1. Introduction
Since its introduction in clinical practice, total knee arthroplasty (TKA) has been considered one of the most successful procedures in orthopedic surgery, with survival rates greater than 90% for 10- and 15-year implants [
1]. TKA procedures are expected to increase remarkably in future years. Forecasts estimate that the annual case number could reach from 1.3 million to nearly 3.5 million primary TKAs per year in the United States by 2030 [
2].
Aging of populations, the increase in risk factors such as obesity, and the necessity of maintaining a good quality of life with an active lifestyle will continue to fuel this trend in developed countries.
A parallel increase in TKA revisions is expected, with a considerable clinical burden on patients and a financial burden on healthcare organizations. The current revision rate at 10-year follow-up varies within narrow limits; the Australian register reported a rate of 5.5%, and the UK rate is slightly lower (5%) [
3]. In a recent review [
4], the cumulative incidence for TKA revision procedure was 1.2% at 1 year, 1.9% at 2 years, 3.1% at 5 years, 4.4% at 10 years, and 6.1% at 15 years after the index primary TKA. Interestingly, the failure causes changed in the last decade, with an increased number of aseptic loosening (29.8%), infections (14.8%), and pain due to the malposition of implants (9.5%) [
3].
A critical point is the achievement of a correct preoperative diagnosis for TKA failure: several authors reported bad outcomes when revision surgery was performed merely to ease subjective pain, without clear explanation and diagnosis [
5]. Vince et al. described eight different mechanisms of implant failure: sepsis, extensor discontinuity, stiffness, tibial femoral instability, patellar tracking, aseptic loosening and osteolysis, periprosthetic fracture, and component breakage. A ninth category, unexplained pain, is an indication for further investigation but not for surgery [
6].
Implant stability, as well as adequate and stable fixation at component–bone interface, concretize the key to long-term survivorship in both primary and revision TKA [
7]. Constrained condylar knee (CCK) prostheses are a common choice for difficult primary TKA and revision total knee arthroplasty [
8]. The choice to use a varus valgus constrained (VVC), such as a CCK prosthesis, depends on the evaluation of the residual bone stock; on the bone defect to manage with augments, stems, cones or sleeves; and on the ligamentous incompetence of the collateral ligaments and posterior capsule.
However, previous literature reports high rates of complications, readmissions, and mortality associated with revision surgery [
9]; moreover, TKA revision procedure consumes more than 50% more resources than primary TKA [
8]. Although several studies have reported the outcomes of the use of CCK implants in the treatment of primary severe osteoarthritis and revision TKA [
10,
11], the relationship between the success rate and the preoperative diagnosis in revision surgery is still unclear.
The first objective of this paper is to report the clinical and functional results of a cohort of patients with different causes of primary failure, who underwent TKA revision at mid- to long-term follow-up.
Given that different preoperative-causes-of-revision may have different effects on postoperative functional and clinical outcomes, the second purpose of this paper is to evaluate possible differences in postoperative functional and clinical outcomes among preoperative-cause-of-revision subpopulations of patients who underwent TKA revision with NexGen® Legacy® Constrained Condylar Knee (LCCK) implants.
2. Materials and Methods
This retrospective study included a consecutive series of patients who underwent surgery for TKA revision with NexGen® LCCK implants. All the surgeries were performed in one institution by the same senior surgeon.
We collected the data of 105 surgeries performed between January 2008 and December 2014.
The exclusion criteria were multiple revisions (5 patients) in which we used cases of rotational-hinge implants (RHK), secondary osteoarthritis as in hemophilia (2 patients), and inflammatory arthritis (8 patients). Multiple revisions were performed in patients with a recurrence of infection after the first revision surgery (3 patients) and in 2 patients in which subjective instability persisted. In all the patients, it was necessary to increase the degree of constraint of the implant. Generally, we used these implants in cases of severe bone loss associated with severe instability with incompetence of the collateral ligaments.
The final cohort in this study was composed of 85 patients, who were divided into subpopulations depending on the causes of revision in order to study the differences among their outcomes.
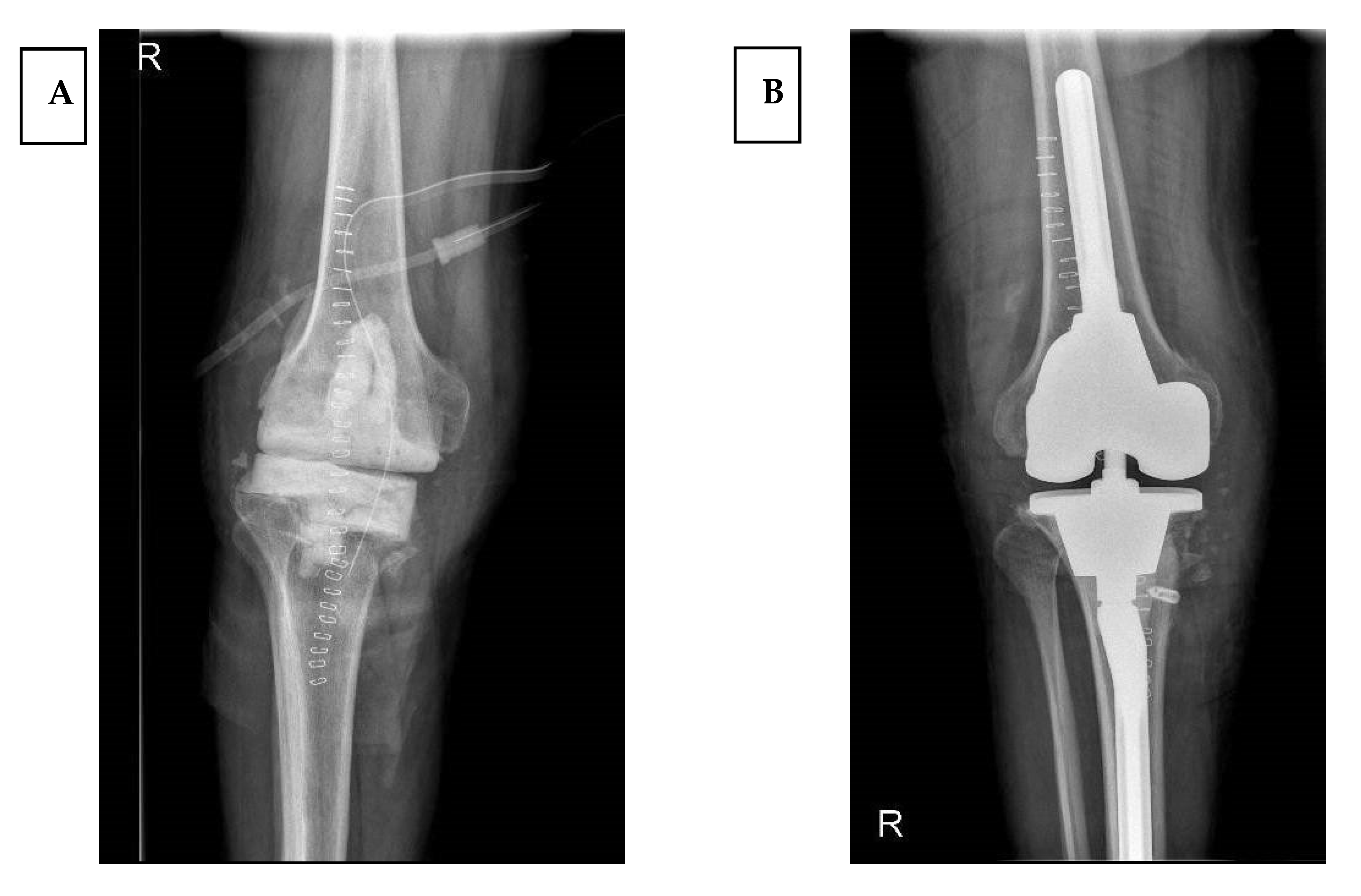
Prosthetic infection was diagnosed following the Musculoskeletal Infection Society (MSIS) criteria [
12], and each infection case underwent a two-stage procedure (
Figure 1).
Instability diagnosis was based on symptoms, physical exams, and intraoperative evaluation. We considered early instability as a consequence of global ligamentous imbalance, failure of intra-operative ligamentous balancing, flexion–extension gap mismatch, iatrogenic ligaments injury during the procedure, or pre-existing neuromuscular impairment. Moreover, we considered late instability when secondary to incorrect alignment, hence leading to progressive ligament stretching, polyethylene wear, components loosening, and finally secondary collapse [
13].
Implant loosening was detected by comparing consecutive radiological exams through time and CT scan evaluation. To assess periprosthetic bone, any radiolucency lines were checked using the Knee Society Total Knee Arthroplasty Radiographic Evaluation and Scoring System [
14]. In an anteroposterior view, the following areas were identified on the tibial component. Areas 1 and 2 correspond to the medial tibial plate, areas 3 and 4 to the lateral tibial plate, and areas 5, 6, and 7 to the fixation zones at the contour of the implant keel. In order to quantify any bone lysis, the sum of the width (expressed in mm) of the radiolucency lines in each of the zones was calculated, and if this was >10 mm it was judged an important indicator of failure.
Malpositioning was detected by conventional X-rays and CT studies. A wrong positioning on the axial plan was often found. The criteria of Berger et al. [
15] were used to assess the positioning of the femoral component. In order to assess the correct femoral component rotation, the normal posterior condylar angle was used as a reference, with a native rotation value of 0.3° (±1.2°) of internal rotation for women and 3.5° (± 1.2°) for men, relative to the surgical epicondylar axis. To evaluate the tibial component correct rotation, the normal relationship between the orientation of the tibial tubercle and the tibial articular surface was used. The normal rotation value for the tibial component, which corresponds to the native articular surface, is 18° (± 2.6°) of internal rotation from the tip of the tubercle.
The diagnosis of fracture followed the usual clinical–radiological path, using the Unified Classification System (UCS); revision surgery was performed exclusively in B2 and B3 types. Massive bone defects, when present, were classified according to the Anderson Orthopedic Research Institute (AORI) system [
16]. The surgical technique adopted was similar for all cases: the three-step technique [
17] was routinely adopted; bone defects were managed after component removal and before cone preparation. In case of bone loss, in order to achieve sound fixation in zone 2 [
18] and reconstruct the bone loss, cones were implanted. On the tibial side, cone preparation consisted of preparation with high-speed burr followed by power reaming of the metaphyseal bone; subsequent broaching was then performed with a metaphyseal broach. A similar procedure was employed on the femoral side with respect to the distal femoral resection level when a femoral cone was used.
The previous approach was used, mostly medial parapatellar, extended proximally where necessary; femoral and tibial intramedullary alignment was always performed. If necessary, stems or augments were used to fill the bone gap and reach the desired stability. All the patients received standard postoperative rehabilitation.
All the patients were subjected to a standard follow-up protocol with clinical and radiological exams at 1, 3, 6, 12, 24, and 36 months, and at last follow-up. During the last follow-up, patient-reported outcome measures (PROMs) [
19] were used to evaluate outcomes, with data derived from the Oxford knee score (OKS), the EQ-5D index, and EQ-VAS questionnaires analyzed. Moreover, we decided to implement the functional outcomes obtained by PROMs with clinical data based on the Knee Society Score (KSS) [
20] and on maximum degree of flexion.
Statistical Analysis
In this paper, the median was used as a measure of central tendency due to the type of data, the sample size, and the outcomes. Continuous or ordinal variables were presented as median and 25° and 75° percentile—interquartile range (IQR). Categorical variables were presented as frequency and percentages. The non-parametric Kruskal–Wallis (KW) test was used to compare functional and clinical outcomes among the preoperative-cause-of-revision groups (i.e., the aseptic loosening, malpositioning, infection, instability, and periprosthetic fracture groups). Where a significant difference was found between groups, post hoc comparisons needed to be performed to determine where the difference lay, by Dunn’s multiple comparison test (in the
Appendix in Supplementary Materials). All the statistical analyses were performed by SAS 9.4 Institute Inc., Cary, NC, USA, 2016, considering
p value < 0.05 statistically significant.
3. Results
The median follow-up was 99.7 months (IQR 80.2–115.3 months) and the mean period from index surgery to revision surgery was 36 months (range 9–72 months). The patients were predominantly women (63 patients) with a median BMI of 27.9 (IQR 25.3–31.6). The median age was 71.5 (IQR 65.1–74.9).
The group with preoperative diagnosis of aseptic loosening consisted of 25 patients (29% of the total). In this group the median duration of the follow up was 105 months (IQR 89–118), the median value of the OKS was 39 (range 36–43), the median value of the EQ-VAS was 60 (IQR 51–66), the median value of the EQ-5D was 0.81 (IQR 0.74–0.85), the median value of the KSS was 84 (IQR 81–88), and the median value of the range of motion was 102° (IQR 94–109°).
The group of with preoperative diagnosis of malpositioning included 24 patients (28% of the total); in this group the median duration of the follow up was 100 months (IQR 80–108), the median value of the OKS was 36 (IQR 26–41), the median value of the EQ-VAS was 56 (IQR 48–61), the median value of the EQ-5D was 0.72 (IQR 0.67–0.77), the median value of the KSS was 57 (IQR 50–66), and the median value of the range of motion was 94° (IQR 88–102°).
The group with preoperative diagnosis of infection included 20 patients (24% of the total); in this group the median duration of the follow-up was 92 months (IQR 82–121), the median value of the OKS was 25 (IQR 17–35), the median value of the EQ-VAS was 43 (IQR 37–53), the median value of the EQ-5D was 0.44 (IQR 0.32–0.60), the median value of the KSS was 64 (IQR 53–71), and the median value of the range of motion was 89° (IQR 78–98°).
The group with preoperative diagnosis of instability included 9 patients (11% of the total); in this group the median duration of the follow-up was 97 months (IQR 73–101), the median value of the OKS was 32 (IQR 27–35), the median value of the EQ-VAS was 39 (IQR 36–48), the median value of the EQ-5D was 0.77(IQR 0.75–0.85), the median value of the KSS was 66 (IQR 63–71), and the median value of the range of motion was 98° (IQR 85–104°).
The group with preoperative diagnosis of periprosthetic fracture included 7 patients (8% of total); in this group the median duration of the follow-up was 102 months (IQR 88–125), the median value of the OKS was 44 (IQR 33–45), the median value of the EQ-VAS was 73 (IQR 67–78), the median value of the EQ-5D was 0.71 (IQR 0.68–0.74), the median value of the KSS was 83 (IQR 72–92), and the median value of the range of motion was 105° (IQR 96–111°°).
The preoperative diagnosis, the number of patients, the median follow-up for each subgroup, the PROMs, and the ROM are summarized in
Table 1.
The preoperative-cause-of-revision groups are similar in demographic features, as no significant differences was found (
p > 0.05,
Table 2).
The Kruskal–Wallis test indicated statistically significant differences among the medians of the groups of the outcomes (
Table 3,
p < 0.05).
From a purely descriptive point of view, the difference values of the functional outcomes in preoperative-cause-of-revision groups are shown in (
Table 1). For the Oxford knee score (OKS), the highest median value was in the periprosthetic fracture group (43.25, IQR 32.7-45.3) and the lowest median value was in the infection group (24.8, IQR 17.4–34.8). For the EQ-VAS, the highest median value was in the periprosthetic fracture group (73.0, IQR 67.0-78.0) and the lowest median value was in the instability group (39.0, IQR 36.0–48.0). For the EQ-5D-5L, the highest median value was in the aseptic loosening group (0.81, IQR 0.74–0.85) and the lowest median value was in the infection group (0.44, IQR 0.32–0.60). For the Knee Society Score (KKS), the highest median value was in the aseptic loosening group (84.0, IQR 81.0-88.0) and the lowest median value was in the malpositioning group (56.5, IQR 49.4–66.0). For the range of motion (ROM), the highest median value was in the periprosthetic fracture group (105.0°, IQR 96.0–111.0°) and the lowest median value was in the infection group (88.5°, IQR 77.5–98.0°). The Dunn’s test (with Bonferroni correction) was used to perform post hoc comparisons (see
Supplementary Materials) and determine where the differences lie.
For the OKS, the comparisons between the periprosthetic fracture group and the infection group (p.adj = 0.012) and between the aseptic loosening group and the infection group (p.adj < 0.001) were significant. For the EQ-VAS, the comparisons between the periprosthetic fracture group and the infection group (p.adj < 0.001) and between the instability group (p.adj < 0.001) and the malpositioning group (p.adj = 0.032) were significant. Moreover, the comparisons between the aseptic loosening group with the infection group (p.adj = 0.01) and with the instability group (p.adj = 0.005) were also significant. For the EQ-5D-5L, the comparisons between the infection group and the aseptic loosening group (p.adj < 0.001) and between the instability group (p.adj < 0.001) and the malpositioning group (p.adj < 0.001) were significant. For the KKS, the comparisons between the aseptic loosening group and the infection group (p.adj < 0.001) and between the instability group (p.adj = 0.034) and the malpositioning group (p.adj < 0.001) were significant. Moreover, the comparisons between the periprosthetic fracture group with the infection group (p.adj = 0.035), and with the malpositiong group (p.adj = 0.002) were also significant. For the ROM, the Dunn’s test showed that the comparisons between the infection group with the periprosthetic fracture group (p.unadj = 0.018), and with the aspectic loosening group (p.unadj = 0.0016) were significant only at the level of the incorrect
p-value. All other comparisons were not significant (see
Supplementary Materials).
The group with preoperative diagnosis of aseptic loosening included 25 patients; in this group, according to AORI classification: 0 patients had bone defects classified as AORI I, 6 patients had bone defects classified as AORI IIA, 12 patients had bone defects classified as AORI IIB, and 7 patients had bone defects classified as AORI III.
The group with preoperative diagnosis of malpositioning included 24 patients; in this group, according to AORI classification: 16 patients had bone defects classified as AORI I, 8 patients had bone defects classified as AORI IIA, 0 patients had bone defects classified as AORI IIB, and 0 patients had bone defects classified as AORI III.
The group with preoperative diagnosis of infection included 20 patients; in this group, according to AORI classification: 0 patients had bone defects classified as AORI I, 7 patients had bone defects classified as AORI IIA, 8 patients had bone defects classified as AORI IIB, and 5 patients had bone defects classified as AORI III.
The group with preoperative diagnosis of instability included 9 patients; in this group, according to AORI classification: 0 patients had bone defects classified as AORI I, 2 patients had bone defects classified as AORI IIA, 6 patients had bone defects classified as AORI IIB, and 1 patient had bone defects classified as AORI III.
The group with preoperative diagnosis of periprosthetic fracture included 7 patients; in this group, according to AORI classification: 0 patients had bone defects classified as AORI I, 2 patients had bone defects classified as AORI IIA, 4 patients had bone defects classified as AORI IIB, and 1 patient had bone defects classified as AORI III.
In
Table 4, we report the type of bone defects according to the AORI Classification System.
The group with preoperative diagnosis of aseptic loosening included 25 patients (29% of the total); in this group the femoral long stem was implanted in 23 patients (92% of the total), the femoral short stem was implanted in 2 patients (8% of the total), the tibial long stem was implanted in 24 patients (96% of the total), the tibial short stem was implanted in 1 patient (4% of the total), the femoral cone was implanted in 3 patients (12% of the total), and the tibial cone was implanted in 5 patients (20% of the total).
The group with preoperative diagnosis of malpositioning included 24 patients; in this group the femoral long stem was implanted in 22 patients (92% of the total), the femoral short stem was implanted in 0 patients, the tibial long stem was implanted in 22 patients (92% of the total), the tibial short stem was implanted in 0 patients, the femoral cone was implanted in 3 patients (12.5% of the total), and the tibial cone was implanted in 3 patients (12.5% of the total).
The group with preoperative diagnosis of infection included 20 patients; in this group the femoral long stem was implanted in 16 patients (80% of the total), the femoral short stem was implanted in 4 patients (20% of the total), the tibial long stem was implanted in 15 patients (75% of the total), the tibial short stem was implanted in 5 patients (25% of the total), the femoral cone was implanted in 4 patients (20% of the total), and the tibial cone was implanted in 7 patients (35% of the total).
The group with preoperative diagnosis of instability included 9 patients; in this group the femoral long stem was implanted in 9 patients (100% of the total), the femoral short stem was implanted in 0 patients, the tibial long stem was implanted in 9 patients (100% of the total), the tibial short stem was implanted in 0 patients, the femoral cone was implanted in 0 patients, and the tibial cone was implanted in 2 patients (22% of the total).
The group with preoperative diagnosis of periprosthetic fracture included 7 patients; in this group the femoral long stem was implanted in 7 patients (100% of the total), the femoral short stem was implanted in 0 patients, the tibial long stem was implanted in 3 patients (43% of the total), the tibial short stem was implanted in 2 patients (29% of the total), the femoral cone was implanted in 2 patients (29% of the total), and the tibial cone was implanted in 3 patients (43% of the total).
Other techniques such as impaction grafting or cancellous allograft were used to fill the femoral and tibial defects when cones were not used. All the cones were tantalum (Trabecular Metal; Zimmer, Warsaw, Indiana, USA).
The number and type of stems and cones (
Figure 2a,b) used for each group of patients are summarized in
Table 5.
4. Discussion
Several studies in the literature have reported good results after revision total knee arthroplasty at short and medium follow-up as long as there was a clear diagnosis [
21,
22,
23,
24]]. The use of metaphyseal devices to increase the fixation and stability of the implant is well accepted nowadays [
18,
25]; advantages may include an easier and more predictable surgical technique, versatility of the system, and early mechanical support without the risk of late resorption and collapse. Brown et al. [
26] in 2015 concluded that despite the high complication rate in their series of patients, TM cones represent an attractive option for managing bone loss in complex primary and revision TKA with a high rate of osseointegration, stating that the majority of complications were not related to the implants used. The ideal fixation is still debated, and there is no agreement in the literature on whether hybrid fixation or full cementation is the better method [
27]; we adopted hybrid fixation with cementation of femur and tibia, including zone 2 [
18] and patella, with smooth or splined press-fit modular stems, reserving full cementation only in case of short stubby stems.
Siqueira et al. [
24] in 2015 performed a review of the studies on modes of failure in primary and revision knee arthroplasty; they found that the literature on varus valgus constrained implants was insufficient and that many outcome studies were limited by a small number of cases and short follow-ups. The authors considered ten studies, which included 294 patients overall, and found that the main causes of revision were infection (42%), aseptic loosening (34%), patellar complication (7%), and extensor mechanism complication (7%), but they concluded that a more reliable analysis of the outcomes would require larger cohorts with a longer follow-up.
Based on our data, we were not able to fully demonstrate a clear correlation between preoperative diagnosis and postoperative outcomes in knee arthroplasty revision surgery.
However, we found better outcomes with preoperative diagnosis of malpositioning and aseptic loosening and worse outcomes with infection diagnosis, with statistically significant differences in the clinical and functional outcomes. Despite the small sample, good results were obtained in the case of revision for periprosthetic fractures, but worse scores were observed in the instability group. Our findings are in line with those of van Kempen et al. [
21], who found better outcomes in the aseptic loosening group and moderate results in the malpositioning, instability, and infection groups at a mean follow-up of 24 months. Analyzing the outcomes of each group, we found that our results were worse for all the evaluated scores; however, it is important to underline that our cohort of patients was observed at mid- to long-term follow-up. Indeed, other studies involving series with longer follow-ups [
23] obtained worse clinical and functional results than those obtained for our series.
Our data are in line with those published by Lee et al. [
28], who performed a retrospective review of 206 cases of revision TKA performed in ten years in a single institution (2003–2012). They subdivided patients into a septic (120 cases) and an aseptic group (86 cases, with periprosthetic fracture and loosening being the main causes of the revision surgery) and evaluated the causes and outcome of the second surgery at a minimum follow-up of 2 years. In the septic group, the HSS score and KSS score were, respectively, 79.2 and 75.5 at follow-up, while in the aseptic group, the scores were, respectively, 85.5 and 86.6, showing a statistically significant difference between the two groups (
p < 0.05). The mean range of motion was 101° in the septic group and 117° in the aseptic group (
p < 0.05). The authors stated that mechanical complications that require revision (aseptic loosening and instability) decreased in relation to the development of surgical techniques and design. Finally, they concluded that the outcome of revision TKA was more successful in patients without infection than in patients with infection.
In our study, we observed better results for aseptic loosening and malpositioning than for infection. A possible reason for the good results in the aseptic loosening group could be that complaints in this group are caused solely by loosening of the components from the bone interface without other soft tissue disorders, as described by van Kempen et al. [
21] For the other indications where, theoretically, the soft tissue envelope is more involved, we found smaller improvements.
Moreover, in the infection group, there might have been reduced patient satisfaction due to the difficult revision related to severe bone loss and to the two-stage surgery, confirmed by the extensive use of stems and cones (see
Table 5). Furthermore, we observed that the use of trabecular metal cones for the femur and tibia was more often necessary for patients in the infection group (20% and 35%, respectively) than for patients in the aseptic loosening (12% and 20%, respectively) and malpositioning groups (12.5% and 12.5%, respectively) (see
Table 5).
One limitation of this study is the small simple size of some of the revision groups due to stratification into five main reasons for revision.
Moreover, the decision to stratify into five main reasons for revision is debatable because patients with nonfunctional TKA often have a combination of problems.
Another important limitation is that we encountered no cases of arthrofibrosis, making comparison on this ground unreliable.