The Outcomes of Conservative Nonpharmacological Treatments for Achilles Tendinopathy: An Umbrella Review
Abstract
:1. Introduction
2. Materials and Methods
2.1. Information Sources and Search Strategy
2.2. Eligibility Criteria
- Population—Human population with IAT or MAT, regardless of age, physical activity status, and duration of symptoms.
- Intervention—Interventions that consisted of one or more different conservative nonpharmacological treatments (exercise (ISOM, isokinetic, ISOT, ECC, CON, etc.), stretching, ESWT, cold air and high-energy laser therapy, low-level laser therapy, microcurrent therapy, cryotherapy, ultrasound therapy, ultrasound, carbon dioxide laser, TECAR therapy, physiotherapy and massage (i.e., manual therapy, deep friction massage, soft tissue massage, ASTYM therapy, etc.), splint/brace, orthoses, tape, acupuncture, wait-and-see, etc.).
- Comparison—Comparison between the aforementioned different conservative nonpharmacological treatments.
- Outcome—Outcomes describing patient’s pain, function, strength, power, endurance, work, functional performance (e.g., jumping performance, etc.), range of motion, tendon properties (e.g., tendon diameter, tendon volume, tendon thickness, tendon neovascularisation, tendon cross-sectional area, tendon length, tendon stiffness, etc.), nervous system sensitization, satisfaction, general health status, quality of life, the incidence of injury, the severity of injury, return-to-sports, and efficacy.
- Study design—Systematic reviews with or without meta-analyses were included, whereas narrative reviews, literature reviews, a protocol for systematic reviews and/or meta-analysis, topical reviews, and intervention reviews were excluded.
2.3. Data Extraction
2.4. Methodological Quality Assessment
- High: no or one noncritical weakness;
- Moderate: more than one noncritical weakness, multiple noncritical weaknesses may diminish confidence in the review, and it may be appropriate to move the overall appraisal down from moderate to low confidence;
- Low: one critical flaw with or without noncritical weaknesses;
- Critically low: more than one critical flaw with or without noncritical weaknesses.
3. Results
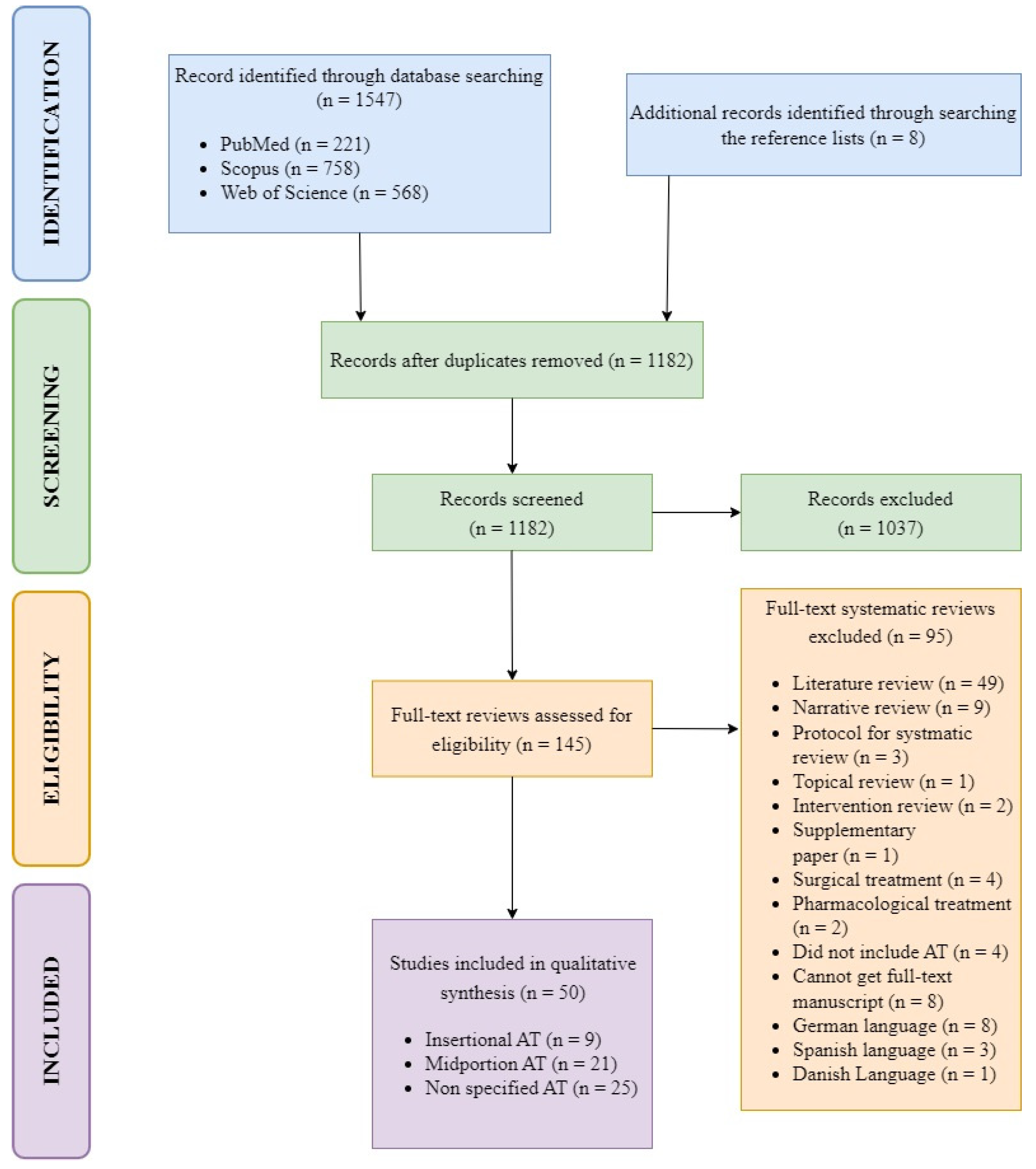
3.1. Selection of Studies
3.2. Methodological Quality Assessment of Studies
3.3. Key Findings
3.3.1. Midportion Achilles Tendinopathy
3.3.2. Insertional Achilles Tendinopathy
3.3.3. Non Specified Achilles Tendinopathy
4. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Van Der Vlist, A.C.; Breda, S.J.; Oei, E.H.G.; Verhaar, J.A.N.; De Vos, R.J. Clinical Risk Factors for Achilles Tendinopathy: A Systematic Review. Br. J. Sports Med. 2019, 53, 1352–1361. [Google Scholar] [CrossRef]
- Miyamoto, T.; Shinohara, Y.; Matsui, T.; Kurokawa, H.; Taniguchi, A.; Kumai, T.; Tanaka, Y. Effects of Achilles Tendon Moment Arm Length on Insertional Achilles Tendinopathy. Appl. Sci. 2020, 10, 6631. [Google Scholar] [CrossRef]
- Barfod, K.W. Achilles Tendon Rupture: Assessment of Non-Operative Treatment Achilles Tendon Total Rupture Score Standard Error of the Measurement. Dan. Med. J. 2014, 61, B4837. [Google Scholar]
- Maffulli, N. Current concept review—Rupture of the Achilles Tendon. J. Bone Jt. Surg. Am. 1999, 81, 1019–1036. [Google Scholar] [CrossRef]
- Järvinen, T.A.H.; Kannus, P.; Paavola, M.; Järvinen, T.L.N.; Józsa, L.; Järvinen, M. Achilles Tendon Injuries. Curr. Opin. Rheumatol. 2001, 13, 150–155. [Google Scholar] [CrossRef]
- Alfredson, H. Chronic Midportion Achilles Tendinopathy: An Update on Research and Treatment. Clin. Sports Med. 2003, 22, 727–741. [Google Scholar] [CrossRef]
- Maffulli, N.; Khan, K.M.; Puddu, G. Overuse Tendon Conditions: Time to Change a Confusing Terminology. Arthroscopy 1998, 14, 840–843. [Google Scholar] [CrossRef]
- van Dijk, C.N.; van Sterkenburg, M.N.; Wiegerinck, J.I.; Karlsson, J.; Maffulli, N. Terminology for Achilles Tendon Related Disorders. Knee Surg. Sport. Traumatol. Arthrosc. 2011, 19, 835–841. [Google Scholar] [CrossRef] [Green Version]
- Sharma, P.; Maffulli, N. Understanding and Managing Achilles Tendinopathy. Br. J. Hosp. Med. 2006, 67, 64–67. [Google Scholar] [CrossRef]
- Almekinders, L.C.; Temple, J.D. Etiology, Diagnosis, and Treatment of Tendonitis: An Analysis of the Literature. Med. Sci. Sports Exerc. 1998, 30, 1183–1190. [Google Scholar] [CrossRef]
- Rhim, H.C.; Kim, M.S.; Choi, S.; Tenforde, A.S. Comparative Efficacy and Tolerability of Nonsurgical Therapies for the Treatment of Midportion Achilles Tendinopathy: A Systematic Review With Network Meta-Analysis. Orthop. J. Sports Med. 2020, 8, 2325967120930567. [Google Scholar] [CrossRef]
- Woitzik, E.; Jacobs, C.; Wong, J.J.; Cote, P.; Shearer, H.M.; Randhawa, K.; Sutton, D.; Southerst, D.; Varatharajan, S.; Brison, R.J.; et al. The Effectiveness of Exercise on Recovery and Clinical Outcomes of Soft Tissue Injuries of the Leg, Ankle, and Foot: A Systematic Review by the Ontario Protocol for Traffic Injury Management (OPTIMa) Collaboration. Man. Ther. 2015, 20, 633–645. [Google Scholar] [CrossRef]
- Irwin, T.A. Current Concepts Review: Insertional Achilles Tendinopathy. Foot Ankle Int. 2010, 31, 933–939. [Google Scholar] [CrossRef]
- Wiegerinck, J.I.; Kerkhoffs, G.M.; van Sterkenburg, M.N.; Sierevelt, I.N.; van Dijk, C.N. Treatment for Insertional Achilles Tendinopathy: A Systematic Review. Knee Surg. Sports Traumatol. Arthrosc. 2013, 21, 1345–1355. [Google Scholar] [CrossRef]
- Jarin, I.J.; Bäcker, H.C.; Vosseller, J.T. Functional Outcomes of Insertional Achilles Tendinopathy Treatment: A Systematic Review. JBJS Rev. 2021, 9, e20. [Google Scholar] [CrossRef]
- Kearney, R.; Costa, M.L. Insertional Achilles Tendinopathy Management: A Systematic Review. Foot Ankle Int. 2010, 31, 689–694. [Google Scholar] [CrossRef]
- Lagas, I.F.; Fokkema, T.; Verhaar, J.A.N.; Bierma-Zeinstra, S.M.A.; van Middelkoop, M.; de Vos, R.J. Incidence of Achilles Tendinopathy and Associated Risk Factors in Recreational Runners: A Large Prospective Cohort Study. J. Sci. Med. Sport 2020, 23, 448–452. [Google Scholar] [CrossRef]
- Tegner, Y.; Lysholm, J.; Lysholm, M.; Gillquist, J. A Performance Test to Monitor Rehabilitation and Evaluate Anterior Cruciate Ligament Injuries. Am. J. Sports Med. 1986, 14, 156–159. [Google Scholar] [CrossRef]
- De Jonge, S.; Van Den Berg, C.; De Vos, R.J.; Van Der Heide, H.J.L.; Weir, A.; Verhaar, J.A.N.; Tol, J.L. Incidence of Midportion Achilles Tendinopathy in the General Population. Br. J. Sports Med. 2011, 45, 1026–1028. [Google Scholar] [CrossRef] [Green Version]
- Li, H.Y.; Hua, Y.H. Achilles Tendinopathy: Current Concepts about the Basic Science and Clinical Treatments. Biomed. Res. Int. 2016, 2016, 6492597. [Google Scholar] [CrossRef] [Green Version]
- Richard, P.; Ames, J.; Longo, U.G.; Denaro, V.; Maffulli, N. Achilles Tendon Problems: Not Just an Orthopaedic Issue. Disabil. Rehabil. 2008, 30, 1646–1650. [Google Scholar] [CrossRef]
- Rolf, C.; Mavin, T. Etiology, Histopathology, and Outcome of Surgery in Achillodynia. Am. Orthop. Foot Ankle Soc. 2015, 565–569. [Google Scholar] [CrossRef]
- Kvist, M. Achilles Tendon Injuries in Athletes. Sport. Med. 1994, 18, 173–201. [Google Scholar] [CrossRef]
- Raman, J.; MacDermid, J.C.; Grewal, R. Effectiveness of Different Methods of Resistance Exercises in Lateral Epicondylosis—A Systematic Review. J. Hand Ther. 2012, 25, 5–26. [Google Scholar] [CrossRef]
- Rompe, J.D.; Furia, J.P.; Maffulli, N. Mid-Portion Achilles Tendinopathy—Current Options for Treatment. Disabil. Rehabil. 2008, 30, 1666–1676. [Google Scholar] [CrossRef]
- Johannsen, F.; Olesen, J.L.; Øhlenschläger, T.F.; Lundgaard-Nielsen, M.; Cullum, C.K.; Jakobsen, A.S.; Rathleff, M.S.; Magnusson, P.S.; Kjær, M. Effect of Ultrasonography-Guided Corticosteroid Injection vs Placebo Added to Exercise Therapy for Achilles Tendinopathy: A Randomized Clinical Trial. JAMA Netw. Open 2022, 5, E2219661. [Google Scholar] [CrossRef]
- Alfredson, H.; Pietila, T. Heavy-Load Eccentric Calf Muscle Training For the Treatment of Chronic Achilles Tendinosis. Am. J. Sports Med. 1998, 26, 360–366. [Google Scholar] [CrossRef] [Green Version]
- Pavone, V.; Vescio, A.; Mobilia, G.; Dimartino, S.; Di Stefano, G.; Culmone, A.; Testa, G. Conservative Treatment of Chronic Achilles Tendinopathy: A Systematic Review. J. Funct. Morphol. Kinesiol. 2019, 4, 46. [Google Scholar] [CrossRef] [Green Version]
- Magnussen, R.A.; Dunn, W.R.; Thomson, A.B. Nonoperative Treatment of Midportion Achilles Tendinopathy: A Systematic Review. Clin. J. Sport Med. 2009, 19, 54–64. [Google Scholar] [CrossRef] [Green Version]
- Meyer, A.; Tumilty, S.; Baxter, G.D. Eccentric Exercise Protocols for Chronic Non-Insertional Achilles Tendinopathy: How Much Is Enough? Scand. J. Med. Sci. Sport. 2009, 19, 609–615. [Google Scholar] [CrossRef]
- Merza, E.; Pearson, S.; Lichtwark, G.; Ollason, M.; Malliaras, P. Immediate and Long-Term Effects of Mechanical Loading on Achilles Tendon Volume: A Systematic Review and Meta-Analysis. J. Biomech. 2021, 118, 110289. [Google Scholar] [CrossRef] [PubMed]
- Murphy, M.; Travers, M.; Gibson, W.; Chivers, P.; Debenham, J.; Docking, S.; Rio, E. Rate of Improvement of Pain and Function in Mid-Portion Achilles Tendinopathy with Loading Protocols: A Systematic Review and Longitudinal Meta-Analysis. Sports Med. 2018, 48, 1875–1891. [Google Scholar] [CrossRef] [PubMed]
- Head, J.; Mallows, A.; Debenham, J.; Travers, M.J.; Allen, L. The Efficacy of Loading Programmes for Improving Patient-Reported Outcomes in Chronic Midportion Achilles Tendinopathy: A Systematic Review. Musculoskelet. Care 2019, 17, 283–299. [Google Scholar] [CrossRef]
- Malliaras, P.; Barton, C.J.; Reeves, N.D.; Langberg, H. Achilles and Patellar Tendinopathy Loading Programmes: A Systematic Review Comparing Clinical Outcomes and Identifying Potential Mechanisms for Effectiveness. Sports Med. 2013, 43, 267–286. [Google Scholar] [CrossRef] [PubMed]
- Kristensen, J.; Franklyn-Miller, A. Resistance Training in Musculoskeletal Rehabilitation: A Systematic Review. Br. J. Sports Med. 2012, 46, 719–726. [Google Scholar] [CrossRef]
- Burton, I.; McCormack, A. Assessment of the Reporting Quality of Resistance Training Interventions in Randomised Controlled Trials for Lower Limb Tendinopathy: A Systematic Review. Clin. Rehabil. 2022, 36, 026921552210887. [Google Scholar] [CrossRef]
- Cox, J.; Varatharajan, S.; Côté, P. Effectiveness of Acupuncture Therapies to Manage Musculoskeletal Disorders of the Extremities: A Systematic Review. J. Orthop. Sports Phys. Ther. 2016, 46, 409–429. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Al-Abbad, H.; Simon, J.V. The Effectiveness of Extracorporeal Shock Wave Therapy on Chronic Achilles Tendinopathy: A Systematic Review. Foot Ankle Int. 2013, 34, 33–41. [Google Scholar] [CrossRef]
- Zhi, X.; Liu, X.; Han, J.; Xiang, Y.; Wu, H.; Wei, S.; Xu, F. Nonoperative Treatment of Insertional Achilles Tendinopathy: A Systematic Review. J. Orthop. Surg. Res. 2021, 16, 233. [Google Scholar] [CrossRef]
- Chughtai, M.; Newman, J.M.; Sultan, A.A.; Samuel, L.T.; Rabin, J.; Khlopas, A.; Bhave, A.; Mont, M.A. Astym(®) Therapy: A Systematic Review. Ann. Transl. Med. 2019, 7, 70. [Google Scholar] [CrossRef]
- Santacaterina, F.; Miccinilli, S.; Bressi, F.; Sterzi, S.; Bravi, M. An Overview of Achilles Tendinopathy Management. Osteology 2021, 1, 175–186. [Google Scholar] [CrossRef]
- Gatz, M.; Spang, C.; Alfredson, H. Partial Achilles Tendon Rupture—A Neglected Entity: A Narrative Literature Review on Diagnostics and Treatment Options. J. Clin. Med. 2020, 9, 3380. [Google Scholar] [CrossRef] [PubMed]
- Methley, A.M.; Campbell, S.; Chew-Graham, C.; McNally, R.; Cheraghi-Sohi, S. PICO, PICOS and SPIDER: A Comparison Study of Specificity and Sensitivity in Three Search Tools for Qualitative Systematic Reviews. BMC Health Serv. Res. 2014, 14, 579. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aromataris, E.; Fernandez, R.; Godfrey, C.M.; Holly, C.; Khalil, H.; Tungpunkom, P. Summarizing Systematic Reviews: Methodological Development, Conduct and Reporting of an Umbrella Review Approach. Int. J. Evid.-Based Healthc. 2015, 13, 132–140. [Google Scholar] [CrossRef] [Green Version]
- Shea, B.J.; Reeves, B.C.; Wells, G.; Thuku, M.; Hamel, C.; Moran, J.; Moher, D.; Tugwell, P.; Welch, V.; Kristjansson, E.; et al. AMSTAR 2: A Critical Appraisal Tool for Systematic Reviews That Include Randomised or Non-Randomised Studies of Healthcare Interventions, or Both. BMJ 2017, 358, j4008. [Google Scholar] [CrossRef] [Green Version]
- Burton, I.; McCormack, A. The Implementation of Resistance Training Principles in Exercise Interventions for Lower Limb Tendinopathy: A Systematic Review. Phys. Ther. Sport 2021, 50, 97–113. [Google Scholar] [CrossRef]
- Drew, B.T.; Smith, T.O.; Littlewood, C.; Sturrock, B. Do Structural Changes (Eg, Collagen/Matrix) Explain the Response to Therapeutic Exercises in Tendinopathy: A Systematic Review. Br. J. Sports Med. 2014, 48, 966–972. [Google Scholar] [CrossRef]
- Färnqvist, K.; Pearson, S.; Malliaras, P. Adaptation of Tendon Structure and Function in Tendinopathy With Exercise and Its Relationship to Clinical Outcome. J. Sport Rehabil. 2020, 29, 107–115. [Google Scholar] [CrossRef] [Green Version]
- Frizziero, A.; Trainito, S.; Oliva, F.; Aldini, N.N.; Masiero, S.; Maffulli, N. The Role of Eccentric Exercise in Sport Injuries Rehabilitation. Br. Med. Bull. 2014, 110, 47–75. [Google Scholar] [CrossRef] [Green Version]
- Hasani, F.; Vallance, P.; Haines, T.; Munteanu, S.E.; Malliaras, P. Are Plantarflexor Muscle Impairments Present Among Individuals with Achilles Tendinopathy and Do They Change with Exercise? A Systematic Review with Meta-Analysis. Sports Med.-Open 2021, 7, 18. [Google Scholar] [CrossRef]
- Luan, X.; Tian, X.; Zhang, H.; Huang, R.; Li, N.; Chen, P.; Wang, R. Exercise as a Prescription for Patients with Various Diseases. J. Sport Health Sci. 2019, 8, 422–441. [Google Scholar] [CrossRef] [PubMed]
- Mani-Babu, S.; Morrissey, D.; Waugh, C.; Screen, H.; Barton, C. The Effectiveness of Extracorporeal Shock Wave Therapy in Lower Limb Tendinopathy: A Systematic Review. Am. J. Sports Med. 2015, 43, 752–761. [Google Scholar] [CrossRef] [PubMed]
- Obst, S.J.; Barrett, R.S.; Newsham-West, R. Immediate Effect of Exercise on Achilles Tendon Properties: Systematic Review. Med. Sci. Sports Exerc. 2013, 45, 1534–1544. [Google Scholar] [CrossRef]
- Peters, J.A.; Zwerver, J.; Diercks, R.L.; Elferink-Gemser, M.T.; van den Akker-Scheek, I. Preventive Interventions for Tendinopathy: A Systematic Review. J. Sci. Med. Sport 2016, 19, 205–211. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rabello, L.M.; Van Den Akker-Scheek, I.; Brink, M.S.; Maas, M.; Diercks, R.L.; Zwerver, J. Association between Clinical and Imaging Outcomes after Therapeutic Loading Exercise in Patients Diagnosed with Achilles or Patellar Tendinopathy at Short- And Long-Term Follow-up: A Systematic Review. Clin. J. Sport Med. 2020, 30, 390–403. [Google Scholar] [CrossRef]
- Rowe, V.; Hemmings, S.; Barton, C.; Malliaras, P.; Maffulli, N.; Morrissey, D. Conservative Management of Midportion Achilles Tendinopathy. Sports Med. 2012, 42, 941–967. [Google Scholar] [CrossRef]
- Scott, L.A.; Munteanu, S.E.; Menz, H.B. Effectiveness of Orthotic Devices in the Treatment of Achilles Tendinopathy: A Systematic Review. Sporta Med. 2015, 45, 95–110. [Google Scholar] [CrossRef] [PubMed]
- Speed, C. A Systematic Review of Shockwave Therapies in Soft Tissue Conditions: Focusing on the Evidence. Br. J. Sports Med. 2014, 48, 1538–1542. [Google Scholar] [CrossRef]
- Sussmilch-Leitch, S.P.; Collins, N.J.; Bialocerkowski, A.E.; Warden, S.J.; Crossley, K.M. Physical Therapies for Achilles Tendinopathy: Systematic Review and Meta-Analysis. J. Foot Ankle Res. 2012, 5, 15. [Google Scholar] [CrossRef] [Green Version]
- Tengku Yusof, T.N.B.; Seow, D.; Vig, K.S. Extracorporeal Shockwave Therapy for Foot and Ankle Disorders: A Systematic Review and Meta-Analysis. J. Am. Podiatr. Med. Assoc. 2022, 112, 18–191. [Google Scholar] [CrossRef]
- Van Der Vlist, A.C.; Winters, M.; Weir, A.; Ardern, C.L.; Welton, N.J.; Caldwell, D.M.; Verhaar, J.A.N.; De Vos, R.J. Which Treatment Is Most Effective for Patients with Achilles Tendinopathy? A Living Systematic Review with Network Meta-Analysis of 29 Randomised Controlled Trials. Br. J. Sports Med. 2021, 55, 249–255. [Google Scholar] [CrossRef] [PubMed]
- Young, J.L.; Rhon, D.I.; de Zoete, R.M.J.; Cleland, J.A.; Snodgrass, S.J. The Influence of Dosing on Effect Size of Exercise Therapy for Musculoskeletal Foot and Ankle Disorders: A Systematic Review. Braz. J. Phys. Ther. 2018, 22, 20–32. [Google Scholar] [CrossRef] [PubMed]
- Wasielewski, N.J.; Kotsko, K.M. Does Eccentric Exercise Reduce Pain and Improve Strength in Physically Active Adults with Symptomatic Lower Extremity Tendinosis? A Systematic Review. J. Athl. Train. 2007, 42, 409–421. [Google Scholar]
- Tumilty, S.; Munn, J.; McDonough, S.; Hurley, D.A.; Basford, J.R.; Baxter, G.D. The Dose That Works: Low Level Laser Treatment of Tendinopathy. AIP Conf. Proc. 2010, 1226, 170–178. [Google Scholar] [CrossRef]
- Ortega-Castillo, M.; Martin-Soto, L.; Medina-Porqueres, I. Benefits of Kinesiology Tape on Tendinopathies: A Systematic Review. Montenegrin J. Sports Sci. Med. 2020, 9, 73–86. [Google Scholar] [CrossRef]
- Mitham, K.; Mallows, A.; Debenham, J.; Seneviratne, G.; Malliaras, P. Conservative Management of Acute Lower Limb Tendinopathies: A Systematic Review. Musculoskelet. Care 2021, 19, 110–126. [Google Scholar] [CrossRef]
- Kingma, J.J.; de Knikker, R.; Wittink, H.M.; Takken, T. Eccentric Overload Training in Patients with Chronic Achilles Tendinopathy: A Systematic Review. Br. J. Sports Med. 2007, 41, 5–10. [Google Scholar] [CrossRef] [Green Version]
- Korakakis, V.; Whiteley, R.; Tzavara, A.; Malliaropoulos, N. The Effectiveness of Extracorporeal Shockwave Therapy in Common Lower Limb Conditions: A Systematic Review Including Quantification of Patient-Rated Pain Reduction. Br. J. Sports Med. 2018, 52, 387–407. [Google Scholar] [CrossRef] [Green Version]
- Martimbianco, A.L.C.; Ferreira, R.E.S.; Latorraca, C.D.O.C.; Bussadori, S.K.; Pacheco, R.L.; Riera, R. Photobiomodulation with Low-Level Laser Therapy for Treating Achilles Tendinopathy: A Systematic Review and Meta-Analysis. Clin. Rehabil. 2020, 34, 713–722. [Google Scholar] [CrossRef]
- Murphy, M.C.; Travers, M.J.; Chivers, P.; Debenham, J.R.; Docking, S.I.; Rio, E.K.; Gibson, W. Efficacy of Heavy Eccentric Calf Training for Treating Mid-Portion Achilles Tendinopathy: A Systematic Review and Meta-Analysis. Br. J. Sports Med. 2019, 53, 1070–1077. [Google Scholar] [CrossRef]
- Wilson, F.; Walshe, M.; O’Dwyer, T.; Bennett, K.; Mockler, D.; Bleakley, C. Exercise, Orthoses and Splinting for Treating Achilles Tendinopathy: A Systematic Review with Meta-Analysis. Br. J. Sports Med. 2018, 52, 1564–1574. [Google Scholar] [CrossRef] [PubMed]
- Woodley, B.L.; Newsham-West, R.J.; Baxter, G.D. Chronic Tendinopathy: Effectiveness of Eccentric Exercise. Br. J. Sports Med. 2007, 41, 188–198. [Google Scholar] [CrossRef] [PubMed]
- Yu, H.; Randhawa, K.; Côté, P.; Collaboration, O. The Effectiveness of Physical Agents for Lower-Limb Soft Tissue Injuries: A Systematic Review. J. Orthop. Sports Phys. Ther. 2016, 46, 523–554. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Clifford, C.; Challoumas, D.; Paul, L.; Syme, G.; Millar, N.L. Effectiveness of Isometric Exercise in the Management of Tendinopathy: A Systematic Review and Meta-Analysis of Randomised Trials. BMJ Open Sport Exerc. Med. 2020, 6, e000760. [Google Scholar] [CrossRef] [PubMed]
- Escriche-Escuder, A.; Casanã, J.; Cuesta-Vargas, A.I. Load Progression Criteria in Exercise Programmes in Lower Limb Tendinopathy: A Systematic Review. BMJ Open 2020, 10, e041433. [Google Scholar] [CrossRef]
- Fan, Y.; Feng, Z.; Cao, J.; Fu, W. Efficacy of Extracorporeal Shock Wave Therapy for Achilles Tendinopathy: A Meta-Analysis. Orthop. J. Sports Med. 2020, 8, 2325967120903430. [Google Scholar] [CrossRef]
- Habets, B.; van Cingel, R.E.H. Eccentric Exercise Training in Chronic Mid-Portion Achilles Tendinopathy: A Systematic Review on Different Protocols. Scand. J. Med. Sci. Sports 2015, 25, 3–15. [Google Scholar] [CrossRef]
- Young, J.L.; Press, J.M. The Physiologic Basis of Sports Rehabilitation. Phys. Med. Rehabil. Clin. N. Am. 1994, 5, 9–36. [Google Scholar] [CrossRef]
- Lindstedt, S.L.; Lastayo, P.C.; Reich, T.E. When Active Muscles Lengthen: Properties and Consequences of Eccentric Contractions. Physiology 2001, 16, 256–261. [Google Scholar] [CrossRef] [Green Version]
- Dussault, R.G.; Kaplan, P.A.; Roederer, G. MR Imaging of Achilles Tendon in Patients with Familial Hyperlipidemia: Comparison with Plain Films, Physical Examination, and Patients with Traumatic Tendon Lesions. Am. J. Roentgenol. 1995, 164, 403–407. [Google Scholar] [CrossRef]
- Schweitzer, M.E.; Karasick, D. MR Imaging of Disorders of the Achilles Tendon. Am. J. Roentgenol. 2000, 175, 613–625. [Google Scholar] [CrossRef] [PubMed]
- Gattereau, A.; Davignon, J.; Langelier, M.; Levesque, H.P. An Improved Radiological Method for the Evaluation of Achilles Tendon Xanthomatosis. Can. Med. Assoc. J. 1973, 108, 39–42. [Google Scholar] [PubMed]
- Åstrom, M.; Gentz, C.F.; Nilsson, P.; Rausing, A.; Sjöberg, S.; Westlin, N. Imaging in Chronic Achilles Tendinopathy: A Comparison of Ultrasonography, Magnetic Resonance Imaging and Surgical Findings in 27 Histologically Verified Cases. Skelet. Radiol. 1996, 25, 615–620. [Google Scholar] [CrossRef]
- Knobloch, K. Tendinopathy and Neovascularization in Rheumatology. Curr. Rheumatol. Rev. 2007, 3, 135–146. [Google Scholar] [CrossRef]
- Knobloch, K. Eccentric Training in Achilles Tendinopathy: Is It Harmful To. Br. J. Sports Med. 2006, 41, e2. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Steere, H.K.; DeLuca, S.; Borg-Stein, J.; Malanga, G.A.; Tenforde, A.S. A Narrative Review Evaluating Extracorporeal Shockwave Therapy as a Potential Regenerative Treatment for Musculoskeletal Conditions in Military Personnel. Mil. Med. 2021, 186, 682–706. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Križaj, L.; Kozinc, Ž.; Šarabon, N. The Outcomes of Conservative Nonpharmacological Treatments for Achilles Tendinopathy: An Umbrella Review. Appl. Sci. 2022, 12, 12132. https://doi.org/10.3390/app122312132
Križaj L, Kozinc Ž, Šarabon N. The Outcomes of Conservative Nonpharmacological Treatments for Achilles Tendinopathy: An Umbrella Review. Applied Sciences. 2022; 12(23):12132. https://doi.org/10.3390/app122312132
Chicago/Turabian StyleKrižaj, Luka, Žiga Kozinc, and Nejc Šarabon. 2022. "The Outcomes of Conservative Nonpharmacological Treatments for Achilles Tendinopathy: An Umbrella Review" Applied Sciences 12, no. 23: 12132. https://doi.org/10.3390/app122312132
APA StyleKrižaj, L., Kozinc, Ž., & Šarabon, N. (2022). The Outcomes of Conservative Nonpharmacological Treatments for Achilles Tendinopathy: An Umbrella Review. Applied Sciences, 12(23), 12132. https://doi.org/10.3390/app122312132






