Developing a Specific MRI Technology to Identify Complications Caused by Breast Implants
Abstract
:1. Introduction
2. Materials and Methods
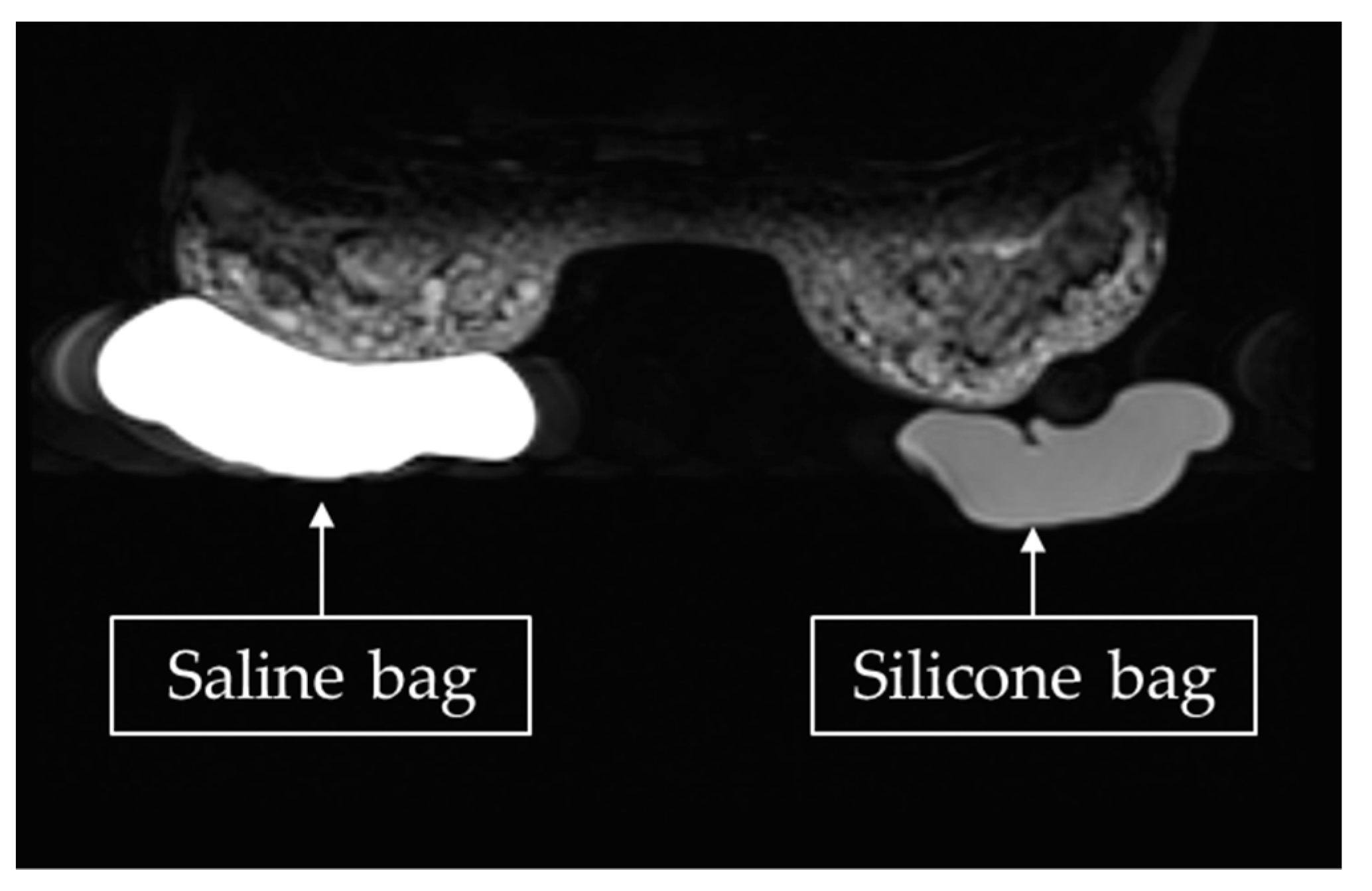
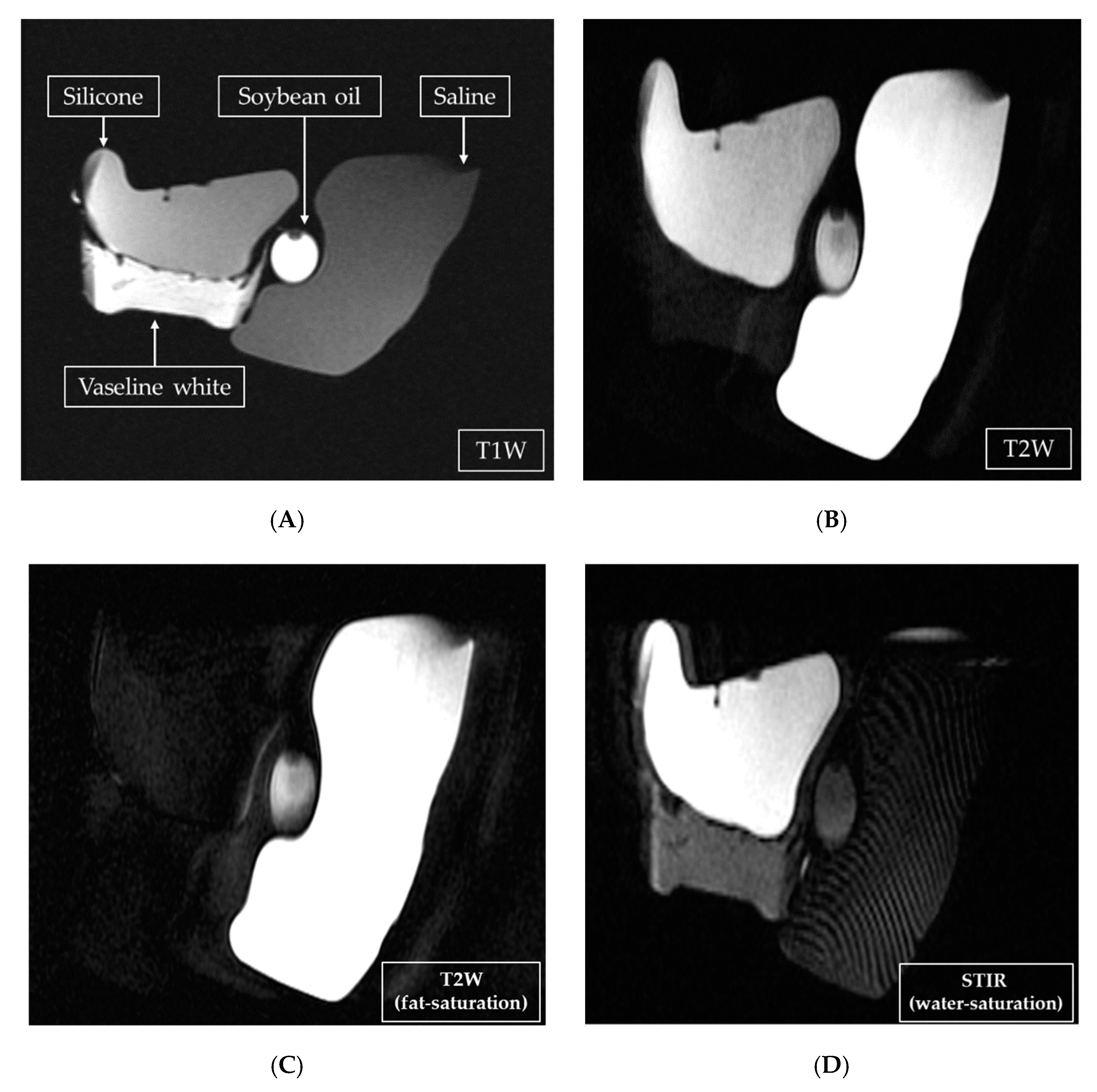
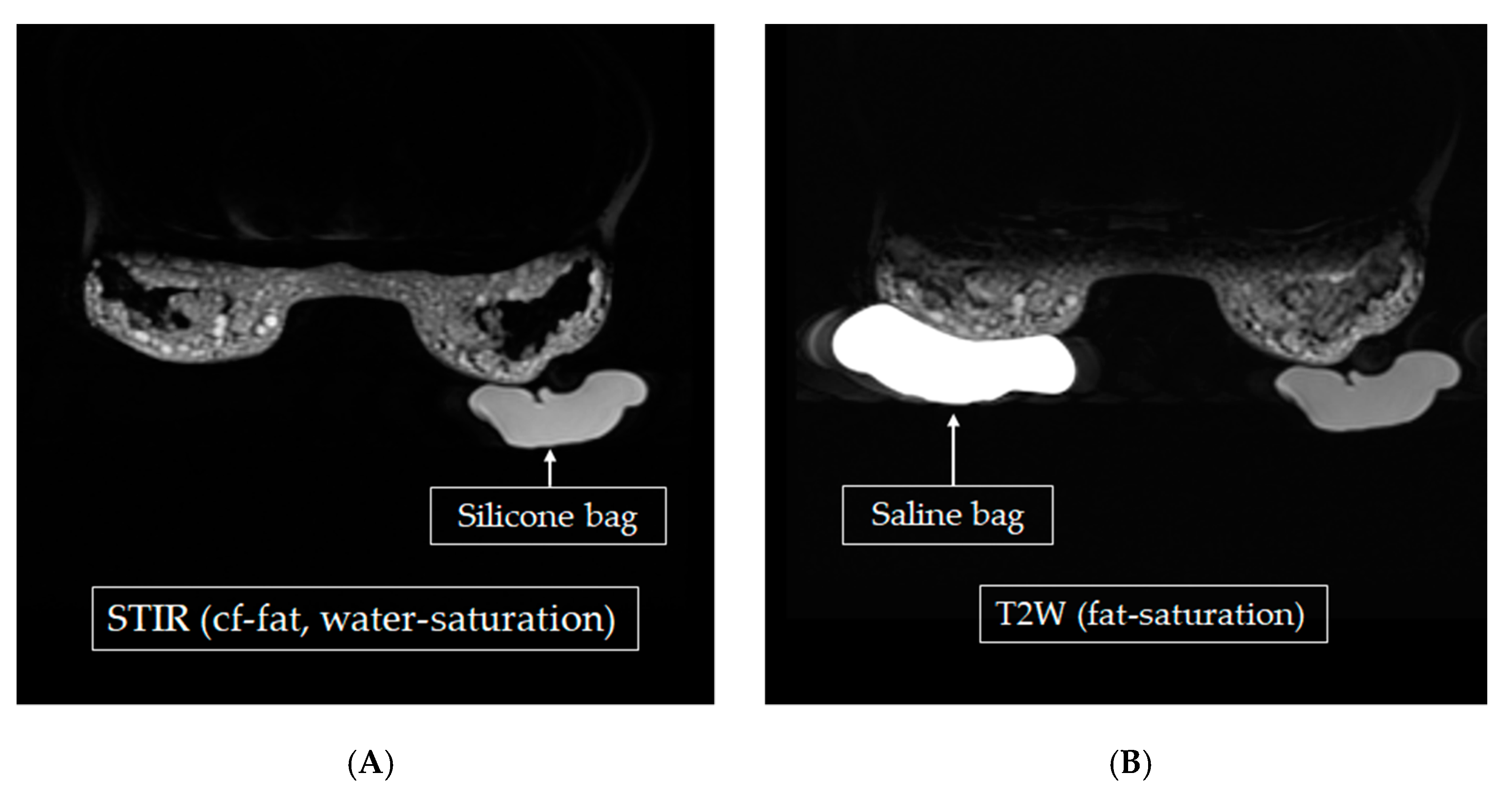
2.1. Homemade Phantom for MRI Scan
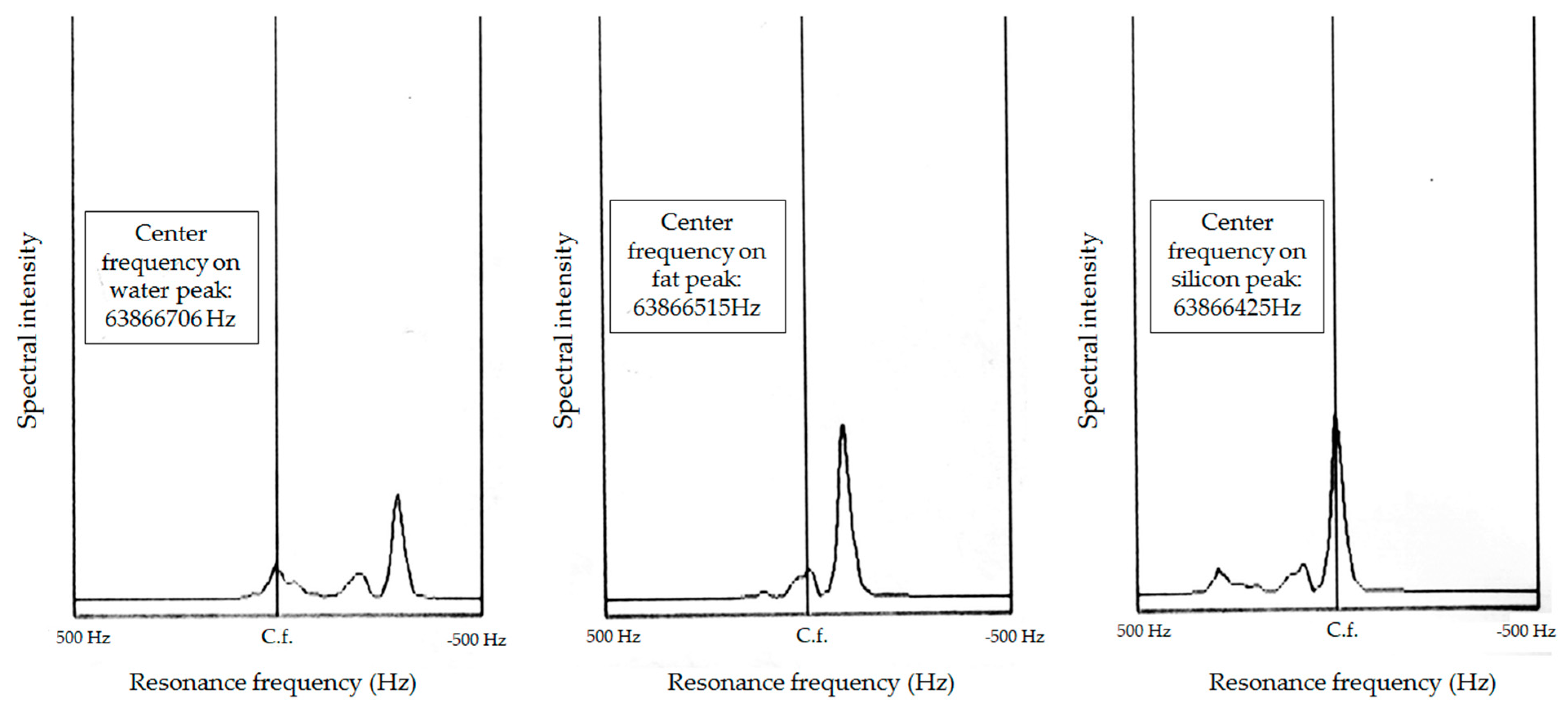
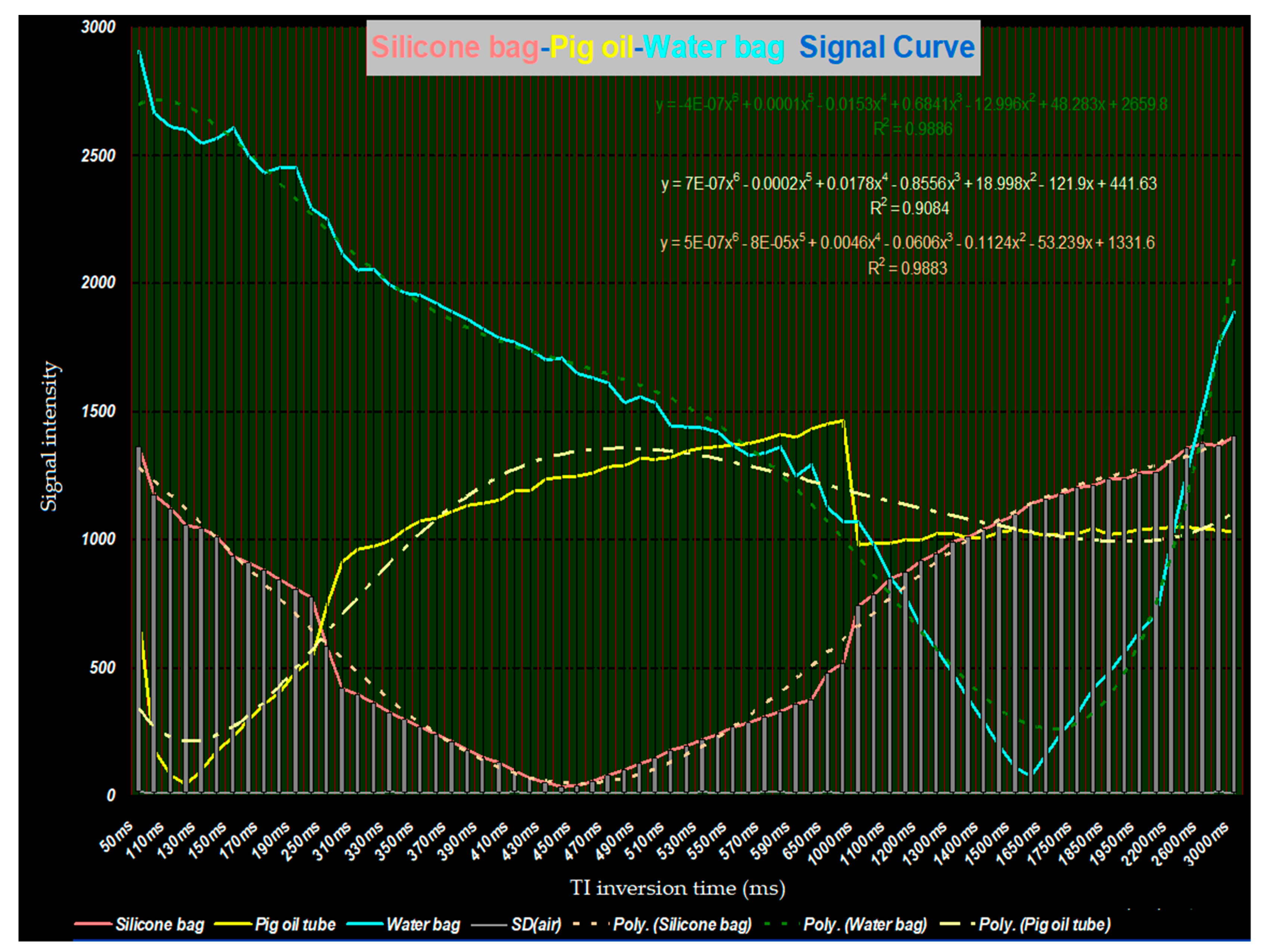
2.2. MRI Scanning Parameters and Image Acquisition
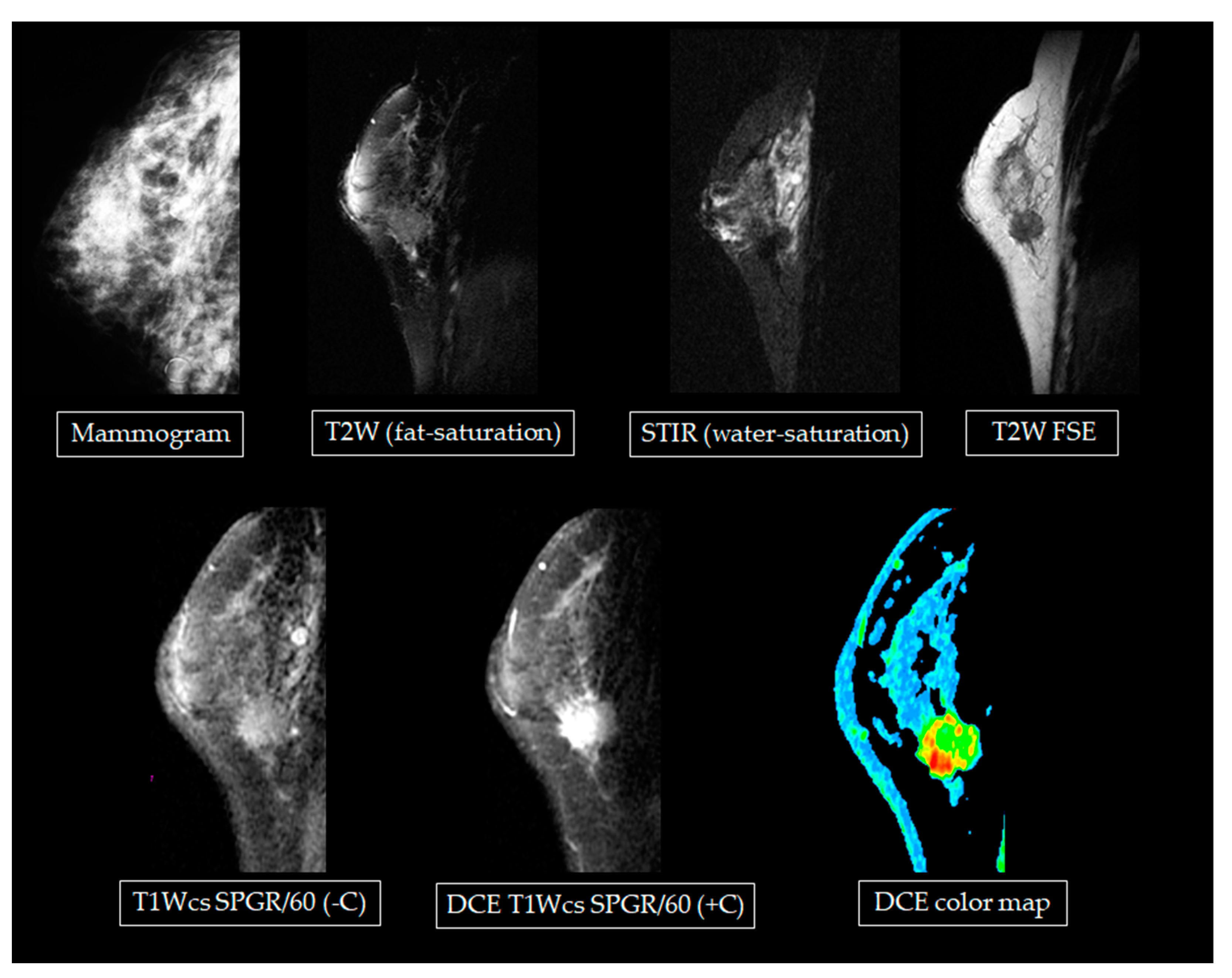
2.3. Scanning Participants who Received Fine-Needle Silicone Injections
2.4. Data Analysis
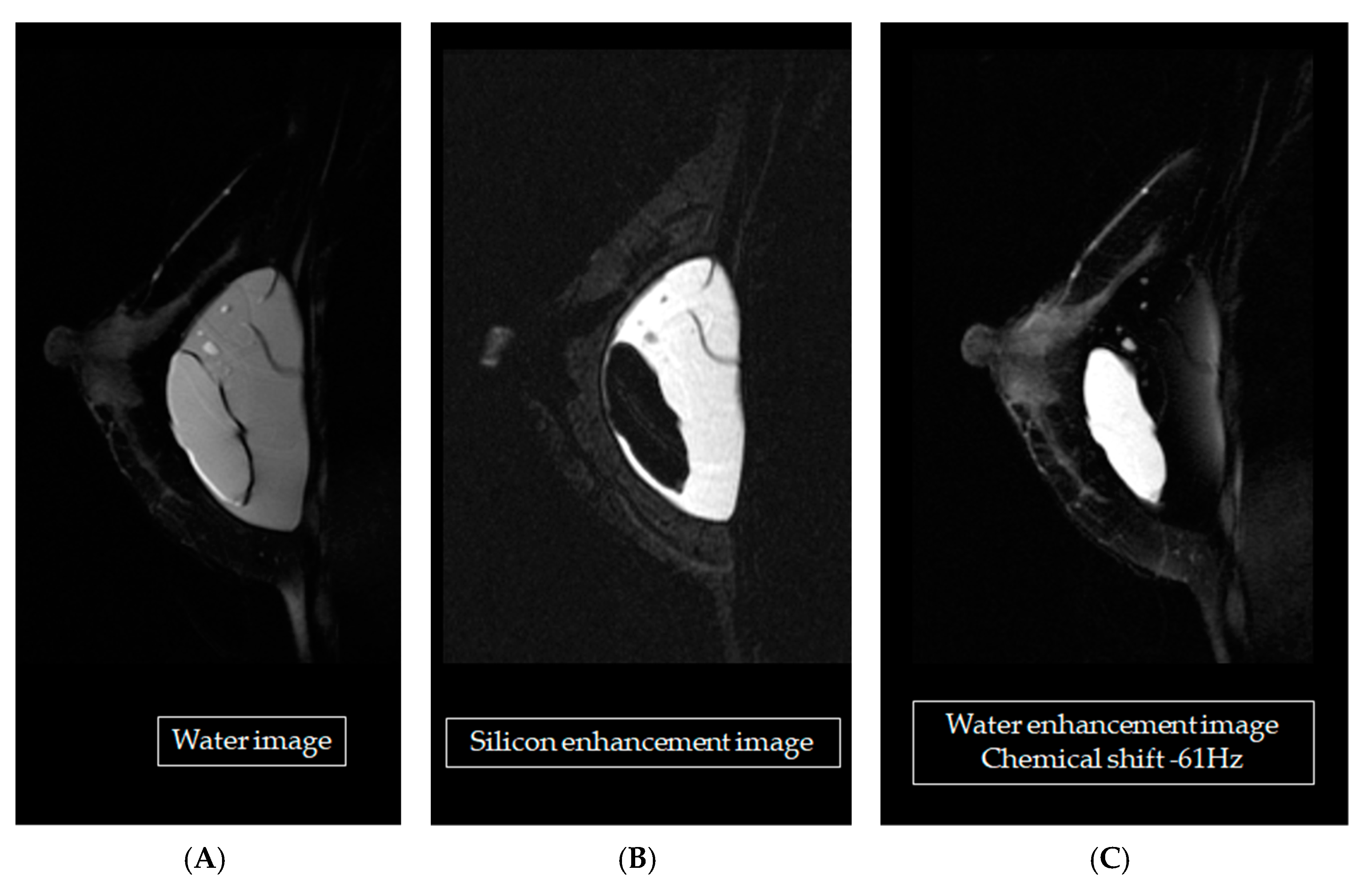
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lalani, T. Breast implant infections: An update. Infect. Dis. Clin. 2018, 32, 877–884. [Google Scholar] [CrossRef] [PubMed]
- Washer, L.L.; Gutowski, K. Breast implant infections. Infect. Dis. Clin. 2012, 26, 111–125. [Google Scholar] [CrossRef] [PubMed]
- Hölmich, L.R.; Friis, S.; Fryzek, J.P.; Vejborg, I.M.; Conrad, C.; Sletting, S.; Olsen, J.H. Incidence of silicone breast implant rupture. Arch. Surg. 2003, 138, 801–806. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hillard, C.; Fowler, J.D.; Barta, R.; Cunningham, B. Silicone breast implant rupture: A review. Gland Surg. 2017, 6, 163. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bretaudeau, C.; Vaysse, C.; Guerby, P.; Lairez, O.; Soule-Tholy, M.; Vidal, F.; Chantalat, E. Pericarditis after breast implant rupture: A case report. Cardiol. Res. 2018, 9, 381. [Google Scholar] [CrossRef] [PubMed]
- Doren, E.L.; Miranda, R.N.; Selber, J.C.; Garvey, P.B.; Liu, J.; Medeiros, L.J.; Butler, C.E. U.S. epidemiology of breast implant-associated anaplastic large cell lymphoma. Plast. Reconstr. Surg. 2017, 139, 1042–1050. [Google Scholar] [CrossRef] [PubMed]
- Seiler, S.J.; Sharma, P.B.; Hayes, J.C.; Ganti, R.; Mootz, A.R.; Eads, E.D.; Evans, W.P. Multimodality imaging-based evaluation of single-lumen silicone breast implants for rupture. Radiographics 2017, 37, 366–382. [Google Scholar] [CrossRef] [PubMed]
- Spear, S.L.; Murphy, D.K.; Allergan Silicone Breast Implant U.S. Core Clinical Study Group. Natrelle round silicone breast implants: Core Study results at 10 years. Plast. Reconstr. Surg. 2014, 133, 1354–1361. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Di Benedetto, G.; Cecchini, S.; Grassetti, L.; Baldassarre, S.; Valeri, G.; Leva, L.; Bertani, A. Comparative study of breast implant ruptures using mammography, sonography, and magnetic resonance imaging: Correlation with surgical findings. Breast J. 2008, 14, 532–537. [Google Scholar] [CrossRef] [PubMed]
- O’Toole, M.; Caskey, C.I. Imaging spectrum of breast implant complications: Mammography, ultrasound, and magnetic resonance imaging. Semin. Ultrasound CT MR. 2000, 21, 351–361. [Google Scholar] [CrossRef]
- Saunders, W.B.; Everson, L.I.; Parantainen, H.; Detlie, T.; Stillman, A.E.; Olson, P.N.; Landis, G.; Griffiths, H.J. Diagnosis of breast implant rupture: Imaging findings and relative efficacies of imaging techniques. AJR Am. J. Roentgenol. 1994, 163, 57–60. [Google Scholar]
- Gomi, N.; Kikuchi, M.; Matsumoto, A.; Tanakura, K.; Sawaizumi, M.; Yano, T.; Ohno, S. Comparison of usefulness of ultrasound and MRI for diagnosis of silicone breast implant rupture in screening asymptomatic women. In Proceedings of the European Congress of Radiology, Vienna, Austria, 15–19 July 2020. [Google Scholar]
- Stivala, A.; Rem, K.; Leuzzi, S.; Moris, V.; François, C.; Revol, M.; Cristofari, S. Efficacy of ultrasound, mammography and magnetic resonance imaging in detecting breast implant rupture: A retrospective study of 175 reconstructive and aesthetic sub-pectoral breast augmentation cases. J. Plast. Reconstr. Aesthet. Surg. 2017, 70, 1520–1526. [Google Scholar] [CrossRef]
- Fleury, E.D.F.C.; Gianini, A.C.; Ayres, V.; Ramalho, L.C.; Seleti, R.O.; Roveda, D. Breast magnetic resonance imaging: Tips for the diagnosis of silicone-induced granuloma of a breast implant capsule (SIGBIC). Insights Imaging 2017, 8, 439–446. [Google Scholar] [CrossRef] [PubMed]
- Maijers, M.C.; Niessen, F.B.; Veldhuizen, J.F.H.; Ritt, M.J.P.F.; Manoliu, R.A. MRI screening for silicone breast implant rupture: Accuracy, inter- and intraobserver variability using explanation results as reference standard. Eur. Radiol. 2014, 24, 1167–1175. [Google Scholar] [CrossRef] [PubMed]
- Rietjens, M.; Villa, G.; Toesca, A.; Rizzo, S.; Raimondi, S.; Rossetto, F.; Petit, J.Y. Appropriate use of magnetic resonance imaging and ultrasound to detect early silicone gel breast implant rupture in postmastectomy reconstruction. Plast. Reconstr. Surg. 2014, 134, 13–20. [Google Scholar] [CrossRef]
- Lindenblatt, N.; El-Rabadi, K.; Helbich, T.H.; Czembirek, H.; Deutinger, M.; Benditte-Klepetko, H. Correlation between MRI results and intraoperative findings in patients with silicone breast implants. Int. J. Womens Health 2014, 6, 703. [Google Scholar] [CrossRef] [Green Version]
- Song, J.W.; Kim, H.M.; Bellfi, L.T.; Chung, K.C. The effect of study design biases on the diagnostic accuracy of magnetic resonance imaging to detect silicone breast implant ruptures: A meta-analysis. Plast. Reconstr. Surg. 2011, 127, 1029. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shah, A.T.; Jankharia, B.B. Imaging of common breast implants and implant-related complications: A pictorial essay. Indian J. Radiol. Imaging 2016, 26, 216. [Google Scholar] [CrossRef]
- Chuangsuwanich, A.; Warnnissorn, M.; Lohsiriwat, V. Siliconoma of the breasts. Gland Surg. 2013, 2, 46. [Google Scholar] [PubMed]
- Hashemi, R.H.; Bradley, W.G.; Lisanti, C.J. MRI: The Basics; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2012. [Google Scholar]
| Pulse Sequence | TR (ms) | TE (ms) | TI (ms) |
|---|---|---|---|
| T1W FSE | 400 | 14 | |
| T1W SPGR/60 | 200 | 1.7 | |
| T2W | 3000 | 103 | |
| T2W fat-saturation | 3000 | 103 | |
| STIR | 4000 | 45 | 170 |
| STIR (water-saturation) | 4000 | 45 | 170 |
| Implant Sequences | Phantom | Breast Tissue | |||
|---|---|---|---|---|---|
| Silicone | Normal Saline | Oil | Gland | Carcinoma | |
| T2W FSE | - | ++ | + | - | - |
| T2W (fat-saturation) | --- | +++ | -- | + | + |
| STIR | + | +++ | -- | + | + |
| STIR (water-saturation) | +++ | --- | -- | -- | - |
| T1W FSE | + | -- | +++ | - | -- |
| T1Wcs SPGR/60 (-C) | -- | + | -- | + | + |
| DCE T1Wcs SPGR/60 (+C) | - | + | - | + | +++ |
| T1Wcs SPGR/60 (+C) | -- | + | -- | ++ | ++ |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lin, M.-F.; Lai, L.-H.; Hsiao, W.-T.; Yao, M.M.-S.; Chan, W.-P. Developing a Specific MRI Technology to Identify Complications Caused by Breast Implants. Appl. Sci. 2021, 11, 3434. https://doi.org/10.3390/app11083434
Lin M-F, Lai L-H, Hsiao W-T, Yao MM-S, Chan W-P. Developing a Specific MRI Technology to Identify Complications Caused by Breast Implants. Applied Sciences. 2021; 11(8):3434. https://doi.org/10.3390/app11083434
Chicago/Turabian StyleLin, Ming-Fang, Lu-Han Lai, Wen-Tien Hsiao, Melissa Min-Szu Yao, and Wing-P Chan. 2021. "Developing a Specific MRI Technology to Identify Complications Caused by Breast Implants" Applied Sciences 11, no. 8: 3434. https://doi.org/10.3390/app11083434
APA StyleLin, M.-F., Lai, L.-H., Hsiao, W.-T., Yao, M. M.-S., & Chan, W.-P. (2021). Developing a Specific MRI Technology to Identify Complications Caused by Breast Implants. Applied Sciences, 11(8), 3434. https://doi.org/10.3390/app11083434






