Novel Dual-Threaded Pedicle Screws Provide Fixation Stability That Is Comparable to That of Traditional Screws with Relative Bone Preservation: An In Vitro Biomechanical Study
Abstract
:1. Introduction
2. Materials and Methods
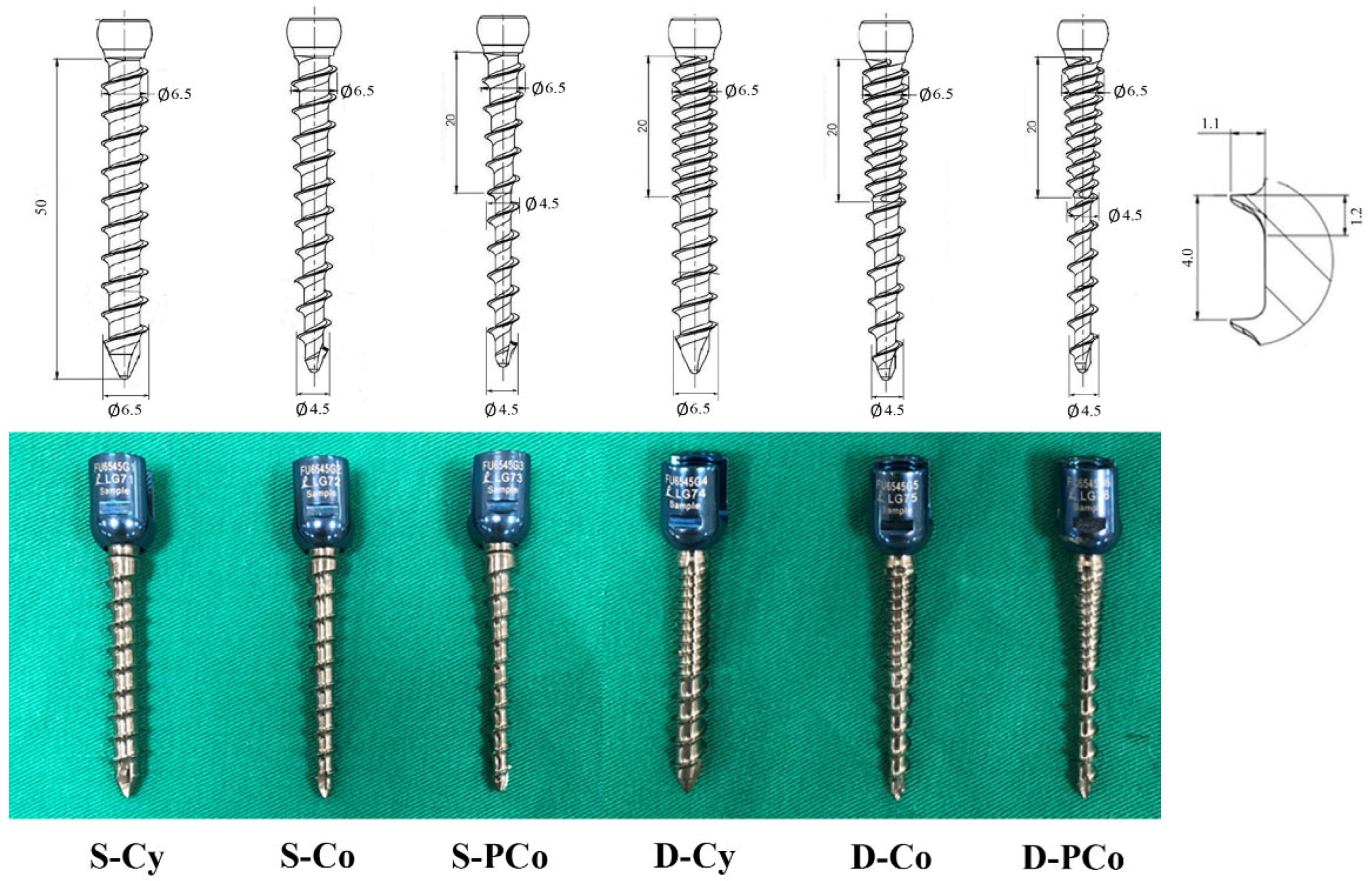
2.1. Pedicle Screw Design
2.2. Specimen Preparation and Screw Insertion
2.3. Image Analysis
2.4. Biomechanical Testing
2.5. Screw Volume in Bone (SV)
2.5.1. Thread Volume of Screws
- Thread volume in cylindrical screw =whereA denotes cross-section area of the thread and equals 1.2 × 1.1 × 0.5.C denotes circumference of screw and equals .N denotes thread number, and the thread number in the single-thread screw is 10 and that in the dual-thread screw is 15.
- Thread volume in conical screw =whereA denotes cross-section area of the thread and equals 1.2 × 1.1 × 0.5denotes mean circumference of screw and equalsN denotes thread number, and the thread number in the single-thread screw is 10 and that in the dual-thread screw is 15.
- Thread volume in proximal-conical screw = + (AwhereA denotes cross-section area of the thread and equals 1.2 × 1.1 × 0.5denotes the mean circumference of the proximal-conical region and equalsNp denotes thread number at proximal-conical region, and the thread number in a single-thread screw is 5 and that in the dual-thread screw is 10.Cd denotes the circumference of the distal-cylindrical region and equalsNd denotes thread number at distal-cylindrical region and the thread number is 5 in both single-thread and dual-thread screws.
2.5.2. Inner Core Volume of Screws
- Inner core volume in S-Cy/D-Cy groups =whereR denotes the radius of the screw core and equalsL denotes the length of the screw and equals 50
- Inner core volume in S-Co/D-Co groups =whereR denotes the radius of the screw core at the hub and equalsr denotes the radius of the screw core at the tip and equalsL denotes the length of the screw and equals 50
- Inner core volume in S-PCo/D-PCo groups =whereR denotes the radius of the screw core at the hub and equalsr denotes the radius of the screw core at the tip and equals
2.6. Statistical Analysis
3. Results
3.1. Biomechanical Performance
3.2. Screw Volume in Bone (SV)
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kao, F.C.; Hsieh, M.K.; Yu, C.W.; Tsai, T.T.; Lai, P.L.; Niu, C.C.; Chen, L.H.; Chen, W.J. Additional vertebral augmentation with posterior instrumentation for unstable thoracolumbar burst fractures. Injury 2017, 48, 1806–1812. [Google Scholar] [CrossRef] [PubMed]
- Chang, C.W.; Fu, T.S.; Lin, D.Y.; Lai, P.L.; Chiu, P.Y.; Kao, F.C.; Tsai, T.T.; Hsieh, M.K. Percutaneous Balloon Kyphoplasty and Short Instrumentation Compared with Traditional Long Instrumentation for Thoracolumbar Metastatic Spinal Cord Compression. World Neurosurg. 2019, 130, e640–e647. [Google Scholar] [CrossRef] [PubMed]
- Hsieh, M.K.; Bowles, D.R.; Canseco, J.A.; Sherman, M.B.; Schroeder, G.D.; Vaccaro, A.R. Is open surgery for metastatic spinal cord compression secondary to lung cancer really beneficial? A systematic review. World Neurosurg. 2020, 144, e253–e263. [Google Scholar] [CrossRef] [PubMed]
- Liao, J.C.; Chen, W.P.; Wang, H. Treatment of thoracolumbar burst fractures by short-segment pedicle screw fixation using a combination of two additional pedicle screws and vertebroplasty at the level of the fracture: A finite element analysis. BMC Musculoskelet. Disord. 2017, 18, 262. [Google Scholar] [CrossRef] [Green Version]
- Su, K.C.; Chen, K.H.; Pan, C.C.; Lee, C.H. Biomechanical evaluation of cortical bone trajectoryfixation with traditional pedicle screw in the lumbar spine: A finite element study. Appl. Sci. 2021, 11, 10583. [Google Scholar] [CrossRef]
- Hsieh, M.K.; Chen, L.H.; Niu, C.C.; Fu, T.S.; Lai, P.L.; Chen, W.J. Combined anterior lumbar interbody fusion and instrumented posterolateral fusion for degenerative lumbar scoliosis: Indication and surgical outcomes. BMC Surg. 2015, 15, 26. [Google Scholar] [CrossRef] [Green Version]
- Tsuang, F.Y.; Chen, C.H.; Wu, L.C.; Kuo, Y.J.; Hsieh, Y.Y.; Chiang, C.J. Partial threading of pedicle screws in a standard construct increases fatigue life: A biomechanical analysis. Appl. Sci. 2021, 11, 1503. [Google Scholar] [CrossRef]
- Chan, A.; Parent, E.; Narvacan, K.; San, C.; Lou, E. Intraoperative image guidance compared with free-hand methods in adolescent idiopathic scoliosis posterior spinal surgery: A systematic review on screw-related complications and breach rates. Spine J. 2017, 17, 1215–1229. [Google Scholar] [CrossRef]
- Galbusera, F.; Volkheimer, D.; Reitmaier, S.; Berger-Roscher, N.; Kienle, A.; Wilke, H.J. Pedicle screw loosening: A clinically relevant complication? Eur. Spine J. 2015, 24, 1005–1016. [Google Scholar] [CrossRef]
- Hsieh, M.K.; Li, Y.D.; Li, Y.C.; Liu, M.Y.; Tsai, T.T.; Lai, P.L.; Tai, C.L. Improved fixation stability for repairing pedicle screw loosening using a modified cement filling technique in porcine vertebrae. Sci. Rep. 2022, 12, 2739. [Google Scholar] [CrossRef]
- Xu, F.; Zhou, S.; Zou, D.; Li, W.; Sun, Z.; Jiang, S. The relationship between S1 screw loosening and postoperative outcome in patients with degenerative lumbar scoliosis. BMC Musculoskelet. Disord. 2022, 23, 186. [Google Scholar] [CrossRef] [PubMed]
- Weegens, R.; Carreon, L.Y.; Voor, M.; Gum, J.L.; Laratta, J.L.; Glassman, S.D. Dual pitch screw design provides equivalent fixation to upsized screw diameter in revision pedicle screw instrumentation: A cadaveric biomechanical study. Spine J. 2022, 22, 168–173. [Google Scholar] [CrossRef] [PubMed]
- Hsieh, M.K.; Liu, M.Y.; Chen, J.K.; Tsai, T.T.; Lai, P.L.; Niu, C.C.; Tai, C.L. Use of longer sized screws is a salvage method for broken pedicles in osteoporotic vertebrae. Sci. Rep. 2020, 10, 10441. [Google Scholar] [CrossRef] [PubMed]
- Liu, D.; Shi, L.; Lei, W.; Wei, M.Q.; Qu, B.; Deng, S.L.; Pan, X.M. Biomechanical comparison of expansive pedicle screw and polymethylmethacrylate-augmented pedicle screw in osteoporotic synthetic bone in primary implantation: An experimental study. Clin. Spine Surg. 2016, 29, E351–E357. [Google Scholar] [CrossRef] [PubMed]
- Hsieh, M.K.; Liu, M.Y.; Chen, J.K.; Tsai, T.T.; Lai, P.L.; Niu, C.C.; Tai, C.L. Biomechanical study of the fixation stability of broken pedicle screws and subsequent strategies. PLoS ONE 2019, 14, e0219189. [Google Scholar] [CrossRef]
- Weiser, L.; Sehmisch, S.; Viezens, L.; Lehmann, W. Intraoperative revision of initially loosened pedicle screws. Oper. Orthop. Traumatol. 2019, 31, 293–300. [Google Scholar] [CrossRef] [Green Version]
- Isik, C.; Kose, K.C.; Inanmaz, M.E.; Tagil, S.M.; Sarman, H. The Mechanisms of Medial Pedicle Wall Violation: Insertion Method Is as Important as Correct Cannulation of the Pedicle. Adv. Orthop. 2014, 2014, 283783. [Google Scholar] [CrossRef] [Green Version]
- Goda, Y.; Higashino, K.; Toki, S.; Suzuki, D.; Kobayashi, T.; Matsuura, T.; Fujimiya, M.; Hutton, W.C.; Fukui, Y.; Sairyo, K. The pullout strength of pedicle screws following redirection after lateral wall breach or end-plate breach. Spine 2016, 41, 1218–1223. [Google Scholar] [CrossRef] [Green Version]
- Irie, T.Y.; Irie, T.; Espinoza Orías, A.A.; Segami, K.; Iwasaki, N.; An, H.S.; Inoue, N. Micro-computed tomography analysis of the lumbar pedicle wall. PLoS ONE 2021, 16, 2021. [Google Scholar] [CrossRef]
- Maeda, T.; Higashino, K.; Manabe, H.; Yamashita, K.; Hayashi, F.; Goda, Y.; Tsuruo, Y.; Sairyo, K. Pullout strength of pedicle screws following redirection after lateral or medial wall breach. Spine 2018, 43, E983–E989. [Google Scholar] [CrossRef]
- Takenaka, S.; Kaito, T.; Ishii, K.; Watanable, K.; Shinohara, A.; Harada, T.; Nakada, F.; Majima, Y.; Matsumoto, M. Influence of novel design alteration of pedicle screw on pull-out strength: A finite element study. J. Orthop. Sci. 2020, 25, 66–72. [Google Scholar] [CrossRef] [PubMed]
- Mehta, H.; Santos, E.; Ledonio, C.; Sembrano, J.; Ellingson, A.; Pare, P.; Murrell, B.; Nuckley, D.J. Biomechanical analysis of pedicle screw thread differential design in an osteoporotic cadaver model. Clin. Biomech. 2012, 27, 234–240. [Google Scholar] [CrossRef] [PubMed]
- Brasiliense, L.B.C.; Lazaro, B.C.R.; Reyes, P.M.; Reyes, P.M.; Newcomb, A.G.U.S.; Turner, J.L.; Crandall, D.G.; Crawford, N.R. Characteristics of immediate and fatigue strength of a dual-threaded pedicle screw in cadaveric spines. Spine J. 2013, 13, 947–956. [Google Scholar] [CrossRef]
- Liu, M.Y.; Tsai, T.T.; Lai, P.L.; Hsieh, M.K.; Chen, L.H.; Tai, C.L. Biomechanical comparison of pedicle screw fixation strength in synthetic bones: Effects of screw shape, core/thread profile and cement augmentation. PLoS ONE 2020, 15, e0229328. [Google Scholar] [CrossRef] [PubMed]
- Weiser, L.; Sellenschloh, K.; Püsche, L.K.; Morlock, M.M.; Viezens, L.; Lehmann, W.; Huber, G. Cortical threaded pedicle screw improves fatigue strength in decreased bone quality. Eur. Spine J. 2021, 30, 128–135. [Google Scholar] [CrossRef] [PubMed]
- Bokov, A.; Bulkin, A.; Aleynik, A.; Kutlaeva, M.; Mlyavykh, S. Pedicle Screws Loosening in Patients With Degenerative Diseases of the Lumbar Spine: Potential Risk Factors and Relative Contribution. Glob. Spine J. 2019, 9, 55. [Google Scholar] [CrossRef] [Green Version]
- Tai, C.L.; Tsai, T.T.; Lai, P.L.; Chen, Y.L.; Liu, M.Y.; Chen, L.H. A Biomechanical Comparison of Expansive Pedicle Screws for Severe Osteoporosis: The Effects of Screw Design and Cement Augmentation. PLoS ONE 2015, 10, e0146294. [Google Scholar] [CrossRef] [Green Version]
- Patil, C.G.; Lad, S.P.; Santarelli, J.; Boakye, M. National inpatient complications and outcomes after surgery for spinal metastasis from 1993–2002. Cancer 2007, 110, 625–630. [Google Scholar] [CrossRef]
- Dea, N.; Versteeg, A.; Fisher, C.; Kelly, A.; Hartig, D.; Boyd, M.; Paquette, S.; Kwon, B.; Dvorak, M.; Street, J. Adverse events in emergency oncological spine surgery: A prospective analysis. J. Neurosurg. Spine 2014, 21, 698–703. [Google Scholar] [CrossRef]
- Versteeg, A.L.; Verlaan, J.J.; de Baat, P.; Jiya, T.U.; Stadhouder, A.; Diekerhof, C.H.; van Solinge, G.B.; Oner, F.C. Complications After Percutaneous Pedicle Screw Fixation for the Treatment of Unstable Spinal Metastases. Ann. Surg. Oncol. 2016, 23, 2343. [Google Scholar] [CrossRef] [Green Version]
- Formiga, M.C.; Gehrke, A.F.; DeBortoli, J.P.; Gehrke, S.A. Can the design of the instruments used for undersized osteotomies influence the initial stability of implants installed in low-density bone? An in vitro pilot study. PLoS ONE 2021, 16, e0257985. [Google Scholar]
- Calvert, K.L.; Trumble, K.P.; Webster, T.J.; Kirkpatrick, L.A. Characterization of commercial rigid polyurethane foams used as bone analogs for implant testing. J. Mater. Sci. Mater. Med. 2010, 21, 1453–1461. [Google Scholar] [CrossRef] [PubMed]
- Abshire, B.B.; McLain, R.F.; Valdevi, A.; Kambic, H.E. Characteristics of pullout failure in conical and cylindrical pedicle screws after full insertion and back-out. Spine J. 2001, 1, 408–414. [Google Scholar] [CrossRef]
- Krenn, M.H.; Piotrowski, W.P.; Penzkofer, R.; Augat, P. Influence of thread design on pedicle screw fixation. Laboratory investigation. J. Neurosurg. Spine 2008, 9, 90–95. [Google Scholar] [CrossRef]
- Addevico, F.; Morandi, M.; Scaglione, M.; Solitro, G.F. Screw insertion torque as parameter to judge the fixation. Assessment of torque and pull-out strength in different bone densities and screw-pitches. Clin Biomech 2020, 72, 130–135. [Google Scholar] [CrossRef]
- Ricci, W.M.; Tornetta, P.; Petteys, T.; Gerlach, D.; Cartner, J.; Walker, Z.; Russell, T.A. A comparison of screw insertion torque and pullout strength. J. Orthop. Traum. A 2010, 24, 374–378. [Google Scholar] [CrossRef] [Green Version]
- Pfeiffer, F.M.; Abernathie, D.L. A comparison of pullout strength for pedicle screws of different designs: A study using tapped and untapped pilot holes. Spine 2006, 31, E867–E870. [Google Scholar] [CrossRef]
- Hsieh, M.K.; Li, Y.D.; Liu, M.Y.; Lin, C.X.; Tsai, T.T.; Lai, P.L.; Tai, C.L. Biomechanical Comparison of Fixation Stability among Various Pedicle Screw Geometries: Effects of Screw Outer/Inner Projection Shape and Thread Profile. Appl. Sci. 2021, 11, 9901. [Google Scholar] [CrossRef]





Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hsieh, M.-K.; Li, Y.-D.; Hsu, Y.-J.; Tsai, T.-T.; Lai, P.-L.; Lee, D.-M.; Tai, C.-L. Novel Dual-Threaded Pedicle Screws Provide Fixation Stability That Is Comparable to That of Traditional Screws with Relative Bone Preservation: An In Vitro Biomechanical Study. Appl. Sci. 2022, 12, 6172. https://doi.org/10.3390/app12126172
Hsieh M-K, Li Y-D, Hsu Y-J, Tsai T-T, Lai P-L, Lee D-M, Tai C-L. Novel Dual-Threaded Pedicle Screws Provide Fixation Stability That Is Comparable to That of Traditional Screws with Relative Bone Preservation: An In Vitro Biomechanical Study. Applied Sciences. 2022; 12(12):6172. https://doi.org/10.3390/app12126172
Chicago/Turabian StyleHsieh, Ming-Kai, Yun-Da Li, Yun-Ja Hsu, Tsung-Ting Tsai, Po-Liang Lai, De-Mei Lee, and Ching-Lung Tai. 2022. "Novel Dual-Threaded Pedicle Screws Provide Fixation Stability That Is Comparable to That of Traditional Screws with Relative Bone Preservation: An In Vitro Biomechanical Study" Applied Sciences 12, no. 12: 6172. https://doi.org/10.3390/app12126172
APA StyleHsieh, M.-K., Li, Y.-D., Hsu, Y.-J., Tsai, T.-T., Lai, P.-L., Lee, D.-M., & Tai, C.-L. (2022). Novel Dual-Threaded Pedicle Screws Provide Fixation Stability That Is Comparable to That of Traditional Screws with Relative Bone Preservation: An In Vitro Biomechanical Study. Applied Sciences, 12(12), 6172. https://doi.org/10.3390/app12126172





