1. Introduction
Tooth eruption is a complex physiological process with various pathological forms of manifestation that can create discomfort for the patient, both in the temporary and permanent dentition. Wisdom teeth or third molars are the last permanent teeth to erupt on the arch and are located most posteriorly. They usually erupt between the ages of 17 and 25, but they can erupt many years later. Most adults have four wisdom teeth; mandibular third molars are frequently located in a vicious, non-functional position or are partially erupted [
1]. Third molars are frequently associated with pathological changes such as pericoronitis, dental caries, damage to the adjacent oral mucosa, cysts, and tumors. It is unanimously accepted that third molar extraction is indicated when signs or symptoms of local infection are present [
2]. In the permanent dentition, the eruption of the lower wisdom teeth is frequently associated with clinical manifestations that depend on the existing space on the arch, the thickness of the mucous cap (operculum) that it must pass through, and the relationship with the existing teeth on the arch. Among these clinical manifestations, subjective signs can evolve from a simple sensation of local tension to pain intensified by speech, mastication, and swallowing. Locally, distal to the last erupted tooth on the arch, a congestive, edematous, hyperemic mucosa can be highlighted, sometimes associated with the presence of a dehiscent, ulcerative area at the level of the mucosa. Through this dehiscence, the crown of the erupting tooth can be palpated, representing a gateway for various pathogenic factors. This area is frequently subjected to masticatory trauma. All these aspects can be associated with a local inflammatory process that represents the pericoronitis of the erupting tooth [
3].
The discomfort created by this inflammatory process can heal spontaneously or worsen and intensify if the tooth does not fully erupt in the oral cavity. The transition to suppurative pericoronitis can be done very quickly. The subjective signs of a suppurative pericoronitis are the increasing pain with a throbbing quality that can radiate toward the mandible, ear, or tonsillar region. Intraoral examination becomes increasingly difficult due to the trismus, which is accentuated by the inflammation of the area adjacent to the third molar. Increasing in inflammatory phenomena, the presence of pain and trismus is the moment when the patient calls for a dental consultation. Pericoronitis has a reported prevalence of 81% between the 20- and 29-years old group. The general state of health is not a predisposing factor, but in 43% of cases, upper respiratory tract infection precedes the appearance of pericoronitis. Studies have shown that the microflora of pericoronitis is predominantly anaerobic, often including high levels of bacteria such as
Streptococcus,
Staphylococcus,
Actinomyces oris,
Eikenella corodens,
Propionibacterium,
Eubacterium nodatum,
Fusobacterium nucleatum, Treponema denticola, and
Eubacterium saburreum [
1,
4,
5].
The first step of treatment consists of local irrigation with warmed saline solution or at room temperature, chloramine solution, chlorhexidine, D’Alibour solution, Dakin’s solution, or other solutions that may contain hydrogen peroxide [
6], and aims to eliminate detritus nutrition and reduction of local inflammation [
7]. Usually, irrigation may be sufficient to limit the worsening of symptoms [
8]; the appearance of purulent discharge under the operculum implies the administration of antibiotics. Their widespread use, even in the case of pericoronitis, can lead to the emergence of antibiotic resistance over time [
9,
10], which is why it is recommended to restrict the use of antibiotics.
The growing number of drug-resistant pathogens implies the urgency to identify and isolate new bioactive compounds from plants using standardized analytical procedures. Plant extracts, rich in bioactive compounds, could represent alternatives in the fight against pathogenic bacteria. Thus, an effective substitute in the pericoronitis could be natural extracts. Data from the specialized literature highlight the fact that natural extracts obtained from lignocellulosic matrices can be an important source of bioactive compounds with antioxidant, antibacterial, and antifungal effects [
11]. The beech (
Fagus sylvatica L.) represents one of the most widespread woody plants in Europe [
12]. Data from the specialized literature highlight the fact that beech bark can be an important source of bioactive compounds with biological activities, such as antitumoral, antioxidant, and antimicrobial [
13,
14,
15,
16]. The beech bark extracts were active against pathogenic bacteria (Gram-positive and Gram-negative) and some
Candida species [
11].
This study aims to evaluate the degree of change in discomfort represented by pain, trismus, and bleeding in pericoronitis of the lower third molar, following local irrigations performed under the operculum of the erupting tooth and comparing the results obtained for each type of irrigating solution used.
2. Materials and Methods
2.1. Chemicals and Plant Sample
The plant material (bark of beech—Fagus sylvatica L.) was collected from the Gurghiu Mountains, Toplița region, Harghita county, being purchased as industrial waste from the commercial company Copet Dinex, Subcetate, Harghita, Romania. The collection was made between November and December 2021. The age of the tested trees was approximately 15–20 years. This waste was identified by a specialist, then it was left to dry at room temperature and then shredded by grinding and obtaining a particles size between 0.5 to 1 mm.
The plant material was crushed in a GRINDOMIX GM 2000 mill (Retsch, Bucharest, Romania) to an average particle size of 0.5 mm and a moisture content of 10.5%. The biomass was used as such, without any pretreatment.
2.2. Extraction
The ultrasonic extraction was obtained using an Elma Transsonics ultrasonic bath (Schmidbauer GmbH, Singen, Germany) at a frequency of 40 kHz. The sample (10 g of plant material to which 100 mL of distilled water was added) was kept in the ultrasonic bath for 30 min at a temperature of 60 °C [
11]. The solution was filtered through the Buchner funnel; the filtrate was centrifuged for 5 min at 10,000 rpm; the supernatant obtained was transferred to a 100 mL volumetric flask and completed up to the mark with distilled water.
2.3. Study Design
The study was an in vivo experimental design. Ethical clearance to conduct the study was obtained from the Ethical Research Committee of George Emil Palade University of Medicine, Pharmacy, Sciences and Technology from Târgu Mures no. 1627/24.02.2022 and the Ethical Research Committee of Târgu Mureș Emergency Clinical County Hospital no. 2746/04.02.2022. The study was performed in the Oral and Maxillofacial Surgery Clinic from SCJU Târgu Mureș and the discipline of Oral and Maxillofacial Surgery from George Emil Palade University of Medicine, Pharmacy, Sciences and Technology from Târgu Mureș. The study was conducted according to the Declaration of Helsinki.
Between March 2022 and September 2022, 92 patients ranging from ages 18 and 35 years presented themselves for consultation, having symptoms that were later diagnosed as specific for the lower third molar eruption. Only 80 patients of them were selected for the study and then were divided into 4 equal groups of 20 subjects each.
Inclusion criteria: non-smoking patients with an erupting lower third molar presenting to the doctor for discomfort manifested by pain, trismus, and bleeding near the erupting tooth.
Exclusion criteria: diabetic patients, patients with gingivitis, patients who ceased antibiotic therapy in the last 3 months.
Patient grouping was performed according to the substance used for irrigation during treatment as follows: first group (control)—irrigation with saline solution; second group—irrigation with BBE; third group—irrigations with 0.2% chlorhexidine solution, fourth group—irrigations with BBE and chlorhexidine 0.2% solution in a ratio of 1:1.
The reasons why the patients presented to the doctor were: pain felt in the posterior mandibular area, trismus, and bleeding in the posterior mandibular area after brushing the teeth and after oral cavity rinsing.
2.4. Patient Protocol
The patients were informed about the way the study was conducted, the existing pathology, the procedures to be applied, and the patient’s informed consent was signed. The consent-providers were also assured of the anonymity and confidentiality of the study data. Patients showed interest in the study, many of them agreeing with the idea of using a natural product.
Applied working method:
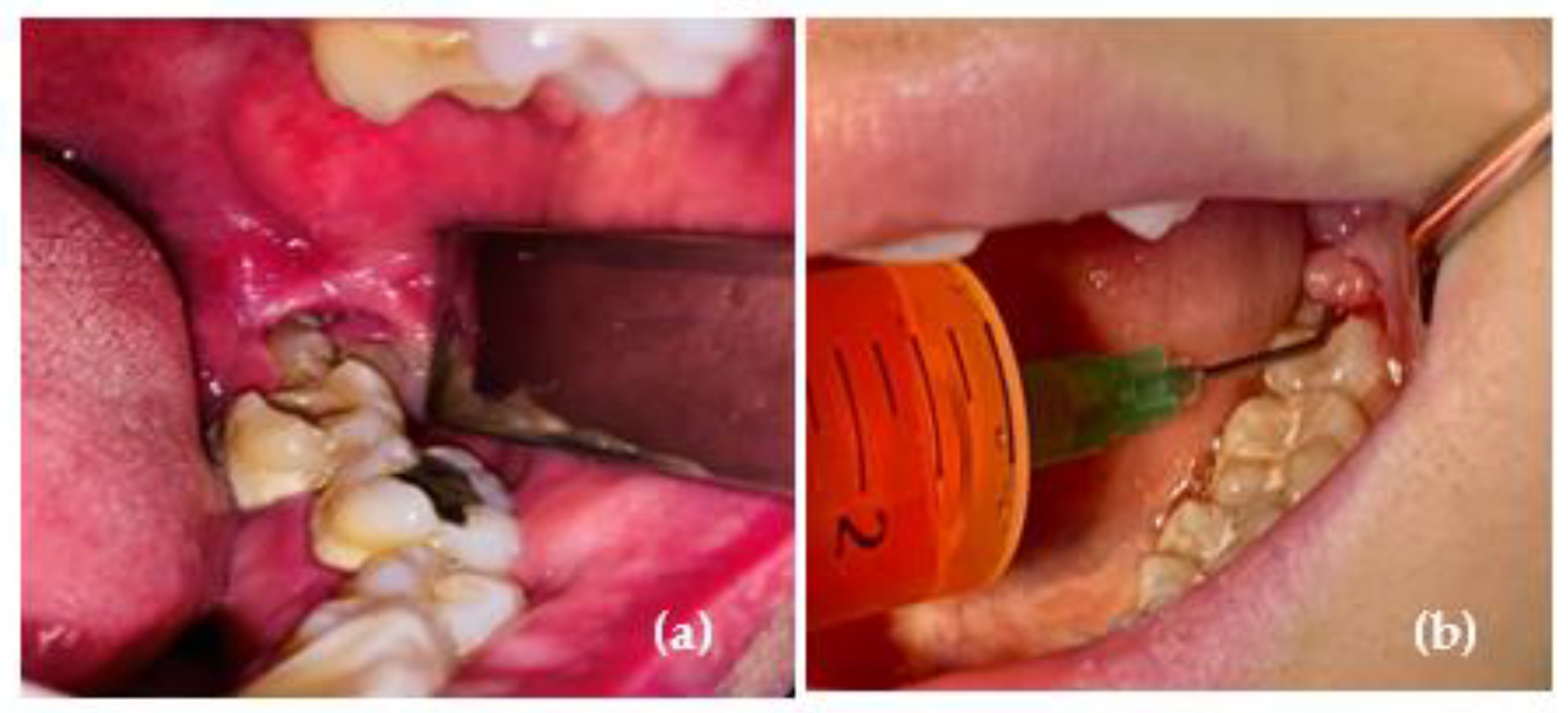
initial consultation, evaluation, and recording of the three parameters (pain, trismus, and bleeding) and local irrigation using 5 mL of solution according to the group to the group it belongs to (
Figure 1);
performing irrigation twice a day, for 2 consecutive days;
on the third day, final evaluation of the three parameters; assessment and registration to the patient files. Patients were told not to use anti-inflammatory pills and antibiotics during these three days.
2.5. Pain Assessment
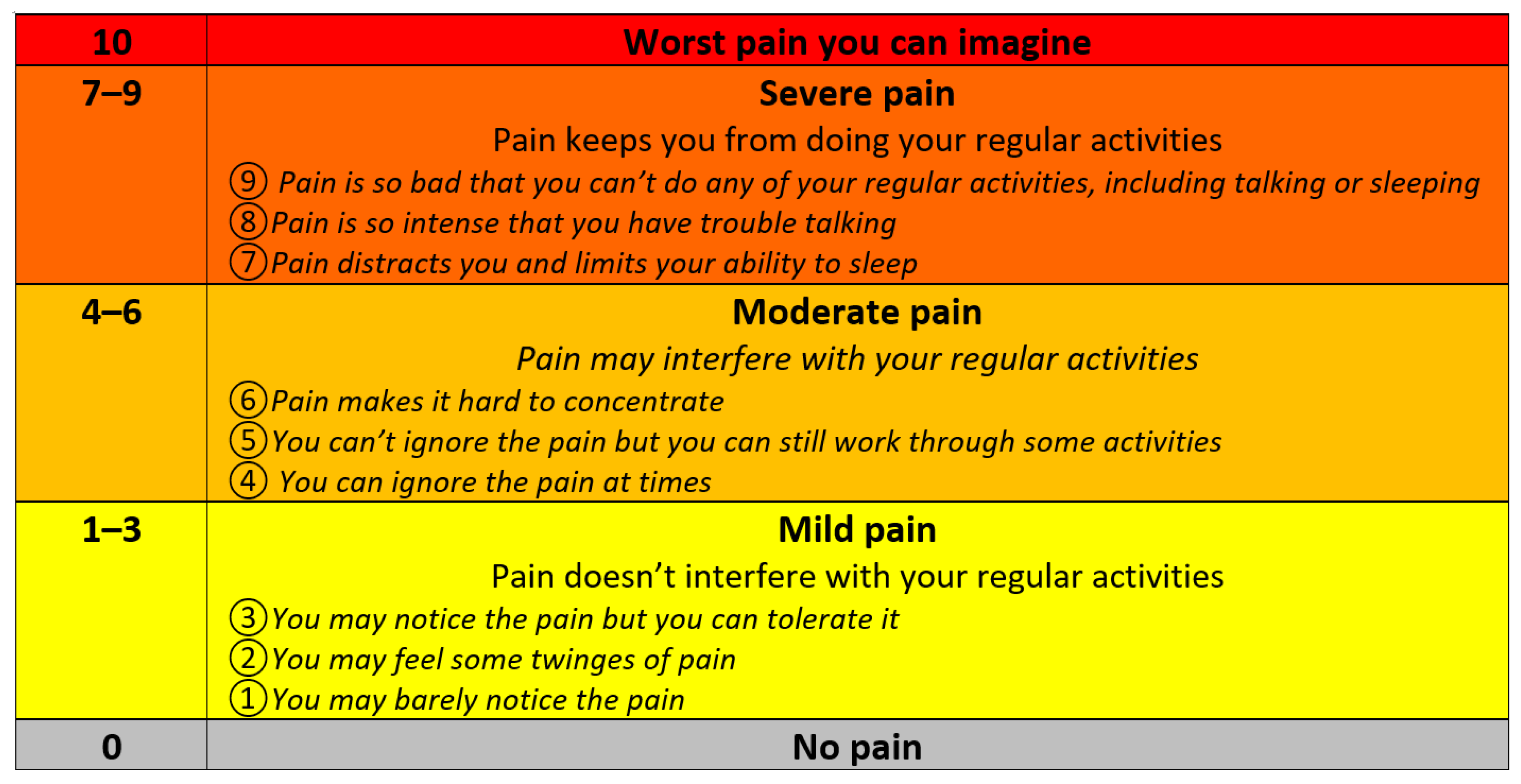
The Universal Pain Assessment Tool (UPAT) was used [
17], which uses items from 1 to 10 and classifies pain into 5 types: 0 = no pain; 1–3 = mild pain; 4–6 = moderate pain; 7–9 = severe pain; 10 = worst pain possible.
Each patient received a form explaining the level of pain (
Figure 2) and they were asked to choose on the formulary the level of pain they feel on the form they received. Additionally, they received an explanatory image of the pain level. The obtained values were entered into an Excel file, generating the average values and the representative graphs.
2.6. Trismus Assessment
The maximum distance between the edges of the upper and lower incisors is called the maximum interincisal opening (MIO), and it is widely used to objectively measure trismus. These measurements can be made using calipers or other devices [
18]. In this study, the measurement of the mouth opening was performed using the ruler and the patients were classified into 4 categories: 1 = maximum mouth opening of 4 cm; 2 = maximum mouth opening for 3 cm; 3 = maximum mouth opening for 2 cm; 4 = maximum mouth opening for 1 cm. The obtained values were entered into an Excel file, generating the average values and the representative graphs.
2.7. Assessment of Gingival Bleeding
For gingival bleeding, the Silness–Löe gingival index [
19] was used. This index has 4 levels: 0 = normal gingiva without inflammation, congestion, or bleeding; 1 = mild inflammation and congestion, absence of bleeding; 2 = mild inflammation, reduced erythema, and bleeding on probing; 3 = severe inflammation severe erythema, spontaneous bleeding tendency. The measurement was performed using a periodontal probe on the vestibular face of each tooth since access was easiest at this point for all patients. The obtained values were entered into an Excel file, generating the average values and the representative graphs.
2.8. Statistical Analysis
Data were statistically processed using IBM SPSS statistical analysis software (Version 25.0. IBM Corp., Armonk, NY, USA). The Kolmogorov–Smirnov test was used to assess the normality of data distribution to determine whether or not the values of a variable follow a normal distribution, and to determine the appropriate parametric or nonparametric test for each analysis. Levels of pain, inflammation/bleeding, and trismus were assessed for each group of patients before and after the irrigation sessions using the Wilcoxon test. The Kruskal–Wallis non-parametric test was also used to compare trismus rating and bleeding rating for the four solutions. The significance threshold was set, α = 0.05 which corresponds to a confidence level of 95%.
4. Discussion
Pericoronitis is a common inflammatory disease most frequently associated with the eruption of the mandibular third molar. However, the treatment of pericoronitis varies among specialists of dental medicine because no therapeutic protocol based on concrete evidence has been established yet to be able to minimize the period of localized pain at identifying the stage of the erupting tooth and other associated complications [
20].
Specialized literature shows the use of natural extracts in oral hygiene and prophylactic therapy. Other natural extracts, although they have demonstrated their effects, are still slightly studied and used in the field of dental medicine and used for treatment of various oral pathologies. There are studies demonstrating the antibacterial and antifungal effect of essential oils such as oregano, thyme, and green tea essential oil [
21], and a group of researchers demonstrated the inhibitory effect of essential oils on
Enterococcus faecalis present in the root canal [
22]. These data from the literature demonstrate the growing interest in natural therapy in the field of dental medicine and constitute an impetus for future research. Among natural bioactive compounds, spruce (
Picea abies L.) bark extract has been shown to be effective against gram-negative bacteria, such as
Pseudomonas Aeruginosa and
Klebsiella Pneumoniae [
23].
The microbiological profile associated with pericoronitis is mixed and difficult to highlight, because most of the patients present periodontal diseases with the presence of specific bacteria located in the gingival groove of the neighboring tooth, including species of
Streptococcus,
Staphylococcus, and
Fusobacterium [
5,
24]. The first-line treatment of acute pericoronitis is represented by local irrigation with various solutions, with the aim of removing food debris, reducing local inflammation, and limiting the transformation into a suppurative pericoronitis.
In pericoronitis, when the infection spreads, the indication for antibiotics use is essential. Any use of antibiotics to fight bacteria of all types produces over time or resistance of the body to this means of fighting the disease and their effective reduction. To avoid inappropriate and incorrect use, it is necessary to carry out the antibiogram for exact antibiotics treatment. Doctors need to be regularly trained in prescribing antibiotics, and they need to know that their inappropriate use can lead to antibiotic resistance over time. Since antibiotics are one of the most prescribed drugs, their consumption should be reported and statistically evaluated at regional, state, and global levels. If possible, it is recommended to avoid them and replace them with natural extract.
During pericoronitis management, early and adequate treatment is essential, and proper therapy reduces the patient’s discomfort and complications. This can also eliminate or reduce the need for antibiotic prescribing, thus decreasing the use of antibiotics and the risk of resistance development. These aspects, accentuated by the frequency of pericoronitis, are solid arguments for raising awareness of this disease, especially its efficient treatment [
10].
The large amounts of forest waste and the results regarding the antibacterial, antifungal and antioxidant effect of the beech extract were premised in testing the effect of this extract in the treatment of pericoronitis as an alternative to the use of chlorhexidine.
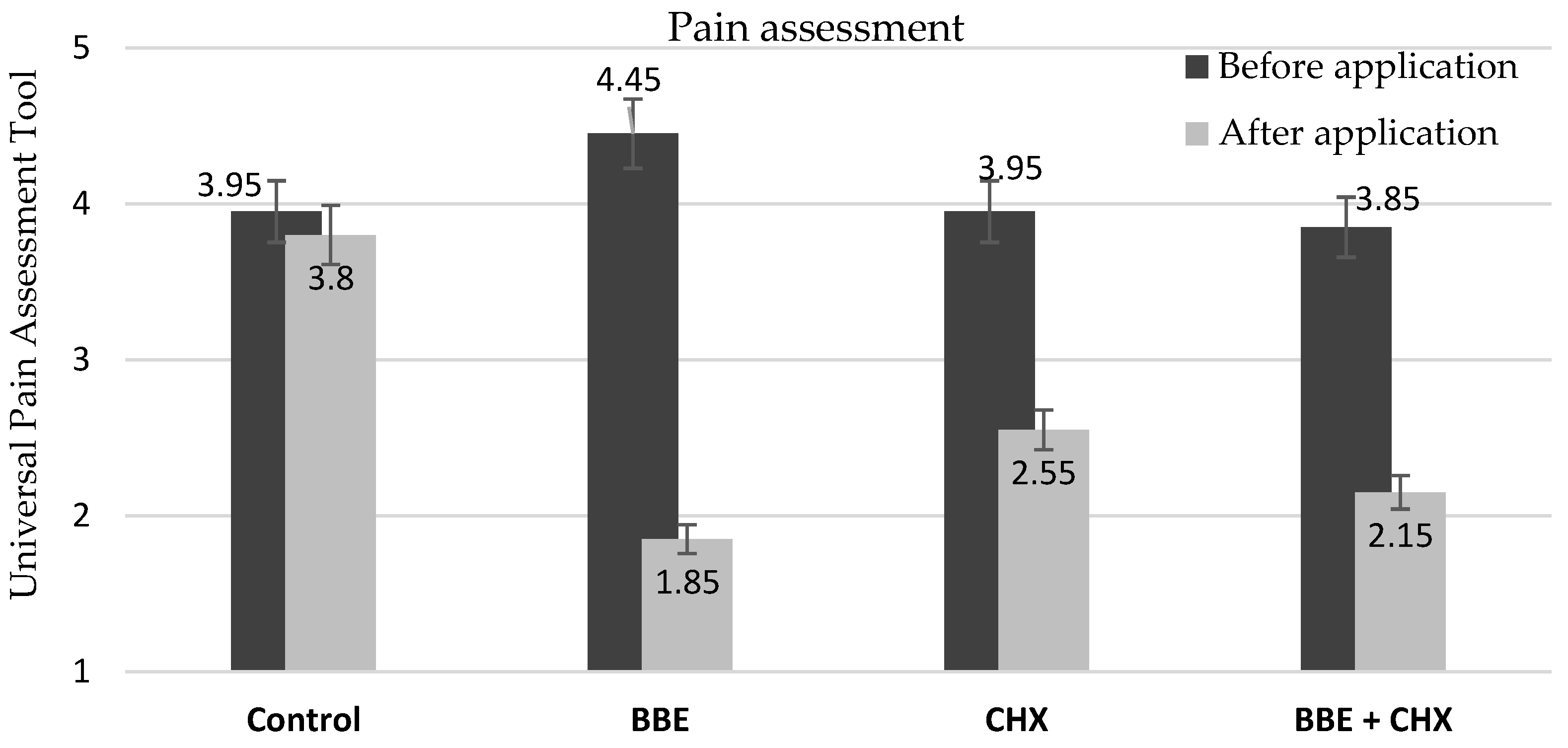
After treatment, the results of this study showed a decrease of pain in most of the patients and 75% of them registered a trismus with lower values, while in the case of 25% of the patients, the reported changes were insignificant. Although there is a limit of subjectivity related to what the patient feels which cannot be avoided, the decrease of pain intensity after irrigation was recorded for all patients with values of one, two, three, to four points on the pain scale. BBE achieved statistically significant values, with most patients reporting a decrease of pain intensity of 4–5 points on the universal pain rating scale. Patients treated with CHX and BBE + CHX had decreases in pain intensity of one, two, and three points each on the pain scale.
Compared to other similar studies [
6], 68% patients treated with CHX irrigations reported pain relief. Irrigation with BBE resulted in reduction of trismus for 85% of patients. On the other hand, for 25% of the patients, the associated pain was completely relieved. In case of irrigations using the mixed solution of BBE and CHX (ratio 1:1), the decrease of pain was similar to that of the group irrigated with CHX, and the trismus values decreased considerably, although 25% of the patients did not register improvements. This may be due to the fact that BBE has an antibacterial and analgesic effect. In the case of chlorhexidine, the antiseptic effect is well-known in the medical field, the antibacterial and anti-inflammatory effect, and the results obtained after the irrigations were materialized in a decrease of the values with different intensities on all levels, for all patients and all parameters: pain, bleeding, and trismus. Additionally, the mixture of chlorhexidine and BBE proved by the results that it maintained the antiseptic effect of chlorhexidine, and the properties of BBE maintained an antibacterial and anti-gingival inflammation effect.
Starting from the already existing evidence [
25] supporting the effectiveness of CHX in the control of microbial plaque, gingivitis, and the symptomatic management of some infections of the oral cavity, we observed that in the case of pericoronitis it confirmed both its effectiveness and its limits. In this context, our study aimed to demonstrate the efficacy of BBE in the primary treatment of pericoronitis of the lower third molar and to compare the effects of this extract with chlorhexidine.
We highlighted the beneficial effects of the BBE in the pathology of the eruption of third lower molars, more specifically in the case of pericoronitis, obtaining satisfactory results that were slightly superior to the chlorhexidine solution.
The results confirmed the effectiveness of BBE used in the treatment of congestive pericoronitis and open prospects for further use in field of dental medicine as a possible primary treatment in pericoronitis with or without the intake of an antiseptic chemical solution such as chlorhexidine and for the treatment of other oral pathologies. Of course, further studies are needed to deepen and characterize the effects on different types of microbial cultures and to establish the limits of effectiveness, and as with CHX, depending on the situation, the benefits should always be weighed against the disadvantages (see anaphylactic reactions to CHX, rare but still present and tooth staining).
Even if the effectiveness of CHX in controlling microbial plaque is demonstrated and accepted both in theory and in practice, in areas such as the prevention or treatment of certain conditions such as dental caries, chronic marginal periodontitis, and post-extraction alveolitis, the effectiveness is less proven [
14], and a variant of applying an alternative treatment with a natural antiseptic can be a solution.
Most of the patients involved in the study had a positive response to the presented treatment options, were cooperative, complied with the indications received during the study, and had a positive and open attitude regarding the availability of participation in this clinical study. Most of them were pleased that no antibiotics were used. Some patients were also not satisfied with the results obtained after the treatment, although they confidently participated in the study.