Adjustable Stiffness-Based Supination–Pronation Forearm Physical Rehabilitator
Abstract
:1. Introduction
- Phase 1. Immediate motion (Passive)
- Phase 2. Intermediate (Active-assisted)
- Phase 3. Advanced strengthening (Active)
2. Methodology
- Medical requirements identification: The characterization of the required motion is established by performing a literature review and by consulting physiotherapists. Range of motion, torques, and physical dimensions are some of the requirements that must be defined.
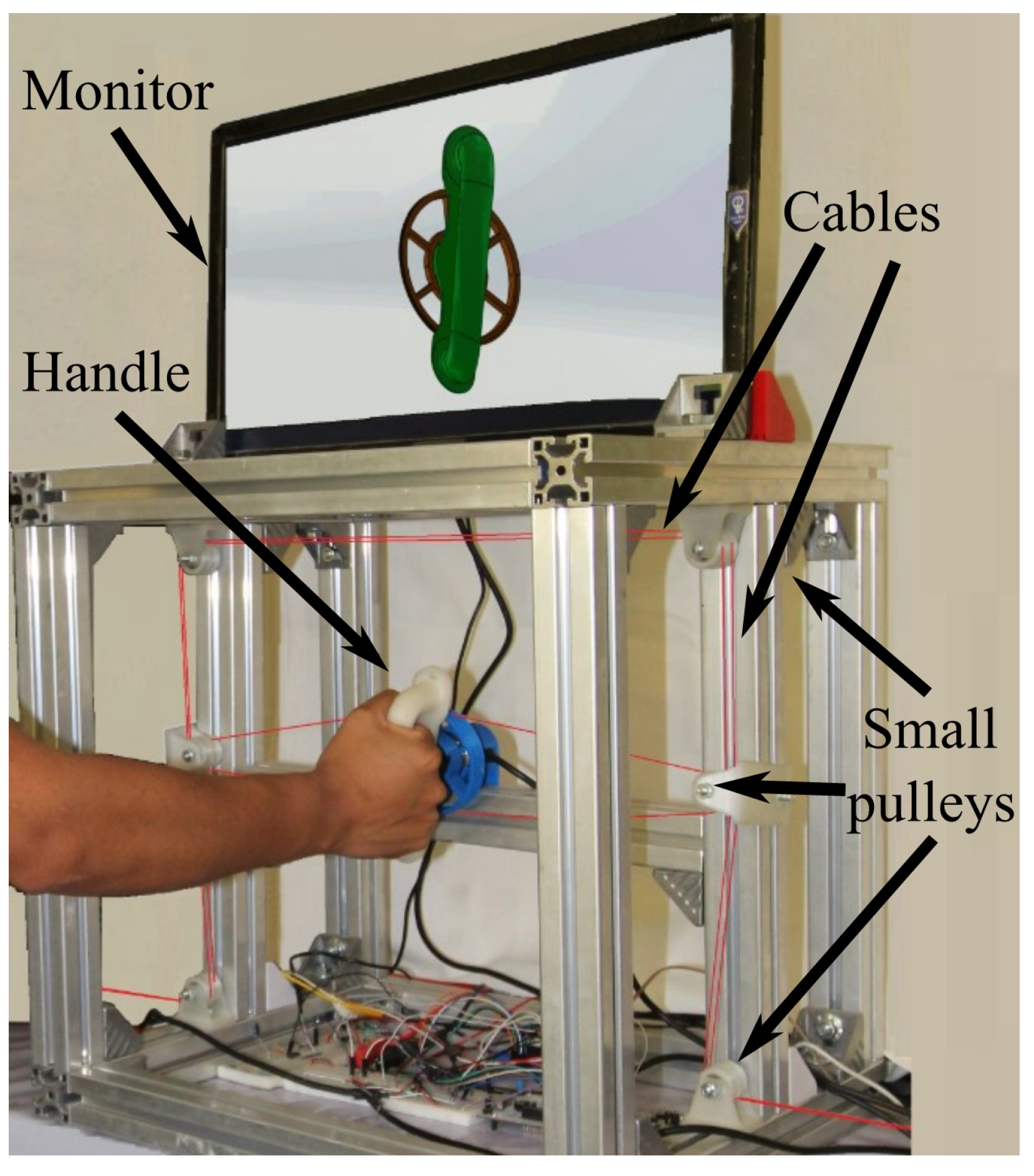
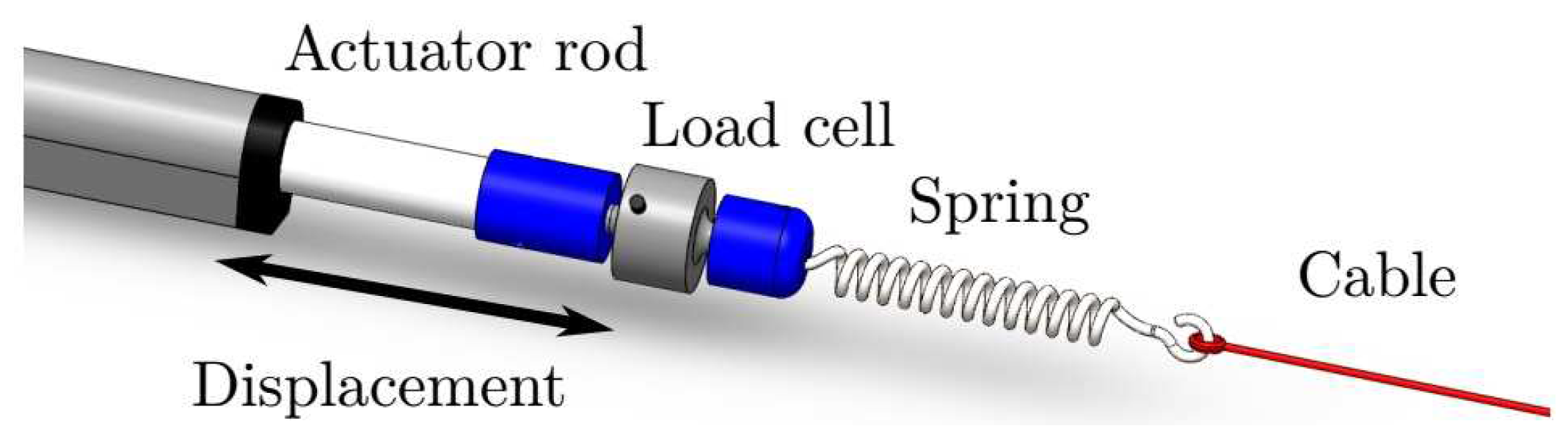
- Mechanical design conceptualization: In this iterative phase, several concepts of the rehabilitator are generated in order to be evaluated based on medical requirements. Different mechanical elements and materials are considered, as well as manufacturing processes. The best option is selected to be developed. Figure 2 and Figure 3 show a schematic representation of some elements of the rehabilitator.
- Dynamic mathematical model synthesis: A dynamic mathematical representation of the selected option is synthesized, taking into account mechanical interactions defined by physical laws and behaviors of the respective materials. The dynamic mathematical model (DMM) can be obtained in the time domain. If the mathematical model is linear, a frequency domain representation can be obtained too. The DMM representing the adjustable stiffness rehabilitator is provided in Equation (2) in the time domain.
- Open loop numerical simulations: In order to analyze the behavior of the mathematical model under specific excitation signals, numerical simulations are performed. If needed, adjustments can be made to the mathematical model.
- Closed-loop control strategy synthesis: starting from a precise mathematical model of the rehabilitator, the synthesis of a closed-loop control strategy is generated by taking into account the angular position trajectory tracking (supination–pronation) and the cable’s tension regulation (resistance to be overcome). This is, in general, an iterative step. Section 5 shows the proposed closed-loop control strategy.
- Closed-loop numerical simulations: Several numerical simulations are performed in order to analyze the closed-loop behavior of the mathematical model (the rehabilitator) based on the established requirements. It is in this phase where the controllers are tuned. This step represents a first validation that allows one to initiate the manufacturing process.
- Experimental platform manufacturing: Based on the materials, on the mechanical elements, and on the manufacturing processes considered in the selected proposal, an experimental platform is built (see Figure 2). This platform will allow one to, experimentally, validate the mechanical design, the dynamic mathematical model, and the control strategy.
- Experimental platform instrumentation: Actuators, sensors, and other elements are incorporated to the experimental platform that will interact with an embedded system.
- Embedded system generation: Generally speaking, in this step a microcontroller is selected, programmed and connected to the manufactured and instrumented platform. At this point, the electronic interface (see Section 4) is ready for performing experiments.
- Experimental tests: Before using new medical technology in patients for clinical trials or treatment, it is necessary to validate, experimentally, its performance. The angular trajectory tracking and the stiffness (tension or torque) regulation are the two main aspects of interest to validate the performance of the rehabilitator reported in this paper (see Section 6).
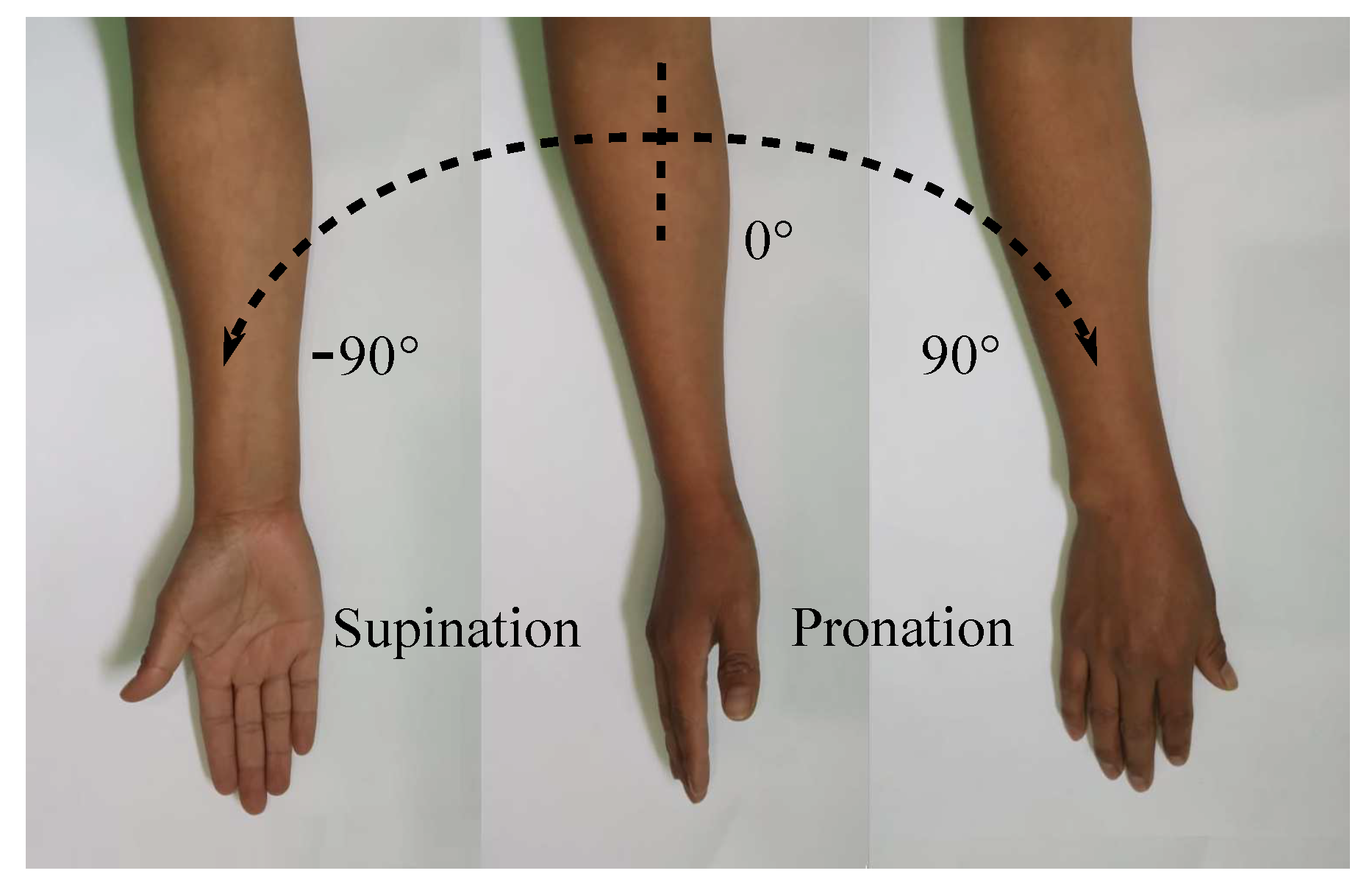
3. Adjustable Stiffness Rehabilitation Device
- •
- Grasp the patient’s wrist, supporting the hand with the handle, and stabilize the elbow and the forearm whether sitting or standing;
- •
- Supination and pronation should be performed with a 90° elbow/forearm flexion or with a 90° shoulder/arm flexion;
- •
- Supinate or pronate the forearm until a slight pain arises with previously established trajectories;
- •
- Apply resistance through stiffness control actions as the patient evolves in his/her rehabilitation.
- Passive: A trajectory, previously established by a therapist as a function of the patient’s medical condition, is tracked at different angular speeds by the adjustable stiffness rehabilitator. In this therapy phase, the patient will not make any effort to perform the movement because the actuators will be in charge.
- Active-Assisted: The therapist defines a desired trajectory, and the patient is asked to move his/her wrist–forearm from the neutral position () toward a desired one. If the patient is not able to perform the desired movement, the rehabilitation device completes the task.
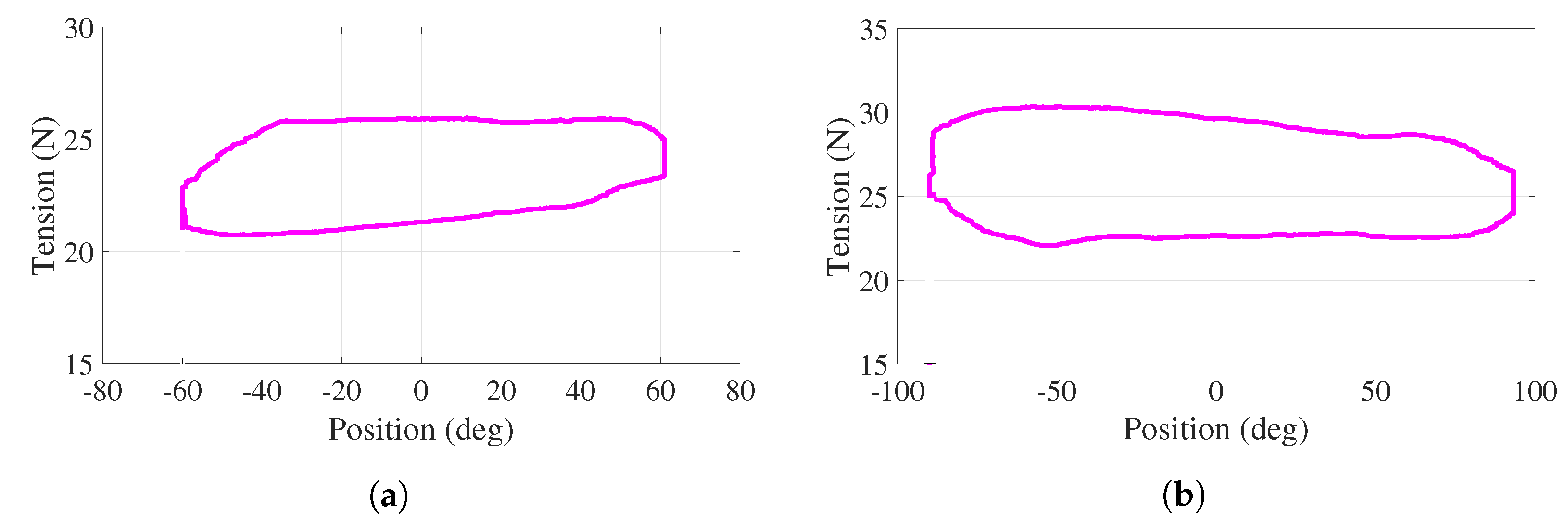
- Active: In this resisted phase, the desired trajectory and the tension values are previously established by the therapist. The rehabilitation device measures angular positions and tensions in the cables and provides the required forces to successfully complete the exercises. The control delivers a part of the required tension through springs deformations.
- The springs are assumed to be linear elements working under tension at all times.
- Vibration and elongation in the cables are neglected.
- The linear actuators are mounted outside the system workspace. The standing or seated position of the patient requires that the actuators are not mounted under or above the forearm to prevent injuries.
- Safety must always be guaranteed for both the patient and the therapist by considering the following: to avoid sharp edges in the mechanical structure (aluminum and polylactic acid (PLA) parts). Several components of the experimental platform are manufactured by 3D-printing using PLA material. The design respects the anatomical ROM of human upper limbs. The chances of a severe accident are low because the maximum speed is limited by the properties of the linear actuators and by electronic-computational restrictions.
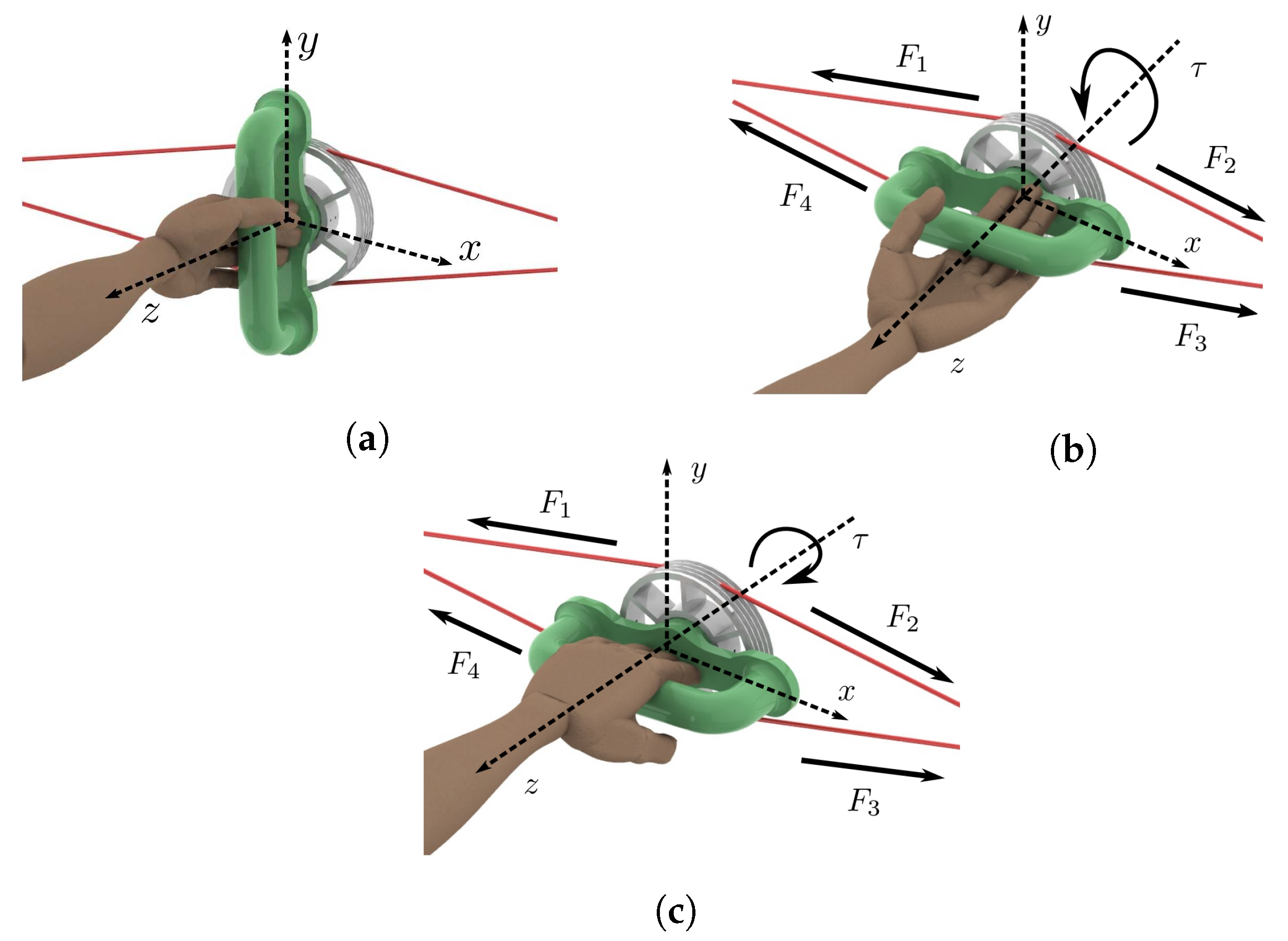
- The motion of the rehabilitation system is generated as follows (see Figure 4). Each linear actuator transmits a linear displacement to one end of the respective spring. Once the spring is deformed, the displacement is transmitted to the associated rigid cables. Each spring provides the possibility to modify the tensions in the cables according to a particular rehabilitation phase since smooth motions could be required depending on the patient’s medical condition. Moreover, tensions adjustments are required when performing assisted-active and active rehabilitation phases.
- The cables (copolymer monofilament) are used to connect the springs with the handle through a series of pulleys that modify the direction of each force in order to guarantee a constraint-free operation of the system.
- The system requires to meet and exceed the torque and the ROM requirements while recreating ADL movements (see Table 2).
4. Electronic Interface
- The master board NUCLEO-F767ZI [45] is in charge to manage the control loop process at 1 kHz sample rate and the signal processing. It contains a low/high-level (general purpose input/output and trajectory/tension controllers) control strategy.
- Two linear actuators (TGA-Y-300-24-5-405) of 24 VDC and 900 N of maximum load are implemented. Additionally, it includes an internal micro switch to make the actuator’s stem stop automatically after it ends. Its displacement corresponds to 300 mm. Moreover, an external encoder (LPD3806-400BM-G5-24C) of 400 pulses per revolution (ppr) has been adapted to each actuator. Based on a quadrature method, the number of ppr has been incremented to 1600 in such a manner that the respective resolution equals 37,600 pulses per each displaced millimeter.
- To move the actuators, an L298N dual H-bridge DC motor driver module has been implemented. The speed and direction of each actuator is controlled by means of applying 12 bits pulse width modulation (PWM).
- Two load cells (JLBM-1-100) of 100 N, with mv/V of sensitivity, were implemented to convert the mechanical force of the cables-springs into analogue values to measure/calculate the system stiffness by means of two 12-bit ADC.
- In order to measure the angular position of the handle and to close the feedback trajectory loop, another incremental encoder with 1600 ppr was implemented.
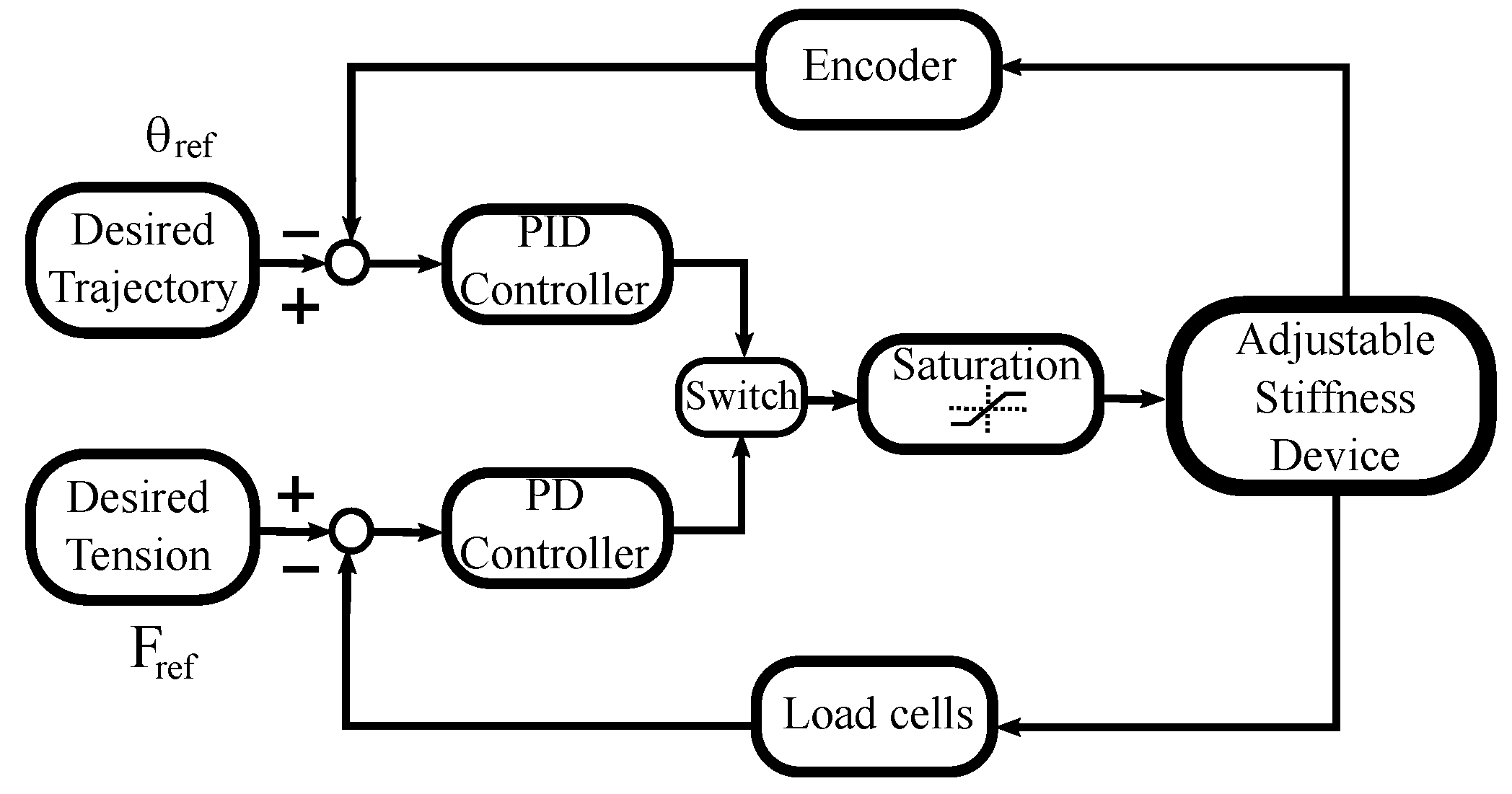
5. Control Strategy
- A proportional-integral-derivative (PID) controller in charge of ensuring trajectory tracking. The trajectories of interest are of the sinusoidal type , where represents the desired behavior of the handle angular position in degrees, A is the amplitude of the angular displacement in degrees, is the angular frequency in radians per second, and t is the time in seconds.Remark 2.Parameters A and ω can be adjusted according to a therapist recommendation based on the patient’s medical condition.
- A proportional-derivative (PD) controller focused on a regulation task. While the handle of the rehabilitation device changes its angular position, it is necessary to guarantee a desirable value of the tension force in the cables to ensure that the two springs always work with a minimum of elongation. It is highlighted that a desired tension value depends on the rehabilitation phase and on the patient’s medical condition.
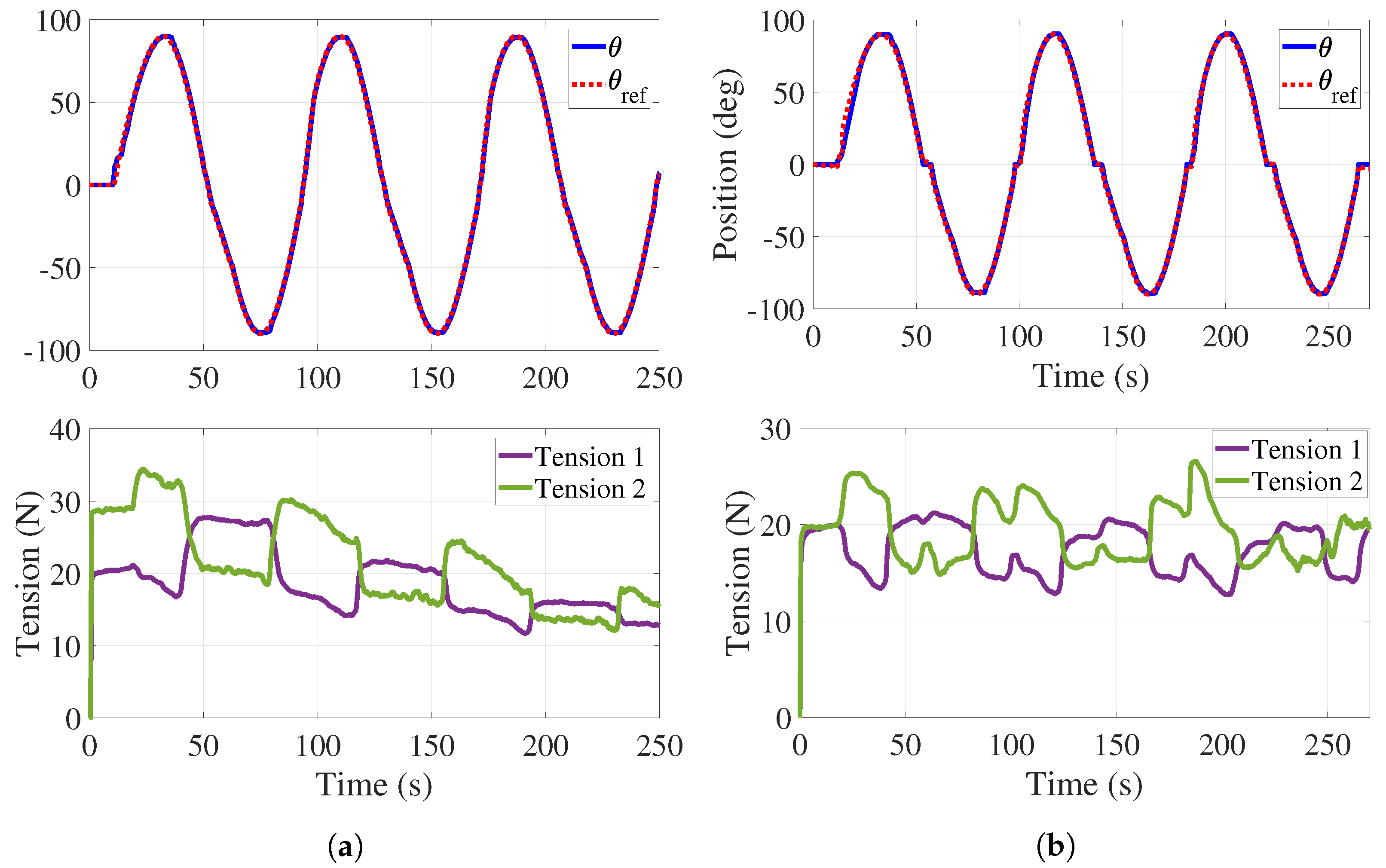
6. Experimental Results
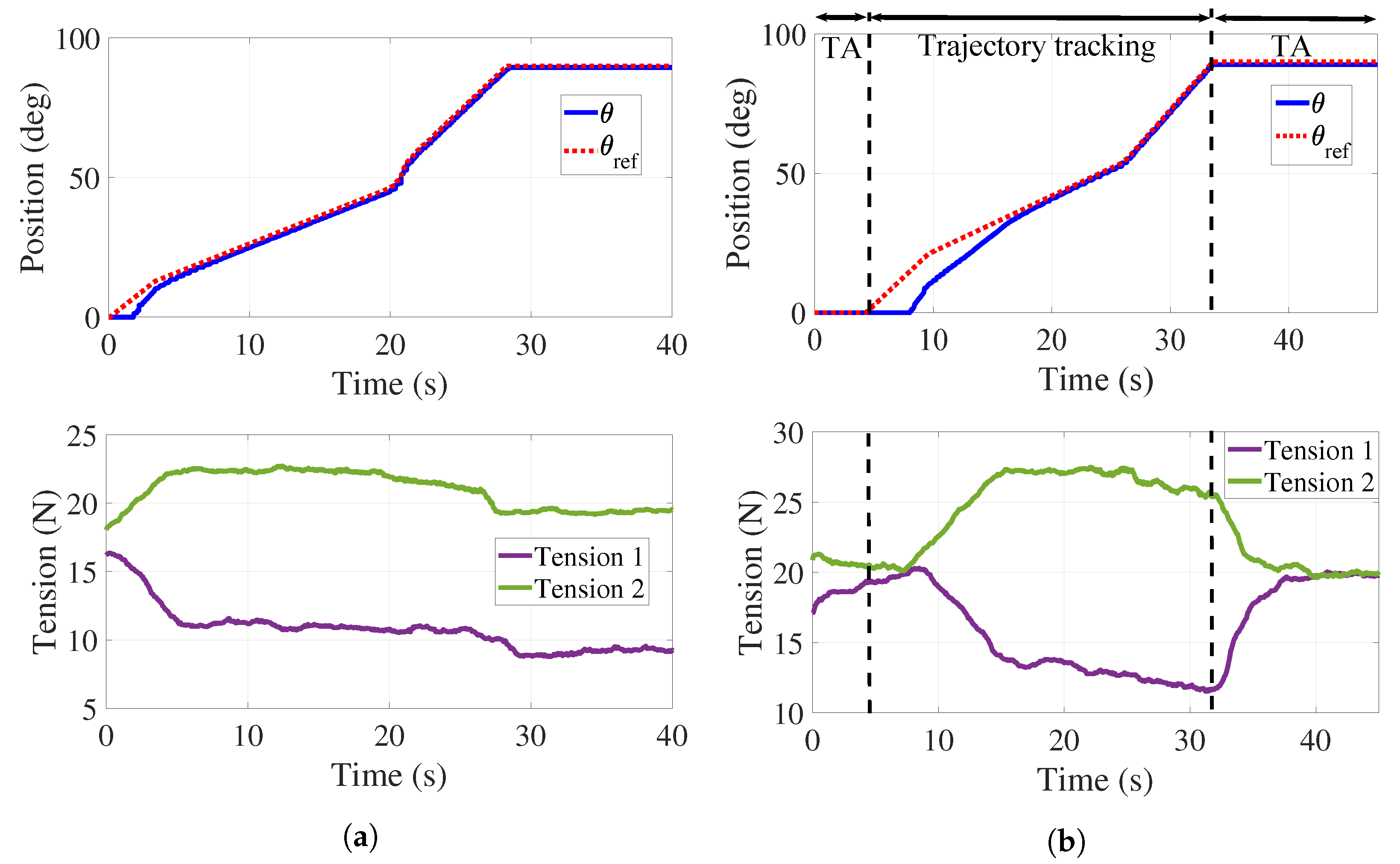
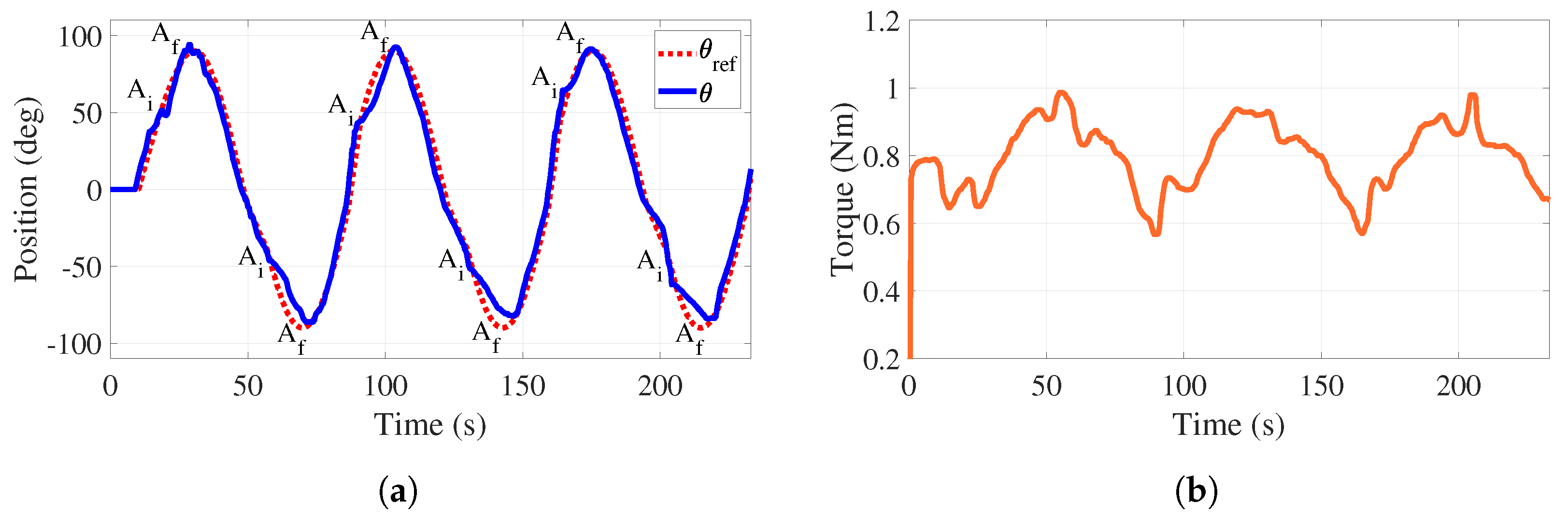
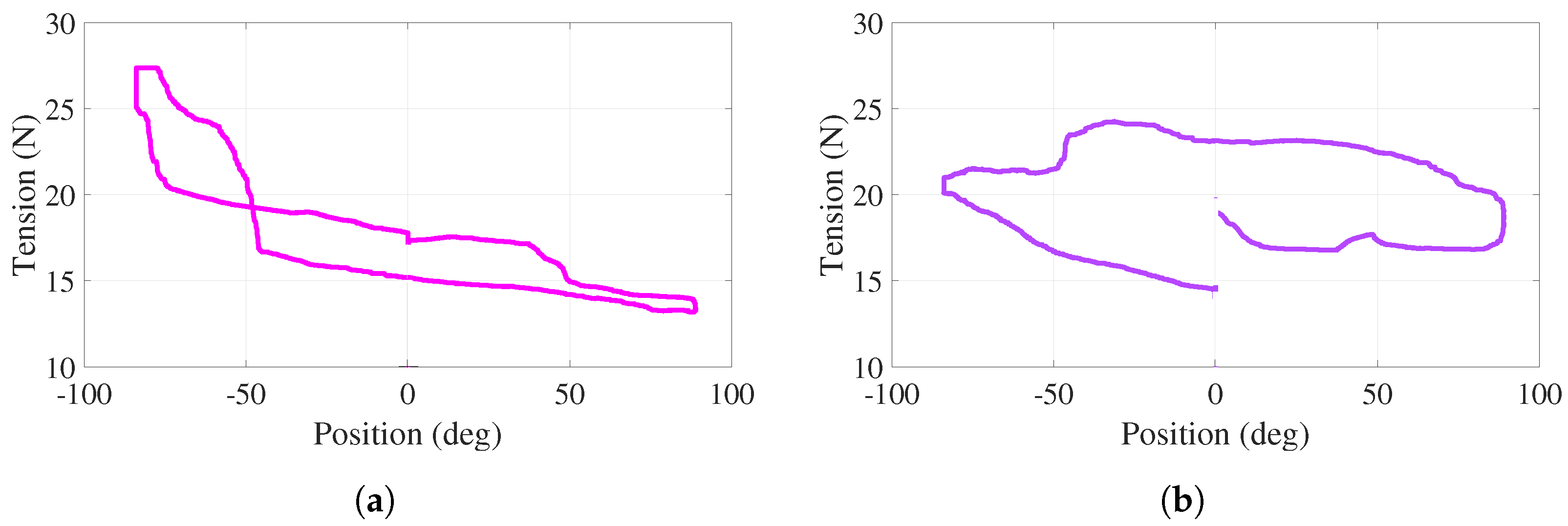
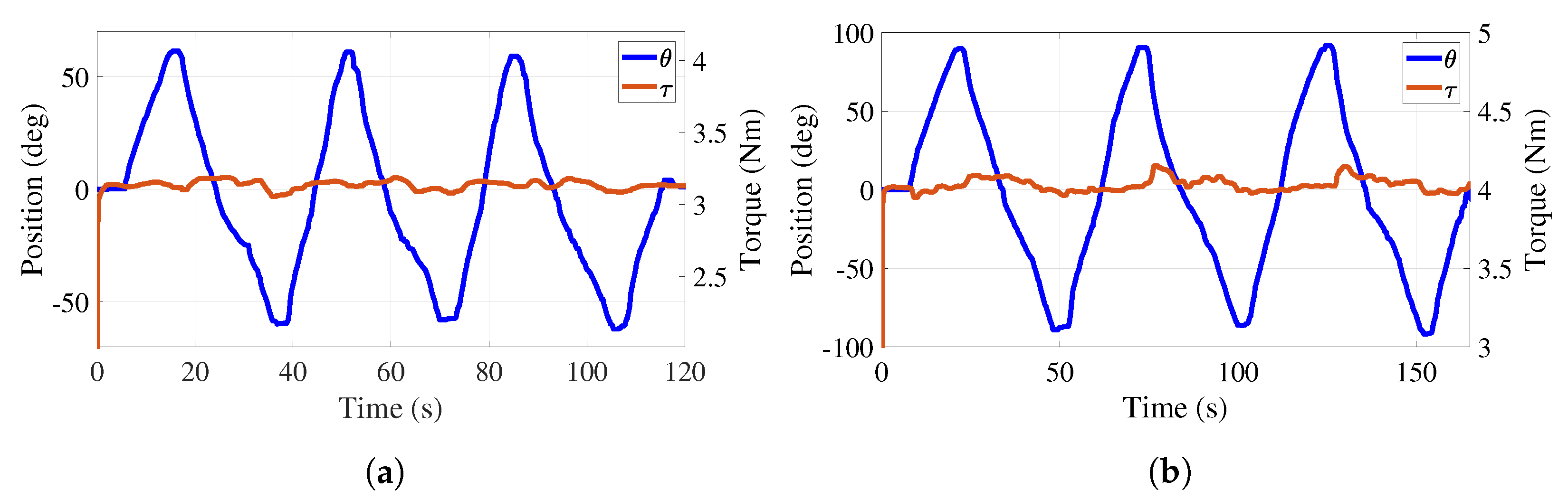
- The handle angular motion with respect to a desired trajectory ;
- The tensions in the cables looking to keep a desired value;
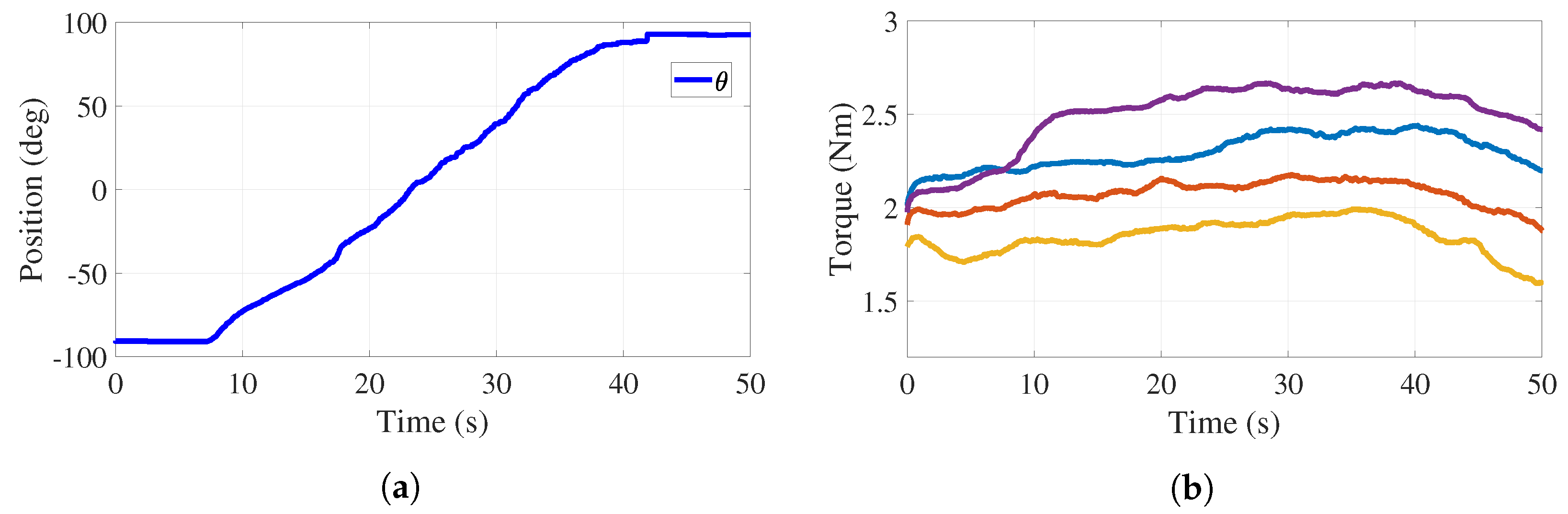
- The total torque applied to the handle pulley that should be adjusted based on a desired value.
6.1. Passive
6.2. Active-Assisted
6.3. Active
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- INEGI. Estadísticas a Propósito del día Internacional de las Personas con Discapacidad. 2019. Available online: https://www.inegi.org.mx/contenidos/saladeprensa/aproposito/2019/Discapacidad2019_Nal.pdf (accessed on 29 December 2021).
- Nusselder, W.J.; Looman, C.C.; Van Oyen, H.; Yokota, R.T.D.C. Attributing causes to disability. In International Handbook of Health Expectancies; Springer: Berlin/Heidelberg, Germany, 2020; Volume 9, pp. 87–105. [Google Scholar] [CrossRef]
- ATrain Education. Regaining Use of the Upper Extremity. 2022. Available online: https://www.atrainceu.com/content/13-regaining-use-upper-extremity (accessed on 18 May 2022).
- Kennedy Krieger Institute. Neurodevelopmental Treatment in Physical Therapy. 2022. Available online: https://www.kennedykrieger.org/patient-care/centers-and-programs/physical-therapy-clinic/neurodevelopmental-treatment (accessed on 17 May 2022).
- Canadian Partnership for Stroke Recovery. Upper Extremity Motor Rehabilitation Interventions. 2018. Available online: http://www.ebrsr.com/sites/default/files/ch%2010_v19.pdf (accessed on 17 May 2022).
- Narayan, J.; Kalita, B.; Dwivedy, S.K. Development of robot-based upper limb devices for rehabilitation purposes: A systematic review. Augment. Hum. Res. 2021, 6, 4. [Google Scholar] [CrossRef]
- World Health Organization. World Report on Disability; World Health Organization: Geneva, Switzerland, 2011. [Google Scholar]
- Masiero, S.; Poli, P.; Rosati, G.; Zanotto, D.; Iosa, M.; Paolucci, S.; Morone, G. The value of robotic systems in stroke rehabilitation. Expert Rev. Med. Devices 2014, 11, 187–198. [Google Scholar] [CrossRef] [PubMed]
- Nef, T.; Klamroth-Marganska, V.; Keller, U.; Riener, R. Three-dimensional multi-degree-of-freedom arm therapy robot (ARMin). In Neurorehabilitation Technology; Springer: Berlin/Heidelberg, Germany, 2016; pp. 351–374. [Google Scholar] [CrossRef]
- Sale, P.; Lombardi, V.; Franceschini, M. Hand robotics rehabilitation: Feasibility and preliminary results of a robotic treatment in patients with hemiparesis. Stroke Res. Treat. 2012, 2012, 820931. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lo, A.C. Clinical designs of recent robot rehabilitation trials. Am. J. Phys. Med. Rehabil. 2012, 91, S204–S216. [Google Scholar] [CrossRef] [PubMed]
- Sale, P.; Franceschini, M.; Mazzoleni, S.; Palma, E.; Agosti, M.; Posteraro, F. Effects of upper limb robot-assisted therapy on motor recovery in subacute stroke patients. J. Neuroeng. Rehabil. 2014, 11, 104. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hatem, S.M.; Saussez, G.; della Faille, M.; Prist, V.; Zhang, X.; Dispa, D.; Bleyenheuft, Y. Rehabilitation of motor function after stroke: A multiple systematic review focused on techniques to stimulate upper extremity recovery. Front. Hum. Neurosci. 2016, 10, 442. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bertani, R.; Melegari, C.; Maria, C.; Bramanti, A.; Bramanti, P.; Calabrò, R.S. Effects of robot-assisted upper limb rehabilitation in stroke patients: A systematic review with meta-analysis. Neurol. Sci. 2017, 38, 1561–1569. [Google Scholar] [CrossRef] [PubMed]
- Padilla-Castañeda, M.A.; Sotgiu, E.; Barsotti, M.; Frisoli, A.; Orsini, P.; Martiradonna, A.; Laddaga, C.; Bergamasco, M. An orthopaedic robotic-assisted rehabilitation method of the forearm in virtual reality physiotherapy. J. Healthc. Eng. 2018, 2018, 7438609. [Google Scholar] [CrossRef] [PubMed]
- Jamwal, P.K.; Hussain, S.; Ghayesh, M.H.; Rogozina, S.V. Impedance control of an intrinsically compliant parallel ankle rehabilitation robot. IEEE Trans. Ind. Electron. 2016, 63, 3638–3647. [Google Scholar] [CrossRef]
- Duret, C.; Grosmaire, A.G.; Krebs, H.I. Robot-assisted therapy in upper extremity hemiparesis: Overview of an evidence-based approach. Front. Neurol. 2019, 10, 412. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- UN. Transforming Our World: The 2030 Agenda for Sustainable Development. 2015. Available online: https://www.un.org/ga/search/viewdoc.asp?symbol=A/RES/70/1&Lang=E (accessed on 5 December 2021).
- Verl, A.; Albu-Schäffer, A.; Brock, O.; Raatz, A. Soft Robotics; Springer: Berlin/Heidelberg, Germany, 2015. [Google Scholar] [CrossRef]
- Wolf, S.; Grioli, G.; Eiberger, O.; Friedl, W.; Grebenstein, M.; Höppner, H.; Burdet, E.; Caldwell, D.G.; Carloni, R.; Catalano, M.G.; et al. Variable stiffness actuators: Review on design and components. IEEE/ASME Trans. Mechatronics 2015, 21, 2418–2430. [Google Scholar] [CrossRef]
- Motro, R. Tensegrity: Structural Systems for the Future; Elsevier: Amsterdam, The Netherlands, 2003. [Google Scholar] [CrossRef]
- Jung, E.; Ly, V.; Cessna, N.; Ngo, M.L.; Castro, D.; SunSpiral, V.; Teodorescu, M. Bio-inspired tensegrity flexural joints. In Proceedings of the 2018 IEEE International Conference on Robotics and Automation (ICRA), Brisbane, Australia, 21–25 May 2018; IEEE: Piscataway, NJ, USA, 2018; pp. 5561–5566. [Google Scholar] [CrossRef]
- Lessard, S.; Pansodtee, P.; Robbins, A.; Trombadore, J.M.; Kurniawan, S.; Teodorescu, M. A soft exosuit for flexible upper-extremity rehabilitation. IEEE Trans. Neural Syst. Rehabil. Eng. 2018, 26, 1604–1617. [Google Scholar] [CrossRef] [PubMed]
- Gosselin, C.; Cardou, P.; Bruckmann, T.; Pott, A. Cable-Driven Parallel Robots: Proceedings of the Third International Conference on Cable-Driven Parallel Robots; Springer: Berlin/Heidelberg, Germany, 2017; Volume 53. [Google Scholar] [CrossRef]
- Alamdari, A.; Krovi, V. Design and analysis of a cable-driven articulated rehabilitation system for gait training. J. Mech. Robot. 2016, 8, 051018. [Google Scholar] [CrossRef] [Green Version]
- Boehler, Q.; Abdelaziz, S.; Vedrines, M.; Poignet, P.; Renaud, P. From modeling to control of a variable stiffness device based on a cable-driven tensegrity mechanism. Mech. Mach. Theory 2017, 107, 1–12. [Google Scholar] [CrossRef] [Green Version]
- Manna, S.K.; Dubey, V.N. A Portable Elbow Exoskeleton for Three Stages of Rehabilitation. J. Mech. Robot. 2019, 11, 065002. [Google Scholar] [CrossRef] [Green Version]
- Medical Dictionary. Available online: http://medical-dictionary.thefreedictionary.com/ (accessed on 29 May 2019).
- Krebs, H.I.; Hogan, N.; Aisen, M.L.; Volpe, B.T. Robot-aided neurorehabilitation. IEEE Trans. Rehabil. Eng. 1998, 6, 75–87. [Google Scholar] [CrossRef] [Green Version]
- Charles, S.K.; Krebs, H.I.; Volpe, B.T.; Lynch, D.; Hogan, N. Wrist rehabilitation following stroke: Initial clinical results. In Proceedings of the 9th International Conference on Rehabilitation Robotics, 2005. ICORR 2005, Chicago, IL, USA, 28 June–1 July 2005; IEEE: Piscataway, NJ, USA, 2005; pp. 13–16. [Google Scholar] [CrossRef]
- Pehlivan, A.U.; Celik, O.; O’Malley, M.K. Mechanical design of a distal arm exoskeleton for stroke and spinal cord injury rehabilitation. In Proceedings of the 2011 IEEE International Conference on Rehabilitation Robotics, Zurich, Switzerland, 29 June–1 July 2011; IEEE: Piscataway, NJ, USA, 2011; pp. 1–5. [Google Scholar] [CrossRef]
- Allington, J.; Spencer, S.J.; Klein, J.; Buell, M.; Reinkensmeyer, D.J.; Bobrow, J. Supinator Extender (SUE): A pneumatically actuated robot for forearm/wrist rehabilitation after stroke. In Proceedings of the 2011 Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Boston, MA, USA, 30 August–3 September 2011; IEEE: Piscataway, NJ, USA, 2011; pp. 1579–1582. [Google Scholar] [CrossRef]
- Martinez, J.A.; Ng, P.; Lu, S.; Campagna, M.S.; Celik, O. Design of wrist gimbal: A forearm and wrist exoskeleton for stroke rehabilitation. In Proceedings of the 2013 IEEE 13th International Conference on Rehabilitation Robotics (ICORR), Seattle, WA, USA, 24–26 June 2013; IEEE: Piscataway, NJ, USA, 2013; pp. 1–6. [Google Scholar] [CrossRef]
- Pehlivan, A.U.; Sergi, F.; Erwin, A.; Yozbatiran, N.; Francisco, G.E.; O’Malley, M.K. Design and validation of the RiceWrist-S exoskeleton for robotic rehabilitation after incomplete spinal cord injury. Robotica 2014, 32, 1415–1431. [Google Scholar] [CrossRef] [Green Version]
- Song, Z.; Guo, S.; Pang, M.; Zhang, S.; Xiao, N.; Gao, B.; Shi, L. Implementation of resistance training using an upper-limb exoskeleton rehabilitation device for elbow joint. J. Med. Biol. Eng. 2014, 34, 188–196. [Google Scholar] [CrossRef]
- Pezent, E.; Rose, C.G.; Deshpande, A.D.; O’Malley, M.K. Design and characterization of the openwrist: A robotic wrist exoskeleton for coordinated hand-wrist rehabilitation. In Proceedings of the 2017 International Conference on Rehabilitation Robotics (ICORR), London, UK, 17–20 July 2017; IEEE: Piscataway, NJ, USA, 2017; pp. 720–725. [Google Scholar] [CrossRef] [Green Version]
- Andrews, J.R.; Harrelson, G.L.; Wilk, K.E. Physical Rehabilitation of the Injured Athlete: Expert Consult-Online and Print; Elsevier Health Sciences: Amsterdam, The Netherlands, 2012. [Google Scholar] [CrossRef] [Green Version]
- Kisner, C.; Colby, L.A.; Borstad, J. Therapeutic Exercise: Foundations and Techniques; Fa Davis: Philadelphia, PA, USA, 2017. [Google Scholar]
- Wilk, K.E.; Ellenbecker, T.S.; Macrina, L.C. Rehabilitation of the overhead athlete’s elbow. In Elbow Ulnar Collateral Ligament Injury; Springer: Berlin/Heidelberg, Germany, 2021; pp. 327–356. [Google Scholar] [CrossRef]
- Giangarra, C.E.; Manske, R.C. Clinical Orthopaedic Rehabilitation: A Team Approach E-book; Elsevier Health Sciences: Amsterdam, The Netherlands, 2017. [Google Scholar]
- Avila-Chaurand, R.; Prado-León, L.; González-Muñoz, E. Dimensiones Antropométricas de la Población Latinoamericana: México, Cuba, Colombia, Chile / R. Avila Chaurand, L.R. Prado León, E.L. González Muñoz.; Universidad de Guadalajara: Guadalajara, Mexico, 2007. [Google Scholar]
- Tsagarakis, N.; Caldwell, D.; Medrano-Cerda, G. A 7 DOF pneumatic muscle actuator (pMA) powered exoskeleton. In Proceedings of the 8th IEEE International Workshop on Robot and Human Interaction. RO-MAN’99 (Cat. No. 99TH8483), Pisa, Italy, 27–29 September 1999; IEEE: Piscataway, NJ, USA, 1999; pp. 327–333. [Google Scholar] [CrossRef]
- Jacinto-Villegas, J.M.; Portillo-Rodríguez, O.; Martinez-Mendez, R.; Daza-Merino, C.; Vilchis-González, A.H.; Avila-Vilchis, J.C. Sistema para control de posición basado en Rapid Control Prototyping (RCP) usando Simulink y SWB32. Komput. Sapiens 2019, 3, 11–15. [Google Scholar]
- Martínez, C.C.; Ávila-Vilchis, J.C.; Jacinto-Villegas, J.M.; Saldivar, B.; Vilchis-González, A.H. Sliding Mode Control for the Regulation Problem of an Aerodynamic Angular System: Experimental Platform and Validation. Int. J. Control. Autom. Syst. 2021, 19, 2395–2405. [Google Scholar] [CrossRef]
- STMicroelectronics. NUCLEO-F767ZI. 2020. Available online: https://www.st.com/en/evaluation-tools/nucleo-f767zi.html (accessed on 18 January 2021).

| Supination–Pronation | |||
|---|---|---|---|
| Device | Torque (Nm) | ROM | Characteristics |
| MIT MANUS 1998 [29], 2005 [30] | 1.85 | 180° | Active and passive device configured to assist arm joints movement and hand grasping training through a graphic module that provides a series of video games that the patient must complete. |
| MAHI Exo II 2011 [31] | 2.30 | 180° | Performs wrist bend, adduction, extension, and arm stretching. It has a mechanism to achieve forearm rotation and elbow bend and stretching. |
| SUE 2011 [32] | 2.71 | 180° | A lightweight and compact wrist and forearm rehabilitator with pneumatic actuators and force compensation control. |
| Wrist Gimbal 2013 [33] | 2.87 | 180° | Practical device for clinical implementation with two bearings that provide mechanical robustness and easy to use for the supination–pronation ROM. |
| RiceWrist-S 2014 [34] | 1.69 | 180° | Facilitates rehabilitation of the forearm in supination–pronation, wrist in flexion-extension, and radial-ulnar deviation. It is shown to provide grip force measurements. |
| ULERD 2014 [35] | 9.00 | 85°/75° | Uses a graphical interface for passive and resistance training. Springs are used to estimate, through their deformations, the interaction force between the human limb and the robotic device. |
| Open Wrist 2017 [36] | 3.50 | 180° | Favorable performance with closed-loop movements with ergonomic features but with an increased inertia and static friction in supination–pronation ROM. |
| Supination–Pronation | Torque (Nm) | ROM |
|---|---|---|
| ADL | 0.06 | 150°–180° |
| Human isometric strength | 9.10 | 150°–180° |
| Parameter | Value | Units |
|---|---|---|
| deg/s | ||
| deg/s | ||
| 9772.10 | deg/m·s |
| Gain | PID | PD |
|---|---|---|
| 99.18 | 58.34 | |
| 0.29 | - | |
| 89.26 | 20.42 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Camacho-Ramirez, A.; Ávila-Vilchis, J.C.; Saldivar, B.; Vilchis-González, A.H.; Jacinto-Villegas, J.M. Adjustable Stiffness-Based Supination–Pronation Forearm Physical Rehabilitator. Appl. Sci. 2022, 12, 6164. https://doi.org/10.3390/app12126164
Camacho-Ramirez A, Ávila-Vilchis JC, Saldivar B, Vilchis-González AH, Jacinto-Villegas JM. Adjustable Stiffness-Based Supination–Pronation Forearm Physical Rehabilitator. Applied Sciences. 2022; 12(12):6164. https://doi.org/10.3390/app12126164
Chicago/Turabian StyleCamacho-Ramirez, Adrian, Juan Carlos Ávila-Vilchis, Belem Saldivar, Adriana H. Vilchis-González, and Juan Manuel Jacinto-Villegas. 2022. "Adjustable Stiffness-Based Supination–Pronation Forearm Physical Rehabilitator" Applied Sciences 12, no. 12: 6164. https://doi.org/10.3390/app12126164






