1. Introduction
Wrist braces are commonly used for injury rehabilitation. A wrist brace can help accelerate recovery from a wrist fracture. In addition to providing immobilization, a good fit of the brace in the affect area is effective in allowing the wrist to heal. Court-Brown and Caesar found that fractures around the wrist accounted for over 30% of all clinical fracture cases [
1]. Osteoporosis among the aged population increases the chance of fractures, and often, during a fall, the hands are used reflexively to blunt the impact. Wrist-related symptoms, such as compartment syndrome, ligament injuries, and tendinopathy resulting from long-term immobilization of the fingers and wrist at fixed postures, are also common [
2,
3].
Immobilization of the wrist using a plaster cast is effective in fracture rehabilitation, but internal pressure can cause dermatitis, decubitus, nerve paralysis, and compartment syndrome. Due to a plaster cast’s inability to be removed or adjusted easily, the weeks-long recovery may cause ankylosis in the immobilized area. Furthermore, detumescence of the tissue may create a gap between the limb and brace, thereby reducing the immobilization capability and resulting in secondary fractures. Reswick and Rogers measured the pressure over the peri-sacral bony prominences of 980 seated subjects. The tolerance curve they produced confirmed an inverse relationship between the pressure and duration. This indicated that when allowing pressure across the time curve under 50 mmHg, it was possible to avoid complex decubitus syndrome [
4]. Kawamata et al. investigated the magnitude of pressure on the severity of injury and capillary closure in experimental pressure ulcers in rats. Between 60 and 70 mm Hg, repeated compressions for 4 h daily for 5 consecutive days resulted in partial skin necrosis and eschar formation in the majority of rats, whereas at 50 mmHg, skin injuries were absent or very mild in most of the rats [
5].
Commercially available materials for wrist braces were innovated from traditional plaster to thermoplastic casts or splints, and materials were reshaped as fiberglass resin tape or splints. Fiberglass resin can be reshaped and has a shorter curing time than plaster or thermoplastic. However, these materials have similar issues after application: stuffiness, uncomfortable, not ventilated, and difficult to negotiate for dressing. Furthermore, most splints and casts using these materials can only be removed and replaced by professionals. Compared to the thermoplastic cast, the plaster cast achieves better immobility. Fitting and strength are the two main problems associated with using thermoplastic casts.
Thanks to the rapid development of cutting-edge techniques in additive manufacture, also named rapid prototyping, people can turn their imagined creations into a physical reality. Instead of traditional subtractive molds manufacturing in a factory, additive manufacturing by 3D printers has become more and more popular. Due to easy access and easy use of the equipment and materials, one can easily produce 3D printer equipment at home.
As 3D printing has become more mature and ubiquitous, designers armed with open source software have been able to produce braces, from design to final product, even in a home environment [
6]. Patient-specific wrist orthoses fabricated by a 3D printer may perfectly fit the individual’s wrist, unlike commercial orthoses. However, the cost of the materials, scanning, and manufacture time are much higher than that in mass production [
7]. A hybrid design of 3D-printed wrist orthoses was designed to partially solve this by separating the plastic cast into an inner structure and an outer cover. The personalized inner structure could be combined with three sizes of outer injection molding in order to reduce the additive manufacturing time of the inner part. The time cost was estimated be reduced by two-thirds of that of the additive manufacture of the whole orthosis [
8].
Górski et al. attempted automated computer-aided design modeling for customized limb orthosis design and manufacture. They conducted collision tests on an arbitrary 3 mm gap, which was a comfortable loose fit for less immobility between the patient’s body and orthosis. However, this concept has not been studied for clinical purposes [
9,
10,
11,
12]. A clinical application implemented by Blaya et al. used an additive manufacturing technique to produce a functional splint for partial rupture of the Achilles tendon. The advantages of using the 3D-printed functional splint in the immobilization stage include its easy control and monitoring measures, and the substantial reduction in further lesion deterioration of the Achilles tendon in terms of rupture [
13]. A systematic review concluded that the 3D-printed orthoses/casts appear to be comfortable, provide adequate immobilization, and have pleasing aesthetics [
14]. Another recent systematic review assessed the literature that addressed the effectiveness of 3D-printed orthoses for traumatic and chronic hand conditions, and to identifying knowledge gaps [
15]. Both reviews stated there is a need for well-designed controlled trials including patient-related outcomes, production time, and cost analysis. More recent literature surveys the personalized 3D-printed forearm braces on the design requirement, materials used, technical requirements, and preclinical and clinical results [
16]. The surveys acknowledge that the expensive equipment, lack of appropriate software and scanning tools, and lack of highly skilled clinicians are all factors preventing the implementation of 3D-printed orthoses into current clinical practice.
An alternative to plaster cast treatment in pediatric wrist fracture [
17,
18,
19] was precisely the demonstrated feasibility and safety of 3D-printed brace. It proved to be simple to use and accurate in patient-specific 3D-printed casts that were safe and well-tolerated in children. Janzing et al. investigated left-right differences in wrist circumference of 100 healthy volunteers (age 50 years or older), and the results showed the difference ranged between 0 and 20 mm (mean 3 mm) [
20]. They mirrored the scanned unaffected wrist and adapted the difference between the mirrored wrists and post-traumatic swelling wrist. However, the three-point fixation brace failed to prevent secondary fracture displacement.
In terms of comfort, twelve healthy volunteers were fitted with a 3D-printed brace and fiberglass cast in separate sessions for comfort evaluation when perform the tasks in a normal time. Both castings demonstrated a similar objective function. However, patient’s satisfaction, comfort, and perceived function were superior in the 3D-printed casts [
12,
21]. It was capable of exerting appropriate mechanical correction loads on specific areas to maintain optimal alignment of a fracture forearm to achieve the favorable clinical efficacy and patient comfort [
22].
Although 3D-printed orthoses demonstrate some potential innovations, particularly in appearance, one may question their efficacy from a medical point of view. The lack of science-based, data-centric solutions provides ample motivation to seek better and verifiable results. Therefore, we adopted pres pressure profiles and clearance profiles at certain regions of forearm to assess the effectiveness of immobility from user experiences in comfort levels when wearing a 3D-printed brace. A data-centric, science-based approach was warranted to produce clinically verifiable results.
In the absence of referencing data to judge the appropriate immobility of 3D-printed wrist braces, particularly for different anatomical regions and for individuals [
23,
24], the clinical efficacy was likewise confirmed that the fitting of the cast was always considered satisfactory and deemed to offer adequate immobilization. Therefore, this study provides statistical data of the 3D-printed braces obtained with our developed brace design software, which was dedicated to appropriate regional clearance settings, was able to retain clinical adequate immobility, effectiveness, and comfortability. Efficacy of contention fulfilled the expected tolerance measure between 3 mm and 5 mm in a trial with children [
17]. There was no evidence to state whether or not the tolerance was appropriate. Therefore, we designed experiments to measure and collect pressure profiles in the regions of interest (ROIs) for the new 3D-printed brace and compared the profiles with those from a fiberglass cast. The experiment in phase I was locating sufficient pressure allowance from healthy volunteers; whereas in phase II, we were capable to setup appropriate clearance adjustments accordingly, and apply it to patients with one-year follow up. An expert-based design software was the platform for modeling and applying the design algorithm for clearance adjustments in certain areas of the customized orthosis concluded from the outcomes of experiments. To validate the feasibility of personalized 3D-printed cast, we conducted clinical trials to collect patients’ feedback on immobility, function, speed of recovery, and overall comfort.
In
Section 2.1, we briefly introduce the functions of our developed digital brace software in regional clearance settings for clinical experiments in two phases. Phase I focused on the design aspects with healthy individuals, and Phase I focused on clinical verification with patients. Plaster cast wrapping by casting tape was the immobility goal for designing the customized braces. In Phase I’s experiments, we obtained the proper time of plaster cast curing for pressure measurement in
Section 2.2, and compared immobility test among the plaster casts, vented and unvented 3D-printed brace in
Section 2.3, and approximated immobilization capability test of clearance adjustment in
Section 2.4. In Phase II, we evaluated the disability outcomes of the control and experimental groups by examining the effect of the 3D-printed braces in
Section 3. Finally, we compared the design methods of related research in 3D-printed brace.
2. Materials and Methods
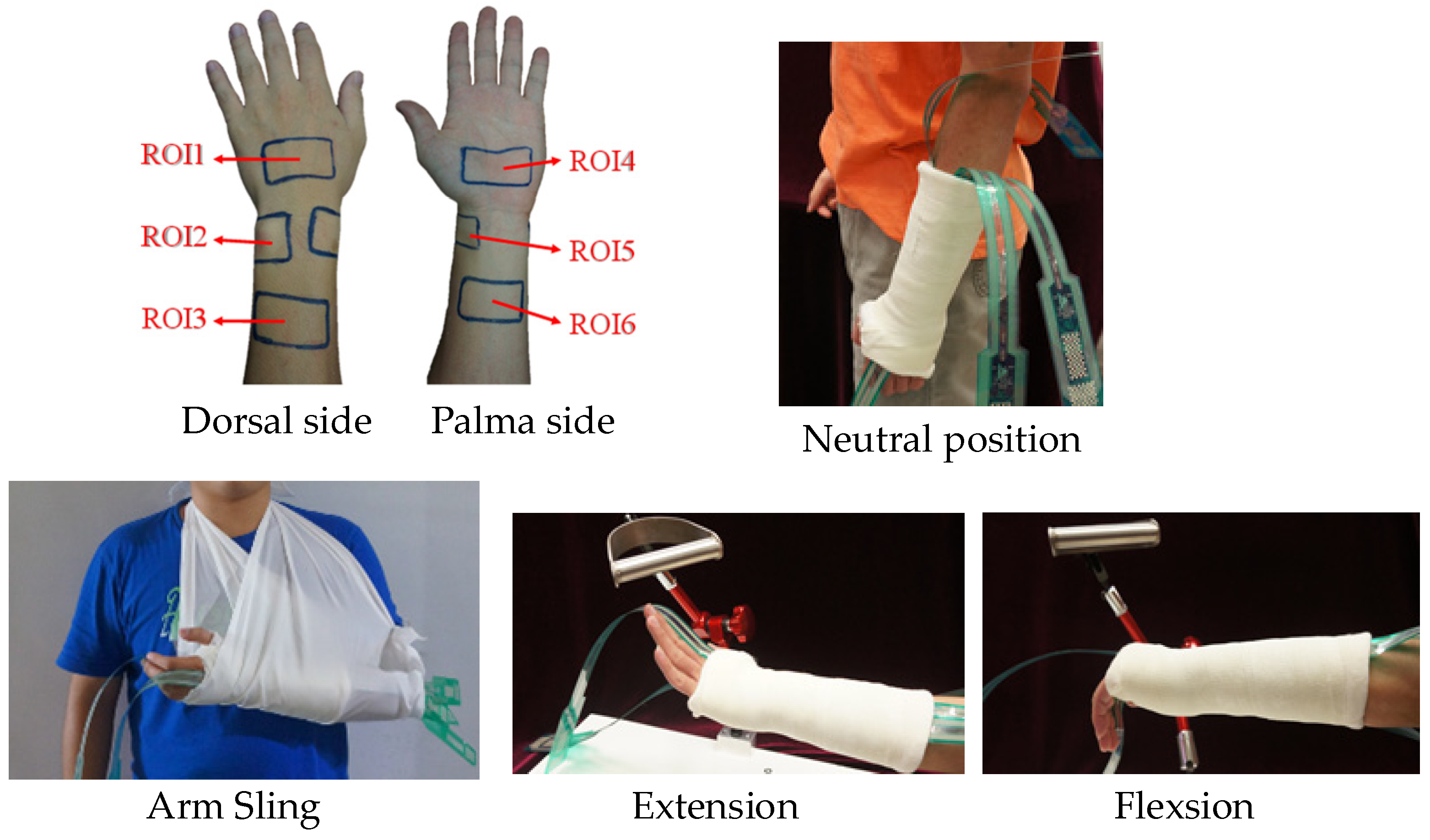
The research was conducted in accordance with the Declaration of the World Medical Association. Informed consent was taken for healthy volunteers and wrist fracture patients under the clinical trial guidelines, B-ER-103-201, approved by the NCKU Hospital IRB Committee. Pressure measurements were taken from patients’ typical wrist representative postures. Twenty healthy volunteers without prior arm or wrist injury were recruited for the Phase I trials. As shown in
Figure 1, industry-grade pressure sensors (Tekscan Inc., The I-Scan
TM Tactile Pressure Mapping System, MA, USA) were wrapped with a bandage at the ROIs of the wrist, and a fiberglass resin cast was then applied. The fiberglass cast was subsequently pressed and molded with 30° extension of the palm relative to the forearm. Pressure maps of the ROIs were also recorded for neutral and arm sling postures. Six ROIs were marked on the palm and forearm of the subjects. The arm and elbow were at rest and positioned on a platform with a posture of palm extension 30° relative to the forearm, as in
Figure 1.
2.1. Design Fundamentals of the 3D-Printed Brace
The construction flow of the 3D-printed brace is shown in
Figure 2. The digital forearm model generated by a hand-held optical scanner (Go!SCAN50, Creaform, Québec City, QC, Canada) was imported into the software. The expert-based brace design software had the orthopedics and rehabilitation experiments embedded to handle a sequence of design processes, including preprocessing, boundary, thickness, surface smoothing, segmentation, and accessories settings. The parameters of clearance setups between the brace and wrist were adjusted accordingly. Based on the clearance in different regions of the inner layer of the brace, we generated the thickness of the brace, divided it into the palmer and dorsal side parts, smoothed the edges, and added accessories for bundling through. For easy dressing and comfort while wearing the wrist brace, dressing windows, ulnar styloid process windows, and vents were generated in the model by Boolean operation. Finally, the brace model was sent for FDM (Fused Deposition Modeling) manufacture in a 20% filling rate with polylactic acid (PLA) material.
Immobility is critical to patient recovery and should not be compromised while pursuing improved comfort. For immobility purposes, flexibility of the plaster cast is not allowed after cast setup. We scanned the patient’s arm at a neutral position as the immobility posture. The 3D-printed brace was designed and fabricated with inflexible PLA material. The aim of the digital wrist brace design was to provide similar immobility as the plaster cast by way of tweaking the clearance. A constant allowance was set to 2 mm from palm to proximal brace boundary (
Figure 3). The 3D-printed personal brace was fitted on the wrist with pressure sensors at the six ROI positions and held in place with a bandage. Pressure maps were collected using the same postures of neutral and arm sling. The trends and deviations of the pressures map from the traditional fiberglass resin brass and the customized 3D-printed brace were compared. If the pressure of any of the six ROIs was greater than a given value β [
4], the process returned to the design step to refine the clearance adjustment region. Such iterations continued until the average pressure of each ROI was less than the given value β. At this point, we obtained the clearance of the personal brace.
2.2. Determine Proper Time of Plaster Cast Curing for Pressure Measurement in Phase I
3MTM ScotchcastTM Plus Casting Tape (4″ × 4 yds, 3MTM Health Care, USA) was used in this experiment. After the fiberglass casts were set, stress relaxation and creep are likely to occur during curing. This could have affected the pressure measurements of the forearm, wrist, and palm over a period of time. Therefore, this experiment aimed to determine the length of time required to obtain stable pressure readings. After the plaster was applied, pressure measurements were taken at 10, 30, 60, 90, 120, and 180 min, in four postures.
Six participants were recruited for this experiment, and there were more than two measurement time points, so the generalized estimating equation (GEE) was used for statistical analyses. As shown in
Table 1, a
p-value less than 0.05 indicated that a significant difference in pressure had occurred. The average pressure was considered a reactive variable. The significant variables were the time point, sensor location, and posture.
For the arm sling posture, the only significant difference was observed at the 10 min time point (p < 0.05). In the neutral position, a significant difference was observed between the 10 min time point and those after the 90 min time point (p-value < 0.05); the 30 min time point also showed a significant difference (p-value < 0.05) to the 90 min, 150 min, and 180 min time points. The 90 min time point showed no significant difference to the 120 min, 150 min, and 180 min time points. Therefore, the 90 min measurement window established in this experiment was confirmed.
2.3. Immobility Test in Phase I
An experiment was conducted to determine if the plaster cast and the customized wrist brace exhibited significant differences in immobilization capability. In addition, we introduced a design variation to the customized wrist brace by adding ventilation. Ventilation, or its lack, might be the key contributor to discomfort when wearing a wrist brace. A 3D-printed customized brace with ventilation can provide relief. A plaster cast, customized wrist brace, and vented customized brace were tested with 10 participants with neutral and arm sling postures. A 2 mm clearance for venting and without venting for the customized braces was used.
The non-parametric Friedman test was used to assess the experimental results. As shown in
Table 2, both medians of pressure data based on time and four postures showed a significant difference,
p < 0.05. Further analysis, shown in
Table 3, compared two braces in three combinations. A significant difference was observed between the plaster cast and the customized braces posture-wise, but there was no significant difference between the vented and unvented customized braces. This implies that the presence of vents had no effect on the pressure exerted by the customized braces under different postures. Although differences between the vented and unvented customized braces were observed timewise, both customized braces did not display hardening or deformation, as the plaster casts did. Therefore, only the vented customized wrist brace was used in the next experiment.
2.4. Immobilization Capability Experiment on Clearance Adjustment
This experiment studied the effect of clearance, depicted by the pressure exerted on the skin of the customized brace, thereby achieving a similar immobilization as the plaster cast by adjusting the regional clearance. Only the arm sling and neutral postures were considered because the extension and flexion postures were deemed unnatural (resulting in unintentional exertion of pressure). Twelve participants participated in the experiment.
The region in which clearance was adjusted is shown in
Figure 3. The region, from the proximal portion of the brace to 6 cm from the distal wrist crease, contained ROIs 3 and 6, and the clearance was reduced to 0.8 mm, 0.6 mm, and 0.3 mm, respectively. The allowance remained 2 mm outside of the region.
Table 4 shows that there was no significant difference between the plaster cast and customized braces with 0.3 mm clearance. The same observation was made for the customized braces with regional clearance at 0.6 mm and 0.8 mm, respectively. However, a significant difference was observed for the customized brace at 0.3 mm clearance compared with the customized braces at 0.6- and 0.8-mm clearance, respectively. The same observation could be made in comparisons between the plaster cast and customized braces at 0.6 mm and 0.8 mm clearance, respectively. As shown in
Table 5, the customized brace at 0.3 mm clearance exhibited a similar immobilization capability as the plaster cast, and that the customized brace at 0.6 mm and 0.8 mm clearance showed no significant difference in immobilization capability. No significant difference between the braces was observed posture-wise.
These results implied that the customized brace at 0.3 mm clearance possessed a very similar immobilization capability to the plaster cast. The following comparison experiment involved only the plaster cast and the customized brace with a local allowance of 0.3 mm.
The Kruskal–Wallis test was used for further comparison of immobility, comfort, and convenience. Significant differences were found between the two braces across the three elements.
Table 6 presents the survey results comparing the two braces and show that immobility, comfort, and convenience all showed significant differences. Compared to customized braces, as shown in
Table 7, plaster cast wrist braces received a higher rating for immobility (pressure), showing that they were perceived as tighter than the customized wrist brace. However, the participants found that the customized wrist brace was superior to the plaster cast in comfort and convenience as both received higher ratings.
4. Discussion
In this study, the basis for determining the immobilization capability was the pressure exerted by the cast and brace on the skin. A previous study showed that the pressure exerted on the skin can be used as a guide to prevent complications [
4]. However, due to differences in individuals and the regions of injury, there is no universal basis to determine the occurrence of complications. In this study, several pressure measurements exceeded 40 mmHg, but there was no reported discomfort from the participants. The reason may be that the participants had only worn the brace for 4 to 5 h, which may be insufficient time for any major discomfort to emerge.
If the clearance of the customized wrist brace at ROIs 3 and 6 was decreased to 0.3 mm, the pressure readings at ROIs 2 and 5 exceeded those from the plaster cast, and the participants reported tightness around the wrist. This was resolved during the clinical trials, with confirmation from the physicians, by loosening the clearance around the wrist from 2 mm to 3 mm. The participants recruited in this study for Phase I were 20 to 30 years of age, healthy, and without a previous history of wrist injuries. The average age of the patients in clinical trial was significantly older than the Phase I participants. Therefore, impressions of the exerted pressure may have been different due to age differences. In addition, a typical patient usually wears a brace for weeks, and the conditions presented in daily life can be quite different from those that occurred during the experiment.
Start time when wearing 3D-printed brace was always an issue. The 3D-printed brace was usually applied to patients 10 days after surgery when swelling reduce. It then took about 2 to 3 days to scan, design, and manufacture. Under these circumstances, the fiberglass cast was inevitably used for temporary protection and immobility until the personal cast was ready. Based on the mirror image of contralateral (non-fractured) wrist for well-tolerated brace design, Janzing et al. applied a three-pad brace on the first day of post-traumatic swelling [
20]. However, a high rate of secondary fracture displacement led to early discontinuation of the study and a very small sample size. Górski et al. proposed an automatic design and manufacture schema to fulfill the strength and possible economic criteria. Therefore, an orthosis on the second day after scanning can be delivered to patients [
11]. In order to judge the representativeness of the Phase II clinical survey results, we listed the most related reference DASH outcomes and compared them with our results in
Table 8. The reference undisplaced/cast data were compared with our non-operative/cast data (N = 9). The primary operation data were compared with customized brace data (N = 24). The 3 month data at values of 37.41 (non-operative/plaster cast) and 24.16 (operative/customized brace) were compared with the reference data at values of 23 (undisplaced/plaster cast) and 22 (operative), respectively. The value sets and clinical survey results for the current study and the reference study were comparable, and they demonstrated the same fracture-healing trend. Customized braces also demonstrated superiority over plaster casts over long wearing periods. In the reference DASH data, the customized brace scored extremely low (0.52 versus reference data 16) after a one-year period. This suggests that the disability level of customized braces have nearly no effect on patients’ daily lives.
Since the technology appears versatile and its cost may decrease in the near future, the identification of further potential applications in orthopedics as an alternative choice of current available plaster casts is of interest.
Functional outcomes were evaluated by DASH and MAM in a one-year follow up in Phase II trial. It shows the 3D-printed orthoses have better daily activity than the fiberglass cast.
Table 9 shows a comparison table of design method for 3D-printed wrist orthoses. Even effectiveness of conventional plaster cast and 3D-printed cast is similar, and most of the research concluded that the customized 3D-printed cast was high in comfort, and had lesser side effects [
12,
17,
18,
19].
In terms of brace structure, most of the design was two halves fixed by a strap which was stable and safe; only the three pads brace structure resulted worse outcomes [
20]. There are a few data regarding the treatment of paediatric upper extremity fracture with 3D-printed casts [
17,
18,
19]. Children were successfully treated with the 3D-printed cast, all with high patient satisfaction.
An appropriate allowance between wrist and the 3D brace is crucial for immobility, effectiveness, and comfortability which were sometimes in opposite directions in design. In current research, there was no evidence to prove whether or not the tolerance appropriate. Regarding immobility test, Graham et al. assessed volunteers by Jebsen Hand Function Test (JHFT) and Patient-Rated Wrist Evaluation (PRWE), whereas in our study, pressure sensor was used to reveal the appropriate clearance between wrist and 3D brace by considering comfort and immobility.
A limitation of this study is that the number of patients was small. This was primarily designed as a safety and proof of concept study. Compared to the experimental group, the number in control group was small in the Phase II trial. Patients in the control group did not undergo wrist correction surgery. Based on patients’ status, physician chose the best treatment for patients.