Abstract
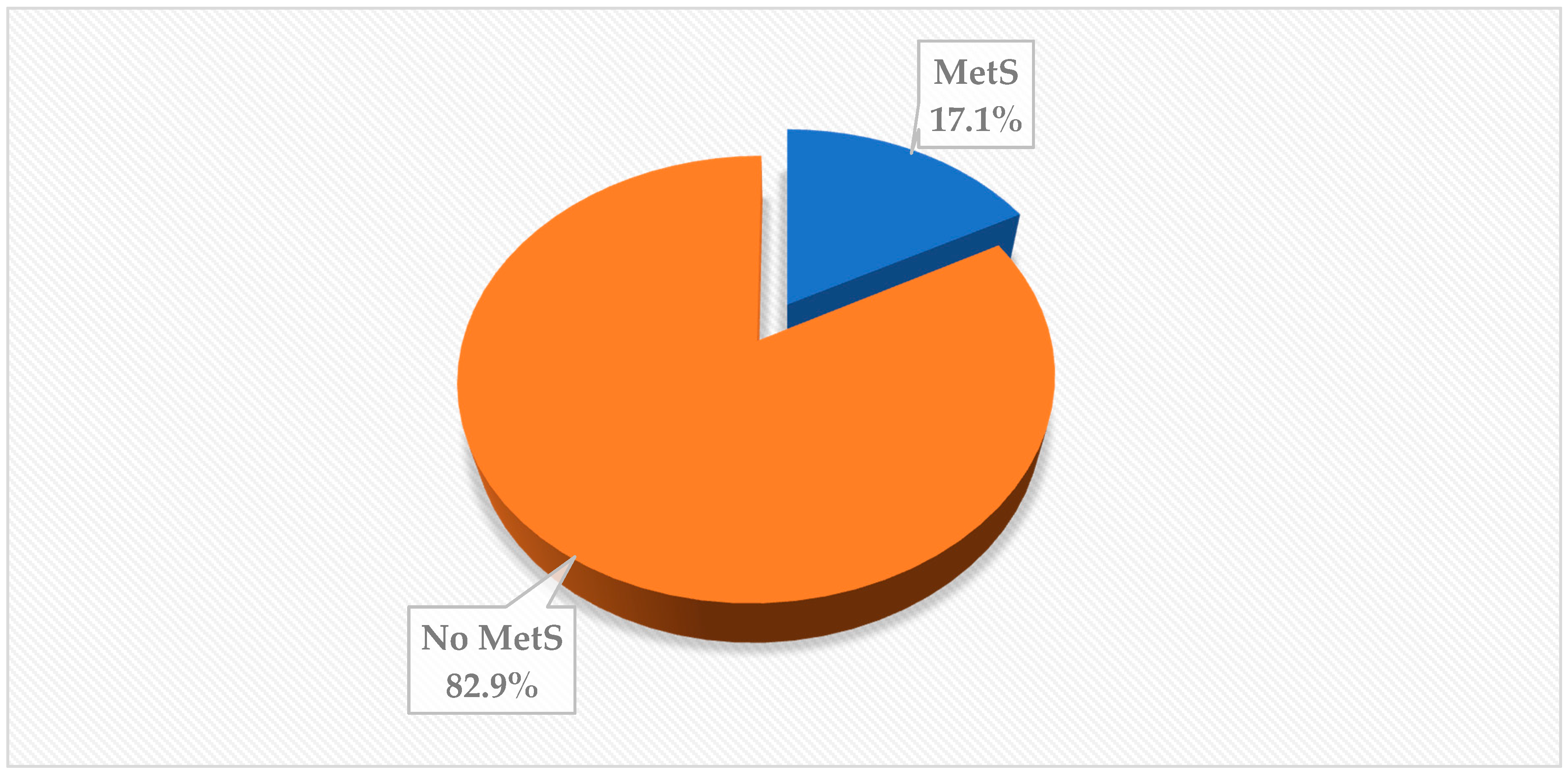
The occupation of taxi driving predisposes drivers to health risks, including obesity, cardiovascular and metabolic disorders. Although individual components of metabolic syndrome (MetS) are documented, data is scarce on concurrent metabolic disturbances among commercial drivers. The prevalence of MetS and its components were determined in a cross-sectional study among taxi drivers (n = 362) in the City of Tshwane, South Africa. Sociodemographic, occupational, and lifestyle factors were assessed using a structured questionnaire. Anthropometry, blood pressure, and glucose were measured. MetS was defined based on BMI strata, hypertension, and glucose levels. Data was analyzed using SPSS. The mean age of taxi drivers was 42 ± 10.9 years. Overall prevalence of MetS was 17.1%, with higher prevalence observed among older taxi drivers (24.2%) and those with longer experience in the industry (22.9%). Individual components of MetS were obesity (36%), hypertension (36%) and diabetes (46%), while smoking (30%), alcohol use (59%), and physical inactivity (71%) were observed. MetS was associated with duration in the taxi industry, and family history of diabetes among taxi drivers. The presence of MetS and its components among taxi drivers calls for early identification of cardiometabolic risks in the taxi industry and efforts towards achieving a healthier workforce.
1. Introduction
Taxis are a common means of transport in South Africa, especially in the urban area [1]. The country draws part of its economy from the taxi industry, which serves the majority of South Africans who are poor, and therefore dependent on public transport [1]. The South African taxi industry has approximately 200,000–300,000 drivers and its turnover is estimated at more than R16, 5 billion (USD ≈1 billion) [1,2]. However, this industry predisposes taxi drivers to occupation-based health risks in their line of work, which is life-threatening [3,4,5,6,7]. The nature of their occupation exposes them to long hours of work, which deprives them of enough sleep required for optimum health [8,9], and these working conditions promote exhaustion, which is associated to sedentary lifestyle and unhealthy eating [9]. The stressfulness of the occupation of commercial drivers, in addition to other factors, such as limited time to access health services during the day, put their health at risk of developing cardiovascular diseases and metabolic syndrome (MetS) [6,10,11,12,13,14]. MetS is on the rise in developing countries, affecting African countries as well, and, in particular, South Africa [15,16,17]. While data on MetS is limited among taxi drivers [11], the prevalence of MetS in the general South African population varies from 5% to 62% [18,19,20,21,22,23,24], which is determined by the group being studied.
Concurrent presence of metabolic disturbances in the general population is more harmful than each single isolated problem, but data is limited among taxi drivers in South Africa [6,12,13]. MetS is characterized by the presence of three or more components such as abdominal obesity, high blood pressure, increased levels of fasting blood glucose and serum triglycerides, and low levels of high-density cholesterol [25,26]. Patients with the components of MetS are at increased risk of cardiovascular diseases and type 2 diabetes mellitus, while obesity, especially abdominal obesity, contributes to the occurrence of MetS and later predisposes to morbidity and mortality [27,28]. South Africa has recorded alarming rates of undiagnosed hypertension (13.5–75.5%) [29,30], diabetes (69%) [31], overweight/obesity (56–68%) [32], abdominal obesity (56.4–65.2%) [17,18], and dyslipidemia (14–69%) [33,34] among adults. Furthermore, previous studies have reported high prevalence of diabetes (16%), hypertension (57.0%), obesity (24.5–75.5%), and abdominal obesity (29–71%) among taxi drivers in South Africa [6,12,13]. These cardiometabolic abnormalities impair the quality of life, while the health care system continues to be burdened [26,27].
In addition to occupational stresses, the prevalence of MetS has been attributed to socioeconomic, lifestyle, genetic, metabolic, and environmental factors including improper dietary intake, obesity, and physical inactivity [35,36,37,38]. All of these factors contribute to cardiovascular health, particularly MetS, in various population groups such as taxi drivers [6,11,12,13,39]. Several studies have reported discrepancies on the link between different jobs and risk of MetS in developing countries [28,40,41]. While some studies showed that the rates of hypertension, blood glucose, and high triglyceride levels were significantly higher among commercial drivers compared to professional workers [40,41], no significant differences of these factors were reported between commercial drivers and non-drivers [28]. In other occupations in South Africa, Kruger and Nell showed variations in obesity indices and blood pressure correlated with MetS and its risk factors influenced by gender among farm workers [18].
Research in South Africa usually focuses on one aspect of the problem among commercial drivers, either obesity or hypertension, or diabetes, and is not mutually referential. The 2030 Agenda for Sustainable Development adopted by the United Nations in 2015 recognizes non communicable diseases (NCDs) as a major public health challenge. Sustainable Development Goal (SDG) 3 includes target 3.4 to reduce premature NCDs mortality by one-third by 2030 [42]. Therefore, the current study determined the prevalence of MetS and its components among taxi drives in the City of Tshwane, South Africa. This study further advocates for health screening and awareness, in risky populations such as taxi drivers, to minimize the burden of MetS in South Africa. MetS deserves attention and screening should be up scaled for all age groups to save the future generations [43].
2. Materials and Methods
2.1. Study Design and Setting
A cross-sectional study using a quantitative approach was conducted among taxi drivers in selected taxi ranks of the City of Tshwane (i.e., Pretoria), Gauteng Province, between September and October 2019. Tshwane is among the largest metropolitan municipalities in South Africa, and has approximately 2,921,488 residents, many of whom rely on minibus taxis. There are approximately 10 taxi ranks in the city, of which three, namely Bloed, Marabastad, and Bosman, are the major ones also serving long distance travelers to different destinations beyond the province borders. Hence, these major taxi ranks were selected purposively because they have a larger population of taxi drivers.
2.2. Study Population, Sampling, and Sample Size
The study consisted of male taxi drivers from taxi ranks in the City of Tshwane, Gauteng Province, aged 18 years and above. A population size of 3500 taxi drivers was estimated for the three taxi ranks (Bloed, Marabastad, and Bosman) and was used to calculate a representative sample of 347 using the Raosoft sample calculator (Raosoft, 2004), taking into consideration 5% margin of error, 95% confidence level, and response distribution of 50%. The sample size was further buffered with 10% to cater for non-response and a final sample size of 390 was obtained. In total, 28 questionnaires had missing data of more than 10%, and were thus excluded from the final analysis. The final response rate was thus 93%.
Convenience sampling method was used to selected taxi driver taxis recruited with the help of research assistants and queue marshals. During recruitment, the researcher informed the taxi drivers about the aims and objectives of the study through information leaflets. Taxi drivers who were awaiting their turn to load commuters to their destinations were asked to participate. Those who agreed to participate in the study were invited to come to the gazebo pitched at the periphery of the taxi rank for data collection. The study included all taxi drivers who were 18 years and older, operating in the selected taxi ranks, gave consent for the study at the time of data collection, and were available for data collection. All taxi drivers who were aged less than 18 years, on medication to control for hypertension and diabetes, and not willing to participate in the study were excluded.
2.3. Data Collection and Tools
Taxi drivers were recruited from the selected taxi ranks, which are Bloed, Marabastad, and Bosman. The researcher was accompanied by a South African National Taxi Council (SANTACO) representative from the selected taxi ranks for formal introduction to the taxi line marshals in the morning. The marshals were asked for permission to conduct the study and to recruit the drivers. They were also asked for permission to distribute posters and to help to gather the participants to be included in the study. The recruitment was undertaken with the assistance of researcher assistants.
A self-administered questionnaire was used to collect data under the supervision of the main researcher (E.M.M) and research assistants. Demographic factors, occupational information (experience and sleeping hours), and anthropometric data, including height and weight, lifestyle (smoking, alcohol use, and physical activity), and MetS components (obesity, hypertension, and diabetes) were recorded using a validated structured questionnaire (see Supplementary Material) informed by several studies [19,40,41]. Validity and reliability were ensured through content and face validity, backward and forward translation using a translator conversant with local language and English, a pilot study, and training of research assistants.
Weight and height were measured twice for each participant and a third measurement was taken if the difference between two measurements was larger than 1 cm for height or 1 kg for weight. The average of two close measurements in height and weight was used in our study. Blood pressure was measured on the left upper arm, using an Elite 1219 Blood Pressure Monitor (Shanghai International Holding Corp. GmbH (Hamburg, Germany), following a five-minute resting period in a sitting position, on the right hand repeated two times with at least a five-minute interval. Capillary blood was taken using disposable lancets to determine glucose with an Accutrend® GCT (Roche Diagnostics, Basel, Switzerland). Participants were requested to fast overnight prior to data collection the following day in the morning. Two consecutive measurements were taken, and the mean value was used for the study. All the instruments were constantly calibrated during data collection for accuracy and consistency. In the present study, we used a modified version of the National Cholesterol Education Program definition of the MetS [44]. Because waist circumference measurements were missing for almost half of the participants, the National Cholesterol Education Program definition was modified by use of a BMI cut point instead of the National Cholesterol Education Program waist circumference criterion (>102 cm), similar to the approach of other researchers [45]. Therefore, MetS was defined by the participant having any three conditions, high BMI (≥25 kg/m2), hypertension >135/85 mmHg, and Fasting Plasma Glucose (FPG) of >6.1 mmol/L (for 10–12 h).
2.4. Data Analysis
Raw data were captured into Microsoft Excel, edited, coded, verified, and imported to SPSS version 24 for data analysis. Descriptive statistics in the form of frequencies and percentages were used to describe the sample, and to determine the prevalence of MetS and its component. Chi-square was used to test for differences in proportions by age and duration in taxi industry categories. Hierarchical logistic regression analysis was used to assess the associations of MetS with demographic and lifestyle factors, and family health history. Results are presented as adjusted odds ratio (95%confidence interval); (AOR (95%CI)) age was controlled for as a confounding factor. Probability was set at p < 0.05.
2.5. Ethical Considerations
Sefako Makgatho Health Sciences University Research and Ethics Committee, South Africa (SMUREC/H/18/2018: PG) approved the study in accordance with Helsinki II Declaration [46] and consent to conduct the study was granted by SANTACO in written form to access the taxi ranks in City of Tshwane, South Africa. Taxi drivers who participated in the study gave a written informed consent.
3. Results
3.1. The Prevalence of MetS among Taxi Drivers
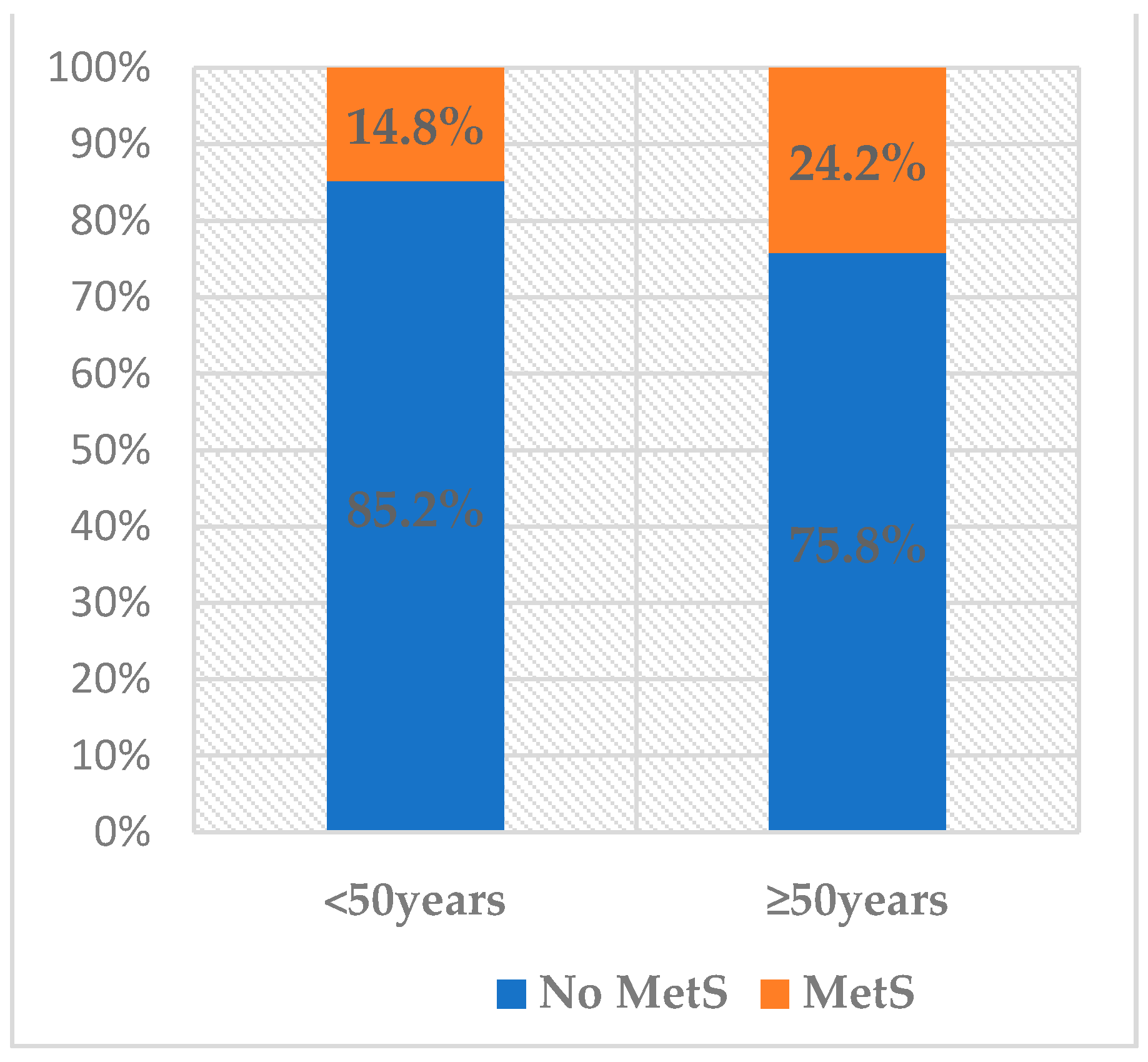
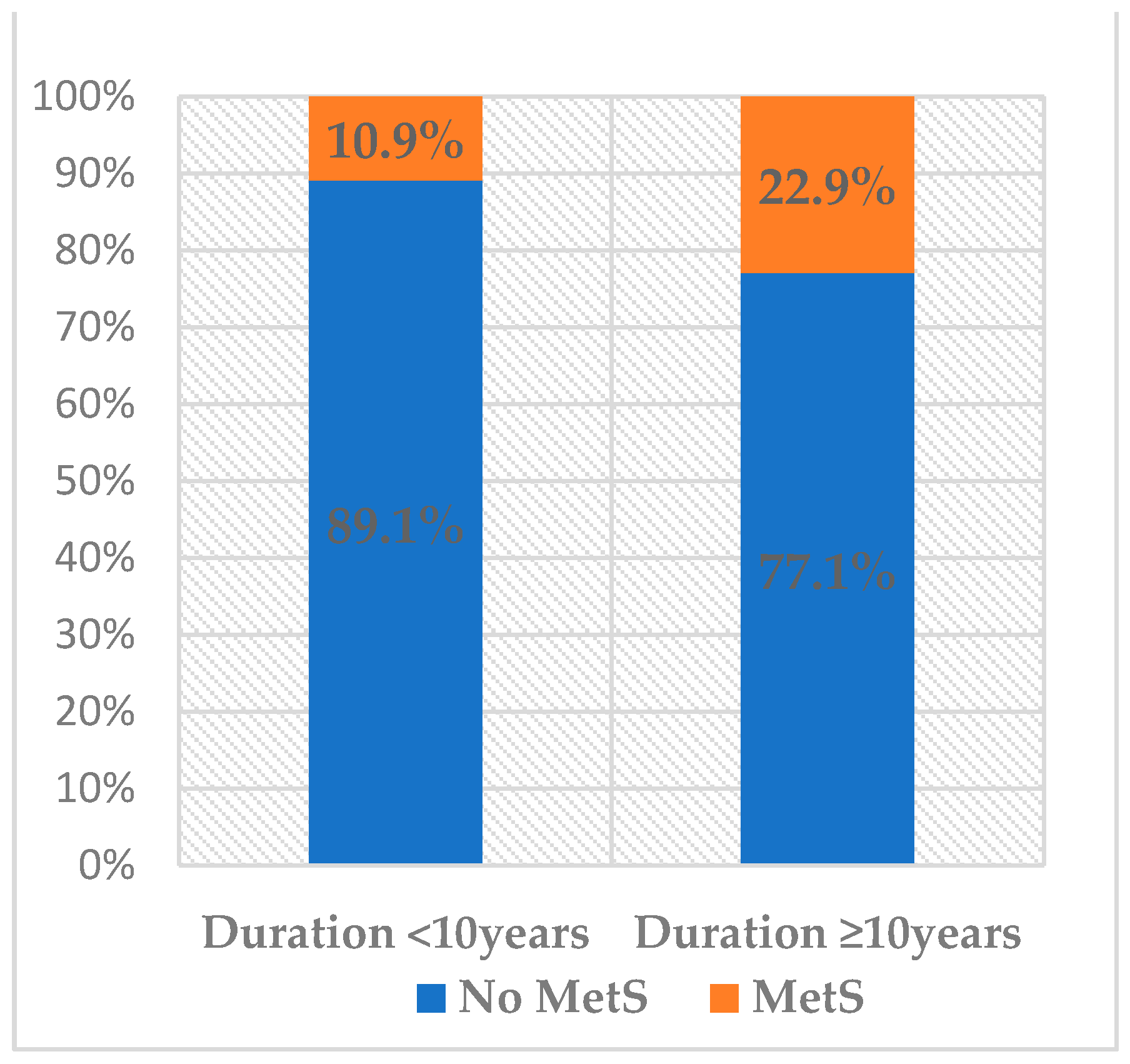
A sample of 362 taxi drivers was obtained in the three taxi ranks of the city of Tshwane in Gauteng Province, South Africa. The mean age of taxi drivers was 42 ± 11 years. From the literature, we identified age (divided into <50 and ≥50 years) [47] and duration of service in the taxi industry (divided into <10 and ≥10 years) [48] as factors for analysis of the prevalence of MetS among taxi drivers. The prevalence of MetS among taxi drivers was 17.1%, shown in Figure 1. The prevalence of MetS among taxi drivers aged less than 50 years was 14.8%, while 24.2% was observed among those aged above 50 years (Figure 2). Taxi drivers who had the highest period of service (≥10 years) recorded the highest prevalence of MetS (22.9%) versus 10.9% among those with a duration less than 10 years, p = 0.003 (Figure 3).
Figure 1.
Prevalence of metabolic syndrome among taxi drivers in Gauteng, South Africa.
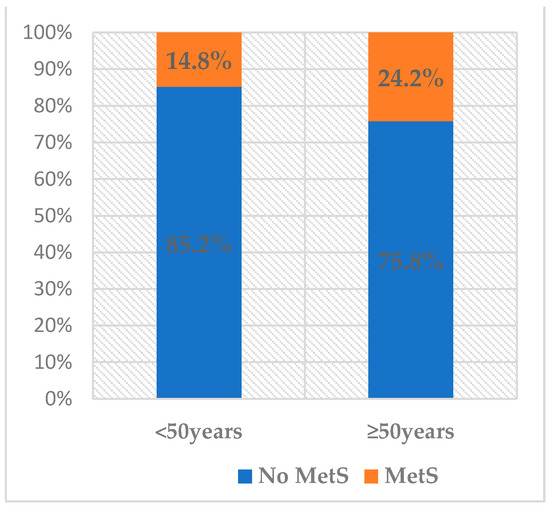
Figure 2.
Prevalence of MetS according to age groups (p = 0.039).
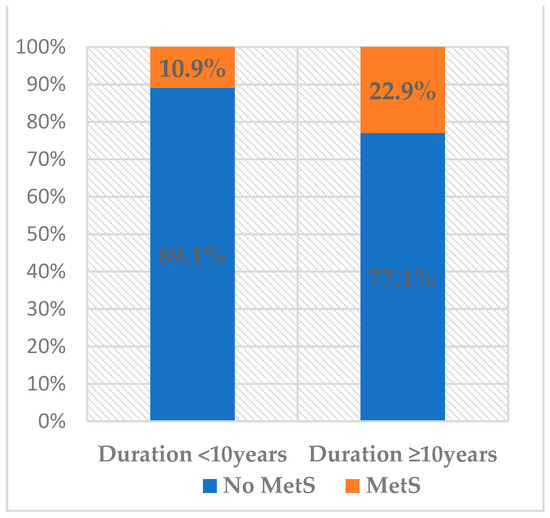
Figure 3.
Prevalence of MetS according to duration in the taxi industry (p = 0.003).
3.2. Characteristics of Taxi Drivers
The selected sociodemographic, occupational information, lifestyle factors, and components of MetS of taxi drivers are presented in Table 1. Seventy-five percent of taxi drivers in this study were aged less than 50 years and 25% were 50 years and above. Fifty-two percent had been in the taxi industry for 10 years and above while 48% for less than 10 years. Few taxi drivers (n = 45, (12%)) reported to sleep less than 5 h/day on most days. Almost all of the taxi drivers were family providers (83%) in their families and 79% had obtained high school education (79%). Over half of the taxi drivers had been married (52%) and 40% were single. Lifestyle factors observed in the study were alcohol users (59%), smoking (30%), physical inactivity (71%), as well as the tendency of eating pap (i.e., a maize staple food) mostly during lunch (84%), not eating at least one piece of fruit per day (29%), and not eating at least one vegetable per day (29%). One third of taxi drivers (32%) have never been screened for hypertension, and over half of them (57%) have never been screened for diabetes. Individual metabolic components in this study were obesity, hypertension, and diabetes. The study showed that 70% of taxi drivers were overweight/obese, 36% had hypertension, and 46% had diabetes. Some taxi drivers reported to have a family history of hypertension (30%) and diabetes (24%) (Table 1).

Table 1.
Characteristics of taxi drivers.
3.3. Association of MetS Components and Selected Variables by Age
Taxi drivers were divided into two age groups; <50 years (young drivers, n = 271) and ≥50 years (older drivers; n = 91). Using a Chi-square test, age was associated with hypertension (p = 0.002), diabetes (p = 0.020), marital status (p = 0.001), education (p = 0.001), duration in the taxi industry and was high among older taxi drivers (44%; p = 0.005), and alcohol use (p = 0.001) (Table 2).

Table 2.
Comparison of age and selected variables among taxi drivers.
Taxi drivers were divided into two groups based on the duration of service in the taxi industry: <10 years (n = 174) and ≥10 years (n = 188). Using a Chi-square test, duration in the taxi industry was associated with age (p = 0.001), hypertension (p = 0.001), marital status (p = 0.001), and education (p = 0.001) (Table 3). Further analysis (result not shown in tables), marital status was significantly associated with diabetes (p = 0.002) and hypertension (p = 0.025). Additionally, marital status was associated with age (p = 0.001), being a family provider (p = 0.001), and alcohol use (p = 0.002).

Table 3.
Comparison of duration in the taxi industry and selected variables among taxi drivers.
3.4. Factors Associated with MetS
Table 4 shows the hierarchical model results for taxi drivers. In Model 1, it was observed that there was no significant association between lifestyle factors and MetS besides for the duration in the driving industry and MetS. In model 2, family health history was added to Model 1. Family health history having diabetes and the duration in the driving industry were significantly associated with MetS (AOR = 2.075 (1.035; 4.160); p = 0.040 and AOR = 2.305 (0.261; 1.161); p = 0.010) shown in Table 4.

Table 4.
Hierarchical logistic regression models for lifestyle and family health history factors associated with MetS among taxi drivers.
4. Discussion
This paper reports on the prevalence of MetS and its components among taxi drives in the City of Tshwane, South Africa, and further shows the associations of MetS with selected variables.
With an average age of 42 years old, over half of the taxi drivers in this study had more than 10 years of experience working in the taxi industry. Older drivers and long working experience are common in the taxi industry [12,48] and this could be because taxi driving is an organized industry where drivers work as employees in South Africa. However, few taxi drivers reported inadequate sleep of less than four hours at most per day. Literature documents that sleeping hours are related to exhaustion among taxi drivers [49], and that the limit of tolerance for exhaustion is about four to five hours of sleep per day [50]. The age of 50 years is considered as approximately the time when illnesses associated with sleep quality and exhaustion are most prominent [47]. According to Lim and Chia [49], lower prevalence of exhausted driving may lead to lower risks of road traffic accidents, decreased economic loss, increased productivity, and safer roads for all. The current study further showed that poor socioeconomic status was characterized by very few taxi drivers having post high school education while many of them were family provider. In South Africa, poverty and unemployment are generally high, and to some extent illiteracy levels are significant among adults [2,51]. Therefore, the majority of the taxi drivers opt for this occupation because they do not have the qualification to secure jobs of their interest due to limited education and financial difficulty [39]. Additionally, almost all drivers in this study consumed pap during most of their lunch times, while, a third were smoking, half was using alcohol, and two thirds were physically inactive. The nature of taxing driving confines drivers to sitting for long periods, making them have irregular dietary patterns and habits [38], which contribute to the development of cardiometabolic risks for MetS [52].
The current study estimated the prevalence of MetS among taxi drivers at 17.1%, with high prevalence observed among older taxi drivers and those who had a longer term in the industry. There is no sufficient data to make a comparison of metabolic syndrome among taxi drivers in South Africa [11]. A 17.3% prevalence of MetS has been reported among men [53] and low prevalence (15.46%) among women [54] in South Africa. High prevalence of MetS among the general population has been reported among people aged 50 years or older, consistent with the prevalence of MetS reported among older commercial drivers in the current study, and in other countries [55,56]. In the present study, the prevalence of MetS among taxi drivers was significantly high among those who had ≥10 years driving experience. The driving duration has been reported as one of the risk factors that relates to MetS [38]. Furthermore, the prevalence of MetS varies by age, settings, and race, and South Africa has recorded a range of 5–62% [18,19,20,21,22,23,24]. Consistent with studies in other developing countries, Africa and SSA, unequal variation in MetS rates (4–63.7%) has been observed [39,57,58,59,60]. Challenges concerning the comparison of the presence of MetS across studies exist due to the various definitions of MetS [61]. The literature further documents the influence of culture differences, occupation, and lifestyle factors [28,37,62,63]. A combination of these factors may explain the similarities or differences in the prevalence of MetS reported in this study in comparison to other studies. To complicate the matter further, diagnosis of MetS based only on the presence of three out of the five risk factors differs by definition [18]. According to Kengne et al. [62], the different criteria for MetS have not been adapted for either the South African or African populations.
The majority of the drivers in this study had individual components of the MetS, which are obesity (36%), hypertension (36%), and diabetes (46%). The coexistence of these components contribute to the prevalence of MetS [63]. Similar to previous studies [17,20,56], the prevalence of MetS in the current study may be driven by the presence of obesity, hypertension, and diabetes. The presence of MetS and its components are attributed to urbanization and epidemiological transition in South Africa [17]. Taxi drivers with MetS had a high prevalence of obesity in this study. Obesity is alarming in South Africa with variations in several factors such as age and gender [64,65,66]. A high prevalence of hypertension was significantly observed among older taxi drivers compared to younger drivers. Disparities in the presence of hypertension by gender, age, and setting in South Africa have been reported [67,68,69]. In addition, hypertension is ascribed to sedentary lifestyle, nutrition, and stress, which might be the case in the current study, in agreement with other researchers [56]. A high proportion of physical inactivity confirms sedentary lifestyle in the current study, which is common among commercial drivers [70].
On the other hand, this study reported higher glucose levels (46%) among taxi drivers than among different population groups (13.8–26.3%) [19,20]. Recent reports by the International Diabetes Federation has reported 1.8 million South Africans with diabetes, and further estimated an additional undiagnosed population of 69% [31]. Elevated glucose level in the current study could be related to a high prevalence of obesity, which is a risk factor for diabetes [27], as well as physical inactivity and excessive alcohol consumption, which has been previously reported [39,71]. Failure to control diabetes might lead to health complications, which include MetS [39]. According to the literature, the prevalence of diabetes is affected by factors such as age, dietary habits, gender, daily work hours, geographical location, obesity rates, economic transition, and the different criteria used for diagnosing diabetes [19,38]. In addition to physical inactivity reported in this study, smoking and alcohol use were high among taxi drivers. Smoking has been reported as one of the major lifestyle factors leading to cardiovascular diseases, subsequent to hypertension [72], and predisposes to several health issues such as MetS [73]. Furthermore, the literature documents that most drivers consume alcohol as a way of relaxation after a strenuous day as well as to boost appetite and as part of social events [74]. Excessive consumption of alcohol has been associated with hypertension and increases calorie intake [73].
The Chi-square test showed that age was associated with hypertension, diabetes, marital status, alcohol use, and duration in the taxi industry among taxi drivers. Furthermore, duration in the taxi industry was associated with hypertension, diabetes, marital status, and education status. As predicted, MetS was associated with its components; hypertension, diabetes, and BMI among drivers (results not shown). Multivariate logistic regression analysis showed that family health history of having diabetes and the duration in the driving industry were significantly associated with MetS. Family history of having diabetes was significantly associated with MetS in this study, consistent with other studies [75,76]. Family history is a common non-modifiable risk factor for most chronic NCDs because it is a collective reflection of the genetic susceptibility, shared environments, and behaviors [77]. Although, in our case, a family history of diabetes had an inverse relationship with MetS (AOR = 0.936, 95%CI: 0.182–0.862). Additionally, taxi drivers with more than 10 years of experience in the taxi industry were two times likely to have MetS (AOR =2.305 (0.261; 1.161)) than those with a driving duration below 10 years. The driving duration is also one of the risk factors that are associated with MetS, similar to other studies [38,56]. This suggests that a long duration of taxi driving occupation could contribute to the occurrence of MetS and mainly affect the increase of cardiovascular events in driver populations, as suggested by Mohebbi et al. [70].
5. Limitations
This study had several limitations. First, the use of the cross-sectional nature of the study is a major limitation because the design can only report on inference. Second, we did not assess dietary intake and practice, as well as the daily exercise and stress risk factors in drivers. Third, the study had recall bias and social desirability, which might condone under or over reporting, in addition to use of dichotomous questions. Fourth, we could not ascertain that the participants answered honestly in regard to fasting when we determined the level of glucose through capillary blood. Finally, we used BMI to define obesity as a component of MetS due to missing data on waist circumference in half of the population and we did not assess the daily exercise and stress risk factors in drivers. There are numerous reasons for risk of MetS in professional drivers, which need to be further studied. However, the study was able to estimate the prevalence of MetS and its components among taxi drivers, as well as interrelated factors. Future research should endeavor to study MetS in detail, and analyze biochemical variables for several components of MetS.
6. Conclusions
MetS is present in taxi drivers and might be driven by the presence of obesity, hypertension, and diabetes as MetS components. The fact that one third of taxi drivers have never screened for hypertension, and over half of them have never screened for diabetes, and were not aware of the possibility of elevated blood pressure and FPG, suggest that taxi drivers are too busy to access the primary healthcare system for medical check-ups. Taxi drivers with undiagnosed hypertension and diabetes/pre-diabetes are at a higher future risk of cardiovascular diseases. Duration in the taxi industry and family history of diabetes were risks for MetS among taxi drivers. High prevalence of smoking, alcohol use, physical inactivity, and poor diet reported in this study pose a threat for cardiovascular diseases if the lifestyles of taxi drivers continue without change. MetS prevalence and its components may be due to lack of awareness and unhealthy lifestyles, indicating the necessity of health education and more preventive measures to decrease cardiometabolic risk factors among taxi drivers. This study identified cases that required referral and further intended to add value to the minimal existing baseline information on MetS among commercial drivers in South Africa to inform intervention programs. The presence of MetS and its components among taxi drivers calls for early identification of cardiometabolic risks in the taxi industry and efforts towards achieving a healthier workforce.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/app12031767/s1, Questionnaire: Metabolic Syndrome and its Components among Taxi Drivers in the City of Tshwane, South Africa.
Author Contributions
Conceptualization, E.M.M. and K.E.M.; formal analysis, P.M. and P.M.M.; investigation, E.M.M.; methodology, E.M.M. and K.E.M.; resources, E.M.M. and K.E.M.; software, P.M. and P.M.M.; validation, P.M.; supervision, K.E.M.; writing—original draft, P.M. and P.M.M.; writing—review and editing, P.M., P.M.M. and K.E.M. All authors have read and agreed to the published version of the manuscript.
Funding
The study was self-funded.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Institutional Review Board (or Ethics Committee) of the Sefako Makgatho Health Sciences University, South Africa, (SMUREC/H/18/2018: PG, approved on 1 February 2018).
Informed Consent Statement
Participation was voluntary and the participants provided written informed consent.
Data Availability Statement
The dataset for participants generated and analyzed during the original study is available from the corresponding author upon reasonable request.
Acknowledgments
The author would like to thank SANTACO for granting us the permission to conduct the study. We also thank the taxi drivers for participating in the study despite the busyness in the taxi ranks. We also acknowledge Machaka Ravhengani and Thabang Serite for helping with data collection.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Arrive Alive: Minibus Taxi and Road Safety. 2021. Available online: https://www.arrivealive.mobi/minibus-taxis-and-road-safety (accessed on 4 November 2021).
- The ConversationInc: South Africa’s Minibus Taxi Industry Has Been Marginalised for Too Long. This Must Change. 2020. Available online: https://theconversation.com/south-africas-minibus-taxi-industry-has-been-marginalised-for-too-long-this-must-change-142060 (accessed on 4 November 2021).
- Burgel, B.J.; Gillen, M.; White, M.C. Health and Safety Strategies of Urban Taxi Drivers. J. Hered. 2012, 89, 717–722. [Google Scholar] [CrossRef] [PubMed]
- Izadi, N.; Malek, M.; Aminian, O.; Saraei, M. Medical risk factors of diabetes mellitus among professional drivers. J. Diabetes Metab. Disord. 2013, 12, 23. [Google Scholar] [CrossRef] [PubMed]
- Mirpuri, S.; Gill, P.; Ocampo, A.; Roberts, N.; Narang, B.; Hwang, S.W.; Gany, F. Discrimination and Health Among Taxi Drivers in New York and Toronto. J. Community Health 2018, 43, 667–672. [Google Scholar] [CrossRef] [PubMed]
- Ramukumba, T.S.; Mathikhi, M.S. Health assessment of taxi drivers in the city of Tshwane. Curationis 2016, 39, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Mathikhi, M.S.; Ramukumba, T.S. Taxi drivers’ perceptions of occupational health risks related to their work environment in the City of Tshwane, South Africa. Afr. J. Phys. Act. Health Sci. (AJPHES) 2020, 26, 393–409. [Google Scholar] [CrossRef]
- Apantaku-Onayemi, F.; Baldyga, W.; Amuwo, S.; Adefuye, A.; Mason, T.; Mitchell, R.; Blumenthal, D.S. Driving to better health: Cancer and cardiovascular risk assessment among taxi cab operators in Chicago. J. Health Care Poor Underserved 2012, 23, 768–780. [Google Scholar] [CrossRef]
- Poó, F.M.; Ledesma, R.D.; López, S.S. The taxi industry: Working conditions and health of drivers, a literature review. Transp. Rev. 2018, 38, 394–411. [Google Scholar] [CrossRef]
- Tobin, E.; Ofili, A.; Asogun, D.; Igbinosun, P.; Igba, K.; Idahosa, A. Prevalence of hypertension and associated factors among inter-city drivers in an urban city in south-south nigeria. Int. J. Res. Med. 2013, 2, 5–12. [Google Scholar]
- Sekgala, D. The Determinants of Metabolic Syndrome and Associated Risk Factors of CVDs Among Taxi Drivers Operating in Cape Town and Surrounding Areas: A focus on Street Food. 2020 (Paper Presented at a Midterm Meeting of Research Networks for Health Innovations in Sub-Saharan Africa, Accra, Ghana, 28–31 January). Available online: http://hdl.handle.net/20.500.11910/15373 (accessed on 22 June 2021).
- Adedokun, A.O.; Ter Goon, D.; Owolabi, E.O.; Adeniyi, O.V.; Ajayi, A.I. Prevalence, awareness, and determinants of type 2 diabetes mellitus among commercial taxi drivers in buffalo city metropolitan municipality South Africa: A cross-sectional survey. Medicine 2019, 98, e14652. [Google Scholar] [CrossRef]
- Adedokun, A.O.; Goon, D.T.; Owolabi, E.M.; Adeniyi, O.V.; Ajayi, A.I. Driving to Better Health: Screening for Hypertension and Associated Factors Among Commercial Taxi Drivers in Buffalo City Metropolitan Municipality, South Africa. TOPHJ 2017, 10, 303–312. [Google Scholar] [CrossRef]
- Lalla-Edward, S.; Ncube, S.; Matthew, P.; Hankins, C.; Venter, F.; Gomez, G. Uptake of health services among truck drivers in South Africa: Analysis of routine data from nine roadside wellness centres. BMC Health Serv. Res. 2017, 17, 649. [Google Scholar] [CrossRef]
- Misra, A.; Khurana, L. Obesity and the Metabolic Syndrome in Developing Countries. J. Clin. Endocrinol. Metab. 2008, 93, s9–s30. [Google Scholar] [CrossRef] [PubMed]
- Okafor, C. The metabolic syndrome in Africa: Current trends. Indian J. Endocrinol. Metab. 2012, 16, 56–66. [Google Scholar] [CrossRef] [PubMed]
- Owolabi, E.O.; Ter Goon, D.; Adeniyi, O.V.; Adedokun, A.O.; Seekoe, E. Prevalence and Correlates of Metabolic Syndrome Among Adults Attending Healthcare Facilities in Eastern Cape, South Africa. Open Public Heath. J. 2017, 10, 148–159. [Google Scholar] [CrossRef]
- Kruger, M.J.; Nell, T.A. The prevalence of the metabolic syndrome in a farm worker community in the Boland district, South Africa. BMC Public Health 2017, 17, 61. [Google Scholar] [CrossRef]
- Erasmus, R.T.; Soita, D.J.; Hassan, M.S.; Blanco-Blanco, E.; Vergotine, Z.; Kengne, A.P.; Matsha, T.E. High prevalence of diabetes mellitus and metabolic syndrome in a South African coloured population: Baseline data of a study in Bellville, Cape Town. South Afr. Med. J. 2012, 102, 841–844. [Google Scholar] [CrossRef]
- Motala, A.A.; Esterhuizen, T.; Pirie, F.J.; Omar, M.A.K. The Prevalence of Metabolic Syndrome and Determination of the Optimal Waist Circumference Cutoff Points in a Rural South African Community. Diabetes Care 2011, 34, 1032–1037. [Google Scholar] [CrossRef] [PubMed]
- Hoebel, S.; Malan, L.; De Ridder, H. Differences in MetS marker prevalence between black African and Caucasian teachers from the North West Province: Sympathetic Activity and Ambulatory Blood Pressure in Africans (SABPA) Study. J. Endocrinol. Metab. Diabetes South Afr. 2011, 16, 49–56. [Google Scholar] [CrossRef][Green Version]
- Sekgala, M.D.; Monyeki, K.D.; Mogale, A.; McHiza, Z.J.; Parker, W.; Choma, S.R.; Makgopa, H.M. The risk of metabolic syndrome as a result of lifestyle among Ellisras rural young adults. J. Hum. Hypertens. 2018, 32, 572–584. [Google Scholar] [CrossRef]
- Sekokotla, M.A.; Goswami, N.; Sewani-Rusike, C.R.; Iputo, J.E.; Nkeh-Chungag, B.N. Prevalence of metabolic syndrome in adolescents living in Mthatha, South Africa. Clin. Risk Manag. 2017, 13, 131–137. [Google Scholar] [CrossRef] [PubMed]
- Cornier, M.A.; Dabelea, D.; Hernandez, T.L.; Lindstrom, R.C.; Steig, A.J.; Stob, N.R.; Van Pelt, R.E.; Wang, H.; Eckel, R.H. The metabolic syndrome. Endocr. Rev. 2008, 29, 777–822. [Google Scholar]
- McNeill, A.M.; Rosamond, W.D.; Girman, C.J.; Golden, S.H.; Schmidt, M.I.; East, H.E.; Ballantyne, C.M.; Heiss, G. The metabolic syndrome and 11-year risk of incident cardiovascular disease in the atherosclerosis risk in communities study. Diabetes Care 2005, 28, 385–390. [Google Scholar] [CrossRef] [PubMed]
- Shiwaku, K.; Nogi, A.; Kitajima, K.; Anuurad, E.; Enkhmaa, B.; Yamasaki, M.; Kim, J.M.; Kim, I.S.; Lee, S.K.; Oyunsuren, T. Prevalence of the metabolic syndrome using the modified ATP III definitions for workers in Japan, Korea and Mongolia. J. Occup. Health 2005, 47, 126–135. [Google Scholar] [CrossRef] [PubMed]
- Isomaa, B. A major health hazard: The metabolic syndrome. Life Sci. 2003, 73, 2395–2411. [Google Scholar] [CrossRef]
- Nasri, H.; Moazenzadeh, M. Coronary artery disease risk factors in drivers versus people in other occupations. ARYA J. 2006, 2, 75–78. [Google Scholar]
- Masilela, C.; Pearce, B.; Ongole, J.J.; Adeniyi, O.V.; Benjeddou, M. Cross-sectional study of prevalence and determinants of uncontrolled hypertension among South African adult residents of Mkhondo municipality. BMC Public Health 2020, 20, 1069. [Google Scholar] [CrossRef]
- Bokaba, M.; Modjadji, P.; Mokwena, K.E. Undiagnosed Hypertension in a Workplace: The Case of a Logistics Company in Gauteng, South Africa. Healthcare 2021, 9, 964. [Google Scholar] [CrossRef]
- Sahadew, N.; Singaram, V.S. A diabetes profile of the eight districts in the public health sector, Eastern Cape Province, South Africa. South Afr. Med. J. 2019, 109, 957–962. [Google Scholar] [CrossRef]
- National Department of Health (NDoH); Statistics South Africa (Stats SA); South African Medical Research Council (SAMRC); ICF International. South Africa Demographic and Health Survey 2016; ICF International: Fairfax, VA, USA, 2019.
- Manning, K.; Senekal, M.; Harbron, J. Non-communicable disease risk factors and treatment preference of obese patients in Cape Town. Afr. J. Prim. Health Care. Fam. Med. 2016, 8, e1–e12. [Google Scholar] [CrossRef]
- Thorogood, M.; Connor, M.; Tollman, S.; Lewando Hundt, G.; Fowkes, G.; Marsh, J. A cross-sectional study of vascular risk factors in a rural South African population: Data from the Southern African Stroke Prevention Initiative (SASPI). BMC Public Health 2007, 7, 326. [Google Scholar] [CrossRef]
- Stern, M.P.; Williams, K.; González-Villalpando, C.; Hunt, K.J.; Haffner, S.M. Does the metabolic syndrome improve identification of individuals at risk of type 2 diabetes and/or cardiovascular disease? Diabetes Care 2004, 27, 2676–2681. [Google Scholar] [CrossRef] [PubMed]
- He, D.; Xi, B.; Xue, J.; Huai, P.; Zhang, M.; Li, J. Association between leisure time physical activity and metabolic syndrome: A meta-analysis of prospective cohort studies. Endocrine 2014, 46, 231–240. [Google Scholar] [CrossRef] [PubMed]
- Yazdi, Z.Z.; Sareshtehdary, M.; Tayefi, M. Prevalence of Metabolic Syndrome among Truck Drivers and Its Relation to Shift Work. Qom. Univ. Med. Sci. J. 2012, 5, 68–72. [Google Scholar]
- Saberi, H.R.; Moravveji, A.R.; Fakharian, E.; Kashani, M.M.; Dehdashti, A.R. Prevalence of metabolic syndrome in bus and truck drivers in Kashan, Iran. Diabetol. Metab. Syndr. 2011, 3, 8. [Google Scholar]
- Appiah, C.A.; Afriyie, E.O.; Hayford, F.E.A.; Frimpong, E. Prevalence and lifestyle-associated risk factors of metabolic syndrome among commercial motor vehicle drivers in a metropolitan city in Ghana. Pan. Afr. Med. J. 2020, 36, 136. [Google Scholar] [CrossRef]
- Kurosaka, K.; Daida, H.; Muto, T.; Watanabe, Y.; Kawai, S.; Yamaguchi, H. Characteristics of coronary heart disease in Japanese taxi drivers as determined by coronary angiographic analyses. Indian Health 2000, 38, 15–23. [Google Scholar] [CrossRef]
- Wang, P.D.; Lin, R.S. Coronary heart disease risk factors in urban bus drivers. Public Health 2001, 115, 261–264. [Google Scholar] [CrossRef]
- Singh Thakur, J.; Nangia, R.; Singh, S. Progress and challenges in achieving noncommunicable diseases targets for the sustainable development goals. FASEB Bioadv. 2021, 3, 563–568. [Google Scholar] [CrossRef]
- Baloyi, S.; Mokwena, K. Metabolic Syndrome in Reproductive Health: Urgent Call for Screening. In Lifestyle and Epidemiology-Poverty and Cardiovascular Diseases a Double Burden in African Populations; online first; IntechOpen: London, UK, 2021. [Google Scholar] [CrossRef]
- Grundy, S.M. Third report of the national cholesterol education program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III) final report. Circulation 2002, 106, 3143–3421. [Google Scholar]
- Ärnlöv, J.; Ingelsson, E.; Sundström, J.; Lind, L. Impact of Body Mass Index and the Metabolic Syndrome on the Risk of Cardiovascular Disease and Death in Middle-Aged Men. Circulation 2010, 121, 230–236. [Google Scholar] [CrossRef]
- Shrestha, B.; Dunn, L. The Declaration of Helsinki on Medical Research involving Human Subjects: A Review of Seventh Revision. J. Nepal Health Res. Counc. 2020, 17, 548–552. [Google Scholar] [CrossRef]
- Di Milia, L.; Smolensky, M.H.; Costa, G.; Howarth, H.D.; Ohayon, M.M.; Philip, P. Demographic factors, fatigue, and driving accidents: An examination of the published literature. Accid. Anal. Prev. 2011, 43, 516–532. [Google Scholar] [CrossRef]
- Bawa, M.S.; Srivastav, M. Study the epidemiological profile of taxi drivers in the background of occupational environment, stress and personality characteristics. Indian J. Occup. Environ. Med. 2013, 17, 108–113. [Google Scholar] [CrossRef]
- Lim, S.M.; Chia, S.E. The prevalence of fatigue and associated health and safety risk factors among taxi drivers in Singapore. Singapore Med. J. 2015, 56, 92–97. [Google Scholar] [CrossRef]
- Brown, I.D. Driver fatigue. Hum. Factors 1994, 36, 298–314. [Google Scholar] [CrossRef]
- Khuluvhe, M. Fact Sheet; Adult Illiteracy in South Africa. Department of Higher Education and Training, Pretoria, South Africa. 2021. Available online: www.dhet.gov.za (accessed on 20 November 2021).
- Passeri, C.; Freitas, A.; Yamashita, J.; Peres, A.; Caracik, J.; Sales Peres, S. Association of diabetes mellitus, hypertention, sleep apnea and tooth loss in class iii obese patients. In Obesity Surgery; Springer: New York, NY, USA, 2014; p. 1204. [Google Scholar]
- Peer, N.; Steyn, K.; Levitt, N. Differential obesity indices identify the metabolic syndrome in Black men and women in Cape Town: The CRIBSA study. J. Public Health 2015, 38, 175–182. [Google Scholar] [CrossRef]
- Baloyi, S.M.; Mokwena, K. Metabolic syndrome among pregnant women attending an antenatal care clinic at a tertiary hospital in the Free State province, South Africa. Obstet. Gynaecol. Forum 2020, 30, 14–18. [Google Scholar]
- Hajian-Tilaki, K. Metabolic syndrome and its associated risk factors in Iranian adults: A systematic review. Casp. J Intern. Med. 2015, 6, 51–61. [Google Scholar]
- Montazerifar, F.; Karajibani, M.; Pirmoradi, B.; Torki, Z.; Moradpour, M.; Dashipour, A. Prevalence of Metabolic Syndrome in Professional Drivers. Zahedan J. Res. Med. Sci. 2019, 21, e79768. [Google Scholar] [CrossRef]
- Ali, N.S.; Khuwaja, A.K.; Adnan Ur, R.; Nanji, K. Retrospective analysis of metabolic syndrome: Prevalence and distribution in executive population in urban pakistan. Int. J. Fam. Med. 2012, 2012, 649383. [Google Scholar] [CrossRef]
- Morimoto, A.; Nishimura, R.; Suzuki, N.; Matsudaira, T.; Taki, K.; Tsujino, D.; Miyashita, Y.; Ebara, F.; Ishikawa, S.; Tajima, N. Low prevalence of metabolic syndrome and its components in rural Japan. Tohoku J. Exp. Med. 2008, 216, 69–75. [Google Scholar] [CrossRef][Green Version]
- Todowede, O.O.; Mianda, S.Z.; Sartorius, B. Prevalence of metabolic syndrome among HIV-positive and HIV-negative populations in sub-Saharan Africa—a systematic review and meta-analysis. Syst. Rev. 2019, 8, 4. [Google Scholar] [CrossRef]
- Jaspers Faijer-Westerink, H.; Kengne, A.P.; Meeks, K.A.C.; Agyemang, C. Prevalence of metabolic syndrome in sub-Saharan Africa. A systematic review and meta-analysis. Nutr. Metab. Cardiovasc. Dis. 2020, 30, 547–565. [Google Scholar] [CrossRef]
- Kassi, E.; Pervanidou, P.; Kaltsas, G.; Chrousos, G. Metabolic syndrome: Definitions and controversies. BMC Med. 2011, 9, 48. [Google Scholar] [CrossRef]
- Kengne, A.P.; Limen, S.N.; Sobngwi, E.; Djouogo, C.F.; Nouedoui, C. Metabolic syndrome in type 2 diabetes: Comparative prevalence according to two sets of diagnostic criteria in sub-Saharan Africans. Diabetol. Metab. Syndr. 2012, 4, 22. [Google Scholar] [CrossRef]
- Alberti, K.G.; Eckel, R.H.; Grundy, S.M.; Zimmet, P.Z.; Cleeman, J.I.; Donato, K.A.; Fruchart, J.C.; James, W.P.; Loria, C.M.; Smith, S.C., Jr. Harmonizing the metabolic syndrome: A joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 2009, 120, 1640–1645. [Google Scholar]
- Kruger, H.S.; Puoane, T.; Senekal, M.; van der Merwe, M.T. Obesity in South Africa: Challenges for government and health professionals. Public Health Nutr. 2005, 8, 491–500. [Google Scholar] [CrossRef]
- Puoane, T.; Steyn, K.; Bradshaw, D.; Laubscher, R.; Fourie, J.; Lambert, V.; Mbananga, N. Obesity in South Africa: The South African demographic and health survey. Obes. Res. 2002, 10, 1038–1048. [Google Scholar] [CrossRef]
- Modjadji, P. Socio-demographic Determinants of Overweight and Obesity Among Mothers of Primary School Children Living in a Rural Health and Demographic Surveillance System Site, South Africa. Open Public Health J. 2020, 13, 518–528. [Google Scholar] [CrossRef]
- Motlhale, M.; Ncayiyana, J.R. Migration status and prevalence of diabetes and hypertension in Gauteng province, South Africa: Effect modification by demographic and socioeconomic characteristics-a cross-sectional population-based study. BMJ Open 2019, 9, e027427. [Google Scholar] [CrossRef]
- Peltzer, K.; Phaswana-Mafuya, N. Hypertension and associated factors in older adults in South Africa. Cardiovasc. J. Afr. 2013, 24, 67–71. [Google Scholar] [CrossRef]
- Gaziano, T.A.; Abrahams-Gessel, S.; Gomez-Olive, F.X.; Wade, A.; Crowther, N.J.; Alam, S.; Manne-Goehler, J.; Kabudula, C.W.; Wagner, R.; Rohr, J.; et al. Cardiometabolic risk in a population of older adults with multiple co-morbidities in rural south africa: The HAALSI (Health and Aging in Africa: Longitudinal studies of INDEPTH communities) study. BMC Public Health 2017, 17, 206. [Google Scholar] [CrossRef]
- Mohebbi, I.; Saadat, S.; Aghassi, M.; Shekari, M.; Matinkhah, M.; Sehat, S. Prevalence of metabolic syndrome in Iranian professional drivers: Results from a population based study of 12,138 men. PLoS ONE 2012, 7, e31790. [Google Scholar] [CrossRef]
- Miranda, P.J.; DeFronzo, R.A.; Califf, R.M.; Guyton, J.R. Metabolic syndrome: Definition, pathophysiology, and mechanisms. Am. Heart J. 2005, 149, 33–45. [Google Scholar] [CrossRef]
- Vardavas, C.I.; Linardakis, M.K.; Hatzis, C.M.; Saris, W.H.; Kafatos, A.G. Cardiovascular disease risk factors and dietary habits of farmers from Crete 45 years after the first description of the Mediterranean diet. Eur. J. Prev. Cardiol. 2010, 17, 440–446. [Google Scholar] [CrossRef]
- Åberg, F.; Helenius-Hietala, J.; Puukka, P.; Färkkilä, M.; Jula, A. Interaction between alcohol consumption and metabolic syndrome in predicting severe liver disease in the general population. Hepatology 2018, 67, 2141–2149. [Google Scholar] [CrossRef]
- Abban, H. Cardiovascular Diseases Risk Factors Among Commercial Long Distance Bus Drivers in Cape Coast; University of Ghana: Accra, Ghana, 2013. [Google Scholar]
- Hu, X.; Yu, W.; Yang, L.; Pan, W.; Si Qya Chen, X.; Li, Q.; Gu, X. The Association Between First-Degree Family History of Diabetes and Metabolic Syndrome. Endocr. Pract. 2019, 25, 678–683. [Google Scholar] [CrossRef]
- Ranasinghe, P.; Cooray, D.N.; Jayawardena, R.; Katulanda, P. The influence of family history of Hypertension on disease prevalence and associated metabolic risk factors among Sri Lankan adults. BMC Public Health 2015, 15, 576. [Google Scholar] [CrossRef]
- Khanna, N.; Sharma, R.S.; Sidhu, R.S. A study of the basic and derived anthropometric indices among the healthy adults (20–30 years of age) of amritsar city (punjab) having family history of hypertension. Int. J. Biol. Med. Res. 2011, 2, 743–746. [Google Scholar]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).