Abstract
Background: After bilateral transfemoral amputation, people may experience limitations in everyday life due to limited mobility and prosthesis problems. Materials and method: The case study covered a 54-year-old man after bilateral traumatic amputation of his lower limbs. Transfemoral amputations were performed using the Caldwell method; disproportion in the length of stumps was 5 mm. The motion task was recorded using the SMART-E optoelectronic system (BTS Bioengineering, Milan, Italy) according to the standard Davis protocol (the Newington model). Biomechanical evaluation included the measurement of angle-time relationships, characterizing the range of motion (ROM) in lower limb joints and Ground Reaction Force (GRF). The analyzed tasks are walking with self selected speed, fast gait and walking in stubby prostheses. Results: Step width was the most similar to the gait of healthy persons walking with stubby prostheses (0.17 ± 0.01 m for healthy people, 29% higher for stubbies, 35% for prosthetic gait with self-selected gait speed and 41% for fast gait speed). Step width was the smallest when walking with stubbies. Conclusions: The reduction of body height allows to reduce the risk of fall. Higher metabolic cost of gait in people after amputation result from a greater need to maintain balance and posture, and to perform walking movement.
1. Introduction
The percentage of people who have undergone a double amputation above the knee joints (BTA—bilateral transtibial amputation) and use orthopedic products on a daily basis is low. The surgeon, as much as possible, tries to perform the amputation so that the remaining stump will be as highly functional as possible for the patient in terms of prosthesis fitting. Nevertheless, the energy expenditure during the gait cycle increases up to 200% with double transfemoral amputation. Oxygen uptake also increases, compared to 38–49% for unilateral amputees and up to 280% for bilateral amputees. According to studies, the metabolic cost of the gait cycle and ambulatory physical activity are influenced by the amputation level and the number of amputated limbs [1]. The energy expenditure of the gait cycle after having undergone a double amputation above the knee joints is 183% higher than in healthy people [1,2]. Therefore, people who have undergone BTA often reduce their physical activity while increasing the risk of developing cardiometabolic diseases [3,4]. In people who have had a BTA, the development of hypertension, coronary artery disease, diabetes mellitus and chronic kidney disease shortens life expectancy [5]. Reconstructing motor abilities after the amputation of the lower limbs is an extremely important element of physiotherapy. The amputation procedure itself is destructive for the patient, significantly worsening their quality of life, making them a disabled person in the eyes of society. For this reason, it is very important to indicate the optimal possibilities of prosthesis fitting and to restore the patient to a vertical position and gait and a more active lifestyle.
To improve the stability of their gait, people who have undergone a double amputation must increase step width, which contributes to an increase in the metabolic cost of gait [6,7,8,9,10,11]. After undergoing a double amputation, the possibilities of compensation with the limb, which are possible for people after unilateral amputation, are reduced [12]. For this reason, in most cases, compensation for the prostheses must solely come from the hip joints and trunk [7,13,14,15]. Advanced technological prostheses and suspension methods (direct skeletal fixation (DSF) osseointegration—insertion of the implant into the femur) have made it possible to develop prostheses that reduce the size of asymmetry in gait [16,17,18]. However, they do not affect the gait efficiency. The reason is shifting the center of the mass in the proximal direction (from the second sacral vertebra to the thoracolumbar passage) [6]. Stubbies are an alternative to the standardly used prostheses. Stubbies are short non-articulating prostheses. This type of prostheses is used to improve the gait function, allowing one to learn how to gradually load the thigh stumps and improve balance. Some people after being fitted with standard prostheses do not stop using stubbies, especially at home. However, there are concerns that the use of stubbies will lead to worsening of the gait with standard prostheses and will increase the risk of falling. For this reason, the purpose of this case study is to compare the gait function with the standard and stubby prostheses used.
2. Case Report
A 54-year-old man who had undergone bilateral traumatic amputation of his lower limbs was examined. His limbs were amputated on 27 January 2015. Amputations were performed using the Caldwell method at the femoral level. The disproportion in the length of stumps is 5 mm, the right stump is longer. Later, the patient had skin grafting onto the right stump. In the first days after the procedure, early physiotherapy was implemented, including pose positions to prevent contractures; hardening and shaping of stumps using a suction drainage. Then, 6 months after the procedure, the patient was provided with prostheses for early treatment, with a hydraulic monocentric knee joint and a locking mechanism in one of them. The patient was provided with final prostheses which included a hydraulic microprocessor-controlled (Genium X3) monocentric knee joint in November 2016. Biomechanical analysis was performed approximately 4 years after the final prosthesis. The patient’s final prostheses are composed of the following modules: a MAS-type vacuum prosthesis funnel, silicone liners with Ossur seal (put on stumps to improve the comfort of placing the stump in the funnel), hydraulic microprocessor-controlled monocentric knee joint with built-in gyroscopes and a Triton prosthesis foot. The stubby prostheses (stubbies) were made of a MAS-type vacuum prosthesis funnel, silicone liners with Ossur seal and short pylons ended with flat oval overlays (an “elephant foot” shape).
2.1. Outcomes
The examination was conducted in a certified Biomechanical Analysis Laboratory. The motion task was recorded using the SMART-E optoelectronic system (BTS Bioengineering, Milan, Italy) according to the standard Davis protocol (the Newington model) [19]. The system comprises six infrared cameras detecting reflective markers with a sampling rate of 120 Hz. A total of 12 markers were placed on the patient’s skin, lying above the following anatomical points: C7, acromion processes, sacrum, anterior superior iliac spines (ASIS), greater trochanters, thighs (midpoint between greater trochanter and lateral head of the femur), knees (lateral axis of rotation on the Genium X3 knee prosthesis). The measuring station was equipped with Smart Capture software for data recording, Smart Tracker for tracking recording markers and Smart Analyzer for data analysis and processing. The central unit of the computer included a video controller (System VIX) and three ethernet hubs (one 32-channel analogue hub and two digital hubs, each with four communication ports). IR- infrared cameras were fixed rigidly on the walls of the laboratory using support frames.
2.2. Gait Analysis
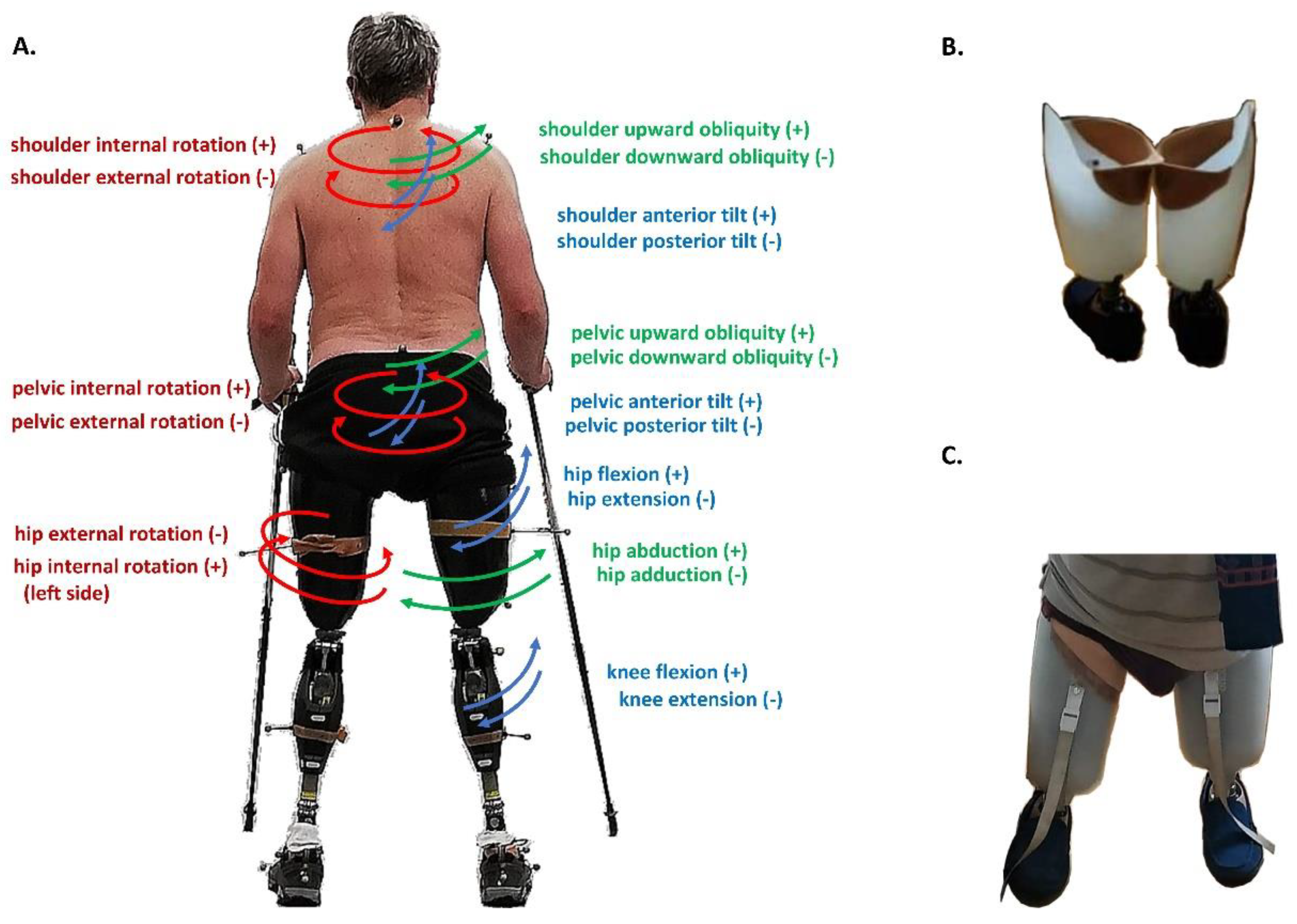
The gait cycle began when a limb first contacted the ground (at 0% Gait C ycle). The participant was asked to walk in both directions on a 6 meter-long path. He covered the distance three times with his preferred gait speed and then three times with a fast gait speed (Figure 1B,C). After walking with standard prostheses, the same path was followed using stubbies with self-selected gait speed. The biomechanical evaluation included the measurement of angle-time relationships, characterizing the range of motion (ROM) in lower limb joints (Figure 1A), in particular:
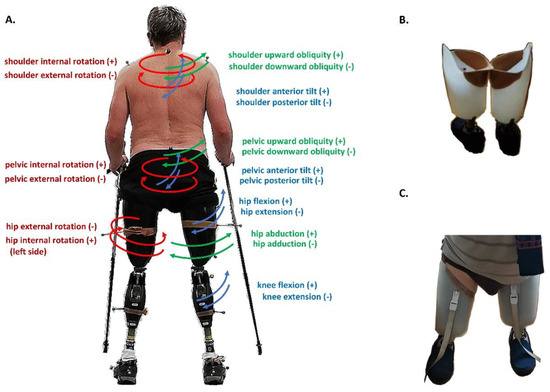
Figure 1.
The main actions at shoulder, pelvis, hip and knee in sagittal (blue), frontal (green) and transversal (red) planes with arrows to explain the directions of motion (A). The stubby prosthesis used in the study is presented from back (B) and front (C).
- shoulder girdle obliquity angle (up/down)—rotation of the mediolateral axis out of the horizontal plane in the frontal plane; a positive value (up) corresponds to the situation in which acromion process markers are higher than the corresponding markers on the contralateral side
- shoulder girdle tilt—anterior/posterior rotation around the mediolateral axis in the transversal plane; a positive value (up) corresponds to the normal situation in which acromion process markers are higher than the corresponding markers on the contralateral side
- shoulder girdle rotation—rotation of the mediolateral axis around the vertical axis in horizontal plane
- pelvic obliquity angle (up/down)—rotation of the mediolateral axis out of the horizontal plane in the frontal plane; a positive value (up) corresponds to the situation in which anterior and posterior superior iliac spine (ASIS and PSIS) markers are higher than the corresponding markers on the contralateral side
- pelvic tilt angle (up/down)—anterior/posterior rotation around the mediolateral axis in the transversal plane; a positive value (up) corresponds to a normal situation in which PSIS is higher than ASIS
- pelvic rotation angle (internal/external)—rotation of the mediolateral axis around the vertical axis in the horizontal plane
- hip ad/abduction angle—rotation of the proximal-distal axis out of the sagittal plane in the frontal plane
- hip flexion/extension angle—rotation of the proximal-distal axis around the mediolateral axis in the sagittal plane; a positive (flexion) angle value corresponds to a situation in which the knee is in front of the body
- hip rotation angle (internal/external)—rotation around the proximal-distal axis in the horizontal plane
- knee flexion/extension angle—rotation of the proximal-distal axis around the mediolateral axis in the sagittal plane; a positive angle corresponds to a flexed knee.
GRF (ground reaction force) data were collected using two Kistler 9286AA-A platforms with a frequency of 1 kHz placed in the middle of the measurement path. Raw GRF measurements were filtered through a second-order Butterworth filter with a cutoff frequency of 6 Hz. For Cartesian principal components of the GRF vector, such as vertical ground reaction force (vGRF), the parameterization was performed by calculating the following variables:
- vF1: maximal vGRF of overweight during the initial weight acceptance phase
- vF2: minimal vGRF of underweight during the middle stance phase
- vF3: maximal vGRF of overweight during the terminal stance phase
From the angle-time series the following parameters were numerically extracted: mean value (an average of 100 values computed over whole gait cycle), maximum and minimum values (peak positive, Peak+ and peak negative, Peak-) and range of motion (the extent of movement, ROM) and expressed in degrees. The values were calculated to compare in descriptive statistics. The obtained data were compared to the gait of non-disabled people [20].
3. Results
In the discussed temporo-spatial parameters, stride length depended on the gait speed and the prosthetic product used; higher values were recorded at a fast gait while lower ones during the gait with stubby prostheses (Table 1). Step width was the most similar to the gait of non-disabled persons. The stride width when walking with stubby prostheses was most similar to the gait of healthy subjects (0.17 ± 0.01 m for healthy people, 29% higher for stubbies, 35% for prosthetic gait with self-selected gait speed and 41% for fast gait speed). The difference in step length between the fast gait and the self-selected gait speed did not exceed 5% compared to the results of healthy people. The gait with stubbies required the highest cadence (gait slower than in healthy people by 81%, cadence higher than in healthy people by 14%) to maintain the gait speed. The division of the gait cycle into phases presented mostly correct proportions, i.e., 60% (stance phase) to 40% (swing phase).

Table 1.
Mean and ± standard deviation of temporo-spatial parameters for prosthetic gait (fast gait, self-selected gait speed and gait with stubby prostheses—stubbies).
The biggest differences in the range of movement (ROM) occurred in the sagittal plane (Table 2). The faster the patient moved, the higher the anterior tilt of the shoulder girdle and pelvis. The difference in the shoulder girdle tilt in ROM between a fast gait and a prosthetic gait with stubbies was 57%. Similarly, the pelvic tilt (physiological gait, ROM 1–2°) during the gait was constantly in anteflexion. When it comes to the gait with stubbies, the difference was the lowest—49% (self-selected gait speed: 59%, fast gait: 56%). Hip flexion/extension in ROM during the gait with stubbies forced higher flexion and extension values due to the lack of knee joints (20%—gait with stubbies, 8%—self-selected gait speed, 4%—fast gait). Due to the need to provide the required gap from the ground, higher values of hip flexion/extension in ROM during the gait with stubbies occurred in the frontal plane. Pelvic obliquity during the gait with stubbies required higher raise to ensure swing (48%—gait with stubbies, 41%—self-selected gait speed, 13%—fast gait).

Table 2.
Parameters characterizing the range of motion for prosthetic gait (fast gait, self-selected gait speed and gait with stubby prostheses—stubbies).
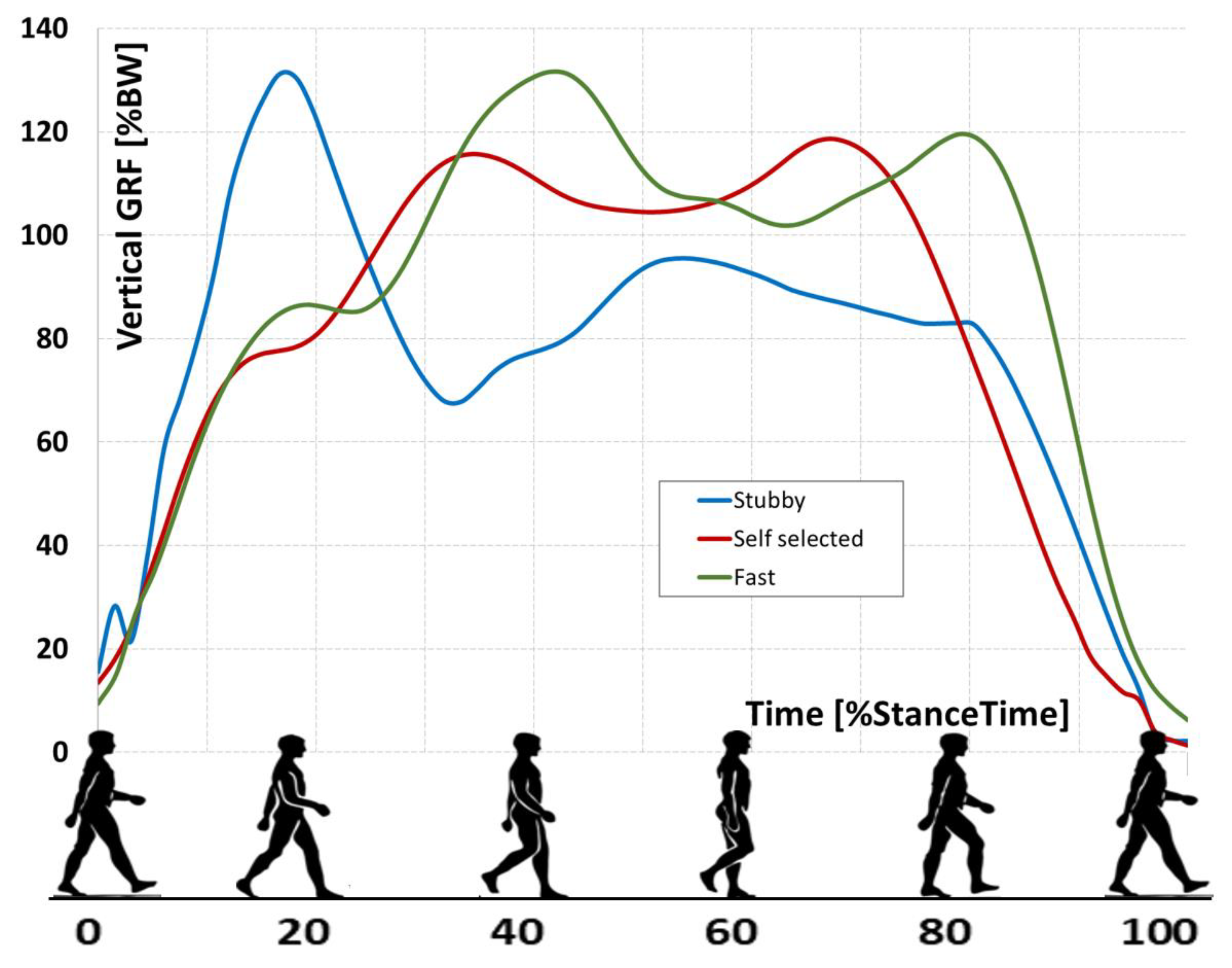
The vGRF (Figure 2) waveforms captured during the gait with standard prostheses were similar in shape to the letter “M”. During the gait with both the self-selected and fast speed, vF1 and vF3 parameters (overweight at the initial weight acceptance phase and overweight during the terminal stance phase) reached higher values than vF2 parameter (underweight during the middle stance phase). During the gait with stubbies prosthesis, despite the time-shift in achievement of the parameter, there was no difference in vGRF values obtained by the vF1 parameter. The vF2 parameter reached the lowest value of approx. 30% for the stance phase (self-selected gait speed—approx. 50%, fast gait speed—70%). The vF3 parameter obtained maximum values much earlier than in other cases (50%, 70% and 80% for the stance phase in the gait cycle, respectively) and took longer stance phases.
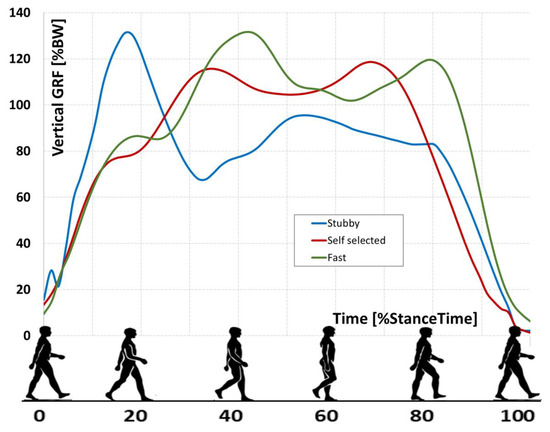
Figure 2.
Vertical ground reaction force (vGRF) in three analyzed gaits.
4. Discussion
The general health status and the state of the stump have an effect on the correctness and efficiency of the gait after a double transfemoral amputation [21]. The properly hardened stump allows for the painless axial load to which it is subjected in the prosthesis funnel. A particularly important element is also the fitting of a prosthesis funnel and full mobility of the hip joint. In many people who have undergone double amputation, flexion-abduction contractures are observed in the hip joint. These contractures can significantly limit the learning of proper gait. A multi-stage rehabilitation process, maintaining normal movement ranges and scar treatment means that the time of actually learning to walk with a prosthesis is sometimes reduced. In addition, the fear of falling and the ability to find oneself in a different situation can prolong the prosthesis fitting process. The first step in improvement is changing position—from a sitting position to a standing one. In many cases, this stage is difficult to achieve due to a fear of falling. Stubby prostheses (stubbies) ensure gradual adaptation to the use of standard prostheses by lowering the center of body mass, which improves coordination and balance. The current limb prosthesis market offers a whole range of products tailored to the patient’s needs. Advances in prosthetics are centered around improved materials and designs that increase the performance of a given prosthesis and improve mobility, and a gait analysis makes it possible to create a product that will successfully reproduce a physiological gait.
The definite advantage of using stubbies is the reduction of the center of body mass. This allows many people who have had a double amputation above the knee joints to be more active. This concerns both home activities as well as outdoor ones. In this case study, the pelvis and trunk were bent while the cadence had to be increased to maintain gait speed. In their research on people have had a double amputation, Carroll et al. also observed a higher cadence than in non-disabled participants (107.7 ± 14.0 step/min for the users of stubby prostheses and 104.4 ± 8.0 step/min for the users of full-length prostheses) [15]. In the studies by Jarvis et al., the cadence in people who have had a double amputation was lower than in both participants who had had a unilateral amputation above the knee joint and in non-disabled people, where it was 96 step/min [14]. However, it should be noted that in this group the reason for the amputation was an improvised explosive device that usually causes additional injury. In cases where people have had an amputation as the result of an explosive device, the fitting of a prosthetic socket is sometimes impossible due to accompanying tissue injuries. In these cases, the DSF becomes an alternative to the traditional prosthetic socket. In the studies of McMenemy et al. and Hoellwarth et al. the DSF suspension method turned out to be safe and the percentage of periprosthetic fractures was between 2 and 3% [17,18]. In our study, the GRF measurement was used to determine the magnitude of force transferred to the thigh stumps. In the above case, the GRF did not reach higher rates than in the other samples. Compared to healthy people, the values achieved by the subject were slightly higher (120% BW for healthy people and 130% BW of stubby prosthesis). It can therefore be assumed that in people who have had DSF in the process of gait rehabilitation, gait training without the use of traditional prostheses does not generate GRF higher than in the case of a stubby prosthesis. Another element discussed in articles concerning the gait after having undergone a double amputation is step width. Weinert-Aplin et al. and Ladlow et al. have shown that the step width affects the energy expenditure of gait. As the stride width increases, the energy expenditure increases [6,11]. Step width was the smallest when walking with stubby prostheses. For this reason, the involvement of muscles bending the hip joint is increased. People who use stubby prostheses should be informed that too long use can result in contractures of muscles bending the hip joint. This is a common complication after amputation above the knee joint. The model in question suggests that a higher metabolic cost of gait in people after amputation resulted from a greater need to maintain balance and posture, and to perform a walking movement. The present study has some potential limitations. First, the research was carried out in the clinical conditions of only one center. Second, conclusions cannot be drawn from one patient case study, especially in the case of biomechanical prothesis where their effects could vary tremendously from person to person depending on body structure and physiology.
5. Conclusions
The authors of the case study found a limited number of similar scientific studies. Due to the high risk of limited walking capacity in people who have had a double amputation, there is a justified need for further research. The use of stubby prostheses can be an alternative to the daily use of standard ones. The results of the biomechanical analysis prove that gait with stubbies is similar to the normal pattern and the one obtained when using standard lower limb prostheses. The reduction of body height reduces the risk of falling.
Author Contributions
A.M.: Conceptualization; M.K.: Metodology, S.W.: Softwere, S.W.: Validation, E.G.: Investigation, I.D.: Resources, data curation, M.K.: Writing, Ż.F.D.: Review, editing; S.W.: Visualization, M.P.-B.: Supervision, A.M.: Project administration; M.P.-B.: Funding. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding. SUB.E060.21.001.
Institutional Review Board Statement
KB-164/2008.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
mateusz.kowal@umed.wroc.pl.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Ladlow, P.; Phillip, R.; Coppack, R.; Etherington, J.; Bilzon, J.; McGuigan, M.P.; Bennett, A.N. Influence of Immediate and Delayed Lower-Limb Amputation Compared with Lower-Limb Salvage on Functional and Mental Health Outcomes Post-Rehabilitation in the UK Military. J. Bone Jt. Surg. Am. Vol. 2016, 98, 1996–2005. [Google Scholar] [CrossRef] [PubMed]
- Hoffman, M.D.; Sheldahl, L.M.; Buley, K.J.; Sandford, P.R. Physiological comparison of walking among bilateral above-knee amputee and able-bodied subjects, and a model to account for the differences in metabolic cost. Arch. Phys. Med. Rehabil. 1997, 78, 385–392. [Google Scholar] [CrossRef]
- Foote, C.E.; Kinnon, J.M.; Robbins, C.; Pessagno, R.; Portner, M.D. Long-term health and quality of life experiences of Vi-etnam veterans with combat-related limb loss. Qual. Life Res. 2015, 24, 2853–2861. [Google Scholar] [CrossRef] [PubMed]
- van Schaik, L.; Geertzen, J.H.B.; Dijkstra, P.U.; Dekker, R. Metabolic costs of activities of daily living in persons with a lower limb amputation: A systematic review and meta-analysis. PLoS ONE 2019, 14, e0213256. [Google Scholar] [CrossRef] [PubMed]
- Stewart, I.J.; Sosnov, J.A.; Howard, J.T.; Orman, J.A.; Fang, R.; Morrow, B.D.; Zonies, D.H.; Bollinger, M.; Tuman, C.; Freedman, B.A.; et al. Retrospective Analysis of Long-Term Outcomes After Combat Injury A Hidden Cost of War. Circulation 2015, 132, 2126–2133. [Google Scholar] [CrossRef]
- Weinert-Aplin, R.; Twiste, M.; Jarvis, H.; Bennett, A.; Baker, R. Medial-lateral centre of mass displacement and base of support are equally good predictors of metabolic cost in amputee walking. Gait Posture 2017, 51, 41–46. [Google Scholar] [CrossRef] [PubMed]
- Lawson, B.E.; Ruhe, B.; Shultz, A.; Goldfarb, M. A Powered Prosthetic Intervention for Bilateral Transfemoral Amputees. IEEE Trans. Biomed. Eng. 2015, 62, 1042–1050. [Google Scholar] [CrossRef] [PubMed]
- Major, M.J.; Stine, R.L.; Gard, S.A. The effects of walking speed and prosthetic ankle adapters on upper extremity dy-namics and stability-related parameters in bilateral transtibial amputee gait. Gait Posture 2013, 38, 858–863. [Google Scholar] [CrossRef]
- Su, P.F.; Gard, S.A.; Lipschutz, R.D.; Kuiken, T.A. Differences in gait characteristics between persons with bilateral tran-stibial amputations, due to peripheral vascular disease and trauma, and able-bodied ambulators. Arch. Phys. Med. Rehabil. 2008, 89, 1386–1394. [Google Scholar] [CrossRef]
- Chereshnev, R.; Kertész-Farkas, A. GaIn: Human Gait Inference for Lower Limbic Prostheses for Patients Suffering from Double Trans-Femoral Amputation. Sensors 2018, 18, 4146. [Google Scholar] [CrossRef] [PubMed]
- Ladlow, P.; Nightingale, T.E.; McGuigan, M.P.; Bennett, A.N.; Phillip, R.D.; Bilzon, J.L.J. Predicting ambulatory energy ex-penditure in lower limb amputees using multi-sensor methods. PLoS ONE 2019, 14, e0209249. [Google Scholar] [CrossRef] [PubMed]
- Kaufman, K.R.; Frittoli, S.; Frigo, C.A. Gait asymmetry of transfemoral amputees using mechanical and microproces-sor-controlled prosthetic knees. Clin. Biomech. 2012, 27, 460–465. [Google Scholar] [CrossRef] [PubMed]
- McNealy, L.L.; Gard, S.A. Effect of prosthetic ankle units on the gait of persons with bilateral trans-femoral amputa-tions. Prosthet. Orthot. Int. 2008, 32, 111–126. [Google Scholar] [CrossRef]
- Jarvis, H.L.; Bennett, A.N.; Twiste, M.; Phillip, R.D.; Etherington, J.; Baker, R. Temporal Spatial and Metabolic Measures of Walking in Highly Functional Individuals With Lower Limb Amputations. Arch. Phys. Med. Rehabil. 2017, 98, 1389–1399. [Google Scholar] [CrossRef] [PubMed]
- Carroll, M.K.; Carroll, K.; Rheinstein, J.; Highsmith, M.J. Functional Differences of Bilateral Transfemo-Ral Amputees Using Full-Length and Stubby-Length Prostheses. Technol. Innov. 2018, 20, 75–83. [Google Scholar] [CrossRef]
- Haque, R.; Al-Jawazneh, S.; Hoellwarth, J.; Akhtar, M.A.; Doshi, K.; Tan, Y.C.; Lu, W.Y.; Roberts, C.; Al Muderis, M. Osseointegrated reconstruction and rehabilitation of transtibial am-putees: The Osseointegration Group of Australia surgical technique and protocol for a prospective cohort study. BMJ Open. 2020, 10, e038346. [Google Scholar] [CrossRef]
- Hoellwarth, J.S.; Tetsworth, K.; Kendrew, J.; Kang, N.V.; van Waes, O.J.F.; Al-Maawi, Q.; Roberts, C.; al Muderis, M. Periprosthetic osseointegration fractures are infrequent and manage-ment is familiar. Bone Jt. J. 2020, 102, 162–169. [Google Scholar] [CrossRef]
- Mcmenemy, L.; Ramasamy, A.; Sherman, K.; Mistlin, A.; Phillip, R.; Evriviades, D.; Kendrew, J. Direct Skeletal Fixation in bilateral above knee amputees following blast: 2 year follow up results from the initial cohort of UK service personnel. Injury 2020, 51, 735–743. [Google Scholar] [CrossRef] [PubMed]
- Wu, G.; Van der Helm, F.C.; Veeger, H.D.; Makhsous, M.; Van Roy, P.; Anglin, C.J.; Karduna, A.R.; McQuade, K.; Wang, X.; Frederick, W.W.; et al. ISB recommendation on definitions of joint coordinate systems of vari-ous joints for the reporting of human joint motion-Part II: Shoulder, elbow, wrist and hand. J. Biomech. 2005, 38, 981–992. [Google Scholar] [CrossRef]
- Pietraszewski, B.; Winiarski, S.; Jaroszczuk, S. Three-dimensional human gait pattern-reference data for normal men. Acta Bioeng. Biomech. 2012, 14, 9–16. [Google Scholar]
- Day, M.C.; Wadey, R.; Strike, S. Living with limb loss: Everyday experiences of “good” and “bad” days in people with lower limb amputation. Disabil. Rehabil. 2019, 41, 2433–2442. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).