1. Introduction
In modern society, the rhythm of activity and rest in humans is largely determined by social rhythms (work/school schedules, etc.). At the same time, the role of the circadian system in the regulation of physiological function and sleep–wake rhythms remains substantial [
1]. The discrepancy of mid-sleep phase between work and free days, most common in individuals with the late chronotype [
2], leads to a mismatch in the function of the circadian system, defined as ‘social jetlag’ (SJL) [
3]. Numerous studies have shown that SJL is associated with cognitive impairment [
4], low academic performance [
5], and a predisposition to depression [
6], bad habits [
3], obesity [
7], and type 2 diabetes [
8].
A comprehensive review of the circadian misalignment concept, its contribution to chronobiology [
9,
10], shortcomings [
9,
11], possible practical applications [
12,
13], and directions for further development [
9] is currently underway. The most reliable and reproducible results have been obtained regarding the association of SJL with cognitive decline in students [
4,
5]. Researchers have found practical application in changing the working hours of educational institutions in order to increase the efficiency of the educational process: a one-hour delay in the start of classes [
12,
14,
15] and a flexible school start time, taking into account the chronotype of students [
13,
16].
Currently, the most serious problem for addressing circadian misalignment is the lack of objective data on the causal relationship between SJL and the clinical manifestations of this form of circadian misalignment. To solve this problem, additional research at a qualitatively higher level is required. The need for the further development of this area of chronobiology was assessed by one of the authors of the concept: “
In fact, most studies investigating the associations between SJL and health are cross-sectional. Further longitudinal studies are needed not only to confirm causal associations but also to clarify under how much and for how long one needs to be exposed to SJL for its consequences to show” [
9].
Based on the foregoing, there is a need to search for and put into practice objective indicators that make it possible to quantify the degree of circadian system misalignment. These methods should be fairly simple and inexpensive. It is important that these methods can be used in conditions as close to natural as possible. It is also important that they allow continuous recording of indicators for a significant amount of time to obtain a time series.
Some progress has been made in this direction. A chronotype or phase of entrainment (MSFsc) [
2,
9] and SJL have been shown to correlate with the dim-light melatonin onset (DLMO) [
17,
18,
19] and the cortisol awakening response (CAR) [
20,
21,
22], indicators that have long been widely used to assess the state of the circadian system. However, the use of these indicators is difficult due to the high cost of consumables and the complexity of the analyses. There was also a correlation between SJL and the amplitude of the 24 h rhythm of the wrist temperature [
23]. This method satisfies the above requirements as much as possible. One of its disadvantages is the fact that it only indirectly reflects the state of the circadian system; thus, it must be used in combination with other methods, such as wrist actimetry
Currently, wrist actimetry is widely used to assess the state of the circadian system [
24,
25,
26,
27,
28] and sleep function [
28,
29]. An important advantage of the method is that it has been used to develop and test a wide range of indicators that have long been actively used in clinical practice [
30,
31,
32]. Wrist actimetry is used to calculate parametric (Midline Estimating Statistic of Rhythm (MESOR), amplitude (
A), and acrophase (
φ) [
33,
34]) and nonparametric (interdaily stability (IS), intradaily variability (IV), the least active 5 h period (L5) that is nocturnal activity, and the most active 10 h period (M10) that is daily activity [
30,
31,
35]) indices. It is of interest to study the relationship of the indicators of the state of the circadian system and sleep function, assessed by the questionnaire survey method, with the objective indicators obtained by the method of wrist actimetry, which will enable future determination of approaches for a reliable assessment of the contribution of the circadian system misalignment to the development of various pathologies.
The aim of this study was to analyze the relationship between the subjective indicators characterizing the state of the circadian system and sleep function on the one hand and the objective indicators characterizing the 24 h rest–activity rhythm on the other hand.
In this article, in accordance to standard procedure [
36], we first calculated basic statistics of the studied indicators (mean, standard deviations, and normality of distribution). We converted some values to normalize them, if necessary, and then analyzed the association between subjective and objective indicators in two ways: (1) we carried out an analysis of covariance for a preliminary assessment of the relationship between the studied indicators and (2) the final conclusion about the presence and nature of relationships between the indicators was made on the basis of multiple regression analysis adjusted for concomitant factors (sex, age, and BMI).
3. Results
Mean values of MSF
SC in study participants was 04:13 (
Table 1). Early chronotype was observed in 39%, intermediate in 35%, and late in 25% of participants (
Table 2). The average value of SJL in our study was 1 h and 90 min (
Table 1). SJL > 1 h was observed in 75% and SJL > 2 h in 43% of study participants (
Table 3). The average sleep duration was 6 h and 53 min (
Table 1). The study participants were approximately equally distributed in three groups: less than 6.5 h, from 6.5 to 7.5 h, and more than 7.5 h (
Table 4). Low sleep quality (PSQI > 5) was observed in 42% of study participants (
Table 5).
As a result of ANCOVAs (
Table 2,
Table 3,
Table 4,
Table 5 and
Table 6), a significant positive association of chronotype (MSFsc) with M10t (
F = 5.435,
p = 0.006) and L5t (
F = 5.618,
p = 0.005) and negative with IS (
F = 3.520,
p = 0.035;
Table 2) was noted. There was also a significant positive relationship between SJL and AciB (
F = 5.901,
p = 0.004;
Table 3). There was a significant negative association SlD with M10t (
F = 3.203,
p = 0.047) and L5t (
F = 5.913,
p = 0.004), as well as a positive relationship with IS (
F = 5.033,
p = 0.009;
Table 4). A significant positive relationship between PSQI and AciB (
F = 12.969,
p = 0.001;
Table 5) and a negative relationship was noted between SlE and
φ (
F = 3.686,
p = 0.030;
Table 6).
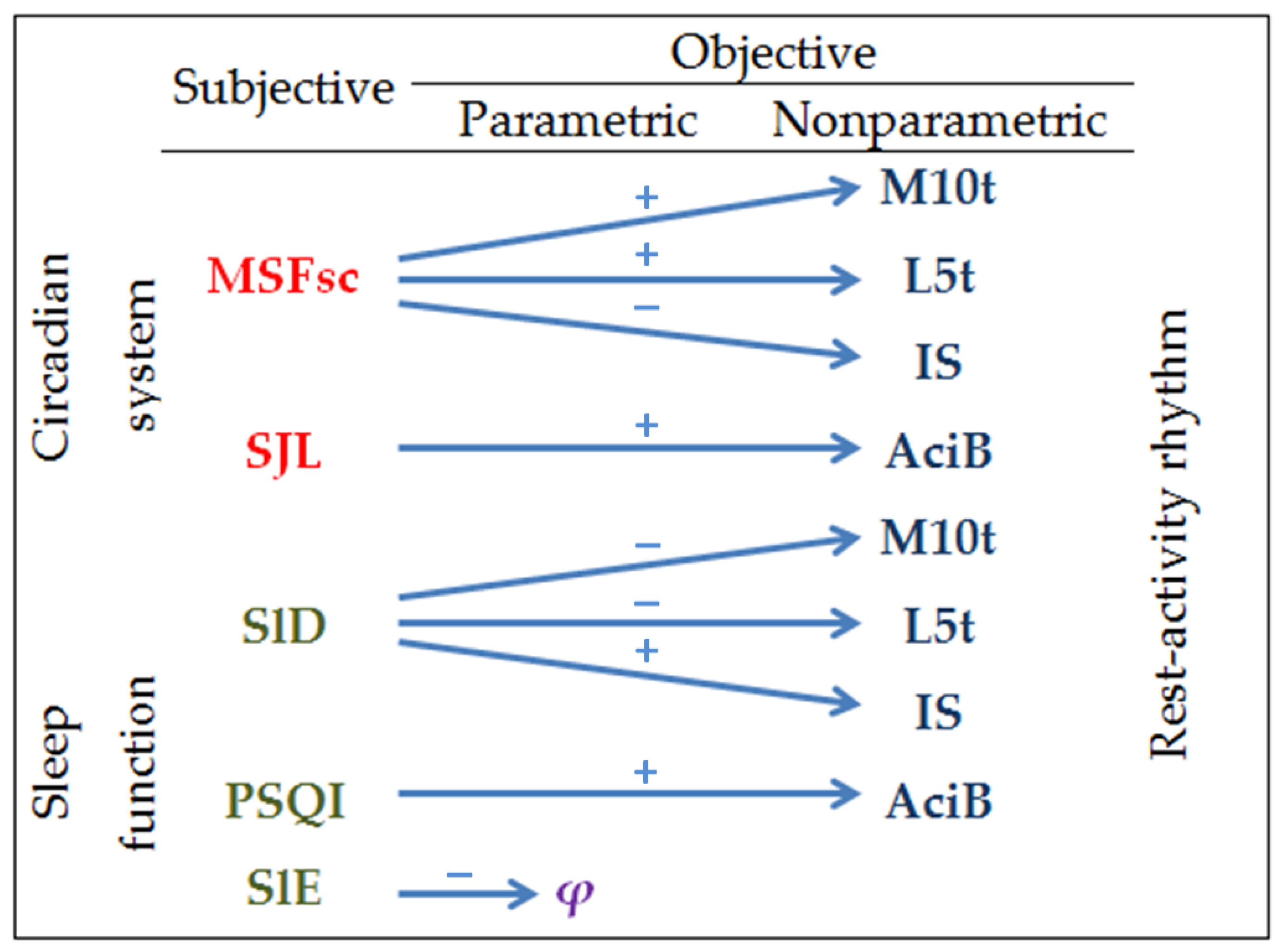
We conducted a multiple regression analysis to identify associations among subjective and objective indices, adjusted for related factors (sex, age, BMIc). In total, seven significant relationships were identified (
Table 7). There was a significant association of MSFsc with M10t (
B = 0.252,
p = 0.015), L5t (
B = 0.338,
p = 0.005), and IS (
B = −0.021,
p = 0.017) and of SlD with M10t (
B = −0.257,
p = 0.003), L5t (
B = −0.340,
p = 0.001), and IS (
B = 0.042,
p = 0.003). There was a significant association of SJL (
B = 0.320,
p = 0.032) and PSQI global scores (
B = 0.990,
p = 0.013) with AciB and of SlE with
φ (
B = −0.043,
p = 0.007;
Table 7).
4. Discussion
This study assessed the relationship between the wrist actimetry-derived 24 h rhythm of motor activity indices and the sleep–wake rhythm characteristics obtained by a questionnaire survey. Parametric (MESOR,
A, and
φ) and nonparametric (IS, IV, L5, L5t, M10, M10t, AcoB, and AciB) indices were used as the objective indicators of the 24 h rhythm of motor activity. The indicators obtained using the MCTQ (MSFsc, SJL, SlD, SlE) and PSQI global score were used as the subjective indicators of the sleep–wake rhythm and sleep quality. In general, a closer relationship was noted between the nonparametric indicators of the 24 h rhythm of motor activity and the sleep–wake rhythm characteristics. According to our data, the IS, L5t, and M10t were predictors of the MSFsc and SlD, and the AciB was a predictor of SJL and the PSQI global score (
Figure 3). Of the parametric indicators, only
φ showed a significant association with the SlE. Based on this, it can be concluded that the nonparametric indicators of the 24 h rhythm of motor activity are more suitable for assessing the state of the circadian system. Therefore, in the further development of the circadian misalignment concept and its contribution to various pathologies, it is necessary to take this circumstance into account.
In previous studies, nonparametric indicators of the 24 h rhythm of motor activity were actively used to assess the state of the circadian system in patients with chronic diseases. It has been shown that women with breast cancer have significantly higher values of IV [
43] and low values of the IS [
44], M10 [
43,
44], and L5 [
43]. Low IS values are associated with elevated blood pressure and a higher incidence of arterial hypertension [
45]. High IV values were observed in individuals with bipolar disorders [
46]. Low IS values and high IV values are associated with increased mortality [
47]. The parametric indicators of the 24 h rest–activity rhythm have been used relatively less frequently. A decrease in the MESOR and
A values was observed in women with breast cancer [
43,
44] and in people suffering from a binge eating disorder [
48]. In [
49], it was suggested that when approximating a time series of motor activity using the Cosinor method, a significant part of the trait variability was considered as unexplained. However, from our point of view, a more fundamental reason for the low sensitivity of the parametric indicators is that the 24 h rest–activity rhythm itself is a complex integral indicator, which, along with the circadian system, is associated with a number of other external and internal factors. As an output, activity is non-sinusoidal and incorporates napping components that vary in timing and duration among individuals. Therefore, in order to increase the sensitivity of the wrist actimetry method in assessing the state of the circadian system, it is necessary to take into account the contribution of these concomitant factors by improving the design of the study and the method of processing the time series. First, it is necessary to use wrist actimetry in combination with other methods, for example, the 24 h rhythm of the wrist temperature. This direction is being successfully developed by scientists under the leadership of Madrid J.A. et al. [
26]. Secondly, it is necessary to improve the data processing algorithm in order to reduce the variability of the indicator introduced by the concomitant factors and to increase the variability associated with the function of the circadian system.
One way to solve the second problem is to use combined indicators based on parametric and nonparametric indices. Consider, for example, the phase of entrainment (MSFsc). It is logical to assume the existence of a close relationship between the MSFsc and
φ. However, we did not find such a relationship. At the same time, there was a significant association of the MSFsc with the L5t and M10t. It is important to emphasize that, despite the difference in the calculation method, the M10t in its meaning is an analogue of
φ, although it differs from it by more than 1.5 h (
Table 1). Therefore, it is obvious that by introducing a correction factor when calculating
φ, it is possible to increase the accuracy of calculating the phase of the 24 h rest–activity rhythm. In addition, we have shown a significant association of the SlD with the L5t and M10t; so, when calculating the phase of the 24 h rest–activity rhythm, it is also necessary to correct for the duration of sleep.
The situation is somewhat more complicated with the SJL indicator, which reflects the state of circadian misalignment. It is known that there is a positive relationship between the MSFsc and SJL [
3], indicating that persons with a late chronotype are more prone to circadian misalignment. Of the previously proposed wrist actimetry-derived indices, the IS is more suitable for use as an objective indicator reflecting the state of circadian misalignment [
24]. In this study, we noted a negative relationship between the MSFsc and the IS, indicating that the stability of the 24 h rest–activity rhythm is reduced in individuals with a late chronotype. Similar results were previously obtained by other authors in healthy individuals [
24] and in patients with spinal cord injury [
50]. However, neither ANCOVA nor multiple regression analysis allowed us to identify a significant association between SJL and the IS, only post hoc comparison showed a significant decrease in the IS in individuals with SJL ≥ 2 h. Unfortunately, there is no information about the nature of the relationship between SJL and the IS in the available literature. There are only indirect data confirming our conclusion. One work [
45] showed that the IS is a stronger predictor of blood pressure disorders in adults than SJL. This indicates that the IS describes the state of circadian misalignment somewhat differently than SJL. In the future, it will be necessary to study in more detail the factors affecting the nature of the relationship between SJL and the IS, which will allow us to create a combined objective indicator that more accurately describes the state of circadian misalignment.
Previously, the relationship between SJL and the PSQI global score has been repeatedly noted [
51,
52], indicating that one of the signs accompanying circadian misalignment is a deterioration in sleep quality. In our study, there was a significant relationship between SJL and the AciB, an indicator reflecting the level of motor activity in bed at night. The AciB can be considered as an objective indicator reflecting the quality of sleep: the higher the level of motor activity at night, the worse the sleep quality. This is evidenced by the significant relationship between the AciB and the PSQI global score. The indicator AciB is an analogue of the previously described nonparametric indicator L5. However, this indicator does not reliably describe sleep quality, since we did not find a significant association between the L5 and the PSQI global score. In the future, when creating an objective indicator characterizing the state of circadian misalignment, one should correct for sleep quality, for example, using the AciB index.
The presented study has a number of limitations. We used an insufficiently large sample size. In addition, the work used actimeters of an outdated model that did not automatically calculate the characteristics of the sleep function, such as the sleep onset and offset, sleep inertia and latency, and sleep efficiency and duration. Therefore, the conclusions presented in this paper should be considered as preliminary, requiring careful rechecking.