Comparison of Spine–Pelvis Kinematics Variability during Sit-to-Stand and Stand-to-Sit in People with & without Chronic Low Back Pain: A Vector Coding and Statistical Parametric Mapping Approach
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Participants
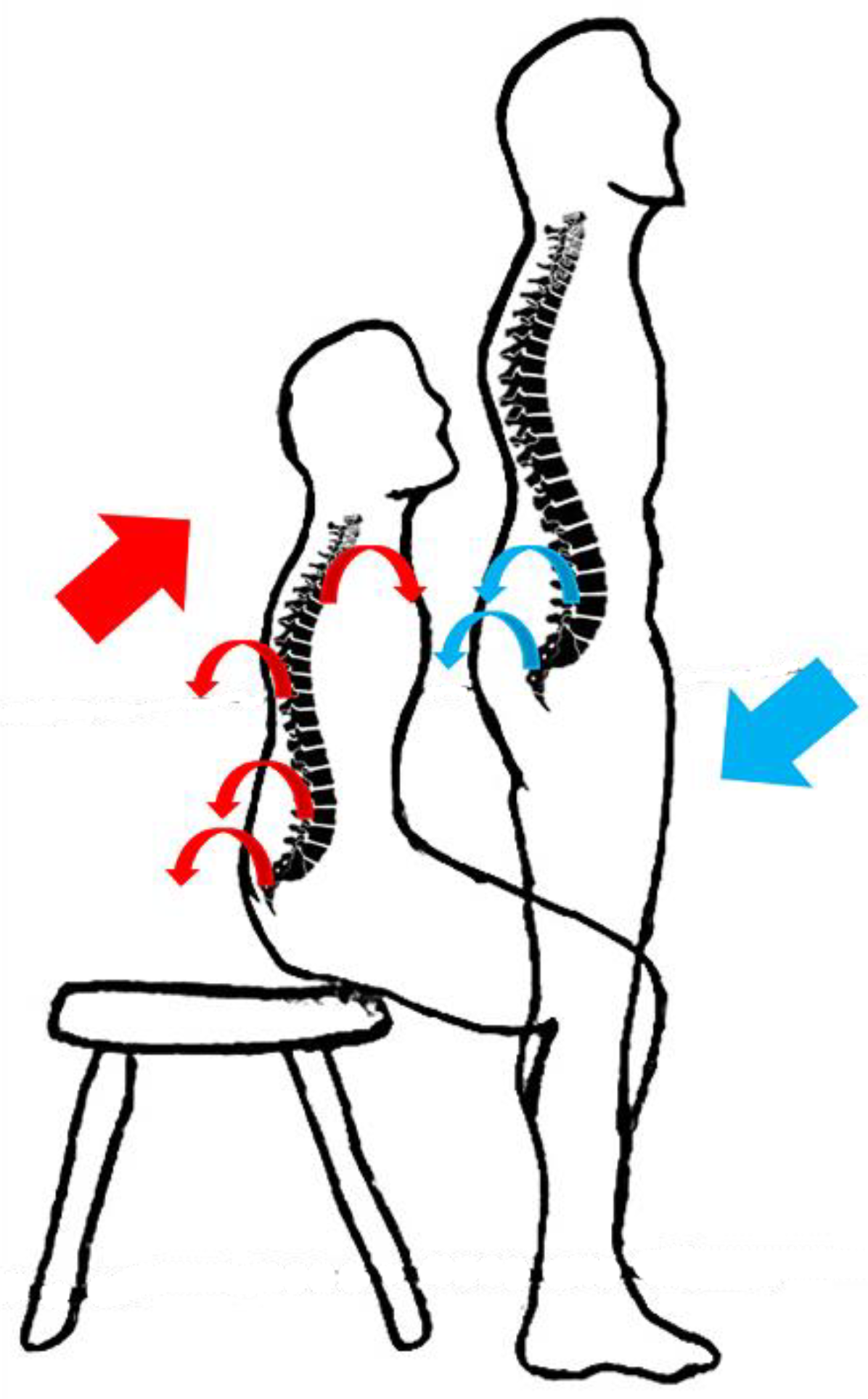
2.2. Experimental Setup
2.3. Data Processing
2.4. Data Analysis
2.5. Pain Measurement
2.6. Performance Evaluation
2.7. Statistical Analysis
3. Results
3.1. ROM Results
3.2. Coordination Pattern Results
3.2.1. Sit-to-Stand
3.2.2. Stand-to-Sit
3.3. Coordination Pattern Variability
3.3.1. Sit-to-Stand
3.3.2. Stand-to-Sit
4. Discussion
4.1. Comparison of Segments’ Range of Motion between Groups
4.2. Comparison of Coordination Patterns between Groups
4.3. Comparison of Coordination Variability between Groups
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Wiens, A.G. Preoperative anxiety in women. AORN J. 1998, 68, 74–88. [Google Scholar] [CrossRef]
- Wand, B.M.; O’Connell, N.E. Chronic non-specific low back pain–sub-groups or a single mechanism? BMC Musculoskelet. Disord. 2008, 9, 11. [Google Scholar] [CrossRef]
- Koes, B.W.; Van Tulder, M.; Thomas, S. Diagnosis and treatment of low back pain. BMJ 2006, 332, 1430–1434. [Google Scholar] [CrossRef]
- Krismer, M.; Van Tulder, M. Low back pain (non-specific). Best Pract. Res. Clin. Rheumatol. 2007, 21, 77–91. [Google Scholar] [CrossRef]
- Rohlmann, A.; Pohl, D.; Bender, A.; Graichen, F.; Dymke, J.; Schmidt, H.; Bergmann, G. Activities of everyday life with high spinal loads. PLoS ONE 2014, 9, e98510. [Google Scholar] [CrossRef]
- Jensen, G.M. Biomechanics of the lumbar intervertebral disk: A review. Phys. Ther. 1980, 60, 765–773. [Google Scholar] [CrossRef]
- Claeys, K.; Dankaerts, W.; Janssens, L.; Brumagne, S. Altered preparatory pelvic control during the sit-to-stance-to-sit movement in people with non-specific low back pain. J. Electromyogr. Kinesiol. 2012, 22, 821–828. [Google Scholar] [CrossRef]
- Crosbie, J.; Nascimento, D.P.; de Faria Negrão Filho, R.; Ferreira, P. Do people with recurrent back pain constrain spinal motion during seated horizontal and downward reaching? Clin. Biomech. 2013, 28, 866–872. [Google Scholar] [CrossRef]
- Shum, G.L.; Crosbie, J.; Lee, R.Y. Effect of low back pain on the kinematics and joint coordination of the lumbar spine and hip during sit-to-stand and stand-to-sit. Spine 2005, 30, 1998–2004. [Google Scholar] [CrossRef]
- Nowakowska, K.; Gzik, M.; Michnik, R.; Myśliwiec, A.; Jurkojć, J.; Suchoń, S.; Burkacki, M. The loads acting on lumbar spine during sitting down and standing up. In Innovations in Biomedical Engineering; Springer: Berlin/Heidelberg, Germany, 2017; pp. 169–176. [Google Scholar]
- Sedrez, J.A.; de Mesquita, P.V.; Gelain, G.M.; Candotti, C.T. Kinematic characteristics of sit-to-stand movements in patients with low back pain: A systematic review. J. Manip. Physiol. Ther. 2019, 42, 532–540. [Google Scholar] [CrossRef]
- Pourahmadi, M.R.; Takamjani, I.E.; Jaberzadeh, S.; Sarrafzadeh, J.; Sanjari, M.A.; Bagheri, R.; Taghipour, M. Kinematics of the spine during sit-to-stand movement using motion analysis systems: A systematic review of literature. J. Sport Rehabil. 2019, 28, 77–93. [Google Scholar] [CrossRef]
- Parkinson, S.; Campbell, A.; Dankaerts, W.; Burnett, A.; O’Sullivan, P. Upper and lower lumbar segments move differently during sit-to-stand. Man. Ther. 2013, 18, 390–394. [Google Scholar] [CrossRef]
- Kerr, K.; White, J.; Barr, D.; Mollan, R. Analysis of the sit-stand-sit movement cycle in normal subjects. Clin. Biomech. 1997, 12, 236–245. [Google Scholar] [CrossRef]
- Panjabi, M.M. The stabilizing system of the spine. Part I. Function, dysfunction, adaptation, and enhancement. J. Spinal Disord. 1992, 5, 383. [Google Scholar] [CrossRef]
- Hodges, P.W.; Richardson, C.A. Contraction of the abdominal muscles associated with movement of the lower limb. Phys. Ther. 1997, 77, 132–142. [Google Scholar] [CrossRef]
- van Dieën, J.H.; Selen, L.P.; Cholewicki, J. Trunk muscle activation in low-back pain patients, an analysis of the literature. J. Electromyogr. Kinesiol. 2003, 13, 333–351. [Google Scholar] [CrossRef]
- Wong, T.K.; Lee, R.Y. Effects of low back pain on the relationship between the movements of the lumbar spine and hip. Hum. Mov. Sci. 2004, 23, 21–34. [Google Scholar] [CrossRef]
- Alijanpour, E.; Abbasi, A.; Needham, R.A.; Naemi, R. Spine and pelvis coordination variability in rowers with and without chronic low back pain during rowing. J. Biomech. 2021, 120, 110356. [Google Scholar] [CrossRef]
- Müller, R.; Ertelt, T.; Blickhan, R. Low back pain affects trunk as well as lower limb movements during walking and running. J. Biomech. 2015, 48, 1009–1014. [Google Scholar] [CrossRef]
- Seay, J.F.; Van Emmerik, R.E.; Hamill, J. Influence of low back pain status on pelvis-trunk coordination during walking and running. Spine 2011, 36, E1070–E1079. [Google Scholar] [CrossRef]
- Mokhtarinia, H.R.; Sanjari, M.A.; Chehrehrazi, M.; Kahrizi, S.; Parnianpour, M. Trunk coordination in healthy and chronic nonspecific low back pain subjects during repetitive flexion–extension tasks: Effects of movement asymmetry, velocity and load. Hum. Mov. Sci. 2016, 45, 182–192. [Google Scholar] [CrossRef]
- Hamill, J.; van Emmerik, R.E.; Heiderscheit, B.C.; Li, L. A dynamical systems approach to lower extremity running injuries. Clin. Biomech. 1999, 14, 297–308. [Google Scholar] [CrossRef]
- Needham, R.A.; Naemi, R.; Hamill, J.; Chockalingam, N. Analysing patterns of coordination and patterns of control using novel data visualisation techniques in vector coding. Foot 2020, 44, 101678. [Google Scholar] [CrossRef]
- Mehdizadeh, S.; Arshi, A.R.; Davids, K. Quantifying coordination and coordination variability in backward versus forward running: Implications for control of motion. Gait Posture 2015, 42, 172–177. [Google Scholar] [CrossRef]
- Heiderscheit, B.C.; Hamill, J.; van Emmerik, R.E. Variability of stride characteristics and joint coordination among individuals with unilateral patellofemoral pain. J. Appl. Biomech. 2002, 18, 110–121. [Google Scholar] [CrossRef]
- Potvin-Gilbert, M. Motor Variability in Rowing. Master’s Thesis, The University of Western Ontario, London, ON, Canada, 2018. [Google Scholar]
- Christe, G.; Redhead, L.; Legrand, T.; Jolles, B.M.; Favre, J. Multi-segment analysis of spinal kinematics during sit-to-stand in patients with chronic low back pain. J. Biomech. 2016, 49, 2060–2067. [Google Scholar] [CrossRef]
- Coghlin, S.; McFadyen, B. Transfer strategies used to rise from a chair in normal and low back pain subjects. Clin. Biomech. 1994, 9, 85–92. [Google Scholar] [CrossRef]
- Needham, R.; Naemi, R.; Healy, A.; Chockalingam, N. Multi-segment kinematic model to assess three-dimensional movement of the spine and back during gait. Prosthet. Orthot. Int. 2016, 40, 624–635. [Google Scholar] [CrossRef]
- Whitney, S.L.; Wrisley, D.M.; Marchetti, G.F.; Gee, M.A.; Redfern, M.S.; Furman, J.M. Clinical measurement of sit-to-stand performance in people with balance disorders: Validity of data for the Five-Times-Sit-to-Stand Test. Phys. Ther. 2005, 85, 1034–1045. [Google Scholar] [CrossRef]
- Needham, R.; Naemi, R.; Chockalingam, N. Quantifying lumbar–pelvis coordination during gait using a modified vector coding technique. J. Biomech. 2014, 47, 1020–1026. [Google Scholar] [CrossRef]
- Needham, R.A.; Naemi, R.; Chockalingam, N. A new coordination pattern classification to assess gait kinematics when utilising a modified vector coding technique. J. Biomech. 2015, 48, 3506–3511. [Google Scholar] [CrossRef]
- Huskisson, E.C. Measurement of pain. Lancet 1974, 304, 1127–1131. [Google Scholar] [CrossRef]
- Hawker, G.A.; Mian, S.; Kendzerska, T.; French, M. Measures of adult pain: Visual analog scale for pain (vas pain), numeric rating scale for pain (nrs pain), mcgill pain questionnaire (mpq), short-form mcgill pain questionnaire (sf-mpq), chronic pain grade scale (cpgs), short form-36 bodily pain scale (sf-36 bps), and measure of intermittent and constant osteoarthritis pain (icoap). Arthritis Care Res. 2011, 63, S240–S252. [Google Scholar]
- Koumantakis, G.A.; Watson, P.J.; Oldham, J.A. Trunk muscle stabilization training plus general exercise versus general exercise only: Randomized controlled trial of patients with recurrent low back pain. Phys. Ther. 2005, 85, 209–225. [Google Scholar] [CrossRef]
- Smeets, R.; Köke, A.; Lin, C.W.; Ferreira, M.; Demoulin, C. Measures of function in low back pain/disorders: Low back pain rating scale (LBPRS), oswestry disability index (ODI), progressive isoinertial lifting evaluation (PILE), quebec back pain disability scale (QBPDS), and roland-morris disability questionnaire (RDQ). Arthritis Care Res. 2011, 63, S158–S173. [Google Scholar]
- Fairbank, J.; Couper, J.; Davies, J.B.; O’Brien, J.P. The Oswestry low back pain disability questionnaire. Physiotherapy 1980, 66, 271–273. [Google Scholar]
- Svendsen, J.H.; Svarrer, H.; Laessoe, U.; Vollenbroek-Hutten, M.; Madeleine, P. Standardized activities of daily living in presence of sub-acute low-back pain: A pilot study. J. Electromyogr. Kinesiol. 2013, 23, 159–165. [Google Scholar] [CrossRef]
- Peydro, M.; López, J.; Cortés, A.; Vivas, M.; Garrido, J.; Tortosa, L. Análisis cinético y cinemático del gesto «levantarse de una silla» en pacientes con lumbalgias. Rehabilitación 2011, 45, 99–105. [Google Scholar] [CrossRef]
- Sánchez-Zuriaga, D.; López-Pascual, J.; Garrido-Jaén, D.; de Moya, M.F.P.; Prat-Pastor, J. Reliability and validity of a new objective tool for low back pain functional assessment. Spine 2011, 36, 1279–1288. [Google Scholar] [CrossRef]
- Sung, P.S. A kinematic analysis for shoulder and pelvis coordination during axial trunk rotation in subjects with and without recurrent low back pain. Gait Posture 2014, 40, 493–498. [Google Scholar] [CrossRef]
- Hodges, P.W.; Smeets, R.J. Interaction between pain, movement, and physical activity: Short-term benefits, long-term consequences, and targets for treatment. Clin. J. Pain 2015, 31, 97–107. [Google Scholar] [CrossRef] [PubMed]
- O’Sullivan, P. It’s Time for Change with the Management of Non-Specific Chronic Low Back Pain; British Association of Sport and Exercise Medicine: Doncaster, UK, 2012; Volume 46, pp. 224–227. [Google Scholar]
- Kim, T.; Chai, E. Trunk and pelvic coordination at various walking speeds during an anterior load carriage task in subjects with and without chronic low back pain. J. Phys. Ther. Sci. 2015, 27, 2353–2356. [Google Scholar] [CrossRef] [PubMed]
- Ebrahimi, S.; Kamali, F.; Razeghi, M.; Haghpanah, S.A. Comparison of the trunk-pelvis and lower extremities sagittal plane inter-segmental coordination and variability during walking in persons with and without chronic low back pain. Hum. Mov. Sci. 2017, 52, 55–66. [Google Scholar] [CrossRef] [PubMed]
- Crosbie, J.; de Faria Negrão Filho, R.; Nascimento, D.P.; Ferreira, P. Coordination of spinal motion in the transverse and frontal planes during walking in people with and without recurrent low back pain. Spine 2013, 38, E286–E292. [Google Scholar] [CrossRef]
- Vereijken, B.; Emmerik, R.E.v.; Whiting, H.; Newell, K.M. Free(z)ing degrees of freedom in skill acquisition. J. Mot. Behav. 1992, 24, 133–142. [Google Scholar] [CrossRef]
- Shafizadeh, M. Movement coordination during sit-to-stand in low back pain people. Hum. Mov. 2016, 17, 107–111. [Google Scholar] [CrossRef]
- Lamoth, C.J.; Daffertshofer, A.; Meijer, O.G.; Beek, P.J. How do persons with chronic low back pain speed up and slow down?: Trunk–pelvis coordination and lumbar erector spinae activity during gait. Gait Posture 2006, 23, 230–239. [Google Scholar] [CrossRef]
- Ippersiel, P.; Robbins, S.; Preuss, R. Movement variability in adults with low back pain during sit-to-stand-to-sit. Clin. Biomech. 2018, 58, 90–95. [Google Scholar] [CrossRef]
- Jewell, C.; Weir, G.; Hamill, J.; Boyer, K.A. The influence of patellofemoral pain on coordination variability over a prolonged treadmill run. ISBS Proc. Arch. 2018, 36, 634. [Google Scholar]
- Silfies, S.P.; Bhattacharya, A.; Biely, S.; Smith, S.S.; Giszter, S. Trunk control during standing reach: A dynamical system analysis of movement strategies in patients with mechanical low back pain. Gait Posture 2009, 29, 370–376. [Google Scholar] [CrossRef]
- Gombatto, S.P.; Brock, T.; DeLork, A.; Jones, G.; Madden, E.; Rinere, C. Lumbar spine kinematics during walking in people with and people without low back pain. Gait Posture 2015, 42, 539–544. [Google Scholar] [CrossRef] [PubMed]
- Madeleine, P.; Mathiassen, S.E.; Arendt-Nielsen, L. Changes in the degree of motor variability associated with experimental and chronic neck–shoulder pain during a standardised repetitive arm movement. Exp. Brain Res. 2008, 185, 689–698. [Google Scholar] [CrossRef] [PubMed]
- Georgoulis, A.D.; Moraiti, C.; Ristanis, S.; Stergiou, N. A novel approach to measure variability in the anterior cruciate ligament deficient knee during walking: The use of the approximate entropy in orthopaedics. J. Clin. Monit. Comput. 2006, 20, 11–18. [Google Scholar] [CrossRef] [PubMed]
 ) placement (left) and marker placement (right).
) placement (left) and marker placement (right).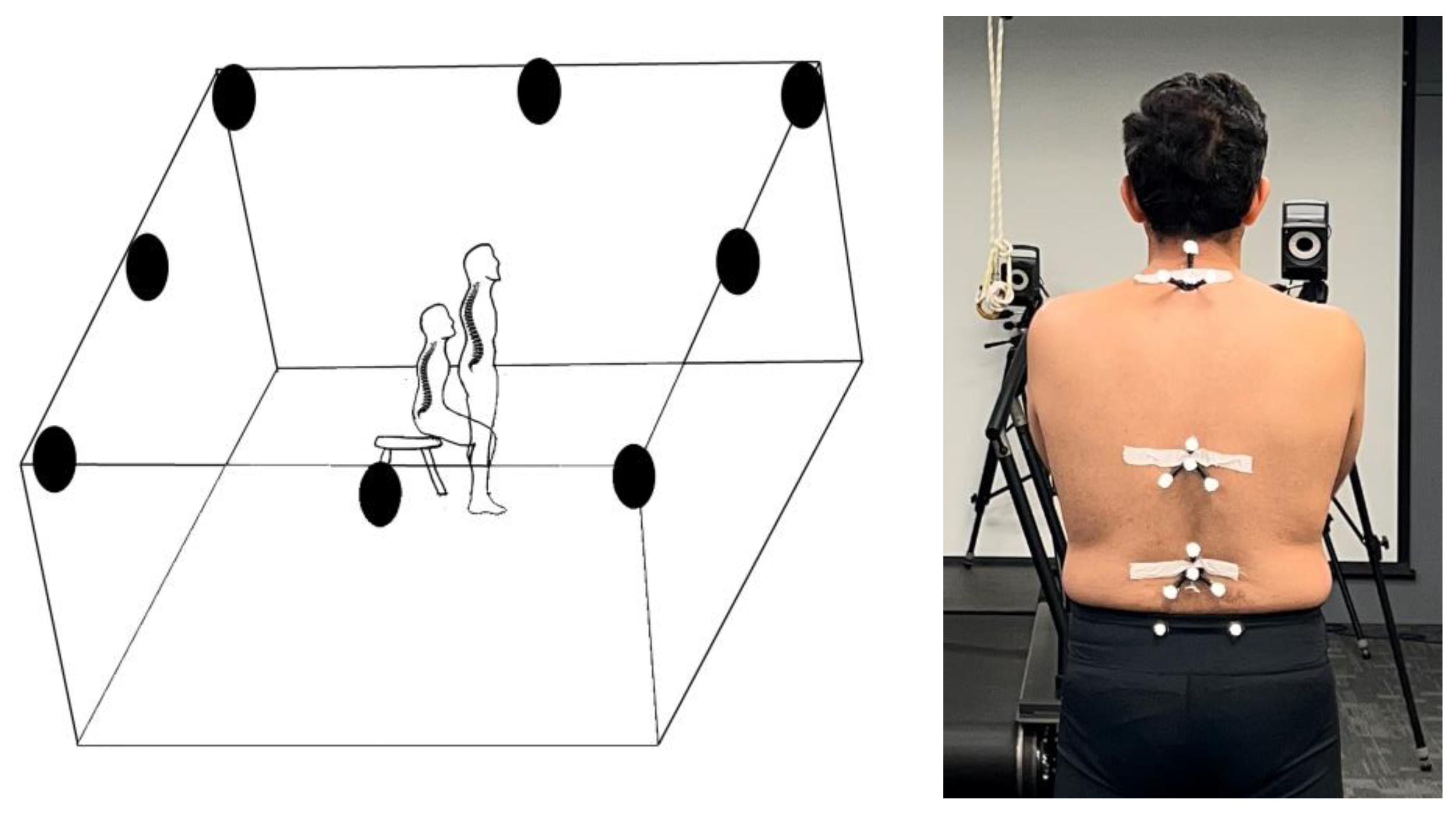





| Group 1. Healthy | Group 2. CLBP | |
|---|---|---|
| Simple size | 10 | 10 |
| Gender (Female/Male) | 5/5 | 5/5 |
| Mean age ± SD (Year) | 29 ± 4.50 | 32 ± 4.90 |
| Mean height ± SD (cm) | 171.5 ± 9.72 | 169.25 ± 4.1 |
| Mean body weight ± SD (Kg) | 70.83 ± 14.60 | 71.87 ± 13.20 |
| Mean VAS ± SD | - | 5.6 ± 1.17 |
| Mean Oswestry Disability Index ± SD | - | 20.8 ± 1.9 |
| Upper Trunk | Lower Trunk | Lower Back | Pelvis | |||||
|---|---|---|---|---|---|---|---|---|
| Sit-to-stand | Stand-to-sit | Sit-to-stand | Stand-to-sit | Sit-to-stand | Stand-to-sit | Sit-to-stand | Stand-to-sit | |
| Healthy group | 45.82 ± 15.71 | 41.60 ± 10.78 | 50.16 ± 22.09 | 44.82 ± 16.36 | 46.48 ± 13.64 | 48.01 ± 16.98 | 32.17 ± 9.38 | 36.28 ± 8.21 |
| CLBP group | 39.45 ± 10.95 | 39.88 ± 12.15 | 42.06 ± 10.84 | 41.42 ± 10.83 | 43.24 ± 11.43 | 43.59 ± 12.41 | 25.37 ± 6.64 | 33.38 ± 8.69 |
| p Value | 0.495 | 0.831 | 0.492 | 0.718 | 0.709 | 0.664 | 0.210 | 0.626 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jangjoo, N.; Alijanpour, E.; Khodabakhsh, S.; Shojaedin, S.S.; Naemi, R. Comparison of Spine–Pelvis Kinematics Variability during Sit-to-Stand and Stand-to-Sit in People with & without Chronic Low Back Pain: A Vector Coding and Statistical Parametric Mapping Approach. Appl. Sci. 2022, 12, 11796. https://doi.org/10.3390/app122211796
Jangjoo N, Alijanpour E, Khodabakhsh S, Shojaedin SS, Naemi R. Comparison of Spine–Pelvis Kinematics Variability during Sit-to-Stand and Stand-to-Sit in People with & without Chronic Low Back Pain: A Vector Coding and Statistical Parametric Mapping Approach. Applied Sciences. 2022; 12(22):11796. https://doi.org/10.3390/app122211796
Chicago/Turabian StyleJangjoo, Narges, Elham Alijanpour, Saeid Khodabakhsh, Seyed Sadredin Shojaedin, and Roozbeh Naemi. 2022. "Comparison of Spine–Pelvis Kinematics Variability during Sit-to-Stand and Stand-to-Sit in People with & without Chronic Low Back Pain: A Vector Coding and Statistical Parametric Mapping Approach" Applied Sciences 12, no. 22: 11796. https://doi.org/10.3390/app122211796
APA StyleJangjoo, N., Alijanpour, E., Khodabakhsh, S., Shojaedin, S. S., & Naemi, R. (2022). Comparison of Spine–Pelvis Kinematics Variability during Sit-to-Stand and Stand-to-Sit in People with & without Chronic Low Back Pain: A Vector Coding and Statistical Parametric Mapping Approach. Applied Sciences, 12(22), 11796. https://doi.org/10.3390/app122211796






