Featured Application
This work allows clinicians to better understand first the colour properties of different resin luting agents and, secondly, their behaviour towards different curing protocols.
Abstract
The colour properties of resin luting agents (RLAs) can influence the aesthetic of an indirect restoration. This in vitro study aims to evaluate the colour stability and translucency of RLAs cured using two different protocols by means of a spectrophotometer. Six RLAs were investigated: Enamel Plus Flow (MF), Enamel Plus (MH), light-cure Nexus Third Generation (NX3L), dual-cure Nexus Third Generation (NX3D), RelyX Veneer (RXL) and RelyX Ultimate (RXD). The samples were randomly divided into two groups (n = 5) according to the curing protocol used: the traditional protocol (P1), in which the samples were cured for 40 s, and the step luting protocol (P2), in which samples were cured for 5 s. Then, after 20 s, they were cured again for an additional 40 s. Colour changes and differences in translucency were calculated before (t0) and 1 day (t1) and 7 days (t7) after immersion of the samples in distilled water. Data were analysed using one-way ANOVA, Tukey’s test for multiple comparisons and a t-test for paired comparisons (α = 0.05). The colour and translucency of the RLAs changed between t0 and t7 (p < 0.05). In particular, only RXD showed a visually perceptible difference in colour and translucency between P1 and P2 (p = 0.00). The results of this study suggest that, except for RXD, the curing protocol does not affect the colour or translucency of the tested RLAs, even if all these materials underwent perceptible changes in colour and translucency.
1. Introduction
Modern restorative dentistry is based on the capability of resin-based materials (RBMs) to bond dental tissues. RBMs allow reconstructing dental tissues lost due to trauma, erosion or dental caries by a simple adhesive and minimally invasive procedures. In particular, in the case of endodontically treated [1,2] and structurally compromised teeth, an indirect restoration is required to re-establish their functionality and aesthetics [3]. Indirect restorations can be made of different materials and thicknesses, and they are bonded to dental substrates using RBMs, or the so-called resin luting agent (RLA) [4,5]. RLAs can be divided into two categories: traditional flowable resin-based composites and resin cements [6]. The latter can be divided into light-, self- or dual-cure according to the curing procedure, their monomers and formulation. Following the concept of minimally invasive dentistry, tooth preparation for an indirect restoration aims to save as much dental tissue as possible. This type of preparation often requires a supragingival margin, and consequently, it may affect the aesthetic result of the indirect restoration, mainly on the buccal and lingual sides. Therefore, in the area of the preparation margin, which is often visible, three different substrates can be identified, each with its own colour properties: the dental tissue, the material that constitutes the indirect restoration and the RLA.
Clinically, the colour of the dental tissue and the material of the indirect restoration are often checked and decided following a colour shade guide or a dental photograph, while the colour of the RLA is rarely checked or evaluated previously. Different try-in gels were proposed from the manufacturer to check the colour of the RLA, but they might not match their final colour after curing [7]. Although the thickness of the cement layer is around 40 µm [8], the choice of the exact colour of the RLA can be fundamental to hiding the preparation margin and “linking” the colour of the indirect restoration to the surrounding dental tissues.
The colour of an object can be recorded by a spectrophotometer and described using the parameters expressed by the Commission Internationale d’Eclairage (CIE), namely with the CIELab and CIELCh systems [9,10]. These systems allow one to calculate both ΔE, which quantifies the difference between two colours, and the translucency, which describes the behaviour of an object for transmitting or diffusing light. Translucency has been emphasised as one of the most important properties of RBMs, since it favours the mimesis of the material with the surrounding dental tissues [11,12]. Translucency can be calculated using the translucency parameter (TP) and contrast ratio. These values are highly correlated and can be used interchangeably [13,14].
The colour and translucency of all RBMs can change over time due to several factors, including storage in water, chemical initiators (such as tertiary amine, benzoyl peroxide or camphorquinone) and the curing protocol [13,15]. In clinical practice, RLAs undergo the curing process, which can influence the chemical and physical properties, including colour and translucency [16]. Both light and dual-cure RLAs can be cured with different protocols, such as the traditional or step luting protocols [17]. The traditional curing protocol involves the polymerisation of RLAs in a single step. Instead, the step luting protocol consists of curing the RLA for 5 s, waiting around 20 s to remove excesses due to the indirect restoration placement, and curing again. The 5-s step allows the easy removal of excesses thanks to the gel phase of RLAs, in which the materials are still soft [17].
Some studies evaluated the colour and translucency of RLAs along with indirect restorations [4,18], but there is no research on the evaluation of RLAs alone. In addition, although the effect of the step luting protocol on the degree of conversion was estimated, no study described its effect on the colour properties. For this reason, the aim of this study was to evaluate the effect of the traditional and step luting protocols on the colour stability and translucency of different RLAs after storage in water.
The null hypotheses were that (1) there were no colour differences when using both curing protocols after 7 days of storage in water, and (2) there were no translucency differences when using both curing protocols after 7 days of storage in water.
2. Materials and Methods
A total of six different RLAs were investigated: the light-cure Nexus Third Generation (NX3L) (Kerr, Orange, CA, USA), dual-cure Nexus Third Generation (NX3D) (Kerr, Orange, CA, USA), light-cure RelyX Veneer (RXL) (3M ESPE, St. Paul, MN, USA), dual-cure RelyX Ultimate (RXD) (3M ESPE, St. Paul, MN, USA), light-cure Enamel Plus HRi Flow (MF) (Micerium, Genova, Italy) and preheated light-cure Enamel Plus HRi (MH) (Micerium, Genova, Italy). The preheated composite MH was obtained by heating a compule of high-viscosity resin composite for 10 min at 55 °C in an Ena Heat composite heater (Micerium, Genova, Italy) by following the manufacturer’s instructions. The compositions of all tested materials are described in Table 1 [17].

Table 1.
Materials used in this study.
For each tested RLA, 10 aliquots of unpolymerised material were withdrawn, placed inside a Teflon ring (0.2 mm in height and a 15.0-mm internal diameter) on a Kaltek glass (1.1-mm thick) and covered by another thin glass (0.2-mm thick), thus obtaining a disk-shaped sample of the material with a diameter of 15.0 mm and a thickness of 0.2 mm. A polymerised composite disk made by Filtek Supreme A3B Plus (3M ESPE, St.Paul, MN) that was 2.0-mm thickn and 25.0 mm in diameter was interposed between the tip of the lamp and the resin cement sample during the curing phases [17].
Then, the samples were randomly divided into two groups (n = 5) according to the curing protocols:
- (1)
- Traditional curing protocol (P1), where the samples were cured for 40 s;
- (2)
- Step luting protocol (P2), where the samples were cured for 5 s and then, after 20 s, cured again for an additional 40 s [17].
In both curing protocols, an Elipar DeepCure S light (3M ESPE, Seefeld, Germany) was adopted with an irradiance of 1470 mW/cm2 ± 20% and a spectrum range between 430 and 480 nm. The colour parameters were recorded by SpectroShade-Micro (MHT S.p.a., Verona, Italy) using the CIELab and CIELCh systems. CIELab consists of the parameters of the lightness (L*), red-green chromatic coordinate (a*) and blue-yellow chromatic coordinate (b*), while CIELCh consists of the parameters of the lightness (L*), chrome (C*) and hue (h*). The colour evaluations were performed 2 weeks after the curing procedures to have the maximum degree of conversion for each RLA [17].
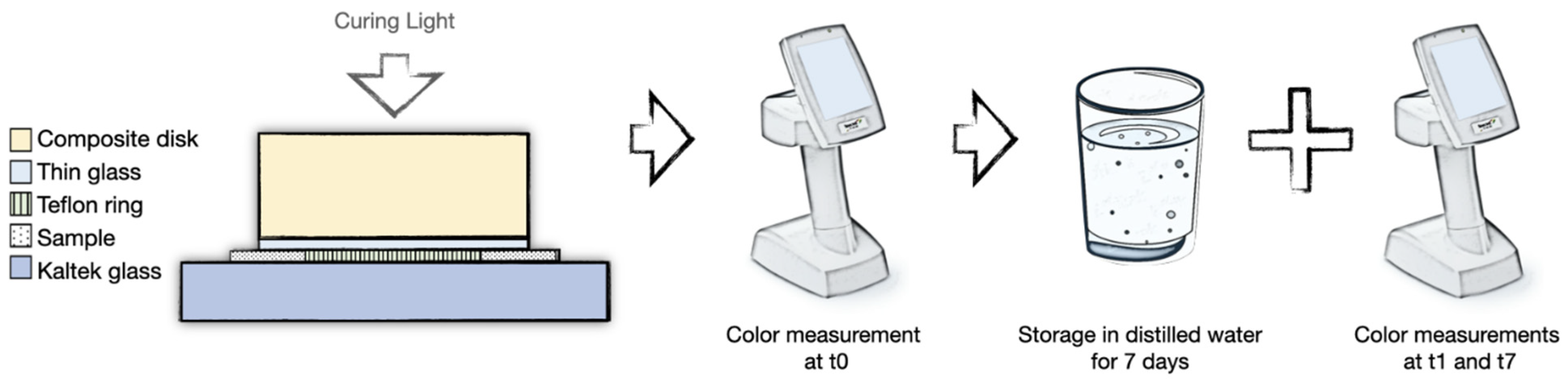
The colour parameters were measured before (t0) and 1 day (t1) and 7 days (t7) after immersion of the samples in distilled water (Figure 1). The colour of each sample was recorded against white (L* = 95.00, a* = −0.07, b* = −4.20) and black (L* = 9.20, a* = 1.47, b* = −3.83) backgrounds. Moreover, each measurement was repeated three times in the centre of each sample without replacement to increase the accuracy. During the experiment, the samples were kept at room temperature, in constant humidity and in the absence of light. The colour variation (ΔE) was calculated using CIELab values on a white background:
ΔE(t0/t1)* = [(Lt0 * − Lt1 *)2 + (at0 * − at1 *)2 + (bt0 * − bt1 *)2]1/2
ΔE(t0/t7)* = [(Lt0 * − Lt7 *)2 + (at0 * − at7 *)2 + (bt0 * − bt7 *)2]1/2
ΔE(P1/P2)* = [(LP1 * − LP2 *)2 + (aP1 * − aP2 *)2 + (bP1 * − bP2 *)2]1/2

Figure 1.
The methodological process followed in the study. Colour parameters were measured before (t0) and 1 day (t1) and 7 days (t7) after immersion of samples in distilled water.
In this study, the perceptibility threshold for colour differences (PTC) was set to 1.2 [19].
The translucency was evaluated using the comparative translucency parameter (TPc), since the backgrounds used during the measurements of the colour parameters were different from the ideal backgrounds (ideal white background, L = 94.3, a = −0.4, b = −0.6; ideal black background, L = 0.2, a = 0.4, b = −0.6) [20]. TPc was calculated as follows:
TPc = ΔE*wb/ΔE backgrounds
The TPc of each specimen was obtained by calculating the colour difference (ΔE*wb) of the sample against black (“s. on black” in the formula) and white backgrounds (“s. on white” in the formula) and dividing it into the colour difference between the black and white backgrounds (ΔE*backgrounds) according to the following formulas [20,21,22]:
ΔE*wb = [(Ls. on black * − Ls. on white*)2 + (as. on black * − as. on white *)2 + (bs. on black * − bs. on white *)2]1/2
ΔE*backgrounds = [(Lblack * − Lwhite *)2 + (ablack * − awhite *)2 + (bblack * − bwhite *)2]1/2
Then, to assess the difference in translucency between the samples at t0 and at t7, ΔTP was calculated as follows [21]:
ΔTPc (t0/t7) = TPc (t0) − TPc (t7)
To evaluate the difference in translucency between P1 and P2, ΔTPc was calculated as follows:
ΔTPc (P1/P2) = TPc (P1) − TPc (P2)
In this study, the perceptibility threshold for translucency differences (PTT) was set to 0.023.
Statistical Analysis
The sample size calculation was performed by considering the preliminary results for ΔE(t0/t7)* with the tested RLAs. An acceptability threshold of 0.5 was used as the minimum detectable difference between the means, and 0.23 was the mean standard deviation. The significance level (alpha) of the test was set to 0.05, and the power (1–β) was set to 80%. After homogeneity and normality evaluations, one-way analysis of variance (ANOVA) and the post hoc Tukey’s HSD test were used for the statistical comparison (α = 0.05). A paired t-test was conducted to examine the colours between the curing protocols. Statistical analysis was performed with R Project for Statistical Computing 4.2.0 [13] and Microsoft Excel 2013 (Microsoft, Washington, DC, USA).
3. Results
The results of CIELCh on a white background are shown in Table 2.

Table 2.
CIELCh parameters of the tested resin luting agents cured with traditional curing protocol (P1) and step luting protocol (P2). L*, C* and h* values are expressed as means (standard deviation), and they were recorded on white background before (t0) and after 7 days (t7) of storage in water.
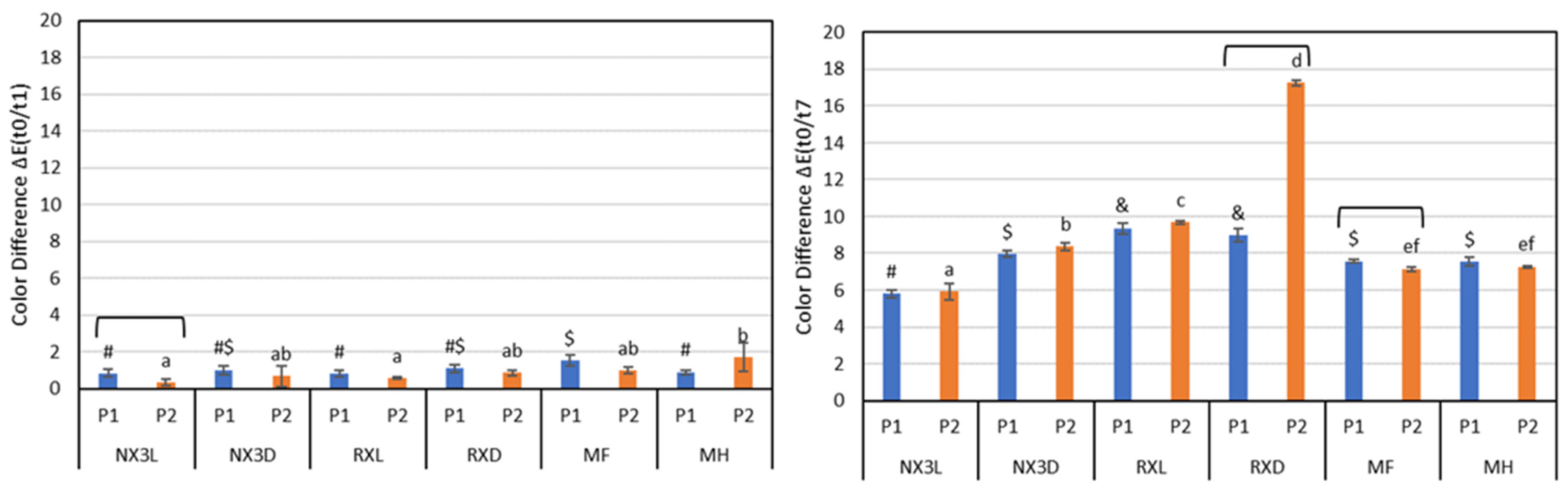
Regarding ΔE, the results are shown in Figure 2. At t1, MF(P1) and MH(P2) achieved the highest ΔE(t0/t1), but only NX3L showed a colour difference between P1 and P2 (p = 0.04). At t7, the ΔE(t0/t7) values of each tested RLA were different from the ΔE(t0/t1) ones. In particular, RXL and RXD showed the highest ΔE(t0/t7) both in P1 and P2. RXD and MF showed different ΔE(t0/t7) values in P1 and P2 (RXD, p = 0.00; MF, p = 0.00), but only RXD was above the PTC (RXD = 17.964 ± 0.318; MF = 0.640 ± 0.107), while only ΔE(t0/t1) of MF (P1) and MH (P2) exceeded the PTC, and the ΔE(t0/t7) values for each RLA were above this value. Then, all RLAs tested changed the colour after 7 days of storage in water (p < 0.05).
Figure 2.
ΔE(t0/t1) and ΔE(t0/t7) results of tested resin luting agents cured with traditional curing protocol (P1) and step luting protocol (P2). Different letters identify statistical differences between P1 groups. Different symbols (#, $ and &) identify statistical differences between P2 groups. Bars identify a statistical difference between P1 and P2 (p < 0.05). NX3L = NX3 light-cure, NX3D = NX3 dual-cure, RXL = RelyX Veneer, RXD = RelyX Ultimate, MF = Enamel Plus HRi Flow, MH = Enamel Plus HRi.
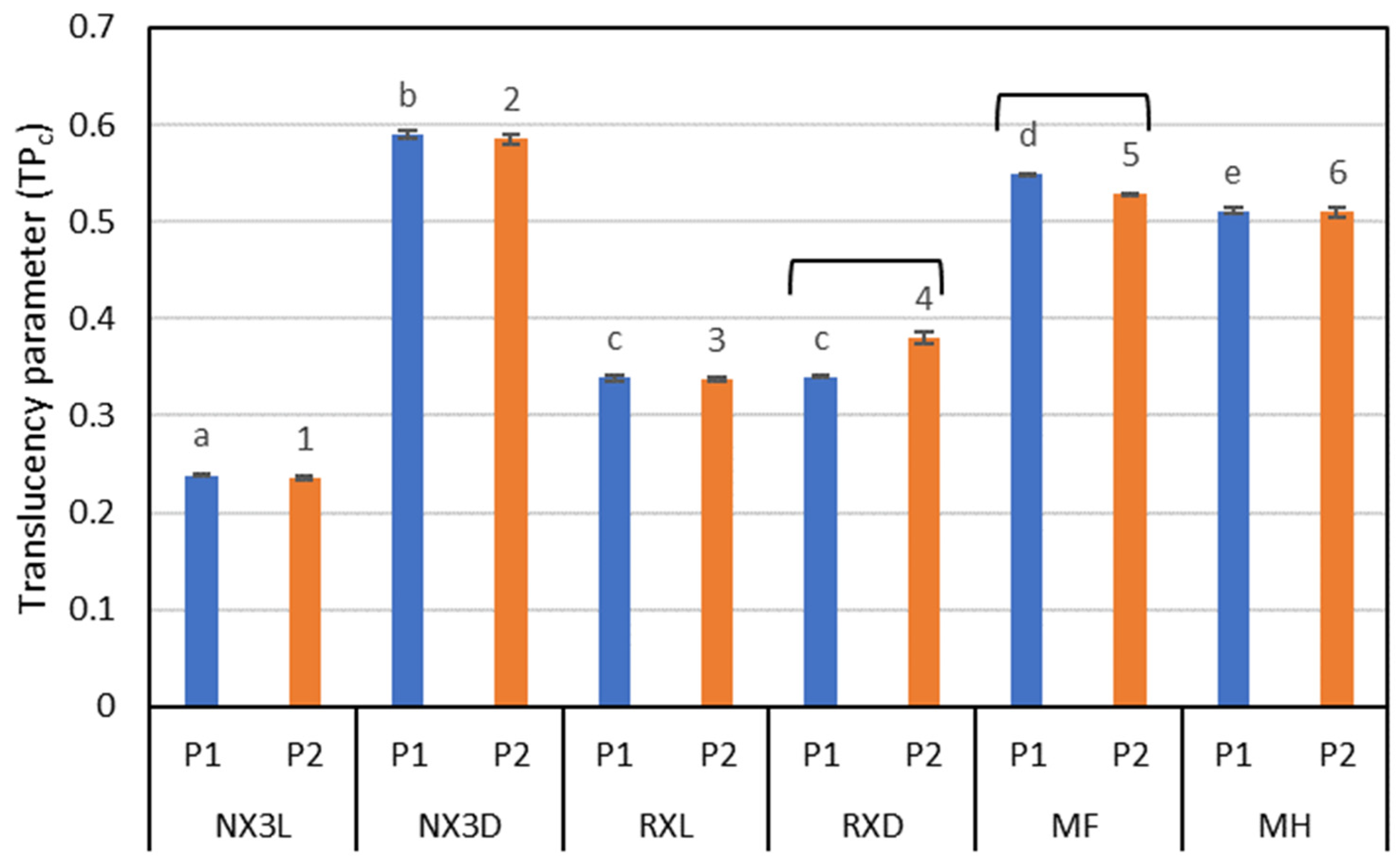
The translucency values are summarised in Table 3. At t1, only MF(P2) showed a different translucency than in t0 (p < 0.05). At t7, the TPc of all RLAs with P1 and P2 changed, except for NX3D (p < 0.05). However, the translucency trend remained the same in both P1 and P2 (NX3L < RXL < RXD < MH < MF < NX3D (opaque < translucent)). Only NX3L (P2), NX3D (P1 and P2) and MH (P1) showed a ΔTPc (t0/7) below the PTT.

Table 3.
Translucency values of the tested resin luting agents cured with the traditional curing protocol (P1) and the step luting protocol (P2) before (t0) and 1 day (t1) and 7 days (t7) of storage in water. ΔTP (t0/t7) describes the difference between translucency value of t0 and t7. Values are expressed as means (standard deviation). Different superscript letters identify statistical differences between groups at the same time point. Different superscript numbers identify differences between each time point (p < 0.05), while * identifies a ΔTP (t0/t7) higher than the perceivable translucency threshold value ± 0.023.
Although RXD and MF reported different TPc values between protocols (both p = 0.00) (Figure 3), only ΔTPc (P1/P2) of RXD exceeded the PTT (RXD = −0.039 ± 0.006; MF = 0.020 ± 0.001).

Figure 3.
Translucency parameter (TPc) values after 7 days of storage in water. Different letters identify statistical differences between P1 groups. Different numbers identify statistical differences between P2 groups. Bars identify a statistical difference between P1 and P2 (p < 0.05). NX3L = NX3 light-cure, NX3D = NX3 dual-cure, RXL = RelyX Veneer, RXD = RelyX Ultimate, MF = Enamel Plus HRi Flow, MH = Enamel Plus HRi.
4. Discussion
Nowadays, the bonding procedures of indirect restorations have been simplified by introducing not only new materials but also new curing protocols. Clinically, although both the traditional and step luting protocols can be used to cement indirect restorations, more and more practitioners use the step luting protocol because it allows easy removal of material excesses without compromising chemical stability [17,23,24]. However, in addition to the chemical and physical properties, other factors can influence the longevity of indirect restorations, some of which are related to the colour stability and translucency of RLAs [25].
In this study, the colours of all RLAs changed after 7 days of storage in water. Differences between P1 and P2 were only detected in RXD and MF. For this reason, the first null hypothesis was partially rejected. The translucency of all RLAs also changed after 7 days of storage in water, except for NX3D. However, although the RLA translucency grading remained the same for both curing protocols, only RXD and MF showed differences between P1 and P2. Therefore, the second null hypothesis was also partially rejected.
In this study, colour was measured using CIELab and CIELCh. These systems allowed describing the colour in an objective manner, achieving a quantitative and reproducible method to determine any colour or translucency changes [26]. According to Paravina et al., the PTC considered in this study was set to 1.2 [19]. As for the translucency, since we used the comparative TP calculation method, the PTT was calculated by dividing the perceptible threshold determined with ideal backgrounds (ΔTP = 2) by the colour difference between the white and black backgrounds used during the measurements [21]. Thus, the final PTT was 0.023.
Colour changes can occur in RBMs—and consequently in RLAs—as a result of intrinsic factors such as the resin matrix, fillers [27], incomplete polymerisation [28] and intrinsic factors [29]. The colour variation of the tested RLAs can be explained by the presence in the resin matrix of diketones used as polymerisation initiators which remain inactivated inside the material [30]. Another explanation could be the higher proportion of filler–matrix interface and the presence of multiple matrices, which can cause hydrolytic instability of the silane bond between the fillers and matrix, provoking the detachment of the filler content and the changes in lightness. In fact, the oxidation reactions of the unreacted double bonds of C=C, due to the presence of water, produce coloured peroxide products, which can provoke the colour variation [31]. Regarding the intrinsic factors, dual-cured RLAs contain tertiary amine (aromatic amine) and benzoyl peroxide, both of which tend to darken over time [29]. In addition, the remaining unreacted benzoyl peroxide or amine leads to the discolouration of RLAs. In contrast, the colour of the camphorquinone photo-initiator and aliphatic amine that are commonly incorporated in the composition of light-cured RLAs is more stable [32].
In this study, ΔE allowed us to describe the colour difference and colour stability of the RLAs, but since the RLAs are clinically used at a thin thickness, their final aspects could also be affected by the translucency [18]. The importance of the translucency of RLAs was highlighted by Perroni et al., concluding that an RLA’s translucency affects the final shade of indirect restorations, particularly in veneers [18]. Basically, RLAs are optically translucent due to their structure, which is composed of a highly transparent matrix and small filler particles. The translucency of RBMs is generally determined by a relationship between the resin matrix and the refractive indices of their filler particles. Although Mitra et al. showed a relationship between translucency and the amount of filler content [33], different parameters can affect the translucency, such as the content, type and size of filler particles, composition of the resin matrix and its fraction, application thickness of the material, light-curing mode, photo initiators and filler coupling agents, pigment additives and opacifying agents [34,35].
The different behaviour of ΔTP (t0/t7) could be due to the water intake of the polymerisation initiators from both the matrix and the unpolymerised chamber, increasing the water inside the resin and modifying the refraction and diffusion index of the matrix. Monomers can also influence the translucency. For example, urethandimethacrylate is a less hydrophilic monomer compared with triethylene glycol dimethacrylate (TEGDMA) and bisphenol-A glycidyl dimethacrylate (BIS-GMA) [36,37]. In fact, Kalachandra and Turner reported that the water uptake in BIS-GMA-based resin materials increased from 3% to 6% as the proportion of TEGDMA increased from 0% to 1%, respectively [38]. For this reason, RLAs containing TEGDMA or BIS-GMA, such as MF and MH, were more susceptible to TP changes after storage in water. Only NX3D showed no differences between t0 and t1. This behaviour of NX3D can be explained by the colour stabilisers claimed by the manufacturer. Among the tested materials, the curing protocol affected the colour stability and the translucency of only MF and RXD. Since the knowledge of all ingredients was not available, the authors can speculate that the step luting protocol made MF and RXD instable, provoking the leakage of its ingredients, such as monomers, fillers and pigments, which are all involved in establishing the colour and translucency properties. Moreover, based on a previous study, the TPc values of healthy dentin and enamel are around 0.28 and 0.24, respectively [39]. Then, among the tested RLAs, NX3L (P1 and P2) showed the closest values to the sound dental tissue.
The limitation of this study might be the use of distilled water and the evaluation of the colour and translucency of RLAs alone without considering the influence of the indirect restoration. Regarding the use of distilled water compared to saliva, while the mechanical behaviour of RBMs might be influenced by the use of one of these solutions, no difference was reported for spectrophotometric evaluations [40]. Erdemir et al. also utilised distilled water as the control group instead of artificial saliva in a study in which they evaluated the colour of different RBMs [41]. Aside from that, Omata et al. concluded that immersion in artificial saliva may cause a biased colour due to its artificial components [42]. Regarding the absence of indirect restorations during the colour measurements, although many studies tested RLAs along with veneers or overlays [43,44,45], the fact is that studying each RLA alone allows better understanding of its behaviour. Moreover, to the best of the authors’ knowledge, no study exists regarding the analysis of RLAs alone after water sorption and using different protocols. In addition to water, in the oral cavity, other solutions can influence RLAs. For this reason, further studies will investigate the influence of the different curing protocols on the staining capability of agents such as tea, cola or coffee.
For carefully translating the results of this in vitro study into clinical practice, it is possible to emphasise that all the tested RLAs changed their colour and translucency after 7 days of storage in water. Moreover, since we used RLAs that were completely cured and not immediately after the curing procedures [17], the translucency and colour changes could be even more visually perceptible in clinical practice. Hence, to establish the exact colours of these RLAs and have a preview of the exact final colour, it may be helpful to create one’s own hydrated shade guide [46] using cured, hydrated RLAs, and using one’s personally chosen cure protocol.
5. Conclusions
This study aimed to evaluate the effect of the traditional and step luting protocols on the colour stability and translucency of different RLAs.
Within the limitations of this study, all tested RLAs changed their colours perceptibly after 7 days of storage in water. The curing protocols influenced the colour perceptibly only for RXD. The translucency of the tested RLAs changed over time and, for both curing protocols, they maintained the same order, from more opaque to more translucent: NX3L < RXL < RXD < MH < MF < NX3D. The curing protocols influenced the translucency perceptibly only for RXD.
This study represents the first attempt to evaluate the colour and translucency changes of luting agents without considering the materials that constitute the indirect restoration and also evaluating the effect of the step luting protocol. Noteworthy, clinicians should be aware of the colour instability of RXD. These results can help clinicians to choose the right RLA based on both its colour and translucency properties and the curing protocol selected.
Author Contributions
Conceptualisation, R.M., A.P. and G.O.; methodology, R.M. and F.V.; software, R.B.; validation, R.M., F.V. and V.T.; formal analysis, V.T. and R.B.; investigation, R.M., F.V. and V.T.; resources, V.T., R.B. and G.O.; data curation, R.M. and F.V.; writing—original draft preparation, R.M. and F.V.; writing—review and editing, R.M., A.P. and G.O.; visualisation, R.M.; supervision, A.P. and G.O. project administration, A.P. and G.O. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Iandolo, A.; Abdellatif, D.; Pantaleo, G.; Sammartino, P.; Amato, A. Conservative Shaping Combined with Three-Dimensional Cleaning Can Be a Powerful Tool: Case Series. J. Conserv. Dent. 2020, 23, 648–652. [Google Scholar] [CrossRef] [PubMed]
- Iandolo, A.; Amato, A.; Martina, S.; Abdel latif, D.; Pantaleo, G. Management of Severe Curvatures in Root Canal Treatment with the New Generation of Rotating Files Using a Safe and Predictable Protocol. Open Dent. J. 2020, 14, 421–425. [Google Scholar] [CrossRef]
- Hardan, L.; Mancino, D.; Bourgi, R.; Cuevas-Suárez, C.E.; Lukomska-Szymanska, M.; Zarow, M.; Jakubowicz, N.; Zamarripa-Calderón, J.E.; Kafa, L.; Etienne, O.; et al. Treatment of Tooth Wear Using Direct or Indirect Restorations: A Systematic Review of Clinical Studies. Bioengineering 2022, 9, 346. [Google Scholar] [CrossRef] [PubMed]
- Turgut, S.; Bagis, B. Effect of Resin Cement and Ceramic Thickness on Final Color of Laminate Veneers: An in Vitro Study. J. Prosthet. Dent. 2013, 109, 179–186. [Google Scholar] [CrossRef]
- D’Addazio, G.; Santilli, M.; Rollo, M.L.; Cardelli, P.; Rexhepi, I.; Murmura, G.; Al-Haj Husain, N.; Sinjari, B.; Traini, T.; Özcan, M.; et al. Fracture Resistance of Zirconia-Reinforced Lithium Silicate Ceramic Crowns Cemented with Conventional or Adhesive Systems: An In Vitro Study. Materials 2020, 13, 2012. [Google Scholar] [CrossRef]
- Lise, D.P.; Van Ende, A.; De Munck, J.; Yoshihara, K.; Nagaoka, N.; Cardoso Vieira, L.C.; Van Meerbeek, B. Light Irradiance through Novel CAD–CAM Block Materials and Degree of Conversion of Composite Cements. Dent. Mater. 2018, 34, 296–305. [Google Scholar] [CrossRef]
- Alghazali, N.; Moaleem, M.; Alamri, S.; Aldosari, A.A.; Preston, A.; Smith, P.; Jarad, F. The Effect of Try-In Paste and Resin Cement Shade on Colour Properties of Dental Veneers. Eur. J. Prosthodont. Restor. Dent. 2018, 26, 144–151. [Google Scholar] [CrossRef]
- White, S.N.; Yu, Z. Film Thickness of New Adhesive Luting Agents. J. Prosthet. Dent. 1992, 67, 782–785. [Google Scholar] [CrossRef]
- Joiner, A.; Luo, W. Tooth Colour and Whiteness: A Review. J. Dent. 2017, 67, S3–S10. [Google Scholar] [CrossRef]
- Kury, M.; Perches, C.; da Silva, D.P.; André, C.B.; Tabchoury, C.P.M.; Giannini, M.; Cavalli, V. Color Change, Diffusion of Hydrogen Peroxide, and Enamel Morphology after in-Office Bleaching with Violet Light or Nonthermal Atmospheric Plasma: An in Vitro Study. J. Esthet. Restor. Dent. 2020, 32, 102–112. [Google Scholar] [CrossRef]
- Winter, R. Visualizing the Natural Dentition. J. Esthet. Dent. 1993, 5, 102–117. [Google Scholar] [CrossRef] [PubMed]
- Yu, B.; Ahn, J.-S.; Lee, Y.-K. Measurement of Translucency of Tooth Enamel and Dentin. Acta Odontol. Scand. 2009, 67, 57–64. [Google Scholar] [CrossRef] [PubMed]
- Bagheri, R.; Burrow, M.F.; Tyas, M. Influence of Food-Simulating Solutions and Surface Finish on Susceptibility to Staining of Aesthetic Restorative Materials. J. Dent. 2005, 33, 389–398. [Google Scholar] [CrossRef]
- Yu, B.; Lee, Y.-K. Translucency of Varied Brand and Shade of Resin Composites. Am. J. Dent. 2008, 21, 229–232. [Google Scholar] [PubMed]
- Fontes, S.T.; Fernández, M.R.; de Moura, C.M.; Meireles, S.S. Color Stability of a Nanofill Composite: Effect of Different Immersion Media. J. Appl. Oral. Sci. 2009, 17, 388–391. [Google Scholar] [CrossRef] [PubMed]
- Kim, I.-J.; Lee, Y.-K. Changes in Color and Color Parameters of Dental Resin Composites after Polymerization. J. Biomed. Mater. Res. B Appl. Biomater. 2007, 80, 541–546. [Google Scholar] [CrossRef]
- Tosco, V.; Monterubbianesi, R.; Orilisi, G.; Sabbatini, S.; Conti, C.; Özcan, M.; Putignano, A.; Orsini, G. Comparison of Two Curing Protocols during Adhesive Cementation: Can the Step Luting Technique Supersede the Traditional One? Odontology 2021, 109, 433–439. [Google Scholar] [CrossRef]
- Perroni, A.P.; Kaizer, M.R.; Della Bona, A.; Moraes, R.R.; Boscato, N. Influence of Light-Cured Luting Agents and Associated Factors on the Color of Ceramic Laminate Veneers: A Systematic Review of in Vitro Studies. Dent. Mater. 2018, 34, 1610–1624. [Google Scholar] [CrossRef]
- Paravina, R.D.; Ghinea, R.; Herrera, L.J.; Bona, A.D.; Igiel, C.; Linninger, M.; Sakai, M.; Takahashi, H.; Tashkandi, E.; del Mar Perez, M. Color Difference Thresholds in Dentistry. J. Esthet. Restor. Dent. 2015, 27, S1–S9. [Google Scholar] [CrossRef]
- Lee, Y.-K. Criteria for Clinical Translucency Evaluation of Direct Esthetic Restorative Materials. Restor. Dent. Endod. 2016, 41, 159–166. [Google Scholar] [CrossRef]
- Balci, M.; Ergucu, Z.; Çelik, E.U.; Turkun, L.S. Comparison between Translucencies of Anterior Resin Composites and Natural Dental Tissues. Color Res. Appl. 2021, 46, 635–644. [Google Scholar] [CrossRef]
- Babina, K.; Turkina, A.; Sokhova, I.; Budina, T.; Makeeva, M. Comparative Assessment of Various Composite Materials and Natural Tooth Tissue Translucencies. Int. J. Esthet. Dent. 2019, 14, 406–419. [Google Scholar] [PubMed]
- Abduo, J.; Sambrook, R.J. Longevity of Ceramic Onlays: A Systematic Review. J. Esthet. Restor. Dent. 2018, 30, 193–215. [Google Scholar] [CrossRef] [PubMed]
- Giorgini, E.; Sabbatini, S.; Conti, C.; Rubini, C.; Rocchetti, R.; Fioroni, M.; Memè, L.; Orilisi, G. Fourier Transform Infrared Imaging Analysis of Dental Pulp Inflammatory Diseases. Oral Dis. 2017, 23, 484–491. [Google Scholar] [CrossRef]
- Mangani, F.; Marini, S.; Barabanti, N.; Preti, A.; Cerutti, A. The Success of Indirect Restorations in Posterior Teeth: A Systematic Review of the Literature. Minerva Stomatol. 2015, 64, 231–240. [Google Scholar]
- Gómez-Polo, C.; Muñoz, M.P.; Lorenzo Luengo, M.C.; Vicente, P.; Galindo, P.; Martín Casado, A.M. Comparison of the CIELab and CIEDE2000 Color Difference Formulas. J. Prosthet. Dent. 2016, 115, 65–70. [Google Scholar] [CrossRef]
- Vichi, A.; Ferrari, M.; Davidson, C.L. Color and Opacity Variations in Three Different Resin-Based Composite Products after Water Aging. Dent. Mater. 2004, 20, 530–534. [Google Scholar] [CrossRef]
- Janda, R.; Roulet, J.-F.; Kaminsky, M.; Steffin, G.; Latta, M. Color Stability of Resin Matrix Restorative Materials as a Function of the Method of Light Activation. Eur. J. Oral Sci. 2004, 112, 280–285. [Google Scholar] [CrossRef]
- Saati, K.; Valizadeh, S.; Anaraki, S.N.; Moosavi, N. Effect of Aging on Color Stability of Amine-Free Resin Cement through the Ceramic Laminate Veneer. Dent. Res. J. 2021, 18, 99. [Google Scholar] [CrossRef]
- de Oliveira, D.C.R.S.; Rocha, M.G.; Gatti, A.; Correr, A.B.; Ferracane, J.L.; Sinhoret, M.A.C. Effect of Different Photoinitiators and Reducing Agents on Cure Efficiency and Color Stability of Resin-Based Composites Using Different LED Wavelengths. J. Dent. 2015, 43, 1565–1572. [Google Scholar] [CrossRef]
- Ferracane, J.L.; Moser, J.B.; Greener, E.H. Ultraviolet Light-Induced Yellowing of Dental Restorative Resins. J. Prosthet. Dent. 1985, 54, 483–487. [Google Scholar] [CrossRef]
- Alkurt, M.; Duymus, Z.Y. Comparison to Color Stability Between Amine with Benzoyl Peroxide Includes Resin Cement and Amine-Reduced, Amine-Free, Lacking of Benzoyl Peroxide Resin Cements After Thermocycle. J. Adv. Oral Res. 2018, 9, 24–30. [Google Scholar] [CrossRef]
- Felippe, L.A.; Monteiro, S.; De Andrada, C.A.C.; Di Cerqueira, A.D.; Ritter, A.V. Clinical Strategies for Success in Proximoincisal Composite Restorations. Part I: Understanding Color and Composite Selection. J. Esthet. Restor. Dent. 2004, 16, 336–347. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.-K. Influence of Filler on the Difference between the Transmitted and Reflected Colors of Experimental Resin Composites. Dent. Mater. 2008, 24, 1243–1247. [Google Scholar] [CrossRef] [PubMed]
- Johnston, W.M. Review of Translucency Determinations and Applications to Dental Materials. J. Esthet. Restor. Dent. 2014, 26, 217–223. [Google Scholar] [CrossRef] [PubMed]
- Kugel, G. Direct and Indirect Adhesive Restorative Materials: A Review. Am. J. Dent. 2000, 13, 35D–40D. [Google Scholar]
- Moszner, N.; Fischer, U.K.; Angermann, J.; Rheinberger, V. A Partially Aromatic Urethane Dimethacrylate as a New Substitute for Bis-GMA in Restorative Composites. Dent. Mater. 2008, 24, 694–699. [Google Scholar] [CrossRef]
- Kalachandra, S.; Turner, D.T. Water Sorption of Polymethacrylate Networks: Bis-GMA/TEGDM Copolymers. J. Biomed. Mater. Res. 1987, 21, 329–338. [Google Scholar] [CrossRef]
- Caneppele, T.; Borges, A.; Torres, C. Effects of Dental Bleaching on the Color, Translucency and Fluorescence Properties of Enamel and Dentin. Eur. J. Esthet. Dent. Off. J. Eur. Acad. Esthet. Dent. 2013, 8, 200–212. [Google Scholar]
- Ardu, S.; Gutemberg, D.; Krejci, I.; Feilzer, A.J.; Di Bella, E.; Dietschi, D. Influence of Water Sorption on Resin Composite Color and Color Variation amongst Various Composite Brands with Identical Shade Code: An in Vitro Evaluation. J. Dent. 2011, 39, e37–e44. [Google Scholar] [CrossRef]
- Erdemir, U.; Yildiz, E.; Eren, M.M.; Ozel, S. Surface Hardness Evaluation of Different Composite Resin Materials: Influence of Sports and Energy Drinks Immersion after a Short-Term Period. J. Appl. Oral Sci. 2013, 21, 124–131. [Google Scholar] [CrossRef] [PubMed]
- Omata, Y.; Uno, S.; Nakaoki, Y.; Tanaka, T.; Sano, H.; Yoshida, S.; Sidhu, S.K. Staining of Hybrid Composites with Coffee, Oolong Tea, or Red Wine. Dent. Mater. J. 2006, 25, 125–131. [Google Scholar] [CrossRef] [PubMed]
- Vafaee, F.; Heidari, B.; Khoshhal, M.; Hooshyarfard, A.; Izadi, M.; Shahbazi, A.; Moghimbeigi, A. Effect of Resin Cement Color on the Final Color of Lithium Disilicate All-Ceramic Restorations. J. Dent. 2018, 15, 143–150. [Google Scholar]
- de Azevedo Cubas, G.B.; Camacho, G.B.; Demarco, F.F.; Pereira-Cenci, T. The Effect of Luting Agents and Ceramic Thickness on the Color Variation of Different Ceramics against a Chromatic Background. Eur. J. Dent. 2011, 5, 245–252. [Google Scholar] [CrossRef]
- Barath, V.S.; Faber, F.-J.; Westland, S.; Niedermeier, W. Spectrophotometric Analysis of All-Ceramic Materials and Their Interaction with Luting Agents and Different Backgrounds. Adv. Dent. Res. 2003, 17, 55–60. [Google Scholar] [CrossRef]
- Paolone, G.; Orsini, G.; Manauta, J.; Devoto, W.; Putignano, A. Composite Shade Guides and Color Matching. Int. J. Esthet. Dent. 2014, 9, 164–182. [Google Scholar]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).