Prediction of Health Problems Using Deep Learning Images and Bio-Signals
Abstract
:1. Introduction
2. Related Work
2.1. Deep-Learning-Based Object Detection
2.2. Face Detection
2.3. Prediction of Health Status Using Bio-Signals
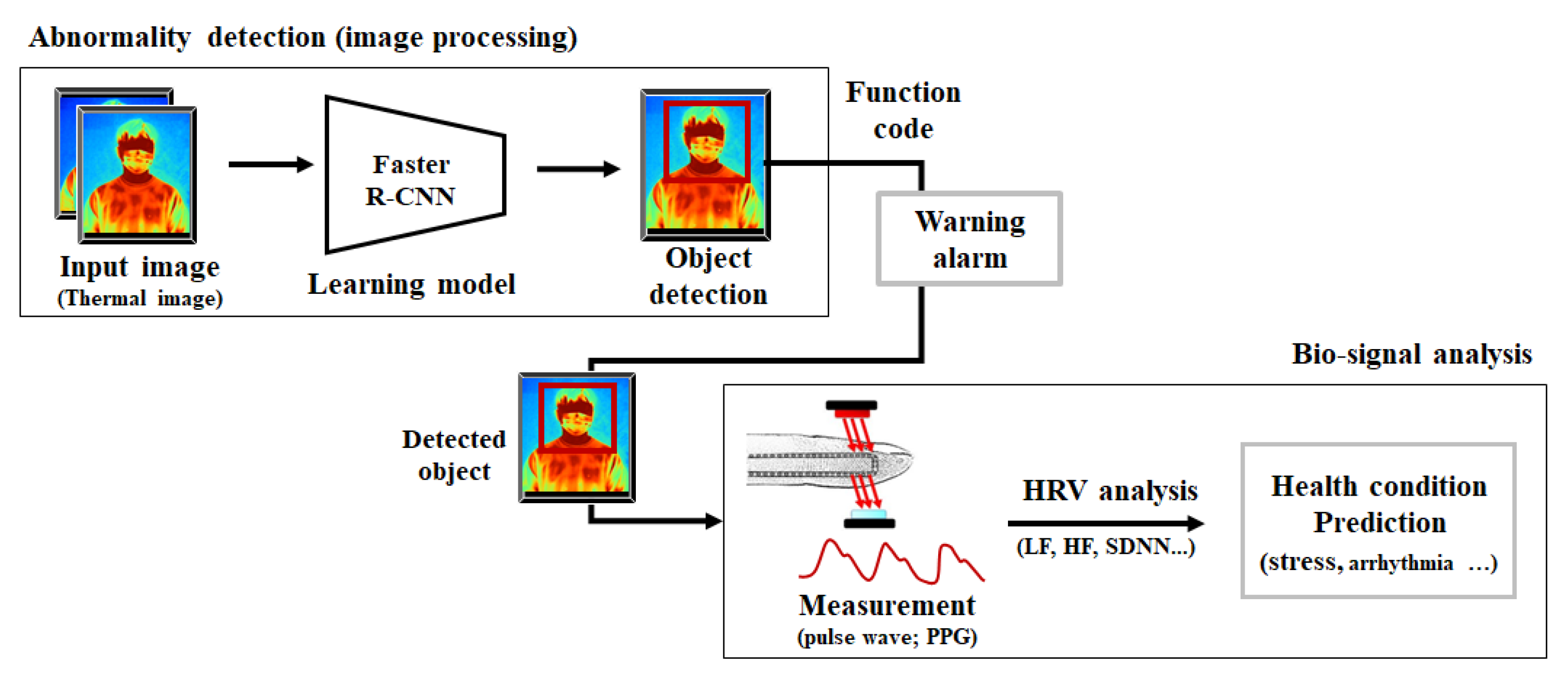
3. Materials and Methods
3.1. Object Detection in Thermal Image
3.1.1. Network Architecture
3.1.2. Learning
3.2. Prediction System of Health Status
3.2.1. Pulse Wave and HRV
3.2.2. Health Status and HRV
4. Experimentation and Discussion
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kim, H. The Response of A.I Systems in other Countries to Corona Virus(COVID-19) Infections: E-Government, Policy, A.I Utilizing Cases. J. Digit. Converg. 2020, 18, 479–493. [Google Scholar] [CrossRef]
- Lin, J.-W.; Lu, M.-H.; Lin, Y.-H.L. A Thermal Camera Based Continuous Body Temperature Measurement System. In Proceedings of the IEEE International Conference on Computer Vision Workshops (ICCVW), Seoul, Republic of Korea, 27–28 October 2019. [Google Scholar] [CrossRef]
- Ting, D.S.W.; Carin, L.; Dzau, V.; Wong, T.Y. Digital Technology and COVID-19. Nat. Med. 2020, 26, 459–461. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Teju, V.; Bhavana, D. An Efficient Object Detection Using OFSA for Thermal Imaging. Int. J. Electr. Eng. Educ. 2020. [Google Scholar] [CrossRef]
- Viola, P.; Jones, M. Rapid Object Detection Using a Boosted Cascade of Simple Features. In Proceedings of the 2001 IEEE Compute Society Conference on Computer Vision and Pattern Recognition (CVPR), Kauai, HI, USA, 8–14 December 2001. [Google Scholar] [CrossRef]
- Krizhevsky, A.; Sutskever, I.; Hinton, G.E. ImageNet Classification with Deep Convolutional Neural Networks. Adv. Neural Inf. Process. Syst. 2012, 25, 1–9. [Google Scholar] [CrossRef] [Green Version]
- Girshick, R.; Donahue, J.; Darrell, T.; Malik, J. Rich Feature Hierarchies for Accurate Object Detection and Semantic Segmentation. In Proceedings of the IEEE Conference on Computer Vision and Pattern Recognition (CVPR), Columbus, OH, USA, 23–28 June 2014; pp. 580–587. [Google Scholar] [CrossRef] [Green Version]
- Batomalaque, M.B.; Camacho, C.M.R.; Dalida, M.J.P.; Delmo, J.A.B. Image to Text Conversion Technique for Anti-Plagiarism System. IJASC 2019, 1, 1–9. [Google Scholar] [CrossRef]
- Ren, S.; He, K.; Girshick, R.; Sun, J. Faster R-CNN: Towards Real-Time Object Detection with Region Proposal Networks. IEEE Trans. Pattern Anal. Mach. Intell. 2017, 39, 1137–1149. [Google Scholar] [CrossRef] [Green Version]
- Redmon, J.; Divvala, S.; Girshick, R.; Farhadi, A. You Only Look Once: Unified, Real-Time Object Detection. In Proceedings of the IEEE Conference on Computer Vision and Pattern Recognition (CVPR), Las Vegas, NV, USA, 27–30 June 2016; pp. 779–788. [Google Scholar] [CrossRef]
- Jiang, H.; Learned-Miller, E. Face Detection with the Faster R-CNN. In Proceedings of the 2017 12th IEEE International Conference on Automatic Face & Gesture Recognition (FG 2017), Washington, DC, USA, 30 May–3 June 2017. [Google Scholar] [CrossRef] [Green Version]
- Yang, W.; Jiachun, Z. Real-Time Face Detection Based on YOLO. In Proceedings of the 2018 1st IEEE International Conference on Knowledge Innovation and Invention (ICKII), Jeju, Republic of Korea, 23–27 July 2018; pp. 221–224. [Google Scholar] [CrossRef]
- Fan, X.; Jiang, M. Retina FaceMask: A Single Stage Face Mask Detector for Assisting Control of the COVID-19 Pandemic. In Proceedings of the 2020 IEEE Computer Society Conference on Computer Vision and Pattern Recognition (CVPR), Melbourne, Australia, 17–20 October 2021. [Google Scholar] [CrossRef]
- Nemechek, P. Pulse rate variability as a biomarker of COVID-19 infection, hospital risk stratification, and post hospitalization recovery. Immunol. Infect. 2020, 1, 1–5. Available online: https://www.sciaeon.org/articles/Pulse-rate-variability-as-a-biomarker-of-COVID-19-infection-hospital-risk-stratification-and-post-hospitalization-recovery.pdf (accessed on 28 May 2021).
- Gingl, Z. A Photoplethysmograph Experiment for Microcontroller Labs. Int. J. Electr. Eng. Educ. 2012, 49, 42–60. [Google Scholar] [CrossRef] [Green Version]
- Suzuki, D.O.; Taques, B.O.; Marques, J.L. Electrocardiogram Experiment for Analog Electronic Laboratory. Int. J. Electr. Eng. Educ. 2015, 52, 248–263. [Google Scholar] [CrossRef]
- Beyaz, A. Air Quality Evaluation with a Low-cost Dust Sensor for a Hencoop. Agric. Sci. Dig. 2019, 39, 236–243. [Google Scholar] [CrossRef]
- Cui, F.; Yue, Y.; Zhang, Y.; Zhang, Z.; Zhou, H.S. Advancing biosensors with machine learning. ACS Sens. 2020, 5, 3346–3364. [Google Scholar] [CrossRef] [PubMed]
- Beyaz, A.; Ozkaya, M. Canopy analysis and thermographic abnormalities determination possibilities of olive trees by using data mining algorithms. Not. Bot. Horti Agrobot.-Cluj-Napoca 2021, 49, 12139. [Google Scholar] [CrossRef]
- Alhadrami, H.A. Biosensors: Classifications, medical applications, and future prospective. Biotechnol. Appl. Biochem. 2018, 65, 497–508. [Google Scholar] [CrossRef]
- Du, X.; Zhou, J. Application of biosensors to detection of epidemic diseases in animals. Res. Vet. Sci. 2018, 118, 444–448. [Google Scholar] [CrossRef] [PubMed]
- Miller, R.; Yazgan, I.; Sadik, O.A. Biosensors for the Detection of Emerging Plants and Animals Fungal Pathogens; Smart Biosensor Technology, CRC Press: Boca Raton, FL, USA, 2018; pp. 487–502. [Google Scholar] [CrossRef]
- Ambreen, L.; Sharma, G. Applications of biosensors in agriculture. Int. J. Mod. Agric. 2021, 10, 1089–1096. Available online: http://www.modern-journals.com/index.php/ijma/article/view/828 (accessed on 5 June 2022).
- Mohanraj, R. Biosensors for Emerging and Re-Emerging Infectious Diseases; Biotechnology and Applied Biochemistry; Elsevier: Amsterdam, The Netherlands, 2022; pp. 123–136. [Google Scholar]
- Mohankumar, P.; Ajayan, J.; Mohanraj, T.; Yasodharan, R. Recent developments in biosensors for healthcare and biomedical applications: A review. Measurement 2021, 167, 108293. [Google Scholar] [CrossRef]
- Liu, W.; Anguelov, D.; Erhan, D.; Szegedy, C.; Reed, S.; Fu, C.-Y.; Berg, A.C. SSD: Single Shot MultiBox Detector. In European Conference on Computer Vision; Springer: Cham, Switzerland, 2016; Volume 9905, pp. 21–37. [Google Scholar] [CrossRef]
- Lee, M.; Mun, H.-J. Comparison Analysis and Case Study for Deep Learning-Based Object Detection Algorithm. IJASC 2020, 2, 7–16. [Google Scholar] [CrossRef]
- Ranjan, R.; Patel, V.M.; Chellappa, R. HyperFace: A Deep Multi-Task Learning Framework for Face Detection, Landmark Localization, Pose Estimation, and Gender Recognition. IEEE Trans. Pattern Anal. Mach. Intell. 2019, 41, 121–135. [Google Scholar] [CrossRef] [Green Version]
- Lee, S.H. Deep Learning Based Face Mask Recognition for Access Control. J. Korea-Acad.-Ind. Coop. Soc. 2020, 21, 395–400. [Google Scholar] [CrossRef]
- Xue, B.; Hu, J.; Zhang, P. Intelligent Detection and Recognition System for Mask Wearing Based on Improved RetinaFace Algorithm. In Proceedings of the 2020 2nd International Conference on Machine Learning, Big Data and Business Intelligence (MLBDBI), Taiyuan, China, 23–25 October 2020. [Google Scholar] [CrossRef]
- Susanto, S.; Putra, F.A.; Analia, R.; Suciningtyas, I.K.L.N. The Face Mask Detection for Preventing the Spread of COVID-19 at Politeknik Negeri Batam. Available online: https://ieeexplore.ieee.org/document/9350556 (accessed on 28 May 2021).
- Lee, M.J.; Kim, Y.M.; Lim, Y.M. Masked Face Temperature Measurement System Using Deep Learning. J. Korea Multimed. Soc. 2021, 24, 208–214. [Google Scholar] [CrossRef]
- Kim, J.-H.; Kim, E.-K. Face Recognition and Temperature Measurement Access Control System Using Machine Learning. J. Korea Inst. Electron. Commun. Sci. 2021, 16, 197–202. [Google Scholar] [CrossRef]
- Lin, C.-H.; Wang, Z.-H.; Jong, G.-J. A De-Identification Face Recognition Using Extracted Thermal Features Based on Deep Learning. IEEE Sens. J. 2020, 20, 9510–9517. [Google Scholar] [CrossRef]
- Taelman, J.; Vandeput, S.; Spaepen, A.; Van Huffel, S. Influence of Mental Stress on Heart Rate and Heart Rate Variability. IFMBE Proc. 2009, 22, 1366–1369. [Google Scholar] [CrossRef]
- Thayer, J.F.; Åhs, F.; Fredrikson, M.; Sollers, J.J.; Wager, T.D. A Meta-Analysis of Heart Rate Variability and Neuroimaging Studies: Implications for Heart Rate Variability as a Marker of Stress and Health. Neurosci. Biobehav. Rev. 2012, 36, 747–756. [Google Scholar] [CrossRef] [PubMed]
- Negishi, T.; Abe, S.; Matsui, T.; Liu, H.; Kurosawa, M.; Kirimoto, T.; Sun, G. Contactless Vital Signs Measurement System Using RGB-Thermal Image Sensors and Its Clinical Screening Test on Patients with Seasonal Influenza. Sensors 2020, 20, 2171. [Google Scholar] [CrossRef] [Green Version]
- Kim, Y.; Park, Y.; Kim, J.; Chul, E.; Lee, E. Remote Heart Rate Monitoring Method Using Infrared Thermal Camera. Int. J. Eng. Res. Technol. 2018, 11, 493–500. [Google Scholar]
- Wang, Z.; Wang, F.; Ji, X. Analysis of Autonomic Nervous System Based on HRV. In Proceedings of the 2019 4th International Conference on Mechanical, Control and Computer Engineering (ICMCCE), Hohhot, China, 5–27 October 2019. [Google Scholar] [CrossRef]





| (a) Control group (normal body temperature) | ||||
| N | Pulse Variability | Mean BPM | SDNN | RMSSD |
| 1 | 44.68 | 77.90 | 58.65 | 38.00 |
| 2 | 39.78 | 74.50 | 55.90 | 42.10 |
| 3 | 35.23 | 77.00 | 73.80 | 44.10 |
| 4 | 34.25 | 76.00 | 66.00 | 40.20 |
| 5 | 35.62 | 75.12 | 63.20 | 43.05 |
| 6 | 38.57 | 74.14 | 67.35 | 44.26 |
| 7 | 37.25 | 72.54 | 65.00 | 41.00 |
| 8 | 35.42 | 76.00 | 71.00 | 44.25 |
| 9 | 37.14 | 74.12 | 69.54 | 46.00 |
| 10 | 38.52 | 77.00 | 57.85 | 39.45 |
| Average | 37.65 | 75.26 | 64.83 | 42.24 |
| (b) Experimental group (fever body temperature) | ||||
| N | Pulse Variability | Mean BPM | SDNN | RMSSD |
| 1 | 24.79 | 93.40 | 45.20 | 28.10 |
| 2 | 30.14 | 86.30 | 44.80 | 27.41 |
| 3 | 31.84 | 82.40 | 40.90 | 25.10 |
| 4 | 33.53 | 83.00 | 43.20 | 26.15 |
| 5 | 35.00 | 85.45 | 41.54 | 26.25 |
| 6 | 29.12 | 80.56 | 40.25 | 24.26 |
| 7 | 34.51 | 91.00 | 41.33 | 25.32 |
| 8 | 33.34 | 87.42 | 43.11 | 27.56 |
| 9 | 34.16 | 80.34 | 40.21 | 28.16 |
| 10 | 32.71 | 83.49 | 42.89 | 27.47 |
| Average | 31.91 | 85.34 | 42.34 | 26.58 |
| Detection Model | mAP (%) | Inference Speed (FPS) |
|---|---|---|
| Faster R-CNN (proposed system) | 76.4 | 5 |
| YOLO | 73.7 | 81 |
| SSD300 | 74.3 | 46 |
| Thermal Imaging System | Proposed System | |
|---|---|---|
| Face Detection (mask) | Yes | Yes |
| Body Temperature | Yes | Yes |
| HRV and Stress Prediction | No | Yes |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, M.-H.; Mun, H.-J.; Kang, S.-K. Prediction of Health Problems Using Deep Learning Images and Bio-Signals. Appl. Sci. 2022, 12, 12457. https://doi.org/10.3390/app122312457
Lee M-H, Mun H-J, Kang S-K. Prediction of Health Problems Using Deep Learning Images and Bio-Signals. Applied Sciences. 2022; 12(23):12457. https://doi.org/10.3390/app122312457
Chicago/Turabian StyleLee, Min-Hye, Hyung-Jin Mun, and Sun-Kyoung Kang. 2022. "Prediction of Health Problems Using Deep Learning Images and Bio-Signals" Applied Sciences 12, no. 23: 12457. https://doi.org/10.3390/app122312457






