A Modified Compact Flexible Vivaldi Antenna Array Design for Microwave Breast Cancer Detection
Abstract
:1. Introduction
2. Materials and Methods
2.1. Antenna 1 Design
2.2. Modified Antenna with One Resonant
2.3. Parametric Study of Modified Antenna
2.3.1. Changing DGS Width, W1
2.3.2. Changing Parasitic Element Width, W2
2.3.3. Changing DGS Length, L1
2.3.4. Changing Parasitic Element Length, L2
2.3.5. Changing DGS Height, h
2.3.6. Changing Parasitic Element Gap, g
2.4. Comparison to Literature
2.5. Antenna Manufacture
2.6. Breast Model
2.7. Imaging Setup
2.8. Image Reconstruction
- Propagation path is estimated from the Euclidian distance between the transmitting antenna, the points of interest, and the receiving antenna;
- Distance traveled through different media along the path is calculated;
- Dielectric properties of the media are estimated based on published dielectric datasets.
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Siegel, R.L.; Miller, K.D.; Fuchs, H.E.; Jemal, A. Cancer statistics. CA Cancer J. Clin. 2022. [Google Scholar] [CrossRef]
- Byrne, D.; Ohalloran, M.; Jones, E.; Glavin, M. A comparison of data-independent microwave beamforming algorithms for the early detection of breast cancer. In Proceedings of the Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Minneapolis, MN, USA, 3–6 September 2009. [Google Scholar] [CrossRef]
- Samsuzzaman, M.; Islam, M.T.; Shovon, A.; Faruque, R.I.; Misran, N. A 16-modified antipodal Vivaldi Antenna Array for microwave-based breast tumor imaging applications. Microw. Opt. Technol. Lett. 2019, 61, 2110–2118. [Google Scholar] [CrossRef]
- Munawar, A.; Adabi, S.; Ismail, A.; Saripan, M.; Mahmood, R.; Mahadi, W.; Abdullah, R. Breast cancer detection using Forward Scattering Radar technique. In Proceedings of the IEEE International RF and Microwave Conference, Kuala Lumpur, Malaysia, 2–4 December 2008. [Google Scholar] [CrossRef]
- Li, Q.; Xiao, X.; Wang, L.; Song, H.; Kono, H.; Liu, P.; Lu, H.; Kikkawa, T. Direct Extraction of Tumor Response Based on Ensemble Empirical Mode Decomposition for Image Reconstruction of Early Breast Cancer Detection by UWB. IEEE Trans. Biomed. Circuits Syst. 2015, 9, 710–724. [Google Scholar] [CrossRef] [PubMed]
- Woten, A.; Lusth, J.; El-Shenawee, M. Interpreting Artificial Neural Networks for Microwave Detection of Breast Cancer. IEEE Microw. Wirel. Compon. Lett. 2007, 17, 825–827. [Google Scholar] [CrossRef]
- Bahrami, H.; Porter, E.; Santorelli, A.; Gosselin, B.; Popovic, M.; Rusch, L.A. Flexible sixteen monopole antenna array for microwave breast cancer detection. In Proceedings of the 36th Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Chicago, IL, USA, 26–30 August 2014. [Google Scholar] [CrossRef]
- Lazebnik, M.; Popovic, D.; McCartney, L.; Watkins, C.B.; Lindstrom, M.J.; Harter, J.; Sewall, S.; Ogilvie, T.; Magliocco, A.; Breslin, T.M.; et al. A large-scale study of the ultrawideband microwave dielectric properties of normal, benign and malignant breast tissues obtained from cancer surgeries. Phys. Med. Biol. 2007, 52, 6093. [Google Scholar] [CrossRef]
- Martellosio, A.; Bellomi, M.; Pasian, M.; Bozzi, M.; Perregrini, L.; Mazzanti, A.; Svelto, F.; Summers, P.E.; Renne, G.; Preda, L. Dielectric properties characterization from 0.5 to 50 GHz of breast cancer tissues. IEEE Trans. Microw. Theory Tech. 2017, 65, 998–1011. [Google Scholar] [CrossRef]
- Di Meo, S.; Espin-Lopez, P.F.; Martellosio, A.; Pasian, M.; Bozzi, M.; Perregrini, L.; Mazzanti, A.; Svelto, F.; Summers, P.E.; Renne, G.; et al. Dielectric properties of breast tissues: Experimental results up to 50 GHz. In Proceedings of the 12th European Conference on Antennas and Propagation, London, UK, 9–13 April 2018. [Google Scholar] [CrossRef]
- Misilmani, H.M.; Naous, T.; Khatib, S.K.; Kabalan, K.Y. A survey on antenna designs for breast cancer detection using microwave imaging. IEEE Access 2020, 8, 102570–102594. [Google Scholar] [CrossRef]
- Woten, D.A.; El-Shenawee, M. Broadband Dual Linear Polarized Antenna for Statistical Detection of Breast Cancer. IEEE Trans. Antennas Propag. 2008, 56, 3576–3580. [Google Scholar] [CrossRef]
- Sugitani, T.; Kubota, S.; Toya, A.; Xiao, X.; Kikkawa, T. A Compact 4 × 4 Planar UWB Antenna Array for 3-D Breast Cancer Detection. IEEE Antennas Wirel. Propag. Lett. 2013, 12, 733–736. [Google Scholar] [CrossRef]
- Ouerghi, K.; Fadlallah, N.; Smida, A.; Ghayoula, R.; Fattahi, J.; Boulejfen, N. Circular antenna array design for breast cancer detection. In Proceedings of the Sensors Networks Smart and Emerging Technologies (SENSET), Beiriut, Lebanon, 12–14 September 2017. [Google Scholar] [CrossRef] [Green Version]
- Alibakhshikenari, M.; Virdee, B.S.; Shukla, P.; Parchin, N.O.; Azpilicueta, L.; See, C.H.; Abd-Alhameed, R.A.; Falcone, F.; Huynen, I.; Denidni, T.A.; et al. Metamaterial-inspired antenna array for application in microwave breast imaging systems for tumor detection. IEEE Access 2020, 8, 174667–174678. [Google Scholar] [CrossRef]
- Jalilvand, M.; Li, X.; Zwirello, L.; Zwick, T. Ultra wideband compact near-field imaging system for breast cancer detection. IET Microw. Antennas Propag. 2015, 9, 1009–1014. [Google Scholar] [CrossRef]
- Craddock, I.J.; Klemm, M.; Leendertz, J.; Preece, A.W.; Benjamin, R. An improved hemispherical antenna array design for breast imaging. In Proceedings of the 2nd European Conference on Antennas and Propagation, Edinburgh, UK, 11–16 November 2007. [Google Scholar] [CrossRef]
- Mahmud, M.; Islam, M.; Misran, N.; Almutairi, A.; Cho, M. Ultra-Wideband (UWB) Antenna Sensor Based Microwave Breast Imaging: A Review. Sensors 2018, 18, 2951. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mobashsher, A.T.; Abbosh, A.M. Performance of Directional and Omnidirectional Antennas in Wideband Head Imaging. IEEE Antennas Wirel. Propag. Lett. 2016, 15, 1618–1621. [Google Scholar] [CrossRef]
- Hailu, D.M.; Safavi-Naeini, S. Narrow focus ultra-wideband antenna for breast cancer detection. In Proceedings of the IEEE Radio and Wireless Symposium, San Diego, CA, USA, 18–22 January 2009. [Google Scholar] [CrossRef]
- Faisal, M.A.; Uddin, M.J.; Ullah, M.W.; Kamrul, M.I.; Haque, K.M.; Rahman, E. Comparative analysis of different types of breast cancer cell detection antennas. In Proceedings of the 2017 International Conference on Inventive Computing and Informatics (ICICI), Coimbatore, India, 23–24 November 2017. [Google Scholar] [CrossRef]
- Sugitani, T.; Kubota, S.; Toya, A.; Kikkawa, T. Compact planar UWB antenna array for breast cancer detection. In Proceedings of the 2012 IEEE International Symposium on Antennas and Propagation, Chicago, IL, USA, 8–14 July 2012. [Google Scholar] [CrossRef]
- Hasan, K.; Hadidy, M.E.; Morsi, H. Reflectarray antenna for breast cancer detection and biomedical applications. In Proceedings of the IEEE Middle East Conference on Antennas and Propagation (MECAP), Beirut, Lebanon, 20–22 September 2016. [Google Scholar] [CrossRef]
- Iliopoulos, I.; Meo, S.D.; Pasian, M.; Zhadobov, M.; Pouliguen, P.; Potier, P.; Perregrini, L.; Sauleau, R.; Ettorre, M. Enhancement of penetration of millimeter waves by field focusing applied to breast cancer detection. IEEE Trans. Biomed. Eng. 2021, 68, 959–966. [Google Scholar] [CrossRef]
- Ley, S.; Sachs, J.; Faenger, B.; Hilger, I.; Helbig, M. MNP-enhanced microwave medical imaging by means of Pseudo-Noise Sensing. Sensors 2021, 21, 6613. [Google Scholar] [CrossRef]
- Botterill, T.; Lotz, T.; Kashif, A.; Chase, G. Reconstructing 3-D Skin Surface Motion for the DIET Breast Cancer Screening System. IEEE Trans. Med. Imaging 2014, 33, 1109–1118. [Google Scholar] [CrossRef]
- Li, X.; Hagness, S.C. A confocal microwave imaging algorithm for Breast Cancer Detection. IEEE Microw. Wirel. Compon. Lett. 2001, 11, 130–132. [Google Scholar] [CrossRef] [Green Version]
- Bond, E.J.; Li, X.; Hagness, S.C.; Van Veen, B.D. Microwave Imaging via space-time beamforming for early detection of breast cancer. In Proceedings of the IEEE International Conference on Acoustics Speech and Signal Processing, Orlando, FL, USA, 13–17 May 2002. [Google Scholar] [CrossRef]
- Klemm, M.; Craddock, I.J.; Leendertz, J.A.; Preece, A.; Benjamin, R. Improved delay-and-sum beamforming algorithm for Breast Cancer Detection. Int. J. Antennas Propag. 2008, 2008, 761402. [Google Scholar] [CrossRef] [Green Version]
- Özmen, H.; Kurt, M.B. Radar-based Microwave Breast Cancer Detection System with a high-performance ultrawide band Antipodal Vivaldi Antenna. Turk. J. Electr. Eng. Comput. Sci. 2021, 29, 2326–2345. [Google Scholar] [CrossRef]
- Guruswamy, S.; Chinniah, R.; Thangavelu, K. Design and implementation of compact ultra-wideband Vivaldi antenna with directors for microwave-based imaging of breast cancer. Analog. Integr. Circuits Signal Processing 2021, 108, 45–57. [Google Scholar] [CrossRef]
- Danjuma, I.M.; Noras, J.M.; Abd-Alhameed, R.A.; Obeidat, H.A.; Oguntala, G.A.; Eya, N.N.; Mohammad, B.A. Microwave imaging using arrays of Vivaldi antenna for breast cancer applications. Int. J. Microw. Appl. 2018, 7, 32–37. [Google Scholar] [CrossRef]
- Islam, M.T.; Mahmud, M.Z.; Islam, M.T.; Kibria, S.; Samsuzzaman, M. A low cost and portable microwave imaging system for breast tumor detection using UWB directional antenna array. Sci. Rep. 2019, 9, 15491. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- O’Loughlin, D.; Elahi, M.A.; Porter, E.; Shahzad, A.; Oliveira, B.L.; Glavin, M.; Jones, E.; O’Halloran, M. Open-source software for microwave radar-based Image Reconstruction. In Proceedings of the 12th European Conference on Antennas and Propagation, London, UK, 9–13 April 2018. [Google Scholar] [CrossRef]
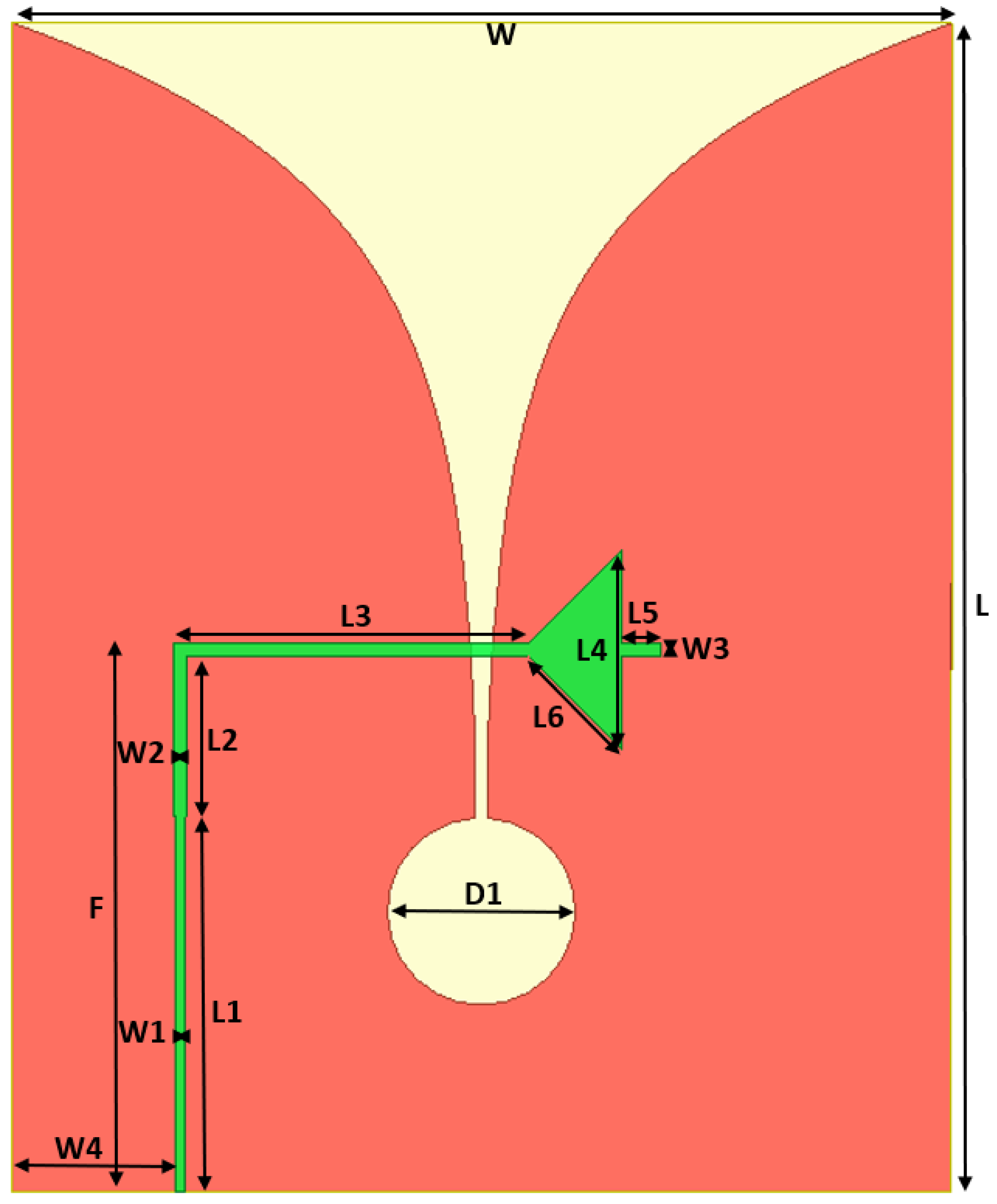























| Parameter | Value (mm) | Parameter | Value (mm) |
|---|---|---|---|
| L | 25 | W | 20 |
| L1 | 8 | L2 | 3.45 |
| L3 | 7.54 | L4 | 4.27 |
| L5 | 0.8 | L6 | 2.83 |
| W1 | 0.21 | W2 | 0.28 |
| W3 | 0.27 | D1 | 4 |
| W4 | 3.5 | F | 11.45 |
| Parameter | Value (mm) | Parameter | Value (mm) |
|---|---|---|---|
| L1 | 2.8 | L2 | 7 |
| W1 | 0.2 | W2 | 0.15 |
| h | 15.2 | g | 0.2 |
| Citation | Type | Radiation | Size mm3 | Band (GHz) | Fc (GHz) | BW (GHz) | Gain (dBi) |
|---|---|---|---|---|---|---|---|
| [3] | Vivaldi | Directional | 40 × 40 × 1.6 | 2.5–11 | NA | 8.5 | 7.2 |
| [7] | Flexible Monopole | Omni-directional | 20 × 20 × 0.05 | 2–4 | 3 | 2 | NA |
| [30] | Vivaldi | Directional | 36 × 36 × 1.6 | 3–12 | 7.2 | 9 | 8.2 |
| [31] | Vivaldi | Directional | 48 × 46 × 0.8 | 3.1–10.6 | 7.8 | 7.5 | 8.25 |
| [32] | Vivaldi | Directional | 57 × 41 × 1.6 | 3–9 | 3.8 | 6 | NA |
| [33] | Vivaldi | Directional | 51 × 42 × 0.05 | 2.8–7 | 5 | 4.2 | 7.5 |
| Proposed 1 With two resonant | Vivaldi | Directional | 25 × 20 × 0.1 | 3.8–4.8 and 9–10 | 4.0 and 9.5 | 1.0 and1.0 | 2.24 and 2.7 |
| Proposed 2 With one resonant | Vivaldi | Directional | 25 × 20 × 0.1 | 4.0–5.2 | 4.4 | 1.2 | 2.33 |
| Frequency Range (GHz) | Minimum Reflected-Signal Magnitude without Tumor (dB) | Minimum Reflected-Signal Magnitude with Tumor (dB) | Variation in Magnitude (dB) | Presence of Tumor |
|---|---|---|---|---|
| 3.65–3.8 | −7.5 | −5.6 | −1.9 | Weak Noticeable |
| 3.8–3.95 | −10.6 | −7.7 | −2.9 | Weak Noticeable |
| 3.95–4.11 | −16.1 | −11.9 | −4.2 | Noticeable |
| 4.1–4.25 | −30.3 | −21.8 | −8.5 | Strong Noticeable |
| 4.25–4.4 | −34.0 | −18.6 | −15.5 | Strong Noticeable |
| 4.4–4.6 | −28.0 | −16.4 | −11.6 | Strong Noticeable |
| 4.6–4.7 | −21.5 | −14.3 | −7.2 | Strong Noticeable |
| 4.7–4.9 | −16.4 | −11.7 | −4.7 | Noticeable |
| 4.9–5 | −14.0 | −10.6 | −3.4 | Noticeable |
| 5–5.2 | −16.5 | −13.0 | −3.5 | Weak Noticeable |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Qashlan, A.M.; Aldhaheri, R.W.; Alharbi, K.H. A Modified Compact Flexible Vivaldi Antenna Array Design for Microwave Breast Cancer Detection. Appl. Sci. 2022, 12, 4908. https://doi.org/10.3390/app12104908
Qashlan AM, Aldhaheri RW, Alharbi KH. A Modified Compact Flexible Vivaldi Antenna Array Design for Microwave Breast Cancer Detection. Applied Sciences. 2022; 12(10):4908. https://doi.org/10.3390/app12104908
Chicago/Turabian StyleQashlan, Ayman M., Rabah W. Aldhaheri, and Khalid H. Alharbi. 2022. "A Modified Compact Flexible Vivaldi Antenna Array Design for Microwave Breast Cancer Detection" Applied Sciences 12, no. 10: 4908. https://doi.org/10.3390/app12104908
APA StyleQashlan, A. M., Aldhaheri, R. W., & Alharbi, K. H. (2022). A Modified Compact Flexible Vivaldi Antenna Array Design for Microwave Breast Cancer Detection. Applied Sciences, 12(10), 4908. https://doi.org/10.3390/app12104908






