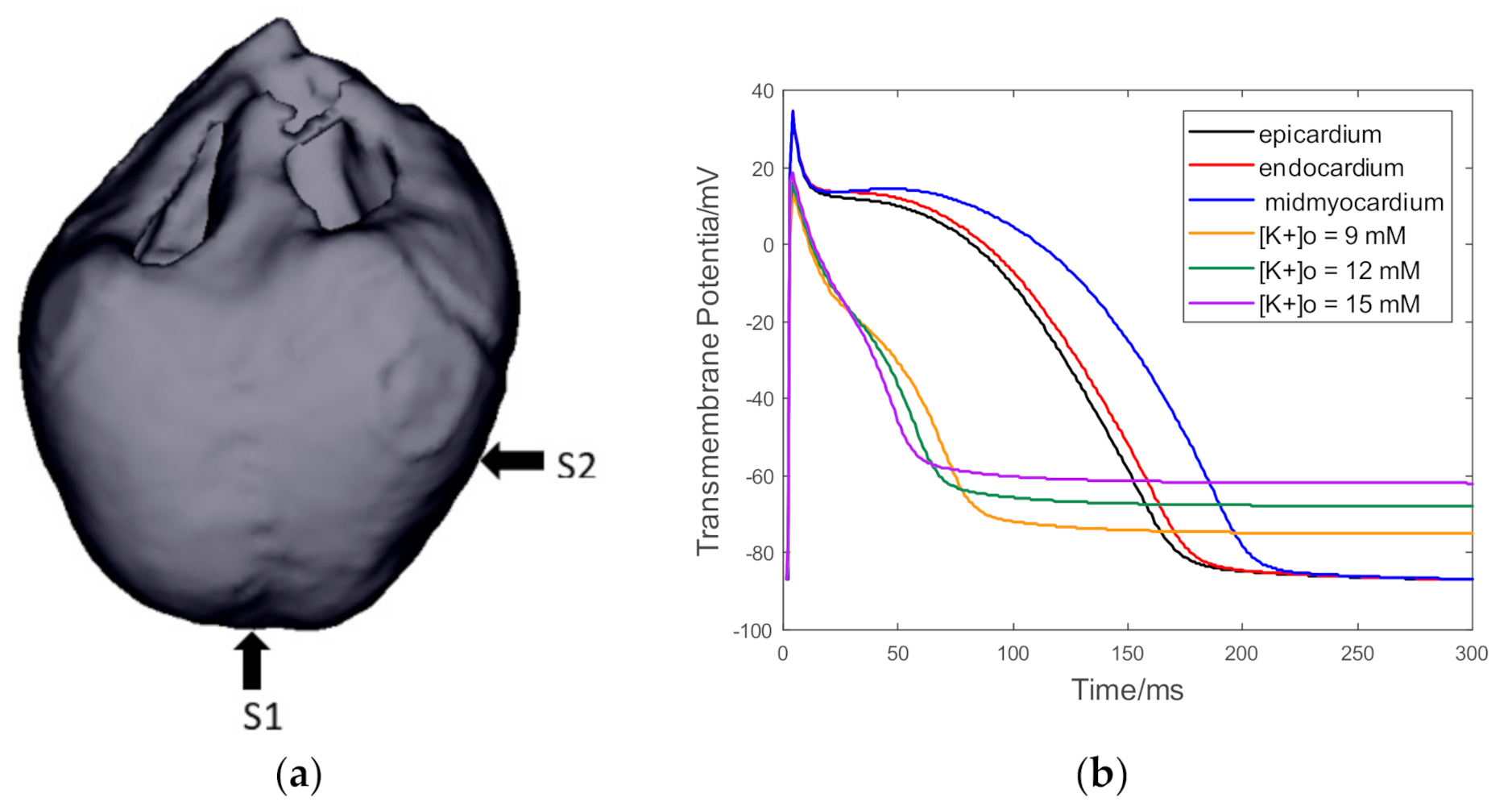
2.1. Construction of Whole Ventricular Electrophysiological Model
2.2. Ventricular Electrophysiological Heterogeneity during Ischemia
2.3. Simulation and Method
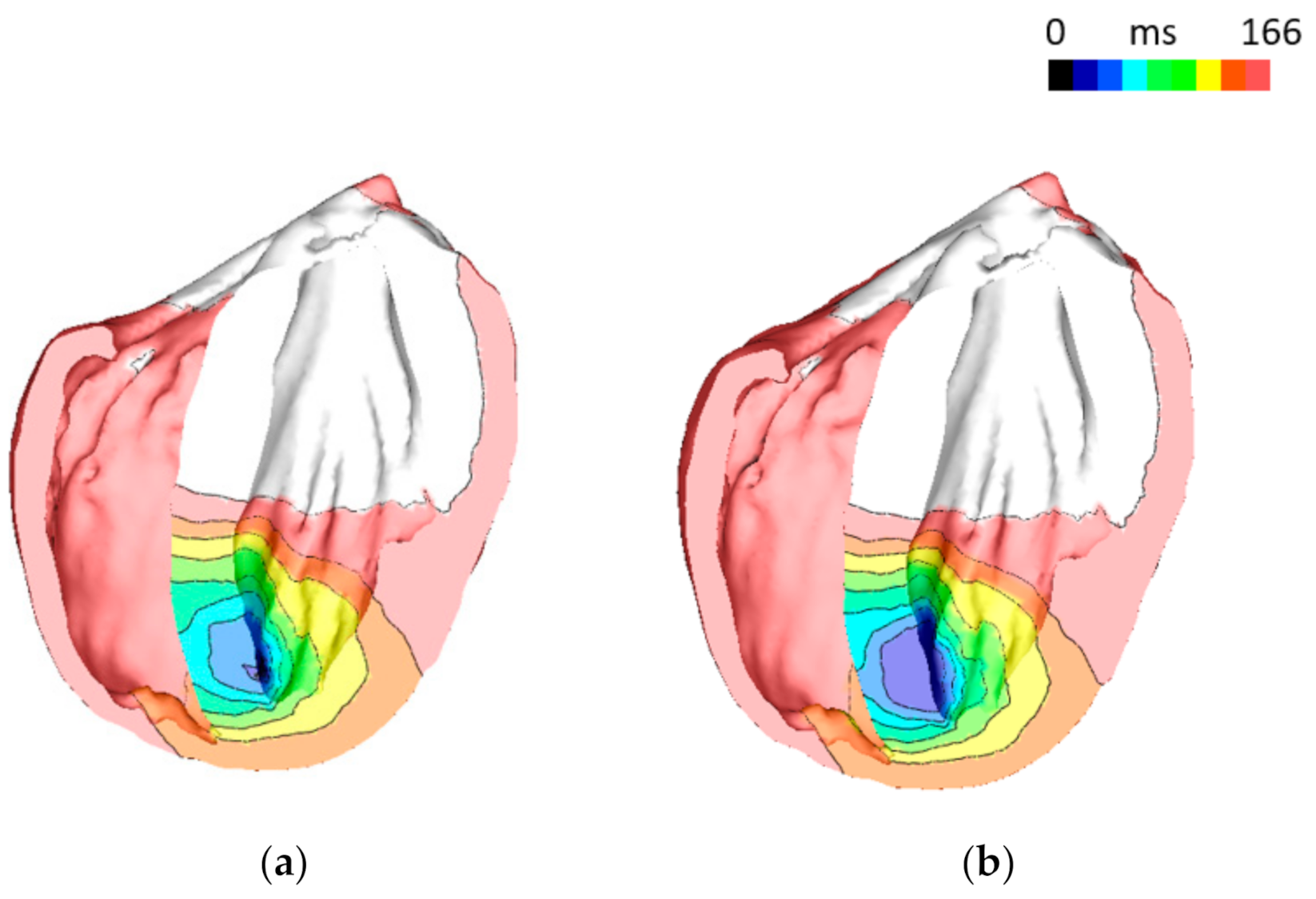
3. Results
4. Discussion
4.1. Verification of Electrophysiological Models of Cardiomyocytes and Ventricles
4.2. Effect of Extracellular Potassium Concentration on Arrhythmia Vulnerability
4.3. Ventricular Depolarization Wave Conduction under the Condition of Myocardial Ischemia
5. Conclusions
6. Limitations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Roger, V.L.; Berry, J.D. Heart disease and stroke statistics—2012 update: A report from the American Heart Association. Circulation 2012, 125, 97–188. [Google Scholar] [CrossRef]
- Kharche, S.R.; Desai, K.; Mcintyre, C.W. Elucidating the relationship between arrhythmia and ischemic heterogeneity: An in silico study. In Proceedings of the 2020 42nd Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Montreal, QC, Canada, 20–24 July 2020. [Google Scholar] [CrossRef]
- Sasaki, T.; Shimazawa, M.; Kanamori, H.; Yamada, Y.; Nishinaka, A.; Kuse, Y.; Suzuki, G.; Masuda, T.; Nakamura, S.; Hosokawa, M.; et al. Effects of progranulin on the pathological conditions in experimental myocardial infarction model. Sci. Rep. 2020, 10, 11842. [Google Scholar] [CrossRef]
- Janse, M.J.; Kleber, A.G. Electrophysiological changes and ventricular arrhythmias in the early phase of regional myocardial ischemia. Circ. Res. 1981, 49, 1069–1081. [Google Scholar] [CrossRef] [Green Version]
- Wagoner, D.R.; Lamorgese, M. Ischemia Potentiates the Mechanosensitive Modulation of Atrial ATP-Sensitive Potassium Channels. Ann. N. Y. Acad. Sci. 2010, 723, 392–395. [Google Scholar] [CrossRef]
- Bozkurt, S. Computational Simulation of Cardiac Function and Blood Flow in the Circulatory System under Continuous Flow Left Ventricular Assist Device Support during Atrial Fibrillation. Appl. Sci. 2020, 10, 876. [Google Scholar] [CrossRef] [Green Version]
- Loewe, A.; Wülfers, E.M.; Seemann, G. Cardiac ischemia-insights from computational models. Herzschrittmacherther. Elektrophysiol. 2018, 29, 48–56. [Google Scholar] [CrossRef] [PubMed]
- Tice, B.M.; Rodríguez, B.; Eason, J.; Trayanova, N. Mechanistic investigation into the arrhythmogenic role of transmural heterogeneities in regional ischaemia phase 1A. Europace 2007, 12, 46–58. [Google Scholar] [CrossRef]
- Rodriguez, B.; Tice, B.M.; Eason, J.C.; Aguel, F.; Trayanova, N. Cardiac vulnerability to electric shocks during phase 1A of acute global ischemia. Heart Rhythm Off. J. Heart Rhythm Soc. 2004, 1, 695–703. [Google Scholar] [CrossRef] [PubMed]
- McDowell, K.S.; Arevalo, H.J.; Maleckar, M.M.; Trayanova, N.A. Susceptibility to Arrhythmia in the Infarcted Heart Depends on Myofibroblast Density. Biophys. J. 2011, 101, 1307–1315. [Google Scholar] [CrossRef] [Green Version]
- Deng, D.; Arevalo, H.J.; Prakosa, A.; Callans, D.J.; Trayanova, N.A. A feasibility study of arrhythmia risk prediction in patients with myocardial infarction and preserved ejection fraction. Europace 2016, 18, 60–66. [Google Scholar] [CrossRef]
- Fallahi, A.; Khorram, H.G.; Kokabi, A. Electrocardiogram signal generation using electrical model of cardiac cell: Application in cardiac ischemia. J. Med. Eng. Technol. 2019, 43, 207–216. [Google Scholar] [CrossRef]
- Bishop, M.J.; Plank, G.; Burton, R.A.B.; Schneider, J.E.; Gavaghan, D.J.; Grau, V.; Kohl, P. Development of an anatomically detailed MRI-derived rabbit ventricular model and assessment of its impact on simulations of electrophysiological function. Am. J. Physiol. Heart Circ. Physiol. 2010, 298, H699–H718. [Google Scholar] [CrossRef] [Green Version]
- Jin, L.; Wang, J.; Song, B.; Wu, X.; Fang, Z. Low-energy defibrillation with multi-electrodes stimulation: A simulation study. In Proceedings of the 2015 37th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Milan, Italy, 25–29 August 2015. [Google Scholar] [CrossRef]
- Clerc, L. Directional differences of impulse spread in trabecular muscle from mammalian heart. J. Physiol. 1976, 255, 335–346. [Google Scholar] [CrossRef]
- Zhu, H.; Jin, L.; Huang, Y.; Wu, X. A Computer Simulation Research of Two Types of Cardiac Physiological Pacing. Appl. Sci. 2021, 11, 449. [Google Scholar] [CrossRef]
- Mahajan, A.; Shiferaw, Y.; Sato, D.; Baher, A.; Olcese, R.; Xie, L.-H.; Yang, M.-J.; Chen, P.-S.; Restrepo, J.G.; Karma, A.; et al. A Rabbit Ventricular Action Potential Model Replicating Cardiac Dynamics at Rapid Heart Rates. Biophys. J. 2008, 94, 392–410. [Google Scholar] [CrossRef] [Green Version]
- Song, B.; Jin, L.; Wang, J.; Qian, L.; Wu, X. Effects of Electrophysiological Heterogeneity on Vulnerability to Re-Entry in Human Ventricular Tissue: A Simulation Study. In Proceedings of the 2017 39th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Jeju, Korea, 11–15 July 2017; pp. 1274–1277. [Google Scholar] [CrossRef]
- Colonna, P.; Cadeddu, C.; Montisci, R.; Chen, L.; Meloni, L.; Iliceto, S. Transmural heterogeneity of myocardial contraction and ischemia. Diagnosis and clinical implications. Ital. Heart J. Off. J. Ital. Fed. Cardiol. 2000, 1, 174–183. [Google Scholar]
- Curtis, M.J. The rabbit dual coronary perfusion model: A new method for assessing the pathological relevance of individual products of the ischaemic milieu: Role of potassium in arrhythmogenesis. Cardiovasc. Res. 1991, 25, 1010–1022. [Google Scholar] [CrossRef]
- Romero, L.; Trénor, B.; Alonso, J.M.; Tobón, C.; Saiz, J.; Ferrero, J.M., Jr. The Relative Role of Refractoriness and Source-Sink Relationship in Reentry Generation during Simulated Acute Ischemia. Ann. Biomed. Eng. 2009, 37, 1560–1571. [Google Scholar] [CrossRef]
- Dutta, S.; Mincholé, A.; Zacur, E.; Quinn, T.A.; Taggart, P.; Rodríguez, B. Early afterdepolarizations promote transmural reentry in ischemic human ventricles with reduced repolarization reserve. Prog. Biophys. Mol. Biol. 2016, 120, 236–248. [Google Scholar] [CrossRef] [Green Version]
- Glukhov, A.V.; Fedorov, V.V.; Lou, Q.; Ravikumar, V.K.; Kalish, P.W.; Schuessler, R.B.; Moazami, N.; Efimov, I.R. Transmural dispersion of repolarization in failing and nonfailing human ventricle. Circ. Res. 2010, 106, 981–991. [Google Scholar] [CrossRef] [Green Version]
- Wilhelms, M.; Seemann, G. Comparing Simulated Electrocardiograms of Different Stages of Acute Cardiac Ischemia. In Functional Imaging and Modeling of the Heart; Springer: Berlin/Heidelberg, Germany, 2011. [Google Scholar]
- Li, S.; Li, Z.; Sheng, J.; Li, S.; Liu, R. Lecture Series 7 on Electrocardiography-Myocardial Ischemia, Injury and Infarction. Chin. Gen. Pract. 2014, 17, 846–848. [Google Scholar]
- Bertella, M.; Nanna, M.; Vanoli, E.; Scalise, F. Assessing the pattern of ST-segment depression during subendocardial ischemia using a computer simulation of the ventricular electrogram. J. Electrocardiol. 2009, 42, 12–18. [Google Scholar] [CrossRef]
- Rivera-Juárez, A.; Hernández-Romero, I.; Puertas, C.; Zhang-Wang, S.; Sánchez-Álamo, B.; Martins, R.; Figuera, C.; Guillem, M.S.; Climent, A.M.; Fernández-Avilés, F.; et al. Clinical Characteristics and Electrophysiological Mechanisms Underlying Brugada ECG in Patients With Severe Hyperkalemia. J. Am. Heart Assoc. 2019, 8, e010115. [Google Scholar] [CrossRef] [Green Version]
- Janse, M.J.; Van Capelle, F.J.; Morsink, H.; Kléber, A.G.; Wilmsschopman, F.J.G.; Cardinal, R.; D’Alnoncourt, C.N.; Durrer, D. Flow of “injury” current and patterns of excitation during early ventricular arrhythmias in acute regional myocardial ischemia in isolated porcine and canine hearts. Evidence for two different arrhythmogenic mechanisms. Circ. Res. 1980, 47, 151–165. [Google Scholar] [CrossRef] [Green Version]
- Gillis, A.M.; Mathison, H.J.; Kulisz, E.; Lester, W.M. Dispersion of Ventricular Repolarization in Left Ventricular Hypertrophy: Influence of Afterload and Dofetilide. J. Cardiovasc. Electrophysiol. 2010, 9, 988–997. [Google Scholar] [CrossRef]
- Ferrero, J.M., Jr.; Saiz, J.; Ferrero, J.M.; Thakor, N.V. Simulation of action potentials from metabolically impaired cardiac myocytes: Role of ATP-sensitive K+ current. Circ. Res. 1996, 79, 208–221. [Google Scholar] [CrossRef]
- Ghannam, M.; Yokokawa, M.; Liang, J.J.; Cochet, H.; Jais, P.; Dabagh, G.S.; Latchamsetty, R.; Jongnarangsin, K.; Morady, F.; Bogun, F. Clinical Significance of Myocardial Scar in Patients with Frequent Premature Ventricular Complexes Undergoing Catheter Ablation. Heart Rhythm 2020, 18, 20–26. [Google Scholar] [CrossRef]






| Main Input Parameters | Values | Units |
|---|---|---|
| Intracellular conductivity (along the fibers) | 0.0522 | S/m |
| Intracellular conductivity (transverse to the fibers) | 0.0057 | S/m |
| Intracellular conductivity (in sheet normal direction) | 0.0057 | S/m |
| Extracellular conductivity (along the fibers) | 0.186 | S/m |
| Extracellular conductivity (transverse to the fibers) | 0.072 | S/m |
| Extracellular conductivity (in sheet normal direction) | 0.072 | S/m |
| Time step | 50 | ms |
| Cell membrane surface area to volume ratio | 1400 | 1/cm |
| Cell membrane capacitance per unit area | 1 | μF/cm2 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Geng, Z.; Jin, L.; Zhu, H.; Wang, J.; Wu, X. Effects of Increased Extracellular Potassium Concentration Induced by Ischemia on the Vulnerability of Ventricular Arrhythmias and the Regularity of Related Ventricular Tachycardia. Appl. Sci. 2021, 11, 2189. https://doi.org/10.3390/app11052189
Geng Z, Jin L, Zhu H, Wang J, Wu X. Effects of Increased Extracellular Potassium Concentration Induced by Ischemia on the Vulnerability of Ventricular Arrhythmias and the Regularity of Related Ventricular Tachycardia. Applied Sciences. 2021; 11(5):2189. https://doi.org/10.3390/app11052189
Chicago/Turabian StyleGeng, Zihui, Lian Jin, Honglei Zhu, Jianfei Wang, and Xiaomei Wu. 2021. "Effects of Increased Extracellular Potassium Concentration Induced by Ischemia on the Vulnerability of Ventricular Arrhythmias and the Regularity of Related Ventricular Tachycardia" Applied Sciences 11, no. 5: 2189. https://doi.org/10.3390/app11052189
APA StyleGeng, Z., Jin, L., Zhu, H., Wang, J., & Wu, X. (2021). Effects of Increased Extracellular Potassium Concentration Induced by Ischemia on the Vulnerability of Ventricular Arrhythmias and the Regularity of Related Ventricular Tachycardia. Applied Sciences, 11(5), 2189. https://doi.org/10.3390/app11052189






