Bringing CT Scanners to the Skies: Design of a CT Scanner for an Air Mobile Stroke Unit
Abstract
:Featured Application
Abstract
1. Introduction
2. Mobile Stroke Unit
3. Helicopter Emergency Medical Services and Air-MSU
3.1. HEMS Applications and Potential
3.2. Air-MSU Concept
3.3. Aircraft Selection
4. Mobile Head CT Scanner and Rotorcraft Retrofitting
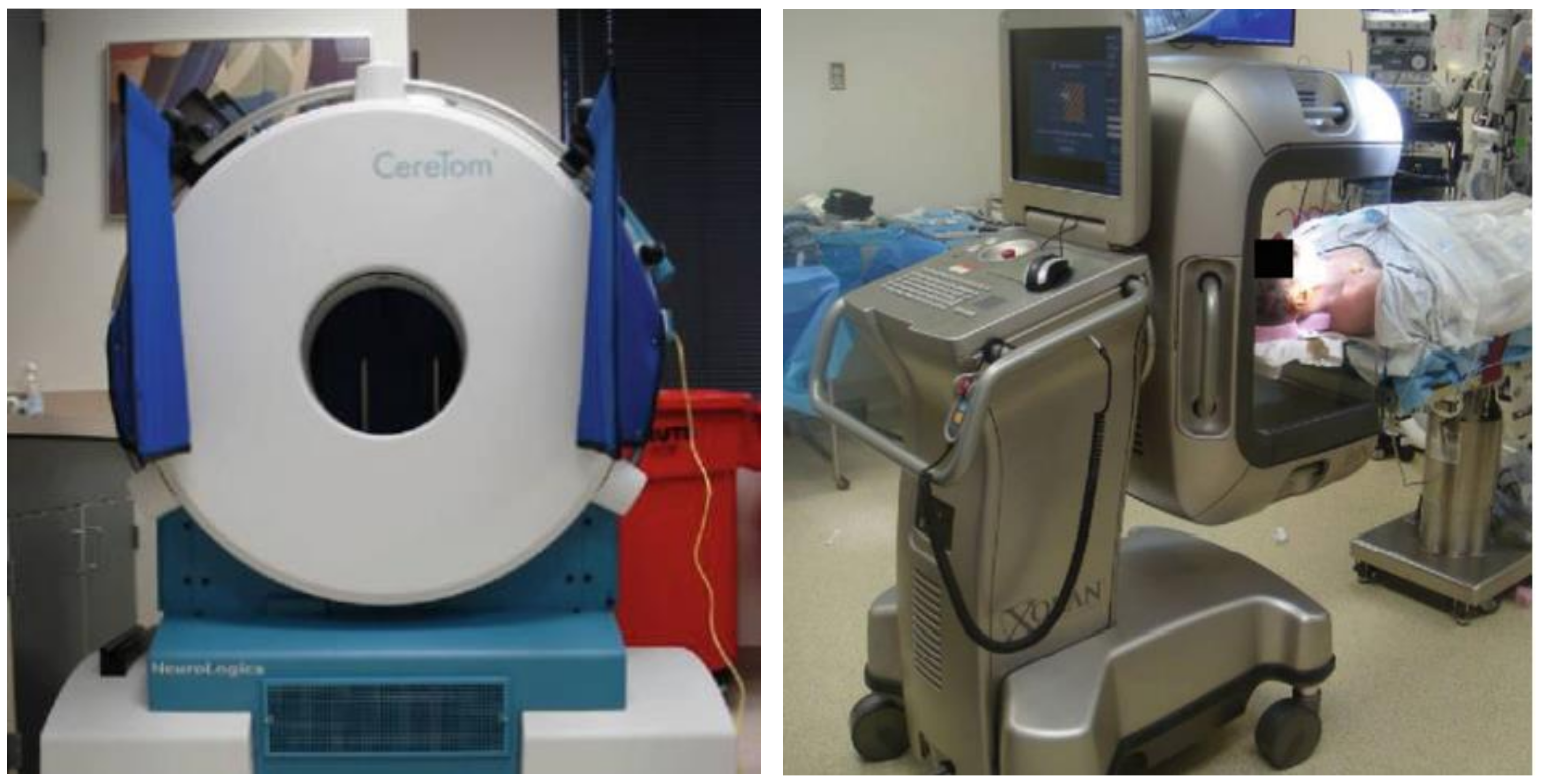
4.1. Types of Portable Head CT Scanners
4.2. Design Considerations for Retrofitting Head CT Scanners into Rotorcraft
- Major components of the mobile head CT scanner;
- Weight and size of the mobile head CT scanner;
- Actuation mechanism of the mobile head CT scanner.
4.2.1. Major Components of the Mobile Head CT Scanner
4.2.2. Weight and Size of the Mobile Head CT Scanner
4.2.3. Actuation Mechanism of the Mobile Head CT Scanner
4.2.4. CereTom and AgustaWestland AW189
5. So, How Can We Take It to the Skies?
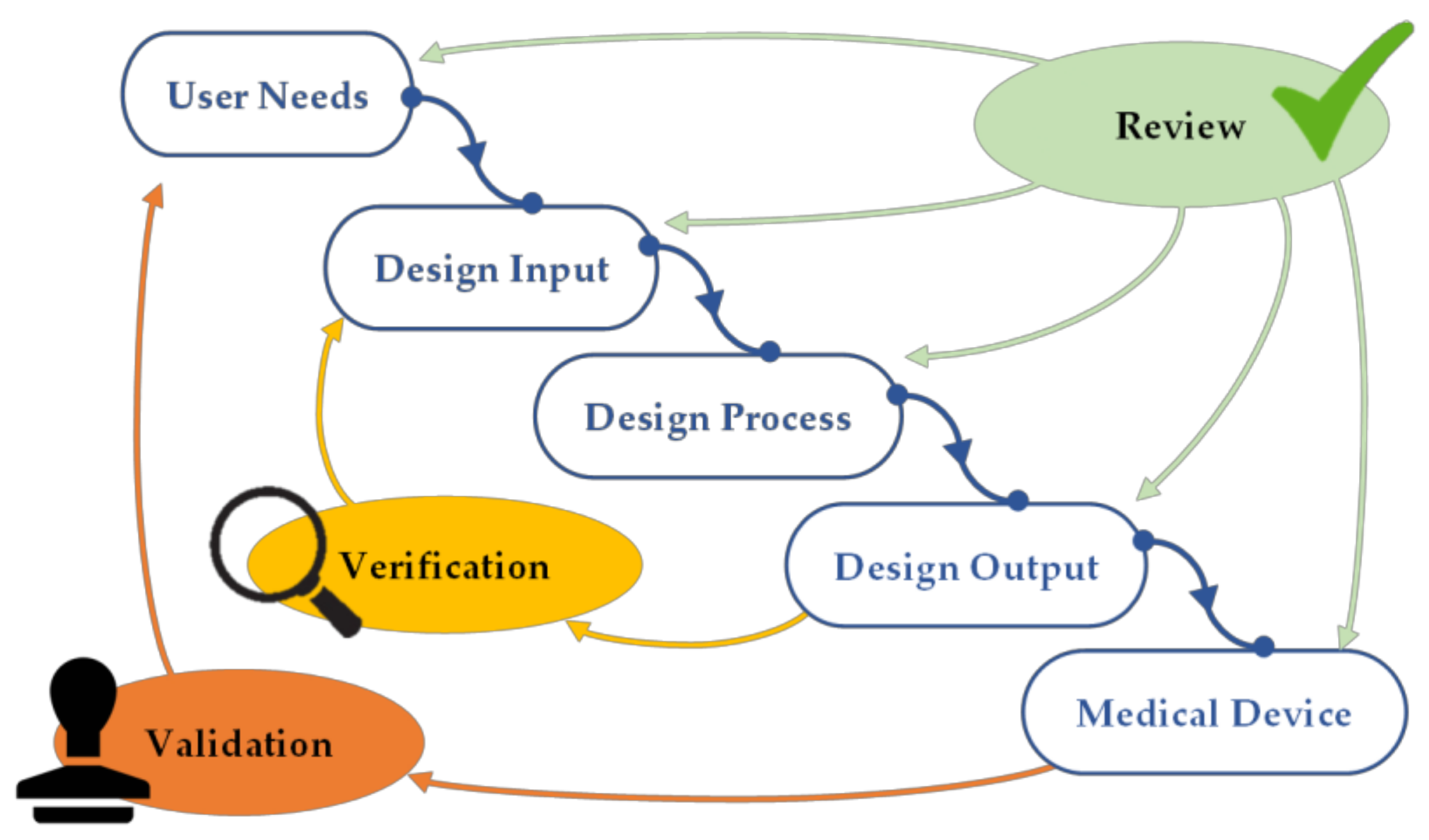
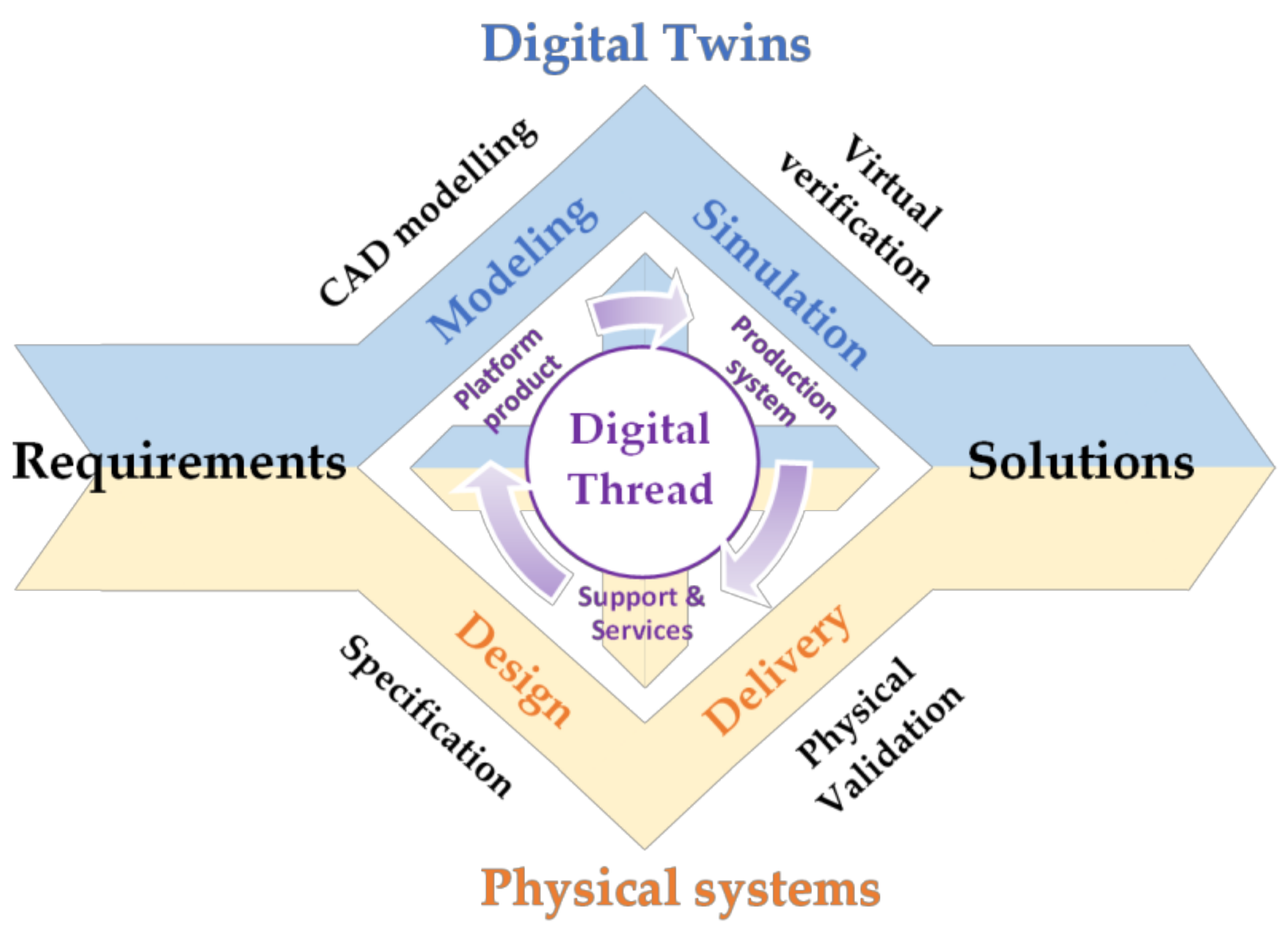
5.1. A Model-Based System Engineering Design (MBSE) Approach
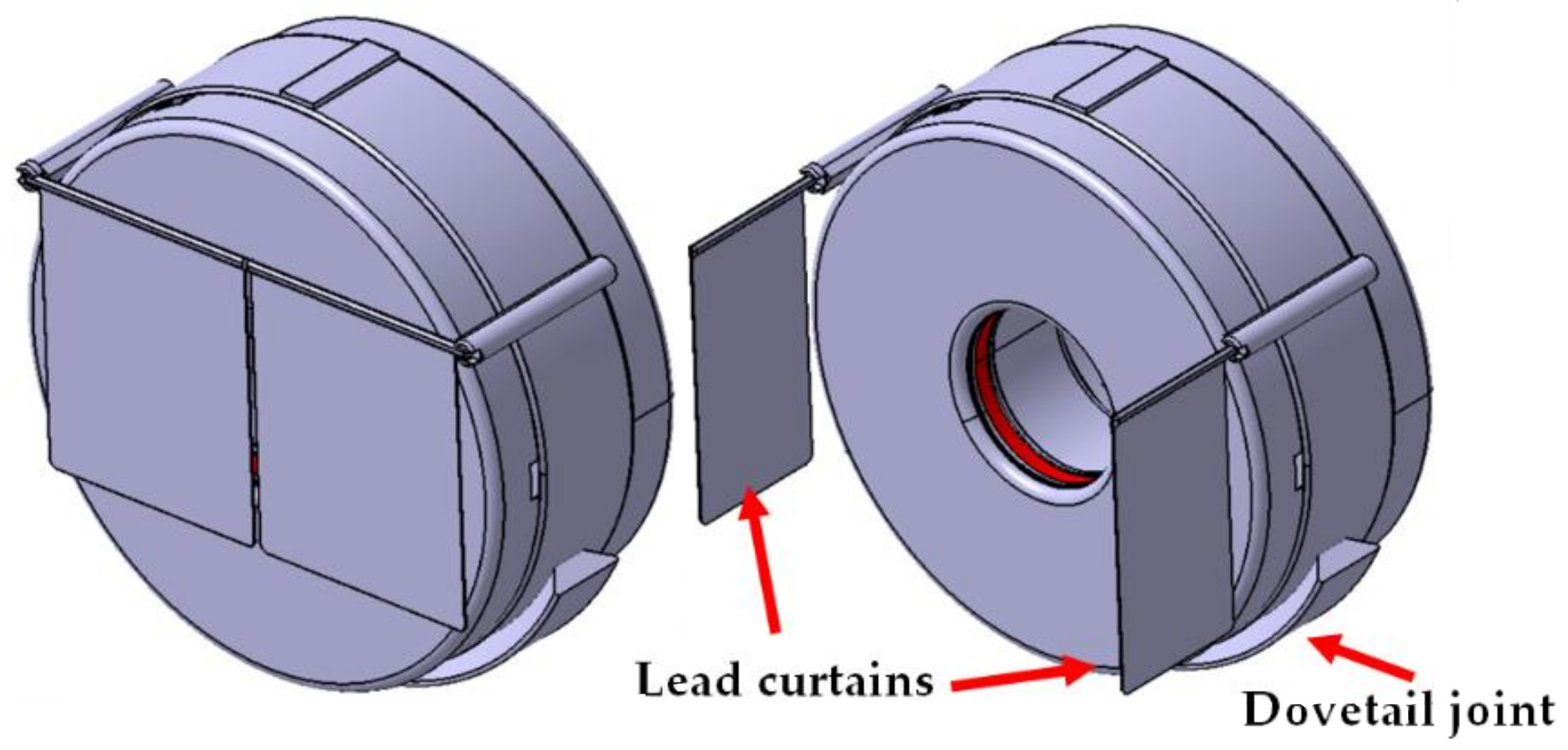
5.2. Reducing a Default CereTom Structure and Geometry
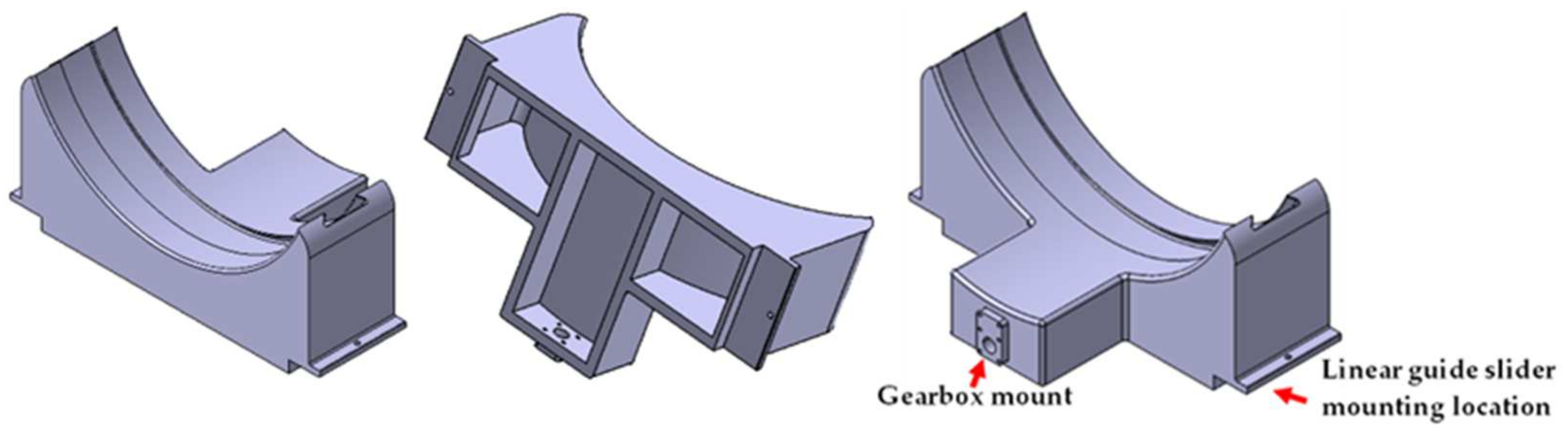
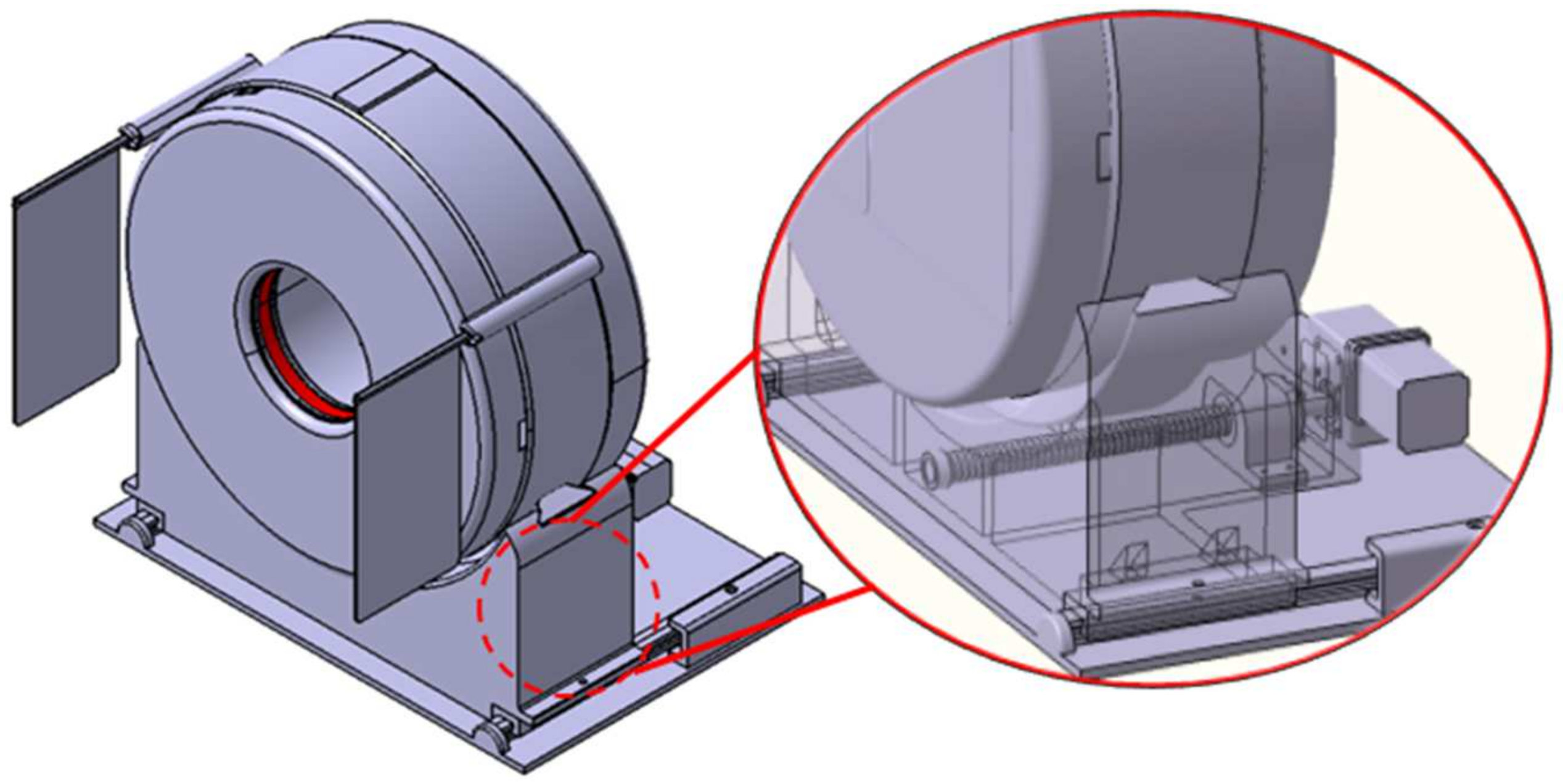
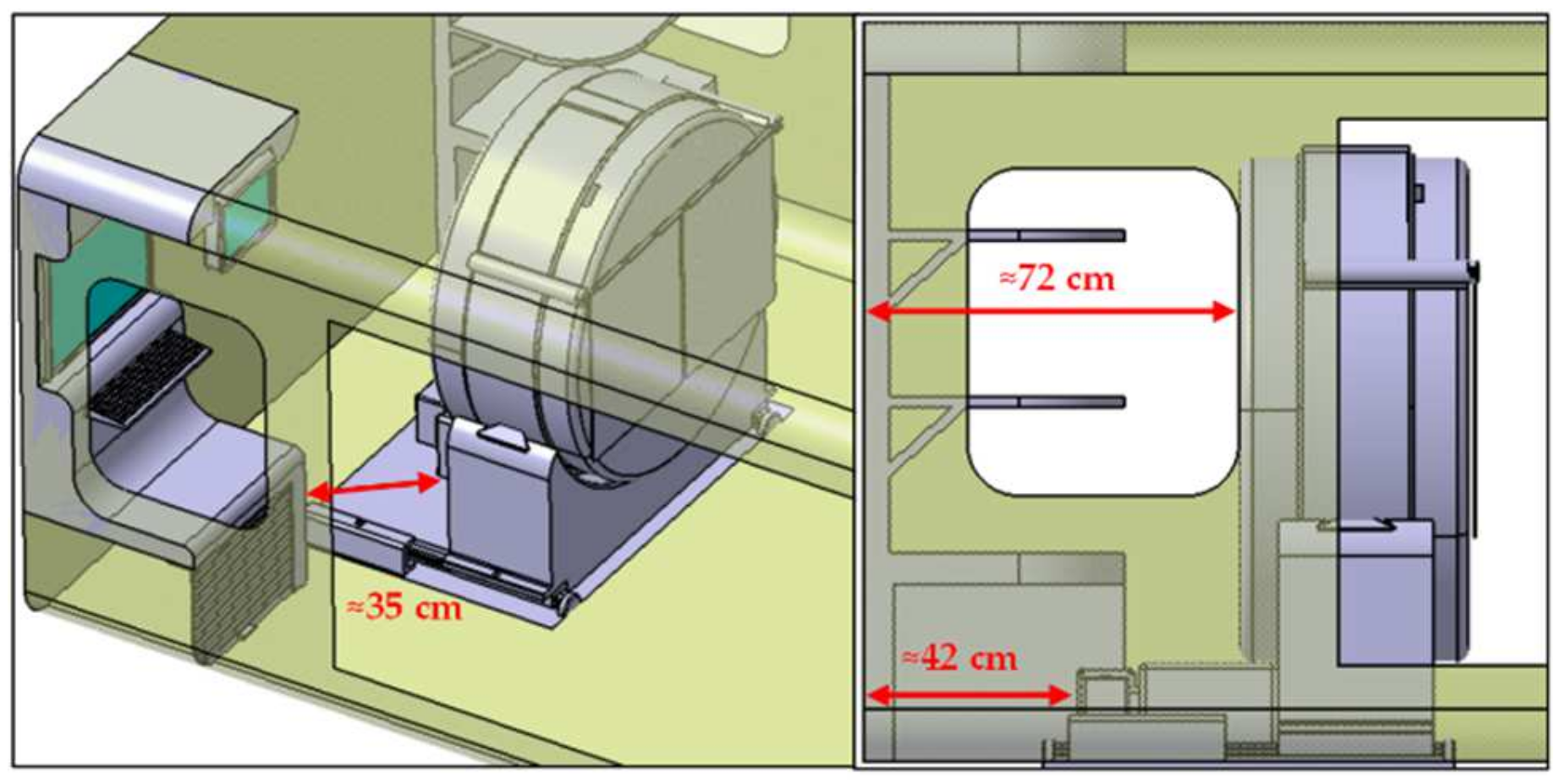
5.3. Designing a Support Structure for Reduced CereTom Gantry
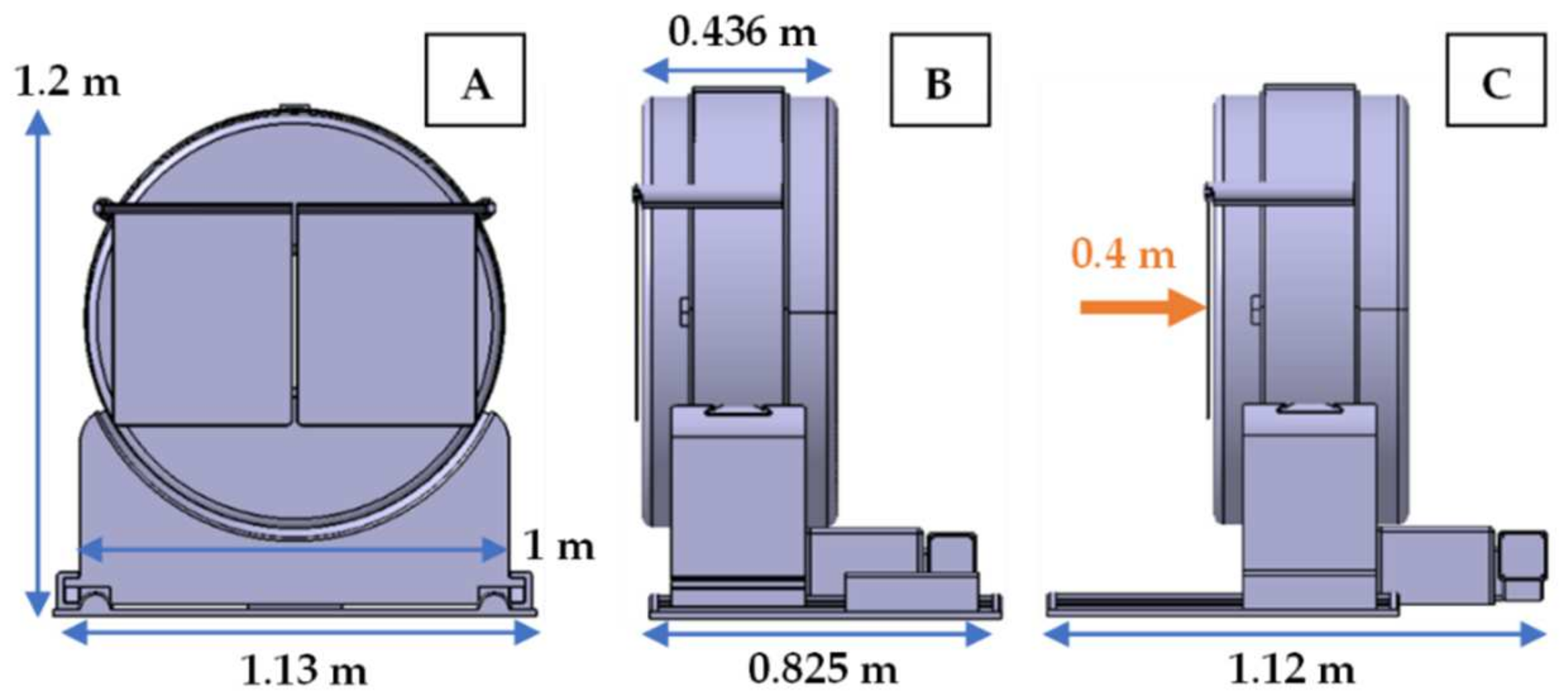
5.4. Designing a Base Plate for Proposed Support Structure and Full Assembly
5.5. How Do We Integrate into a AW189 Helicopter?
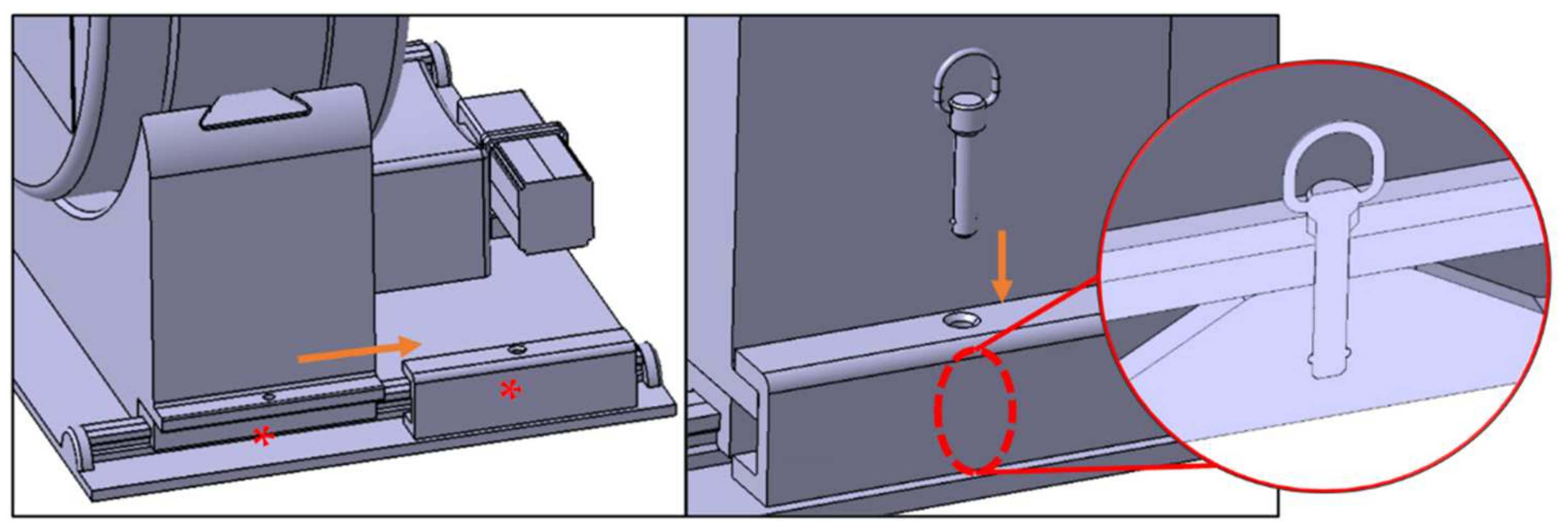
5.6. During Flight and Maintenance
6. Challenges and Perspectives
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Lewandowski, C.A.; Frankel, M.; Tomsick, T.A.; Broderick, J.; Frey, J.; Clark, W.; Starkman, S.; Grotta, J.; Spilker, J.; Khoury, J.; et al. Combined Intravenous and Intra-Arterial r-TPA Versus Intra-Arterial Therapy of Acute Ischemic Stroke. Stroke 1999, 30, 2598–2605. [Google Scholar] [CrossRef] [PubMed]
- Claiborne Johnston, S.; Fung, L.H.; Gillum, L.A.; Smith, W.S.; Brass, L.M.; Lichtman, J.H.; Brown, A.N. Utilization of Intravenous Tissue-Type Plasminogen Activator for Ischemic Stroke at Academic Medical Centers. Stroke 2001, 32, 1061–1068. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ma, H.; Campbell, B.C.V.; Parsons, M.W.; Churilov, L.; Levi, C.R.; Hsu, C.; Kleinig, T.J.; Wijeratne, T.; Curtze, S.; Dewey, H.M.; et al. Thrombolysis Guided by Perfusion Imaging up to 9 Hours after Onset of Stroke. N. Engl. J. Med. 2019, 380, 1795–1803. [Google Scholar] [CrossRef] [PubMed]
- Strbian, D.; Soinne, L.; Sairanen, T.; Happola, O.; Lindsberg, P.J.; Tatlisumak, T.; Kaste, M.; Helsinki Stroke Thrombolysis Registry, G. Ultraearly thrombolysis in acute ischemic stroke is associated with better outcome and lower mortality. Stroke 2010, 41, 712–716. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Emberson, J.; Lees, K.R.; Lyden, P.; Blackwell, L.; Albers, G.; Bluhmki, E.; Brott, T.; Cohen, G.; Davis, S.; Donnan, G.; et al. Effect of treatment delay, age, and stroke severity on the effects of intravenous thrombolysis with alteplase for acute ischaemic stroke: A meta-analysis of individual patient data from randomised trials. Lancet 2014, 384, 1929–1935. [Google Scholar] [CrossRef] [Green Version]
- Fassbender, K.; Walter, S.; Liu, Y.; Muehlhauser, F.; Ragoschke, A.; Kuehl, S.; Mielke, O. “Mobile Stroke Unit” for Hyperacute Stroke Treatment. Stroke 2003, 34, e44. [Google Scholar] [CrossRef]
- Walter, S.; Kostpopoulos, P.; Haass, A.; Helwig, S.; Keller, I.; Licina, T.; Schlechtriemen, T.; Roth, C.; Papanagiotou, P.; Zimmer, A.; et al. Bringing the hospital to the patient: First treatment of stroke patients at the emergency site. PLoS ONE 2010, 5, e13758. [Google Scholar] [CrossRef]
- Audebert, H.; Fassbender, K.; Hussain, M.S.; Ebinger, M.; Turc, G.; Uchino, K.; Davis, S.; Alexandrov, A.; Grotta, J.; Group, P. The PRE-hospital Stroke Treatment Organization. Int. J. Stroke 2017, 12, 932–940. [Google Scholar] [CrossRef] [Green Version]
- Grotta, J.C.; Yamal, J.-M.; Parker, S.A.; Rajan, S.S.; Gonzales, N.R.; Jones, W.J.; Alexandrov, A.W.; Navi, B.B.; Nour, M.; Spokoyny, I.; et al. Prospective, Multicenter, Controlled Trial of Mobile Stroke Units. N. Engl. J. Med. 2021, 385, 971–981. [Google Scholar] [CrossRef]
- Shuaib, A.; Jeerakathil, T.; Alberta Mobile Stroke Unit, I. The mobile stroke unit and management of acute stroke in rural settings. CMAJ 2018, 190, E855–E858. [Google Scholar] [CrossRef] [Green Version]
- Zhao, H.; Coote, S.; Easton, D.; Langenberg, F.; Stephenson, M.; Smith, K.; Bernard, S.; Cadilhac, D.A.; Kim, J.; Bladin, C.F.; et al. Melbourne Mobile Stroke Unit and Reperfusion Therapy: Greater Clinical Impact of Thrombectomy Than Thrombolysis. Stroke 2020, 51, 922–930. [Google Scholar] [CrossRef] [PubMed]
- Ehntholt, M.S.; Parasram, M.; Mir, S.A.; Lerario, M.P. Mobile Stroke Units: Bringing Treatment to the Patient. Curr. Treat. Options Neurol. 2020, 22, 5. [Google Scholar] [CrossRef]
- Fassbender, K.P.; Grotta, J.C.P.; Walter, S.M.D.; Grunwald, I.Q.P.; Ragoschke-Schumm, A.M.D.; Saver, J.L.P. Mobile stroke units for prehospital thrombolysis, triage, and beyond: Benefits and challenges. Lancet Neurol. 2017, 16, 227–237. [Google Scholar] [CrossRef]
- Zhao, H.; Campbell, B.C.V.; Foster, S.; Stephenson, M.; Coote, S.; Langenberg, F.; Easton, D.; Donnan, G.A.; Davis, S.M. Advances in pre-hospital care—Operational experiences from the Melbourne mobile stroke unit. Vessel Plus 2021, 5, 2021. [Google Scholar] [CrossRef]
- Cadilhac, D.A.; Kilkenny, M.F.; Longworth, M.; Pollack, M.R.; Levi, C.R.; Metropolitan Clinical, T.; Stroke Services New South Wales Coordinating, C. Metropolitan-rural divide for stroke outcomes: Do stroke units make a difference? Intern. Med. J. 2011, 41, 321–326. [Google Scholar] [CrossRef]
- Parker, S.A.; Kus, T.; Bowry, R.; Gutierrez, N.; Cai, C.; Yamal, J.M.; Rajan, S.; Wang, M.; Jacob, A.P.; Souders, C.; et al. Enhanced dispatch and rendezvous doubles the catchment area and number of patients treated on a mobile stroke unit. J. Stroke Cerebrovasc. Dis. 2020, 29, 104894. [Google Scholar] [CrossRef] [PubMed]
- Tonsager, K.; Rehn, M.; Ringdal, K.G.; Lossius, H.M.; Virkkunen, I.; Osteras, O.; Roislien, J.; Kruger, A.J. Collecting core data in physician-staffed pre-hospital helicopter emergency medical services using a consensus-based template: International multicentre feasibility study in Finland and Norway. BMC Health Serv. Res. 2019, 19, 151. [Google Scholar] [CrossRef] [Green Version]
- Thomas, S.H.; Kociszewski, C.; Schwamm, L.H.; Wedel, S.K. The evolving role of helicopter emergency medical services in the transfer of stroke patients to specialized centers. Prehosp. Emerg. Care 2002, 6, 210–214. [Google Scholar] [CrossRef] [PubMed]
- Hutton, C.F.; Fleming, J.; Youngquist, S.; Hutton, K.C.; Heiser, D.M.; Barton, E.D. Stroke and Helicopter Emergency Medical Service Transports: An Analysis of 25,332 Patients. Air Med. J. 2015, 34, 348–356. [Google Scholar] [CrossRef]
- Gardiner, F.W.; Bishop, L.; Dos Santos, A.; Sharma, P.; Easton, D.; Quinlan, F.; Churilov, L.; Schwarz, M.; Walter, S.; Fassbender, K.; et al. Aeromedical Retrieval for Stroke in Australia. Cerebrovasc. Dis. 2020, 49, 334–340. [Google Scholar] [CrossRef]
- Walter, S.; Zhao, H.; Easton, D.; Bil, C.; Sauer, J.; Liu, Y.; Lesmeister, M.; Grunwald, I.Q.; Donnan, G.A.; Davis, S.M.; et al. Air-Mobile Stroke Unit for access to stroke treatment in rural regions. Int. J. Stroke 2018, 13, 568–575. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bil, C.; Walter, S.; Sauer, J.; Feldmann, S. Towards an Air Mobile Stroke Unit for Rapid Medical Response in Rural Australia. Adv. Transdiscipl. Eng. 2019, 10, 465–474. [Google Scholar] [CrossRef]
- European Union Aviation Safety Agency. Type Certificate Data Sheet No.: EASA.R.510 AW189. Available online: https://www.easa.europa.eu/document-library/type-certificates/rotorcraft-cs-29-cs-27-cs-vlr/easar510 (accessed on 19 September 2021).
- Civil Aviation Safety Authority. Cabin Interior & Cargo Compartment Flammability. Available online: https://www.casa.gov.au/aircraft/airworthiness/continuing-airworthiness/airworthiness-bulletins (accessed on 19 September 2021).
- Leonardo. AW189. Available online: https://www.leonardocompany.com/en/products/aw189-1 (accessed on 5 September 2021).
- Rumboldt, Z.; Huda, W.; All, J.W. Review of portable CT with assessment of a dedicated head CT scanner. AJNR Am. J. Neuroradiol. 2009, 30, 1630–1636. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Neurologica. OmniTom. Available online: https://www.neurologica.com/mobile-ct/omnitom (accessed on 20 September 2021).
- SIEMENS Healthineers. SOMATOM on Site. Available online: https://www.siemens-healthineers.com/nl/computed-tomography/mobile-head-ct/somatom-on-site#TECHNICAL_SPECIFICATIONS (accessed on 20 September 2021).
- Balachandran, R.; Schurzig, D.; Fitzpatrick, J.M.; Labadie, R.F. Evaluation of portable CT scanners for otologic image-guided surgery. Int. J. Comput. Assist. Radiol. Surg. 2012, 7, 315–321. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gupta, R.; Grasruck, M.; Suess, C.; Bartling, S.H.; Schmidt, B.; Stierstorfer, K.; Popescu, S.; Brady, T.; Flohr, T. Ultra-high resolution flat-panel volume CT: Fundamental principles, design architecture, and system characterization. Eur. Radiol. 2006, 16, 1191–1205. [Google Scholar] [CrossRef] [PubMed]
- Cerejo, R.; John, S.; Buletko, A.B.; Taqui, A.; Itrat, A.; Organek, N.; Cho, S.M.; Sheikhi, L.; Uchino, K.; Briggs, F.; et al. A Mobile Stroke Treatment Unit for Field Triage of Patients for Intraarterial Revascularization Therapy. J. Neuroimaging 2015, 25, 940–945. [Google Scholar] [CrossRef] [PubMed]
- Childs, P.R.N. 1—Design. In Mechanical Design Engineering Handbook, 2nd ed.; Childs, P.R.N., Ed.; Butterworth-Heinemann: Oxford, UK, 2019; pp. 1–47. [Google Scholar]
- Van Norman, G.A. Drugs and Devices: Comparison of European and U.S. Approval Processes. JACC Basic Transl. Sci. 2016, 1, 399–412. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Grieves, M.; Vickers, J. Digital Twin: Mitigating Unpredictable, Undesirable Emergent Behavior in Complex Systems. In Transdisciplinary Perspectives on Complex Systems; Springer: Berlin/Heidelberg, Germany, 2017; pp. 85–113. [Google Scholar]
- Neurologica. CereTom Elite Data Sheet 1-NL3000-065rev13; Neurologica Corporation: Danvers, MA, USA, 2020; Available online: https://www.neurologica.com/mobile-ct/ceretom-elite (accessed on 20 September 2021).






| CT Scanner Model | Manufacturer | Weight | Dimensions (cm) | ||
|---|---|---|---|---|---|
| Height | Width | Depth | |||
| CereTom [26] | Neurologica (Samsung) | 438 kg | 153 | 134 | 73 |
| OmniTom [27] | Neurologica (Samsung) | 726 kg | 152.4 | 137.7 | 73.9 |
| xCAT [26] | Xoran Technologies | 236 kg | 170 | 119 | 81 |
| SOMATOM On.site [28] | Siemens | 998 kg | 155 | 160 | 74 |
| CT Scanner Components | Role | Keep/Remove/Modify | Justification |
|---|---|---|---|
| X-ray tube | Emits X-ray, which goes through the patient’s head and is received by the detectors. | Keep | Primary functional component of CT scanner. |
| Detector | Receives the X-ray emitted from the X-ray tube, which will be used to process X-ray images. | Keep | Primary functional component of CT scanner. |
| Rotating drum | A rotating support where both the X-ray tube and detector are attached diametrically opposite. | Keep | Limited modifiability as it may severely affect the function of the CT scanner. |
| Support frame | Supports the structural weight of the CT scanner. | Modify | The size and correspondingly weight can be further reduced to fit into nominated aircraft, however not compromising on structural integrity. |
| Gantry Cover | Conceals all the internal components of the CT scanner. | Modify | Will be modified according to the shape of the support frame. |
| Caster wheel | Aids hospital staff in maneuvering the CT scanner with ease. | Remove | Not required as the CT scanner will not be mobile once attached to the aircraft interior. |
| Battery | Power source for the CT scanner. | Keep | Must be retained to serve as backup power source for the CT scanner. |
| Processor | Computes and processes transmitted data from the detectors into a greyscale image. | Keep | Primary functional component of CT scanner. |
| Caterpillar tracks | Drives the movement for the entire CT scanner. | Remove | No longer used as the driving mechanism for the CT scanner. |
| Motor | Drives the caterpillar tracks. | Remove | Caterpillar tracks are no longer in use. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kwok, J.S.; Fox, K.; Bil, C.; Langenberg, F.; Balabanski, A.H.; Dos Santos, A.; Bivard, A.; Gardiner, F.; Bladin, C.; Parsons, M.; et al. Bringing CT Scanners to the Skies: Design of a CT Scanner for an Air Mobile Stroke Unit. Appl. Sci. 2022, 12, 1560. https://doi.org/10.3390/app12031560
Kwok JS, Fox K, Bil C, Langenberg F, Balabanski AH, Dos Santos A, Bivard A, Gardiner F, Bladin C, Parsons M, et al. Bringing CT Scanners to the Skies: Design of a CT Scanner for an Air Mobile Stroke Unit. Applied Sciences. 2022; 12(3):1560. https://doi.org/10.3390/app12031560
Chicago/Turabian StyleKwok, Jun Sheng, Kate Fox, Cees Bil, Francesca Langenberg, Anna H. Balabanski, Angela Dos Santos, Andrew Bivard, Fergus Gardiner, Christopher Bladin, Mark Parsons, and et al. 2022. "Bringing CT Scanners to the Skies: Design of a CT Scanner for an Air Mobile Stroke Unit" Applied Sciences 12, no. 3: 1560. https://doi.org/10.3390/app12031560
APA StyleKwok, J. S., Fox, K., Bil, C., Langenberg, F., Balabanski, A. H., Dos Santos, A., Bivard, A., Gardiner, F., Bladin, C., Parsons, M., Zhao, H., Coote, S., Levi, C., De Aizpurua, H., Campbell, B., Davis, S. M., Donnan, G. A., Easton, D., & Pang, T. Y. (2022). Bringing CT Scanners to the Skies: Design of a CT Scanner for an Air Mobile Stroke Unit. Applied Sciences, 12(3), 1560. https://doi.org/10.3390/app12031560







