How to Prevent Aseptic Loosening in Cementless Arthroplasty: A Review
Abstract
1. Introduction
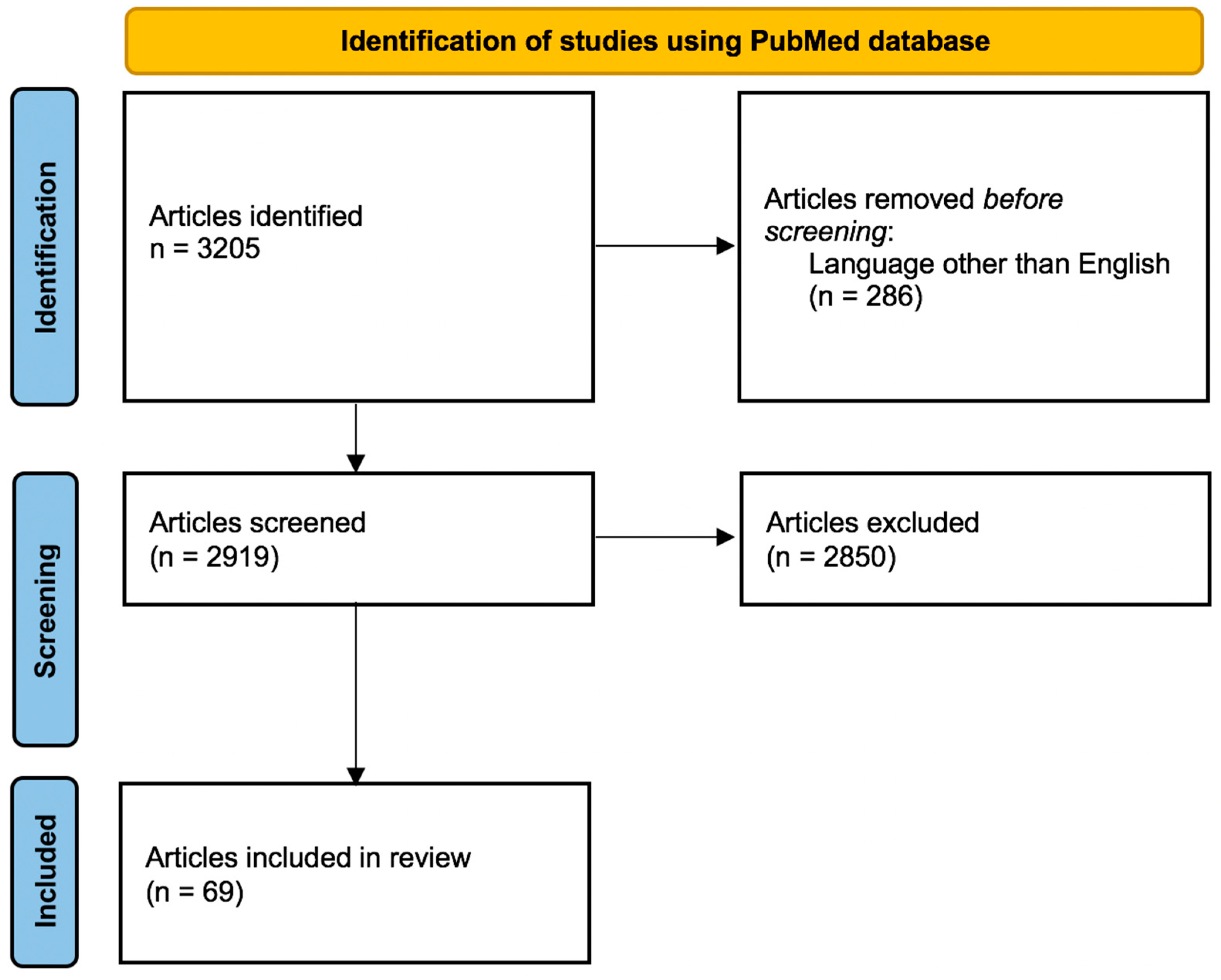
2. Pathophysiology of Aseptic Loosening
3. Materials and Methods
4. Implant Properties
4.1. Acetabular Cup
4.1.1. Alloy
4.1.2. Surface Treatment
4.1.3. Design
4.2. Femoral Stem
4.2.1. Alloy
4.2.2. Surface Treatment
4.2.3. Design
4.3. Bearing Surfaces
5. Surgical Factors
5.1. Surgeon
5.2. Hospital
5.3. Approach
5.4. Acetabular Screws
6. Patient-Related Factors
6.1. Demographics
6.2. Genetics
6.3. Comorbidities
6.3.1. Obesity
6.3.2. Hyperglycemia
6.3.3. Rheumatoid Arthritis
6.3.4. Avascular Necrosis of the Femoral Head
6.3.5. Hip Dysplasia
6.3.6. Sickle Cell Disease and Hemophilia
6.3.7. Spinal Fusion
6.4. Smoking
7. Postoperative Protocol
8. Perioperative Drugs
8.1. Antiosteoporotic Drugs
8.2. Opioids
8.3. Statins
8.4. Beta-Blockers
8.5. Other Drugs
9. Experimental Studies on the Process of Osseointegration
10. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Hailer, N.P.; Garellick, G.; Kärrholm, J. Uncemented and cemented primary total hip arthroplasty in the Swedish Hip Arthroplasty Register. Acta Orthop. 2010, 81, 34–41. [Google Scholar] [CrossRef] [PubMed]
- Haragus, H.; Prejbeanu, R.; Poenaru, D.V.; Deleanu, B.; Timar, B.; Vermesan, D. Cross-cultural adaptation and validation of a patient-reported hip outcome score. Int. Orthop. 2018, 42, 1001–1006. [Google Scholar] [CrossRef] [PubMed]
- Abu-Amer, Y.; Darwech, I.; Clohisy, J.C. Aseptic loosening of total joint replacements: Mechanisms underlying osteolysis and potential therapies. Arthritis Res. 2007, 9 (Suppl. S1), S6. [Google Scholar] [CrossRef] [PubMed]
- Parithimarkalaignan, S.; Padmanabhan, T.V. Osseointegration: An update. J. Indian Prosthodont. Soc. 2013, 13, 2–6. [Google Scholar] [CrossRef]
- Goodman, S.B.; Gallo, J. Periprosthetic Osteolysis: Mechanisms, Prevention and Treatment. J. Clin. Med. 2019, 8, 2091. [Google Scholar] [CrossRef]
- Hoskins, W.; Rainbird, S.; Holder, C.; Graves, S.E.; Bingham, R. Revision for Aseptic Loosening of Highly Porous Acetabular Components in Primary Total Hip Arthroplasty an Analysis of 20,993 Total Hip Replacements. J. Arthroplast. 2021, 37, 312–315. [Google Scholar] [CrossRef]
- Apostu, D.; Lucaciu, O.; Berce, C.; Lucaciu, D.; Cosma, D. Current methods of preventing aseptic loosening and improving osseointegration of titanium implants in cementless total hip arthroplasty: A review. J. Int. Med. Res. 2018, 46, 2104–2119. [Google Scholar] [CrossRef]
- Wegrzyn, J.; Kaufman, K.R.; Hanssen, A.D.; Lewallen, D.G. Performance of Porous Tantalum vs. Titanium Cup in Total Hip Arthroplasty: Randomized Trial with Minimum 10-Year Follow-Up. J. Arthroplast. 2015, 30, 1008–1013. [Google Scholar] [CrossRef]
- Matharu, G.S.; Judge, A.; Murray, D.W.; Pandit, H.G. Trabecular Metal Acetabular Components Reduce the Risk of Revision Following Primary Total Hip Arthroplasty: A Propensity Score Matched Study From the National Joint Registry for England and Wales. J. Arthroplast. 2018, 33, 447–452. [Google Scholar] [CrossRef]
- Lazarinis, S.; Mäkelä, K.T.; Eskelinen, A.; Havelin, L.; Hallan, G.; Overgaard, S.; Pedersen, A.B.; Kärrholm, J.; Hailer, N.P. Does hydroxyapatite coating of uncemented cups improve long-term survival? An analysis of 28,605 primary total hip arthroplasty procedures from the Nordic Arthroplasty Register Association (NARA). Osteoarthr. Cartil. 2017, 25, 1980–1987. [Google Scholar] [CrossRef]
- Palomäki, A.; Hemmilä, M.; Laaksonen, I.; Matilainen, M.; Eskelinen, A.; Haapakoski, J.; Puhto, A.P.; Kettunen, J.; Manninen, M.; Mäkelä, K. Implant Survival of 6,080 Tritanium Cups in Primary Total Hip Arthroplasty: Data from the Finnish Arthroplasty Register from 2009 to 2017. J. Bone Jt. Surg. Am. 2020, 102, 1177–1185. [Google Scholar] [CrossRef] [PubMed]
- Otten, V.; Mukka, S.; Nilsson, K.; Crnalic, S.; Kärrholm, J. Uncemented cups with and without screw holes in primary THA: A Swedish Hip Arthroplasty Register study with 22,725 hips. Acta Orthop. 2019, 90, 258–263. [Google Scholar] [CrossRef] [PubMed]
- Gallen, R.A.; Khan, R.J.K.; Haebich, S.J.; Karamfiles, S.H.; Khan, H. Solid Cup vs Cluster Hole in Total Hip Arthroplasty: A 10-Year Randomized Control Trial. J. Arthroplast. 2018, 33, 1113–1119. [Google Scholar] [CrossRef] [PubMed]
- Keurentjes, J.C.; Pijls, B.G.; Van Tol, F.R.; Mentink, J.F.; Mes, S.D.; Schoones, J.W.; Fiocco, M.; Sedrakyan, A.; Nelissen, R.G. Which implant should we use for primary total hip replacement? A systematic review and meta-analysis. J. Bone Jt. Surg. Am. 2014, 96 (Suppl. S1), 79–97. [Google Scholar] [CrossRef]
- Knutsen, A.R.; Lau, N.; Longjohn, D.B.; Ebramzadeh, E.; Sangiorgio, S.N. Periprosthetic femoral bone loss in total hip arthroplasty: Systematic analysis of the effect of stem design. Hip Int. 2017, 27, 26–34. [Google Scholar] [CrossRef]
- Hailer, N.P.; Lazarinis, S.; Mäkelä, K.T.; Eskelinen, A.; Fenstad, A.M.; Hallan, G.; Havelin, L.; Overgaard, S.; Pedersen, A.B.; Mehnert, F.; et al. Hydroxyapatite coating does not improve uncemented stem survival after total hip arthroplasty! Acta Orthop. 2015, 86, 18–25. [Google Scholar] [CrossRef]
- Chen, Y.L.; Lin, T.; Liu, A.; Shi, M.M.; Hu, B.; Shi, Z.I.; Yan, S. Does hydroxyapatite coating have no advantage over porous coating in primary total hip arthroplasty? A meta-analysis. J. Orthop. Surg. Res. 2015, 10, 21. [Google Scholar] [CrossRef]
- Piolanti, N.; Neri, E.; Bonicoli, E.; Parchi, P.D.; Marchetti, S.; Manca, M.; Bonini, L.; Banci, L.; Scaglione, M. Use of a Plasma-Sprayed Titanium-Hydroxyapatite Femoral Stem in Hip Arthroplasty in Patients Older than 70 Years. Is Cementless Fixation a Reliable Option in the Elderly? J. Clin. Med. 2021, 10, 4735. [Google Scholar] [CrossRef]
- Wagner, M.; Schönthaler, H.; Endstrasser, F.; Dammerer, D.; Nardelli, P.; Brunner, A. Mid-Term Results After 517 Primary Total Hip Arthroplasties With a Shortened and Shoulderless Double-Taper Press-Fit Stem: High Rates of Aseptic Loosening. J. Arthroplast. 2021, 37, 97–102. [Google Scholar] [CrossRef]
- Khanuja, H.S.; Vakil, J.J.; Goddard, M.S.; Mont, M.A. Cementless Femoral Fixation in Total Hip Arthoplasty. J. Bone Jt. Surg. 2021, 93, 500–509. [Google Scholar] [CrossRef]
- Hoskins, W.T.; Bingham, R.J.; Lorimer, M.; de Steiger, R.N. The Effect of Size for a Hydroxyapatite-Coated Cementless Implant on Component Revision in Total Hip Arthroplasty: An Analysis of 41,265 Stems. J. Arthroplast. 2020, 35, 1074–1078. [Google Scholar] [CrossRef] [PubMed]
- Jaeger, S.; Uhler, M.; Schroeder, S.; Beckmann, N.A.; Braun, S. Comparison of Different Locking Mechanisms in Total Hip Arthroplasty: Relative Motion between Cup and Inlay. Materials 2020, 13, 1392. [Google Scholar] [CrossRef] [PubMed]
- Sharplin, P.; Wyatt, M.C.; Rothwell, A.; Frampton, C.; Hooper, G. Which is the best bearing surface for primary total hip replacement? A New Zealand Joint Registry study. Hip Int. 2018, 28, 352–362. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.K.; Yoon, B.H.; Choi, Y.S.; Jo, W.L.; Ha, Y.C.; Koo, K.H. Metal on Metal or Ceramic on Ceramic for Cementless Total Hip Arthroplasty: A Meta-Analysis. J. Arthroplast. 2017, 31, 2637–2645.e1. [Google Scholar] [CrossRef]
- Shang, X.; Fang, Y. Comparison of Ceramic-on-Ceramic vs. Ceramic-on-Polyethylene for Primary Total Hip Arthroplasty: A Meta-Analysis of 15 Randomized Trials. Front. Surg. 2021, 16, 751121. [Google Scholar] [CrossRef]
- van Loon, J.; Sierevelt, I.N.; Spekenbrink-Spooren, A.; Opdam, K.T.; Poolman, R.W.; Kerkhoffs, G.M.; Haverkamp, D. Higher risk of 2-year cup revision of ceramic-on-ceramic versus ceramic-on-polyethylene bearing: Analysis of 33,454 primary press-fit total hip arthroplasties registered in the Dutch Arthroplasty Register (LROI). Hip Int. 2022, 11207000211064975. [Google Scholar] [CrossRef] [PubMed]
- Varnum, C. Outcomes of different bearings in total hip arthroplasty—Implant survival, revision causes, and patient-reported outcome. Dan Med. J. 2017, 64, B5350. [Google Scholar]
- Vendittoli, P.A.; Shahin, M.; Rivière, C.; Barry, J.; Lavoie, P.; Duval, N. Ceramic-on-ceramic total hip arthroplasty is superior to metal-on-conventional polyethylene at 20-year follow-up: A randomised clinical trial. Orthop. Traumatol. Surg. Res. 2021, 107, 102744. [Google Scholar] [CrossRef] [PubMed]
- Hernigou, P.; Trousselier, M.; Roubineau, F.; Bouthors, C.; Flouzat Lachaniette, C.H. Dual-mobility or Constrained Liners Are More Effective Than Preoperative Bariatric Surgery in Prevention of THA Dislocation. Clin. Orthop. Relat. Res. 2016, 474, 2202–2210. [Google Scholar] [CrossRef]
- Berry, D.J.; Abdel, M.P. Dual-Mobility Constructs in Primary and Revision Total Hip Arthroplasty: A Systematic Review of Comparative Studies. J. Arthroplast. 2019, 34, 594–603. [Google Scholar] [CrossRef] [PubMed]
- Kreipke, R.; Rogmark, C.; Pedersen, A.B.; Kärrholm, J.; Hallan, G.; Havelin, L.I.; Mäkelä, K.; Overgaard, S. Dual Mobility Cups: Effect on Risk of Revision of Primary Total Hip Arthroplasty Due to Osteoarthritis: A Matched Population-Based Study Using the Nordic Arthroplasty Register Association Database. J. Bone Jt. Surg. Am. 2019, 101, 169–176. [Google Scholar] [CrossRef] [PubMed]
- Jonker, R.C.; van Beers, L.W.A.H.; van der Wal, B.C.H.; Vogely, H.C.; Parratte, S.; Castelein, R.M.; Poolman, R.W. Can dual mobility cups prevent dislocation without increasing revision rates in primary total hip arthroplasty? A systematic review. Orthop. Traumatol. Surg. Res. 2020, 106, 509–517. [Google Scholar] [CrossRef] [PubMed]
- Darrith, B.; Courtney, P.M.; Della Valle, C.J. Outcomes of dual mobility components in total hip arthroplasty: A systematic review of the literature. Bone Jt. J. 2018, 100, 11–19. [Google Scholar] [CrossRef] [PubMed]
- Hoskins, W.; Rainbird, S.; Lorimer, M.; Graves, S.E.; Bingham, R. What Can We Learn From Surgeons Who Perform THA and TKA and Have the Lowest Revision Rates? A Study from the Australian Orthopaedic Association National Joint Replacement Registry. Clin. Orthop. Relat. Res. 2021. Epub ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Bron, D.M.; Wolterbeek, N.; Poolman, R.W.; Kempen, D.H.; Delawi, D. Resident training does not influence the complication risk in total knee and hip arthroplasty. Acta Orthop. 2021, 92, 689–694. [Google Scholar] [CrossRef] [PubMed]
- Hoskins, W.; Rainbird, S.; Peng, Y.; Graves, S.E.; Bingham, R. The Effect of Surgical Approach and Femoral Prosthesis Type on Revision Rates Following Total Hip Arthroplasty: An Analysis of the Most Commonly Utilized Cementless Stems. J. Bone Jt. Surg. Am. 2021, 104, 24–32. [Google Scholar] [CrossRef]
- Huang, X.T.; Lium, D.G.; Jia, B.; Xu, Y.X. Comparisons between Direct Anterior Approach and Lateral Approach for Primary Total Hip Arthroplasty in Postoperative Orthopaedic Complications: A Systematic Review and Meta-Analysis. Orthop. Surg. 2021, 13, 1707–1720. [Google Scholar] [CrossRef]
- Hoskins, W.; Bingham, R.; Lorimer, M.; Hatton, A.; de Steiger, R.N. Early Rate of Revision of Total Hip Arthroplasty Related to Surgical Approach: An Analysis of 122,345 Primary Total Hip Arthroplasties. J. Bone Jt. Surg. Am. 2020, 102, 1874–1882. [Google Scholar] [CrossRef]
- Docter, S.; Philpott, H.T.; Godkin, L.; Bryant, D.; Somerville, L.; Jennings, M.; Marsh, J.; Lanting, B. Comparison of intra and post-operative complication rates among surgical approaches in Total Hip Arthroplasty: A systematic review and meta-analysis. J. Orthop. 2020, 20, 310–325. [Google Scholar] [CrossRef]
- Mjaaland, K.E.; Svenningsen, S.; Fenstad, A.M.; Havelin, L.I.; Furnes, O.; Nordsletten, L. Implant Survival After Minimally Invasive Anterior or Anterolateral Vs. Conventional Posterior or Direct Lateral Approach: An Analysis of 21,860 Total Hip Arthroplasties from the Norwegian Arthroplasty Register (2008 to 2013). J. Bone Jt. Surg. Am. 2017, 99, 840–847. [Google Scholar] [CrossRef]
- Natera, L.; Valera, M.; Gómez, E.M.; Ibañez, N.; Crusi, X.; Sancho, R. Survival of hydroxyapatite-coated cups: Acetabular screws involve a lower rate of revision surgery due to aseptic loosening. Hip Int. 2017, 27, 153–161. [Google Scholar] [CrossRef] [PubMed]
- Bayliss, L.E.; Culliford, D.; Monk, A.P.; Glyn-Jones, S.; Prieto-Alhambra, D.; Judge, A.; Cooper, C.; Carr, A.J.; Arden, N.K.; Beard, D.J.; et al. The effect of patient age at intervention on risk of implant revision after total replacement of the hip or knee: A population-based cohort study. Lancet 2017, 389, 1424–1430, Erratum in Lancet 2017, 389, 1398. [Google Scholar] [CrossRef]
- Ormsby, R.T.; Solomon, L.B.; Stamenkov, R.; Findlay, D.M.; Atkins, G.J. Evidence for Gender-Specific Bone Loss Mechanisms in Periprosthetic Osteolysis. J. Clin. Med. 2019, 9, 53. [Google Scholar] [CrossRef]
- Prokopetz, J.J.; Losina, E.; Bliss, R.L.; Wright, J.; A Baron, J.; Katz, J.N. Risk factors for revision of primary total hip arthroplasty: A systematic review. BMC Musculoskelet. Disord. 2012, 13, 251. [Google Scholar] [CrossRef]
- Koks, S.; Wood, D.J.; Reimann, E.; Awiszus, F.; Lohmann, C.H.; Bertrand, J.; Prans, E.; Maasalu, K.; Martson, A. The Genetic Variations Associated With Time to Aseptic Loosening After Total Joint Arthroplasty. J. Arthroplast. 2020, 35, 981–988. [Google Scholar] [CrossRef]
- MacInnes, S.J.; Hatzikotoulas, K.; Fenstad, A.M.; Shah, K.; Southam, L.; Tachmazidou, I.; Hallan, G.; Dale, H.; Panoutsopoulou, K.; Furnes, O.; et al. The 2018 Otto Aufranc Award: How Does Genome-wide Variation Affect Osteolysis Risk After THA? Clin. Orthop. Relat. Res. 2019, 477, 297–309. [Google Scholar] [CrossRef] [PubMed]
- Del Buono, A.; Denaro, V.; Maffulli, N. Genetic susceptibility to aseptic loosening following total hip arthroplasty: A systematic review. Br. Med. Bull. 2012, 101, 39–55. [Google Scholar] [CrossRef]
- Electricwala, A.J.; Narkbunnam, R.; Huddleston, J.I., 3rd; Maloney, W.J.; Goodman, S.B.; Amanatullah, D.F. Obesity is Associated With Early Total Hip Revision for Aseptic Loosening. J. Arthroplast. 2016, 31 (Suppl. S9), 217–220. [Google Scholar] [CrossRef]
- Goodnough, L.H.; Finlay, A.K.; Huddleston, J.I., 3rd; Goodman, S.B.; Maloney, W.J.; Amanatullah, D.F. Obesity Is Independently Associated With Early Aseptic Loosening in Primary Total Hip Arthroplasty. J. Arthroplast. 2018, 33, 882–886. [Google Scholar] [CrossRef]
- Haverkamp, D.; Klinkenbijl, M.N.; Somford, M.P.; Albers, G.H.; van der Vis, H.M. Obesity in total hip arthroplasty--does it really matter? A meta-analysis. Acta Orthop. 2011, 82, 417–422. [Google Scholar] [CrossRef]
- Maradit Kremers, H.; Schleck, C.D.; Lewallen, E.A.; Larson, D.R.; Van Wijnen, A.J.; Lewallen, D.G. Diabetes Mellitus and Hyperglycemia and the Risk of Aseptic Loosening in Total Joint Arthroplasty. J. Arthroplast. 2017, 32, S251–S253. [Google Scholar] [CrossRef] [PubMed]
- Moon, J.K.; Jung, J.W.; Kim, Y.; Yang, J.H.; Park, Y.S.; Kim, Y.H. Acetabular cup migration after primary cementless total hip arthroplasty in rheumatoid arthritis and its influencing factors: A comparative study with osteoarthritic hip. Int. Orthop. 2020, 44, 1047–1053. [Google Scholar] [CrossRef] [PubMed]
- Böhler, C.; Weimann, P.; Alasti, F.; Smolen, J.S.; Windhager, R.; Aletaha, D. Rheumatoid arthritis disease activity and the risk of aseptic arthroplasty loosening. Semin. Arthritis Rheum. 2020, 50, 245–251. [Google Scholar] [CrossRef] [PubMed]
- Craiovan, B.; Woerner, M.; Winkler, S.; Springorum, H.R.; Grifka, J.; Renkawitz, T.; Keshmiri, A. Decreased femoral periprosthetic bone mineral density: A comparative study using DXA in patients after cementless total hip arthroplasty with osteonecrosis of the femoral head versus primary osteoarthritis. Arch. Orthop. Trauma Surg. 2016, 136, 709–713. [Google Scholar] [CrossRef] [PubMed]
- Di Martino, A.; Castagnini, F.; Stefanini, N.; Bordini, B.; Geraci, G.; Pilla, F.; Traina, F.; Faldini, C. Survival rates and reasons for revision of different stem designs in total hip arthroplasty for developmental dysplasia: A regional registry study. J. Orthop. Traumatol. 2021, 22, 29. [Google Scholar] [CrossRef]
- Gu, A.; Agarwal, A.R.; Fassihi, S.C.; Pollard, T.G.; Stoll, W.T.; Campbell, J.C.; Golladay, G.J.; Thakkar, S.C. Impact of sickle cell disease on postoperative outcomes following total hip arthroplasty. Hip Int. 2021, 11207000211052224. [Google Scholar] [CrossRef]
- Strauss, A.C.; Rommelspacher, Y.; Nouri, B.; Bornemann, R.; Wimmer, M.D.; Oldenburg, J.; Pennekamp, P.H.; Schmolders, J. Long-term outcome of total hip arthroplasty in patients with haemophilia. Haemophilia 2017, 23, 129–134. [Google Scholar] [CrossRef]
- Fontalis, A.; Kenanidis, E.; Bennett-Brown, K.; Tsiridis, E. Clinical outcomes in elective total hip arthroplasty in Parkinson’s disease: A systematic review of the literature. EFORT Open Rev. 2020, 5, 856–865. [Google Scholar] [CrossRef]
- Onochie, E.; Kayani, B.; Dawson-Bowling, S.; Millington, S.; Achan, P.; Hanna, S. Total hip arthroplasty in patients with chronic liver disease: A systematic review. SICOT J. 2019, 5, 40. [Google Scholar] [CrossRef]
- Lieu, D.; Harris, I.A.; Naylor, J.M.; Mittal, R. Review article: Total hip replacement in haemodialysis or renal transplant patients. J. Orthop. Surg. 2014, 22, 393–398. [Google Scholar] [CrossRef]
- Ofa, S.A.; Lupica, G.M.; Lee, O.C.; Sherman, W.F. Complications following total hip arthroplasty and hemiarthroplasty for femoral neck fractures in patients with a history of lumbar spinal fusion. Arch. Orthop. Trauma Surg. 2021, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Lemme, N.J.; Veeramani, A.; Yang, D.S.; Tabaddor, R.R.; Daniels, A.H.; Cohen, E.M. Total Hip Arthroplasty After Hip Arthroscopy Has Increased Complications and Revision Risk. J. Arthroplast. 2021, 36, 3922–3927.e2. [Google Scholar] [CrossRef] [PubMed]
- Kapadia, B.H.; Issa, K.; Pivec, R.; Bonutti, P.M.; Mont, M.A. Tobacco use may be associated with increased revision and complication rates following total hip arthroplasty. J. Arthroplast. 2014, 29, 777–780. [Google Scholar] [CrossRef] [PubMed]
- Myers, K.; Hajek, P.; Hinds, C.; McRobbie, H. Stopping Smoking Shortly Before Surgery and Postoperative Complications: A Systematic Review and Meta-analysis. Arch. Intern. Med. 2011, 171, 983–989. [Google Scholar] [CrossRef] [PubMed]
- Cherian, J.J.; Jauregui, J.J.; Banerjee, S.; Pierce, T.; Mont, M.A. What Host Factors Affect Aseptic Loosening After THA and TKA? Clin. Orthop. Rel. Res. 2015, 473, 2700–2709. [Google Scholar] [CrossRef]
- Nyström, A.; Kiritopoulos, D.; Ullmark, G.; Sörensen, J.; Petrén-Mallmin, M.; Milbrink, J.; Hailer, N.P.; Mallmin, H. Denosumab Prevents Early Periprosthetic Bone Loss After Uncemented Total Hip Arthroplasty: Results from a Randomized Placebo-Controlled Clinical Trial. J. Bone Min. Res. 2020, 35, 239–247. [Google Scholar] [CrossRef]
- Ro, D.H.; Jin, H.; Park, J.Y.; Lee, M.C.; Won, S.; Han, H.S. The use of bisphosphonates after joint arthroplasty is associated with lower implant revision rate. Knee Surg. Sports Traumatol. Arthrosc. 2019, 27, 2082–2089. [Google Scholar] [CrossRef]
- Prieto-Alhambra, D.; Lalmohamed, A.; Abrahamsen, B.; Arden, N.K.; De Boer, A.; Vestergaard, P.; De Vries, F. Oral bisphosphonate use and total knee/hip implant survival: Validation of results in an external population-based cohort. Arthritis Rheumatol. 2014, 66, 3233–3240. [Google Scholar] [CrossRef]
- Muratore, M.; Quarta, E.; Quarta, L.; Calcagnile, F.; Grimaldi, A.; Orgiani, M.A.; Marsilio, A.; Rollo, G. Ibandronate and cementless total hip arthroplasty: Densitometric measurement of periprosthetic bone mass and new therapeutic approach to the prevention of aseptic loosening. Clin. Cases Min. Bone Metab. 2012, 9, 50–55. [Google Scholar]
- Zhao, X.; Hu, D.; Qin, J.; Mohanan, R.; Chen, L. Effect of bisphosphonates in preventing femoral periprosthetic bone resorption after primary cementless total hip arthroplasty: A meta-analysis. J. Orthop. Surg. Res. 2015, 10, 65. [Google Scholar] [CrossRef]
- Malahias, M.A.; Loucas, R.; Loucas, M.; Denti, M.; Sculco, P.K.; Greenberg, A. Preoperative Opioid Use Is Associated With Higher Revision Rates in Total Joint Arthroplasty: A Systematic Review. J. Arthroplast. 2021, 36, 3814–3821. [Google Scholar] [CrossRef] [PubMed]
- Sorial, A.K.; Anjum, S.A.; Cook, M.J.; Board, T.N.; O’Neill, T.W. Statins, bone biology and revision arthroplasty: Review of clinical and experimental evidence. Adv. Musculoskelet. Dis. 2020, 12, 1759720X20966229. [Google Scholar] [CrossRef] [PubMed]
- Vallés, G.; Pérez, C.; Boré, A.; Martín-Saavedra, F.; Saldaña, L.; Vilaboa, N. Simvastatin prevents the induction of interleukin-6 gene expression by titanium particles in human osteoblastic cells. Acta Biomater. 2014, 9, 4916–4925. [Google Scholar] [CrossRef] [PubMed]
- Lübbeke, A.; Garavaglia, G.; Rothman, K.J.; Bonvin, A.; Roussos, C.; Miozzari, H.; Hoffmeyer, P. Statins may reduce femoral osteolysis in patients with total Hip arthroplasty. J. Orthop. Res. 2013, 31, 814–820. [Google Scholar] [CrossRef] [PubMed]
- De Soto, P.C.-M.; Tamimi-Mariño, I.; Bautista-Enrique, D.; Bravo-Zurita, M.J.; Cáceres, A.G.; Tamimi, F.; Dawid-Milner, M.S. Use of beta-blockers and risk of aseptic loosening in total hip and knee arthroplasty: A nested case—Control study. J. Musculoskelet. Neuronal. Interact. 2019, 19, 104–111. [Google Scholar]
- Wang, Z.; Xue, K.; Bai, M.; Deng, Z.; Gan, J.; Zhou, G.; Qian, H.; Bao, N.; Zhao, J. Probiotics protect mice from CoCrMo particles-induced osteolysis. Int. J. Nanomed. 2017, 12, 5387–5397. [Google Scholar] [CrossRef]
- Qian, Y.; Zhang, X.-L.; Jiang, Y.; Zeng, B.-F.; Wang, Q.; Chen, Y.; Shen, H.; Wang, Q. Alendronate stimulates osteoprotegerin expression in fibroblasts from periprosthetic membrane. Hip Int. 2015, 25, 581–584. [Google Scholar] [CrossRef]
- Duan, J.; Hu, X.; Li, T.; Wu, G.; Dou, P.; Ouyang, Z. Cimifugin Suppresses NF-κB Signaling to Prevent Osteoclastogenesis and Periprosthetic Osteolysis. Front. Pharm. 2021, 12, 724256. [Google Scholar] [CrossRef]
- Yang, C.; Liu, W.; Zhang, X.; Zeng, B.; Qian, Y. Naringin increases osteoprotegerin expression in fibroblasts from periprosthetic membrane by the Wnt/β-catenin signaling pathway. J. Orthop. Surg. Res. 2020, 15, 600. [Google Scholar] [CrossRef]
- Tian, Y.; Terkawi, M.A.; Onodera, T.; Alhasan, H.; Matsumae, G.; Takahashi, D. Blockade of XCL1/Lymphotactin Ameliorates Severity of Periprosthetic Osteolysis Triggered by Polyethylene-Particles. Front. Immunol. 2020, 11, 1720. [Google Scholar] [CrossRef]
- Ma, H.; Zhang, Q.; Shi, J.; Gao, Y.; Sun, C.; Zhang, W. Enalapril inhibits inflammatory osteolysis induced by wear debris in a mouse model. J. Int. Med. Res. 2020, 48, 300060520931612. [Google Scholar] [CrossRef] [PubMed]
- An, S.; Han, F.; Hu, Y.; Liu, Y.; Li, J.; Wang, L. Curcumin Inhibits Polyethylene-Induced Osteolysis via Repressing NF-κB Signaling Pathway Activation. Cell Physiol. Biochem. 2018, 50, 1100–1112. [Google Scholar] [CrossRef]
- Qin, C.Q.; Huang, D.S.; Zhang, C.; Song, B.; Huang, J.B.; Ding, Y. Lentivirus-mediated short hairpin RNA interference targeting TNF-alpha in macrophages inhibits particle-induced inflammation and osteolysis in vitro and in vivo. BMC Musculoskelet. Disord. 2016, 17, 431. [Google Scholar] [CrossRef] [PubMed]
- Zhao, S.; Sun, Y.; Li, X.; Wang, J.; Yan, L.; Zhang, Z.; Wang, D.; Dai, J.; He, J.; Wang, S. Scutellarin inhibits RANKL-mediated osteoclastogenesis and titanium particle-induced osteolysis via suppression of NF-κB and MAPK signaling pathway. Int. Immunopharmacol. 2016, 40, 458–465. [Google Scholar] [CrossRef] [PubMed]
- Xu, Y.; Sang, W.; Zhong, Y.; Xue, S.; Yang, M.; Wang, C.; Lu, H.; Huan, R.; Mao, X.; Zhu, L.; et al. CoCrMo-Nanoparticles induced peri-implant osteolysis by promoting osteoblast ferroptosis via regulating Nrf2-ARE signalling pathway. Cell Prolif. 2021, 54, e13142. [Google Scholar] [CrossRef]
- Zhang, Y.C.; Xiao, J.H.; Deng, S.J.; Yi, G.L. IRAK-4 in macrophages contributes to inflammatory osteolysis of wear particles around loosened hip implants. Innate Immun. 2021, 27, 470–482. [Google Scholar] [CrossRef] [PubMed]
- Vasconcellos, L.M.; Leite, D.O.; Oliveira, F.N.; Carvalho, Y.R.; Cairo, C.A. Evaluation of bone ingrowth into porous titanium implant: Histomorphometric analysis in rabbits. Braz Oral. Res. 2010, 24, 399–405. [Google Scholar] [CrossRef]
- Fender, D.; van der Meulen, H.P.; Gregg, P.J. Relationship between outcome and annual surgical experience for the Charnley total hip replacement. J. Bone Jt. Surg. 2003, 85, 187–190. [Google Scholar] [CrossRef]
- Vermesan, D.; Prejbeanu, R.; Haragus, H.; Ahmadi, M.; Damian, G. Metallosis during partial component hip revision arthroplasty. Rev. Chim. 2021, 63, 953. [Google Scholar]
| Stage | Category | Recommendations | Type of Recommednation |
|---|---|---|---|
| Preoperative | Acetabular cup | Acetabular cups without screw holes | Controversial |
| Trabecular metal acetabular cups | Generally accepted | ||
| Highly porous acetabular components | Controversial | ||
| Porous implant or hydroxyapatite coated | Controversial | ||
| Femoral stem | Titanium alloy femoral stems | Generally accepted | |
| Type 1, 2, 4 and 7 femoral stem designs | Generally accepted | ||
| Bearing surfaces | Ceramic-on-polyethylene | Generally accepted | |
| Dual mobility cup | Controversial | ||
| Patient-related factors | Body mass index < 35 | Generally accepted | |
| Patients with the following are higher risk: - age < 70 years; - genetic variations (ex. IFIT2/IFIT3, CERK, PAPPA, etc.); - Hyperglycemia; - Rheumatoid arthritis; - Femoral head AVN; - Hip dysplasia; - Sickle cell disease; - Parkinson disease; - Chronic liver disease; - Lumbar spinal fusion; - History of hip arthroscopy. | Generally accepted | ||
| Surgical team | More than 100 total hip replacements per year performed by the surgeon | Generally accepted | |
| Use of fewer types of implant by the same surgeon | Generally accepted | ||
| Intraoperative | Surgical factors | Lateral or posterior approach | Generally accepted |
| Avoid excessive drilling and rasping | Generally accepted | ||
| Obtain good stability of implant | Generally accepted | ||
| Obtain acetabular bone coverage of more than 60% | Generally accepted | ||
| Acetabular cup horizontal inclination of around 45 degrees | Generally accepted | ||
| Postoperative | Postoperative protocol | Immediate full weight bearing is accepted | Generally accepted |
| Avoid high impact activities | Controversial | ||
| Postoperative drugs | Use of bisphosphonates | Controversial | |
| Use of statins | Controversial | ||
| Use of beta-blockers | Controversial | ||
| Avoid opioids | Controversial | ||
| Avoid nonsteroidal anti-inflammatory drugs NSAIDs | Controversial | ||
| Replace selective serotonin reuptake inhibitors (SSRIs) | Controversial | ||
| Replace loop diuretics with thiazides. | Controversial |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Apostu, D.; Piciu, D.; Oltean-Dan, D.; Cosma, D.; Lucaciu, O.; Popa, C.; Mester, A.; Benea, H. How to Prevent Aseptic Loosening in Cementless Arthroplasty: A Review. Appl. Sci. 2022, 12, 1571. https://doi.org/10.3390/app12031571
Apostu D, Piciu D, Oltean-Dan D, Cosma D, Lucaciu O, Popa C, Mester A, Benea H. How to Prevent Aseptic Loosening in Cementless Arthroplasty: A Review. Applied Sciences. 2022; 12(3):1571. https://doi.org/10.3390/app12031571
Chicago/Turabian StyleApostu, Dragos, Doina Piciu, Daniel Oltean-Dan, Dan Cosma, Ondine Lucaciu, Catalin Popa, Alexandru Mester, and Horea Benea. 2022. "How to Prevent Aseptic Loosening in Cementless Arthroplasty: A Review" Applied Sciences 12, no. 3: 1571. https://doi.org/10.3390/app12031571
APA StyleApostu, D., Piciu, D., Oltean-Dan, D., Cosma, D., Lucaciu, O., Popa, C., Mester, A., & Benea, H. (2022). How to Prevent Aseptic Loosening in Cementless Arthroplasty: A Review. Applied Sciences, 12(3), 1571. https://doi.org/10.3390/app12031571








