Magnetic Mallet and Laser for a Minimally Invasive Implantology: A Full Arch Case Report
Abstract
:1. Introduction
1.1. Magnetic Mallet
1.2. Lasers in Dentistry
- Both laser families have photoablative effects;
- Low penetrating lasers do not go deep, and they have thermal effects but do not have great photodynamic and decontaminating effects. They are ideal for their ablative abilities on hard tissues (Er: YAG) and on soft tissues (CO2 and Er: YAG);
- Highly penetrating lasers have ablative, thermal (strong, medium, weak), photodynamic (or decontaminating) and biostimulating effects. The deeper we go into the fabric, the more the decontaminating and biostimulating effects increase and the thermal ones are reduced.
1.3. Photodynamic Therapy without Dye
- Use of ultrasonic instruments and irrigation with polyvinyl jodate-based solutions (Betadine), with complete debridement of the periodontal/peri-implant pocket;
- Use of air flow with glycine or bicarbonate with low abrasiveness on dental surfaces (on exposed implant surfaces it is preferable to use powders with high abrasive power, as the goal is not to preserve cellularity on contaminated surfaces, but to perfectly decontaminate the implant surfaces infected);
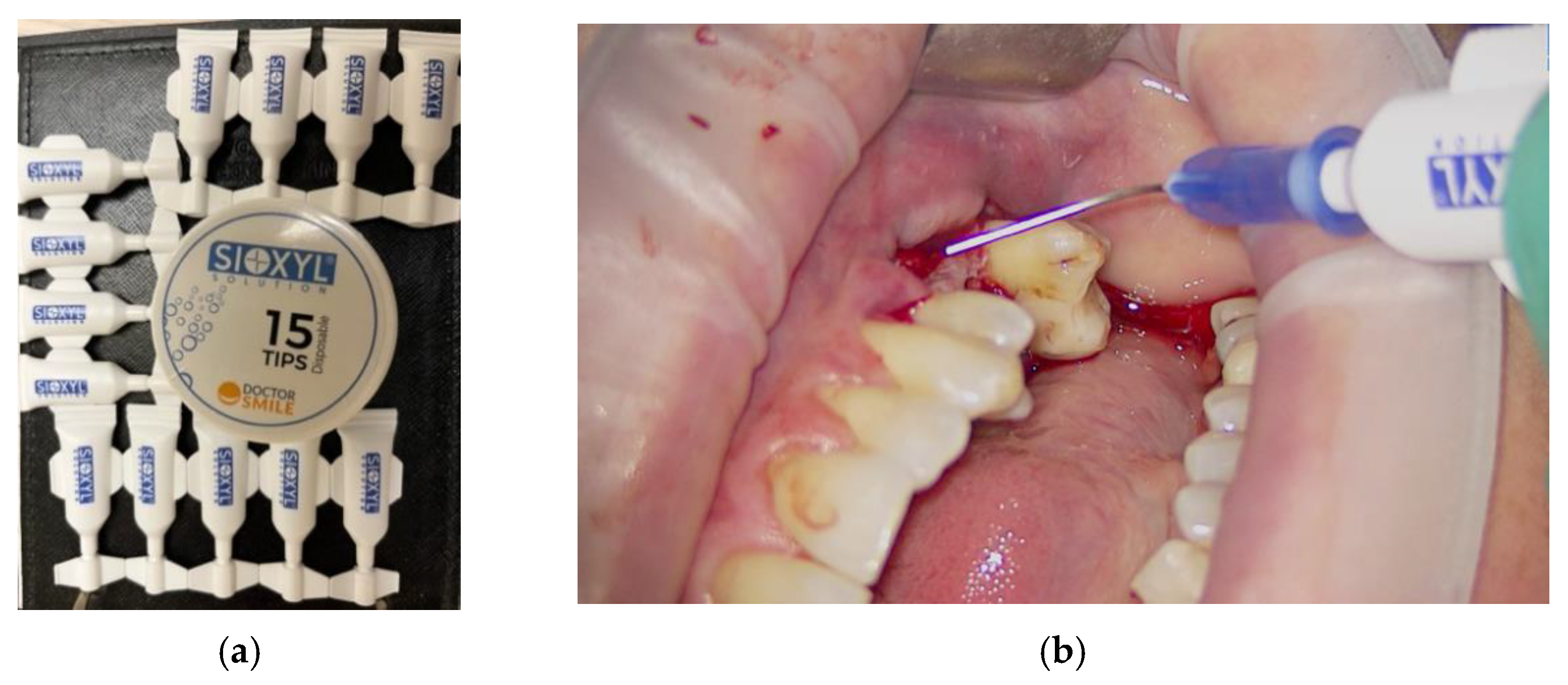
- Insert the 3% 10-volume hydrogen peroxide or Sioxyl solution (Doctor Smile, Vicenza, Italy) into the periodontal/peri-implant pocket and leave to act for at least 2 min, removing the excess with a surgical aspirator or dabbing with a sterile gauze pad;
- After the adequate oxygenation of the periodontal/peri-implant bone defect and of the corresponding soft tissues, the diode laser (980 nm) with 400 micron fiber, peak power 2.5 W but with the zeroing of the thermal effect (Ton by 20/30% and lowering the average power to 0.8 W) is used for 60 s;
- At the end of the treatment, advise the patient not to rinse to keep the bleeding resulting from the thermal effect of vasodilation in place, to refrain from oral hygiene maneuvers for at least 6 h and then resume normal home hygiene protocols.
1.4. OHLLT (Oxygen High Level Laser Therapy) Technology
- Stabilized H2O2 laser irradiation (Sioxyl solution)
- Liberation of molecules of H2O and fundamental oxygen (O2 has two unpaired electrons with parallel spin)
- New laser irradiation allows the passage of an electron to a higher orbital with spin inversion that allows the release of singlet oxygen
- Singlet oxygen causes the oxidation of the lipid membranes of bacteria with consequent bactericidal action.
- DNA denaturation of microorganisms
- Destruction of the lysosomal membrane
- Alteration of mitochondrial functions
1.5. Erbium Lasers
1.6. Minimally Invasive Implant Surgery Protocols
2. Materials, Methods and Results
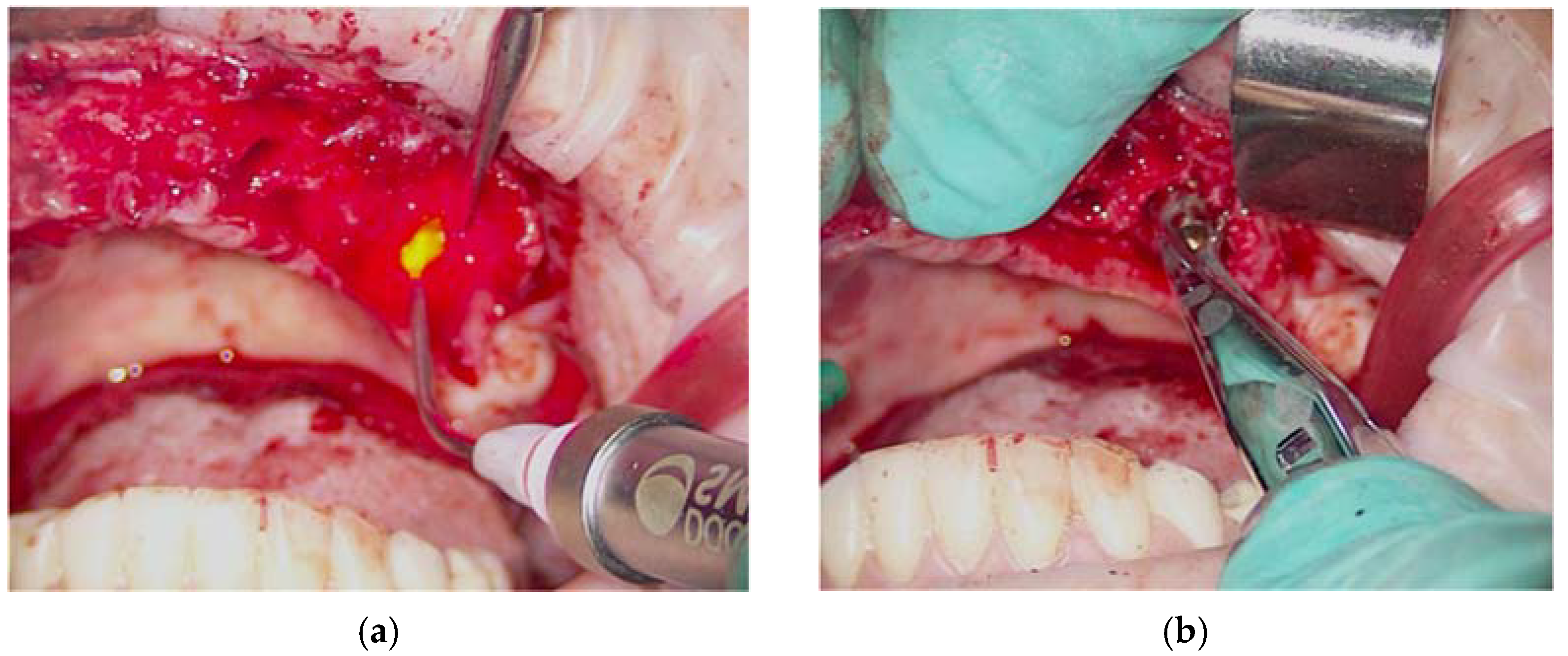
Surgical Procedure
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Cortellini, P.; Tonetti, M.S. Improved wound stability with a modified minimally invasive surgical technique in the regenerative treatment of isolated interdental intrabony defects. J. Clin. Periodontol. 2009, 36, 157–163. [Google Scholar] [CrossRef] [PubMed]
- Aimetti, M.; Ferrarotti, F.; Mariani, G.M.; Romano, F. A novel flapless approach versus minimally invasive surgery in periodontal regeneration with enamel matrix derivative proteins: A 24-month randomized controlled clinical trial. Clin. Oral Investig. 2017, 21, 327–337. [Google Scholar] [CrossRef] [PubMed]
- Aimetti, M.; Ferrarotti, F.; Bergandi, L.; Saksing, L.; Parducci, F.; Romano, F. Increase in periodontal interleukin-1β gene expression following osseous resective surgery using conventional rotary instruments compared with piezosurgery: A split-mouth randomized clinical trial. Int. J. Periodontics Restor. Dent. 2016, 36, 489–496. [Google Scholar] [CrossRef] [PubMed]
- Sharma, S.; Schneider, L.F.; Barr, J.; Aarabi, S.; Chibbaro, P.; Grayson, B. Comparison of minimally invasive versus conventional open harvesting techniques for iliac bone graft in secondary alveolar cleft patients. Plast. Reconstr. Surg. 2011, 128, 485–491. [Google Scholar] [CrossRef]
- Novy, B.B.; Fuller, C.E. The material science of minimally invasive esthetic restorations. Compend. Contin. Educ. Dent. 2008, 29, 338–346. [Google Scholar]
- Vertuani, S.; Nilsson, J.; Borgman, B.; Buseghin, G.; Leonard, C.; Assietti, R.; Quraishi, N.A. A cost-effectiveness analysis of minimally invasive versus open surgery techniques for lumbar spinal fusion in Italy and the United Kingdom. Value Health 2015, 18, 810–816. [Google Scholar] [CrossRef] [Green Version]
- Bennardo, F.; Barone, S.; Vocaturo, C.; Nucci, L.; Antonelli, A.; Giudice, A. Usefulness of Magnetic Mallet in Oral Surgery and Implantology: A Systematic Review. Oral Maxillofac. Surg. 2014, 18, 59–64. [Google Scholar] [CrossRef]
- Menchini-Fabris, G.B.; Toti, P.; Crespi, G.; Covani, U.; Crespi, R. Distal Displacement of Maxillary Sinus Anterior Wall Versus Conventional Sinus Lift with Lateral Access: A 3-Year Retrospective Computerized Tomography Study. Int. J. Environ. Res. Public Health 2020, 17, 7199. [Google Scholar] [CrossRef]
- Schierano, G.; Baldi, D.; Peirone, B.; Mauthe von Degerfeld, M.; Navone, R.; Bragoni, A.; Colombo, J.; Autelli, R.; Muzio, G. Biomolecular, Histological, Clinical, and Radiological Analyses of Dental Implant Bone Sites Prepared Using Magnetic Mallet Technology: A Pilot Study in Animals. Materials 2021, 14, 6945. [Google Scholar] [CrossRef]
- Crespi, R.; Capparè, P.; Gherlone, E. Sinus floor elevation by osteotome: Hand mallet versus electric mallet. A prospective clinical study. Int. J. Oral Maxillofac. Implant. 2012, 27, 1144–1150. [Google Scholar] [PubMed]
- Crespi, R.; Capparè, P.; Gherlone, E.F. Electrical mallet in implants placed in fresh extraction sockets with simultaneous osteotome sinus floor elevation. Int. J. Oral Maxillofac. Implant. 2013, 28, 869–874. [Google Scholar] [CrossRef] [PubMed]
- Crespi, R.; Capparè, P.; Gherlone, E. Electrical Mallet Provides Essential Advantages in Maxillary Bone Condensing. A Prospective Clinical Study. Clin. Implant. Dent. Relat. Res. 2012, 15, 874–882. [Google Scholar] [CrossRef] [PubMed]
- Desai, A.; Patil, S.; Mitra, D.; Shah, R. Magnetic Mallet-Feel the Future. JIDA J. Indian Dent. Assoc. 2020, 14, 26–30. [Google Scholar] [CrossRef]
- Crespi, R.; Capparè, P.; Gherlone, E. A comparison of manual and electrical mallet in maxillary bone condensing for immediately loaded implants: A randomized study. Clin. Implant. Dent. Relat. Res. 2014, 16, 374–382. [Google Scholar] [CrossRef] [PubMed]
- Maggioni, M.; Attanasio, T.; Scarpelli, F. I Laser in Odontoiatria; Piccin: Padova, Italy, 2009. [Google Scholar]
- Caccianiga, G.; Rey, G.; Baldoni, M.; Paiusco, A. Clinical, Radiographic and Microbiological Evaluation of High Level Laser Therapy, a New Photodynamic Therapy Protocol, in Peri-Implantitis Treatment; A Pilot Experience. Biomed Res. Int. 2016, 2016, 6321906. [Google Scholar] [CrossRef] [Green Version]
- Caccianiga, G.; Baldoni, M.; Ghisalberti, C.A.; Paiusco, A. A Preliminary In Vitro Study on the Efficacy of High-Power Photodynamic Therapy (HLLT): Comparison between Pulsed Diode Lasers and Superpulsed Diode Lasers and Impact of Hydrogen Peroxide with Controlled Stabilization. Biomed Res. Int. 2016, 2016, 1386158. [Google Scholar] [CrossRef]
- Caccianiga, G.; Rey, G.; Paiusco, A.; Lauritano, D.; Cura, F.; Ormianer, Z.; Carinci, F. Oxygen high level laser therapy is efficient in treatment of chronic periodontitis: A clinical and microbiological study using PCR analysis. J. Biol. Regul. Homeost. Agents 2016, 30, 87–97. [Google Scholar] [PubMed]
- Caccianiga, G.; Cambini, A.; Donzelli, E.; Baldoni, M.; Rey, G.; Paiusco, A. Effects of laser biostimulation on the epithelial tissue for keratinized layer differentiation: An in vitro study. J. Biol. Regul. Homeost. Agents 2016, 30, 99–105. [Google Scholar] [PubMed]
- Leonida, A.; Paiusco, A.; Rossi, G.; Carini, F.; Baldoni, M.G.; Caccianiga, G. Effects of low-level laser irradiation on proliferation and osteoblastic differentiation of human mesenchymal stem cells seeded on a three-dimensional biomatrix: In vitro pilot study. Lasers Med. Sci. 2013, 28, 125–132. [Google Scholar] [CrossRef]
- Caccianiga, G.; Rey, G.; Baldoni, M.; Caccianiga, P.; Baldoni, A.; Ceraulo, S. Periodontal Decontamination Induced by Light and Not by Heat: Comparison between Oxygen High Level Laser Therapy (OHLLT) and LANAP. Appl. Sci. 2021, 11, 4629. [Google Scholar] [CrossRef]
- Caccianiga, G.; Rey, G.; Caccianiga, P.; Leonida, A.; Baldoni, M.; Baldoni, A.; Ceraulo, S. Rough Dental Implant Surfaces and Peri-Implantitis: Role of Phase- Contrast Microscopy, Laser Protocols, and Modified Home Oral Hygiene in Maintenance. A 10-Year Retrospective Study. Appl. Sci. 2021, 11, 4985. [Google Scholar] [CrossRef]
- Caccianiga, G.; Rey, G.; Caccianiga, P.; Leonida, A.; Baldoni, M.; Baldoni, A.; Ceraulo, S. Peri-Implantitis Management: Surgical versus Non-Surgical Approach Using Photodynamic Therapy Combined with Hydrogen Peroxide (OHLLT—Oxygen High Level Laser Therapy). A Retrospective Controlled Study. Appl. Sci. 2021, 11, 5073. [Google Scholar] [CrossRef]
- Caccianiga, G.; Rey, G.; Caccianiga, P.; Leonida, A.; Baldoni, M.; Baldoni, A.; Ceraulo, S. Laser Management of Peri-Implantitis: A Comparison between Photodynamic Therapy Combined with Hydrogen Peroxide (OHLLT) and OHLLT + Er:YAG Laser. A Retrospective Controlled Study. Appl. Sci. 2021, 11, 6771. [Google Scholar] [CrossRef]
- Seka, W.; Featherstone, J.D.B.; Fried, D.; Visuri, S.R.; Walsh, J.T. Laser ablation of dental hard tissues from explosive ablation to plasma mediate ablation. In Lasers in Dentistry II.; SPIE: Bellingham, WA, USA, 1996; Volume 2672, pp. 144–158. [Google Scholar]
- Adell, R.; Lekholm, U.; Rockler, B.R.; Brånemark, P.I. A study of osseointegrated implants in the treatment of the edentulous jaws. Int. J. Oral Surg. 1981, 6, 387–399. [Google Scholar] [CrossRef]
- Buser, D.; Martin, W.; Belser, U.C. Optimizing esthetics for implant restorations in the anterior maxilla: Anatomic and surgical considerations. Int. J. Oral Maxillofac. Implant. 2004, 19, 43–61. [Google Scholar]
- Evans, C.D.; Chen, S.T. Esthetic outcomes of immediate implant placements. Clin. Oral Implant. Res. 2008, 19, 73–80. [Google Scholar] [CrossRef]
- Alsaadi, G.; Quirynen, M.; Komárek, A.; Van Steenberghe, D. Impact of local and systemic factors on the incidence of late oral implant loss. Clin. Oral Implant. Res. 2008, 19, 670–676. [Google Scholar]
- Berglundh, T.; Lindhe, J. Dimension of the periimplant mucosa. Biological width revisited. J Clin Periodontol. 1996, 23, 971–973. [Google Scholar] [CrossRef] [PubMed]
- Brägger, U.; Karoussis, I.; Persson, R.; Pjetursson, B.; Salvi, G.; Lang, N. Technical and biological complications/failures with single crowns and fixed partial dentures on implants: A 10-year prospective cohort study. Clin. Oral Implants Res. 2005, 16, 326. [Google Scholar] [CrossRef] [PubMed]
- Etter, T.H.; Håkanson, I.; Lang, N.P.; Trejo, P.M.; Caffesse, R.G. Healing after standardized clinical probing of the perlimplant soft tissue seal: A histomorphometric study in dogs. Clin Oral Implants Res. 2002, 13, 571–580. [Google Scholar] [CrossRef] [PubMed]
- Evian, C.I.; Emling, R.; Rosenberg, E.S.; Waasdorp, J.A.; Halpern, W.; Shah, S.; Garcia, M. Retrospective analysis of implant survival and the influence of periodontal disease and immediate placement on long-term results. Int. J. Oral Maxillofac. Implant. 2004, 19, 393–398. [Google Scholar]
- Caccianiga, G.; Caccianiga, P.; Baldoni, M.; Lo Giudice, A.; Perillo, L.; Moretti, N.; Ceraulo, S. Pain Reduction during Rapid Palatal Expansion Due to LED Photobiomodulation Irradiation: A Randomized Clinical Trial. Life 2022, 12, 37. [Google Scholar] [CrossRef]
- Lo Giudice, A.; Nucera, R.; Leonardi, R.; Paiusco, A.; Baldoni, M.; Caccianiga, G. A Comparative Assessment of the Efficiency of Orthodontic Treatment With and Without Photobiomodulation During Mandibular Decrowding in Young Subjects: A Single-Center, Single-Blind Randomized Controlled Trial. Photobiomodulation Photomed. Laser Surg. 2020, 38, 272–279. [Google Scholar] [CrossRef] [Green Version]
- Caccianiga, G.; Rey, G.; Baldoni, M.; Caccianiga, P.; Porcaro, G.; Baldoni, A.; Ceraulo, S. Laser Decontamination and LED Photobiomodulation Promote Bone Regeneration and Wound Healing by Secondary Intention, in Alveolar Ridge Preservation-Clinical and Radiographic Evaluation: A Pilot Experience. Photobiomodulation Photomed. Laser Surg. 2022, 40, 343–354. [Google Scholar] [CrossRef]








Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Caccianiga, G.; Ferri, L.; Baldoni, M.; Bader, A.A.; Caccianiga, P. Magnetic Mallet and Laser for a Minimally Invasive Implantology: A Full Arch Case Report. Appl. Sci. 2022, 12, 9995. https://doi.org/10.3390/app12199995
Caccianiga G, Ferri L, Baldoni M, Bader AA, Caccianiga P. Magnetic Mallet and Laser for a Minimally Invasive Implantology: A Full Arch Case Report. Applied Sciences. 2022; 12(19):9995. https://doi.org/10.3390/app12199995
Chicago/Turabian StyleCaccianiga, Gianluigi, Lorenzo Ferri, Marco Baldoni, Ayt Alla Bader, and Paolo Caccianiga. 2022. "Magnetic Mallet and Laser for a Minimally Invasive Implantology: A Full Arch Case Report" Applied Sciences 12, no. 19: 9995. https://doi.org/10.3390/app12199995
APA StyleCaccianiga, G., Ferri, L., Baldoni, M., Bader, A. A., & Caccianiga, P. (2022). Magnetic Mallet and Laser for a Minimally Invasive Implantology: A Full Arch Case Report. Applied Sciences, 12(19), 9995. https://doi.org/10.3390/app12199995








