Influence of 2% Chlorhexidine on the Bond Strength of Three Adhesive Systems on Primary Molars: An In Vitro Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Specimens Preparation
2.3. Specimen Treatments
2.4. Bond Strength Evaluation
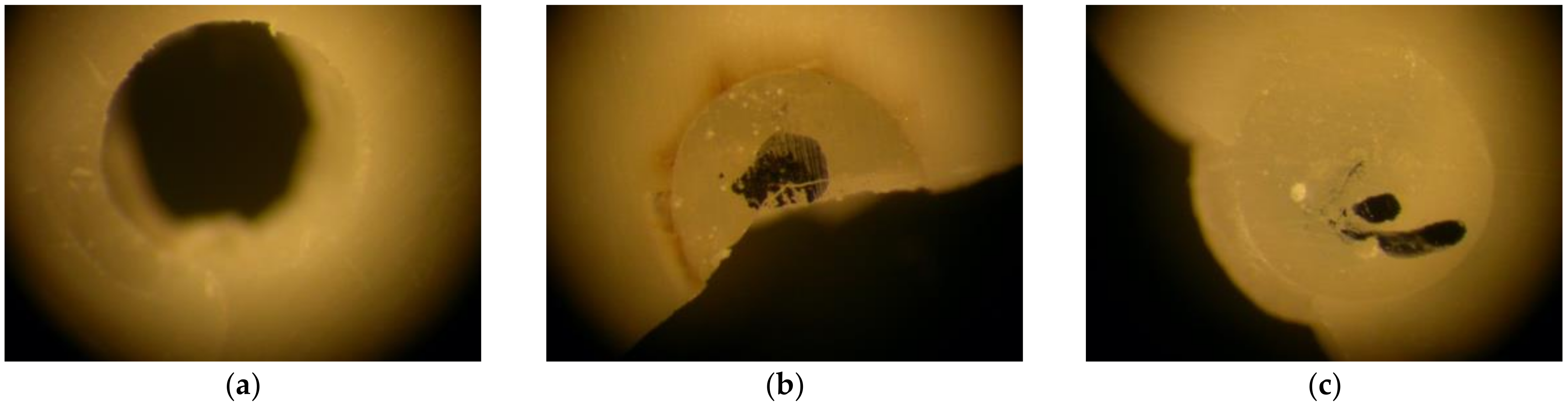
2.5. Failure Type Evaluation
2.6. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
- The application of 2% chlorhexidine for 60 s as dentine pretreatment, with the aim of inhibiting the activity of MMPs, did not impact the immediate bond strength of the different adhesive systems used in primary dentition.
- Self-etch and total-etch adhesive systems were shown to have the best BS values in primary dentition, in contrast to universal adhesive systems, which have the lowest BS values.
- Bonding strategies in the field of paediatric restorative dentistry should be directed towards simplified, effective and efficient adhesive protocols. This study sheds light on this field, corroborating the proposal that the addition of an extra step in the bonding process, without slowing down the process, improves the prospects of these restorations over time, without decreasing their quality. Nevertheless, further clinical studies are needed to confirm these findings.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lenzi, T.L.; Raggio, D.P.; Soares, F.Z.M.; de Oliveira Rocha, R. Bonding Performance of a Multimode Adhesive to Artificially induced Caries-affected Primary Dentin. J. Adhes. Dent. 2015, 17, 125–131. [Google Scholar] [PubMed]
- Coelho, A.; Amaro, I.; Apolónio, A.; Paula, A.; Saraiva, J.; Ferreira, M.; Marto, C.; Carrilho, E. Effect of Cavity Disinfectants on Adhesion to Primary Teeth—A Systematic Review. Int. J. Mol. Sci. 2021, 22, 4398. [Google Scholar] [CrossRef] [PubMed]
- Van Meerbeek, B.; Peumans, M.; Poitevin, A.; Mine, A.; Van Ende, A.; Neves, A.; De Munck, J. Relationship between bond-strength tests and clinical outcomes. Dent. Mater. 2010, 26, e100–e121. [Google Scholar] [CrossRef] [PubMed]
- Pashley, D.H.; Tay, F.R.; Breschi, L.; Tjäderhane, L.; Carvalho, R.M.; Carrilho, M.; Tezvergil-Mutluay, A. State of the art etch-and-rinse adhesives. Dent. Mater. 2011, 27, 1–16. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Manfro, A.R.G.; Reis, A.; Loguercio, A.D.; Imparato, J.C.P.; Raggio, D.P. Effect of different concentrations of chlorhexidine on bond strength of primary dentin. Pediatr. Dent. 2012, 34, 11–15. [Google Scholar]
- Lenzi, T.L.; Soares, F.; Rocha, R. Degradation of resin-dentin bonds of etch-and-rinse adhesive system to primary and permanent teeth. Braz. Oral Res. 2012, 26, 511–515. [Google Scholar] [CrossRef] [Green Version]
- Leitune, V.; Portella, F.; Bohn, P.V.; Collares, F.M.; Samuel, S.M.W. Influence of chlorhexidine application on longitudinal adhesive bond strength in deciduous teeth. Braz. Oral Res. 2011, 25, 388–392. [Google Scholar] [CrossRef] [Green Version]
- Breschi, L.; Mazzoni, A.; Ruggeri, A.; Cadenaro, M.; Di Lenarda, R.; De Stefano Dorigo, E. Dental adhesion review: Aging and stability of the bonded interface. Dent. Mater. 2008, 24, 90–101. [Google Scholar] [CrossRef]
- Kim, J.; Uchiyama, T.; Carrilho, M.; Agee, K.A.; Mazzoni, A.; Breschi, L.; Carvalho, R.M.; Tjäderhane, L.; Looney, S.; Wimmer, C.; et al. Chlorhexidine binding to mineralized versus demineralized dentin powder. Dent. Mater. 2010, 26, 771–778. [Google Scholar] [CrossRef] [Green Version]
- Breschi, L.; Cammelli, F.; Visintini, E.; Mazzoni, A.; Vita, F.; Carrilho, M.; Cadenaro, M.; Foulger, S.; Mazzoti, G.; Tay, F.R.; et al. Influence of chlorhexidine concentration on the durability of etch-and-rinse dentin bonds: A 12-month in vitro study. J. Adhes. Dent. 2009, 11, 191–198. [Google Scholar]
- Tjäderhane, L.; Nascimento, F.D.; Breschi, L.; Mazzoni, A.; Tersariol, I.; Geraldeli, S.; Tezvergil-Mutluay, A.; Carrilho, M.; Carvalho, R.M.; Tay, F.R.; et al. Strategies to prevent hydrolytic degradation of the hybrid layer—A review. Dent. Mater. 2013, 29, 999–1011. [Google Scholar] [CrossRef] [Green Version]
- Montagner, A.; Sarkis-Onofre, R.; Pereira-Cenci, T.; Cenci, M. MMP Inhibitors on Dentin Stability. J. Dent. Res. 2014, 93, 733–743. [Google Scholar] [CrossRef] [Green Version]
- Carrilho, M.R.; Carvalho, R.M.; Sousa, E.N.; Nicolau, J.; Breschi, L.; Mazzoni, A.; Tjäderhane, L.; Tay, F.R.; Agee, K.; Pashley, D.H. Substantivity of chlorhexidine to human dentin. Dent. Mater. 2010, 26, 779–785. [Google Scholar] [CrossRef] [Green Version]
- Carrilho, M.; Geraldeli, S.; Tay, F.; de Goes, M.; Carvalho, R.; Tjäderhane, L.; Reis, A.; Hebling, J.; Mazzoni, A.; Breschi, L.; et al. In vivo Preservation of the Hybrid Layer by Chlorhexidine. J. Dent. Res. 2007, 86, 529–533. [Google Scholar] [CrossRef]
- Visse, R.; Nagase, H. Matrix metalloproteinases and tissue inhibitors of metalloproteinases: Structure, function, and biochemistry. Circ. Res. 2003, 92, 827–839. [Google Scholar] [CrossRef] [Green Version]
- Bourd-Boittin, K.; Fridman, R.; Fanchon, S.; Septier, D.; Goldberg, M.; Menashi, S. Matrix metalloproteinase inhibition impairs the processing, formation and mineralization of dental tissues during mouse molar development. Exp. Cell Res. 2005, 304, 493–505. [Google Scholar] [CrossRef]
- ElKassas, D.W.; Fawzi, E.M.; El Zohairy, A. The effect of cavity disinfectants on the micro-shear bond strength of dentin adhesives. Eur. J. Dent. 2014, 8, 184–190. [Google Scholar] [CrossRef]
- Suma, N.K.; Shashibhushan, K.K.; Reddy, V.S. Effect of Dentin Disinfection with 2% Chlorhexidine Gluconate and 0.3% Iodine on Dentin Bond Strength: An in vitro Study. Int. J. Clin. Pediatr. Dent. 2017, 10, 223–228. [Google Scholar] [CrossRef]
- De Sousa Vieira, R.; Da Silva, I.A. Bond strength to primary tooth dentin following disinfection with a chlorhexidine solution: An in vitro study. Pediatr. Dent. 2003, 25, 49–52. [Google Scholar]
- AENOR. Water for Laboratory Analysis. Specification and Test Methods. UNE-EN ISO 3696:1996. 1996. Available online: https://tienda.aenor.com/norma-une-en-iso-3696-1996-n0013433 (accessed on 2 February 2022).
- World Medical Association. World Medical Association Declaration of Helsinki: Ethical Principles for Medical Research Involving Human Subjects. JAMA 2013, 310, 2191. [Google Scholar] [CrossRef] [Green Version]
- AENOR. Dentistry. Adhesion. Notched-Edge Shear Bond Strength Test. UNE-EN ISO 29022:2013. 2013. Available online: https://www.une.org/encuentra-tu-norma/busca-tu-norma/norma?c=N0052311 (accessed on 2 February 2022).
- Del Río Carrillo, R.M.; Molinero-Mourelle, P.; Vera, V.; Romero Villaba, P.; Casañas, E.; Fonseca, M.; Vera-Gonzalez, V.; Mourelle-Martinez, M.R. Micro Push-Out Bond Strength of Resin Composite to Dentin in Primary Dentition Using Three Universal Adhesives with Different pH: An In Vitro Study. Appl. Sci. 2021, 11, 6349. [Google Scholar] [CrossRef]
- Ghajari, M.F.; Ghasemi, A.; Badiee, M.; Abdolazimi, Z.; Baghban, A.A. Microshear Bond Strength of Scotchbond Universal Adhesive to Primary and Permanent Dentin: A Six-Month In Vitro Study. Front. Dent. 2019, 16, 173–180. [Google Scholar] [CrossRef]
- Abdelmegid, F.Y. Bond Strength to primary teeth dentin following disinfection with 2% chlorhexidine. Int. J. Oral Dent. Health 2018, 4, 49. [Google Scholar]
- Manfro, A.R.G.; Reis, A.; Loguercio, A.D.; Imparato, J.C.P.; Raggio, D.P. Effect of chlorhexidine concentration on the bond strength to dentin in primary teeth. Rev. Odonto Ciênc. 2010, 25, 88–91. [Google Scholar] [CrossRef] [Green Version]
- Lenzi, T.L.; Tedesco, T.K.; Soares, F.; Loguercio, A.D.; Rocha, R.D.O. Chlorhexidine does not increase immediate bond strength of etch-and-rinse adhesive to caries-affected dentin of primary and permanent teeth. Braz. Dent. J. 2012, 23, 438–442. [Google Scholar] [CrossRef] [Green Version]
- Ricci, H.A.; Sanabe, M.E.; Costa, C.A.D.S.; Hebling, J. Effect of chlorhexidine on bond strength of two-step etch-and-rinse adhesive systems to dentin of primary and permanent teeth. Am. J. Dent. 2010, 23, 128–132. [Google Scholar]
- Ricci, H.A.; Sanabe, M.E.; Costa, C.A.D.S.; Pashley, D.H.; Hebling, J. Chlorhexidine increases the longevity of in vivo resin-dentin bonds. Eur. J. Oral Sci. 2010, 118, 411–416. [Google Scholar] [CrossRef]
- Lenzi, T.L.; Tedesco, T.; Soares, F.; Loguercio, A.D.; Rocha, R. Chlorhexidine application for bond strength preservation in artificially-created caries-affected primary dentin. Int. J. Adhes. Adhes. 2014, 54, 51–56. [Google Scholar] [CrossRef]
- Hamdan-Nassar, T.; Bellot-Arcís, C.; Paredes-Gallardo, V.; García-Sanz, V.; Pascual-Moscardó, A.; Almerich-Silla, J.M.; Montiel-Company, J.M. Effect of 2% Chlorhexidine Following Acid Etching on Microtensile Bond Strength of Resin Restorations: A Meta-Analysis. Medicina 2019, 55, 769. [Google Scholar] [CrossRef] [Green Version]
- Nishitani, Y.; Yoshiyama, M.; Wadgaonkar, B.; Breschi, L.; Mannello, F.; Mazzoni, A.; Carvalho, R.M.; Tjaderhane, L.; Tay, F.R.; Pashley, D.H. Activation of gelatinolytic/collagenolytic activity in dentin by self-etching adhesives. Eur. J. Oral Sci. 2006, 114, 160–166. [Google Scholar] [CrossRef]
- Zheng, P.; Zaruba, M.; Attin, T.; Wiegand, A. Effect of different matrix metalloproteinase inhibitors on microtensile bond strength of an etch-and-rinse and a self-etching adhesive to dentin. Oper. Dent. 2015, 40, 80–86. [Google Scholar] [CrossRef] [Green Version]
- Carvalho, R.M.; Yoshiyama, M.; Brewer, P.D.; Pashley, D.H. Dimensional changes of demineralized human dentine during preparation for scanning electron microscopy. Arch. Oral Biol. 1996, 41, 379–386. [Google Scholar] [CrossRef]
- Frassetto, A.; Breschi, L.; Turco, G.; Marchesi, G.; Di Lenarda, R.; Tay, F.; Pashley, D.H.; Cadenaro, M. Mechanisms of degradation of the hybrid layer in adhesive dentistry and therapeutic agents to improve bond durability—A literature review. Dent. Mater. 2016, 32, e41–e53. [Google Scholar] [CrossRef]
- El Mourad, A.M. Assessment of Bonding Effectiveness of Adhesive Materials to Tooth Structure using Bond Strength Test Methods: A Review of Literature. Open Dent. J. 2018, 12, 664–678. [Google Scholar] [CrossRef] [Green Version]
- Chang, Y.-E.; Shin, D.-H. Effect of Chlorhexidine Application Methods on Microtensile Bond Strength to Dentin in Class I Cavities. Oper. Dent. 2010, 35, 618–623. [Google Scholar] [CrossRef]
- Loguercio, A.D.; Stanislawczuk, R.; Polli, L.G.; Costa, J.A.; Michel, M.D.; Reis, A. Influence of chlorhexidine digluconate concentration and application time on resin-dentin bond strength durability. Eur. J. Oral Sci. 2009, 117, 587–596. [Google Scholar] [CrossRef]
- Stanislawczuk, R.; Amaral, R.C.; Zander-Grande, C.; Gagler, D.; Reis, A.; Loguercio, A.D. Chlorhexidine-containing Acid Conditioner Preserves the Longevity of Resin-dentin Bonds. Oper. Dent. 2009, 34, 481–490. [Google Scholar] [CrossRef]
- Zeppieri, I.L.; Chung, C.H.; Mante, F.K. Effect of saliva on shear bond strength of an orthodontic adhesive used with moisture-insesitive and self-etching primers. Am. J. Orthod. Dentofac. Orthop. 2003, 124, 414–419. [Google Scholar] [CrossRef]
- Cacciafesta, V.; Sfondrini, M.F.; Scribante, A.; De Angelis, M.; Klersy, C. Effects of blood contamination on the shear bond strengths of conventional and hydrophilic primers. Am. J. Orthod. Dentofac. Orthop. 2004, 126, 207–212. [Google Scholar] [CrossRef]

| Group | Adhesive Process |
|---|---|
| Scotchbond Universal self-etch (S) | Adhesive, light cure 10 s |
| CHX and Scotchbond Universal total-etch (S-C) | CHX 60 s, dry, adhesive, light cure 10 s |
| Scotchbond Universal total-etch (Sa) | Etching 7 s, wash, adhesive, light cure 10 s |
| CHX and Scotchbond Universal total-etch (Sa-C) | Etching 7 s, wash, CHX 60 s, dry, adhesive, light cure 10 s |
| Adper Prompt L-Pop (PL) | Adhesive, light cure 10 s |
| CHX and Adper Prompt L-Pop (PL-C) | CHX 60 s, dry, adhesive, light cure 10 s |
| Adper Scotchbond 1XT (XTa) | Etching 7 s, wash, adhesive, light cure 10 s |
| CHX and Adper Scotchbond 1XT (XTa-C) | Etching 7 s, wash, CHX 60 s, dry, adhesive, light cure 10 s |
| Material | Type | Composition | Manufacturer |
|---|---|---|---|
| Scotchbond™ Universal | Universal adhesive | MDP phosphate monomer, di-methacrylate resins, HEMA, Vitrebond copolymer, filler, ethanol, water, initiators, silane | 3M ESPE, St Paul, MN, USA |
| Adper™ Prompt™ L-Pop™ | Self-Etch Adhesive | Methacrylate phosphoric esters, Bis-GMA, camphorquinone, stabilizers, water, HEMA, polyalkenoic acid | 3M ESPE, St Paul, MN, USA |
| Adper™ Scotchbond™ 1XT | Total-Etch Adhesive | HEMA, polyalkenoic acid copolymer, Bis-GMA, water-camphorquinone, ethanol | 3M ESPE, St Paul, MN, USA |
| Scotchbond™ Etchant | Etchant Gel | Water, 35% phosphoric acid, synthetic amorphous silica, polyethylene glycol, NUC-Aluminum oxide | 3M ESPE, St Paul, MN, USA |
| Tetric EvoCeram® Bulk Fill | Light-curing nano-hybrid composite | Bis-GMA, urethane dimethacrylate, ytterbium trifluoride, Bis-EMA | Ivoclar Vivadent, AG Gabathuler, Schaan, Liechtenstein |
| Canal Pro CHX 2% | Pretreatment | Chlorhexidine digluconate 2% | Coltène, Langenau, Germany |
| Bond Strength (MPa) | |||||
|---|---|---|---|---|---|
| Type of Adhesive | |||||
| Mean (SD) | Total Mean (SD) | ||||
| Pretreatment | Scotchbond Universal self-etch | Scotchbond Universal total-etch | Adper Prompt L-Pop | Adper Scotchbond 1XT | |
| without CHX | 17.28 (9.48) | 15.28 (4.45) | 20.41 (7.05) | 19.85 (7.47) | 18.21 (7.45) |
| with CHX | 15.01 (7.61) | 17.39 (5.24) | 20.13 (4.69) | 18.59 (5.13) | 17.78 (5.95) |
| Bond Strength (MPa) | ||||
|---|---|---|---|---|
| Type of Adhesive | ||||
| Mean (SD) | Total Mean (SD) | |||
| Scotchbond Universal self-etch | Scotchbond Universal total-etch | Adper Prompt L-Pop | Adper Scotchbond 1XT | |
| 16.15 (8.53) | 16.34 (4.90) | 20.27 (5.89) | 19.22 (6.34) | 17.99 (6.72) |
| Type of Adhesive | Pretreatment | Group | Type of Failure | ||
|---|---|---|---|---|---|
| % (n° Cases) | |||||
| Adhesive | Cohesive | Mixed | |||
| Scotchbond Universal self-etch | without CHX | S | 18.8% (3) | 43.8% (7) | 37.5% (6) |
| with CHX | S-C | 12.5% (2) | 56.3% (9) | 31.3% (5) | |
| Scotchbond Universal total-etch | without CHX | Sa | 6.3% (1) | 62.5% (10) | 31.3% (5) |
| with CHX | Sa-C | 31.3% (5) | 31.3% (5) | 37.5% (6) | |
| Adper Prompt L-pop | without CHX | PL | 31.3% (5) | 37.5% (6) | 31.3% (5) |
| with CHX | PL-C | 25% (4) | 31.3% (5) | 43.8% (7) | |
| Adper Scotchbond 1XT | without CHX | XTa | 43.8% (7) | 18.8% (3) | 37.5% (6) |
| with CHX | XTa-C | 37.5% (6) | 12.5% (2) | 50% (8) | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Velayos-Galán, L.; Molinero-Mourelle, P.; Sevilla, P.; Fonseca, M.; Mourelle-Martínez, M.R.; Vera-González, V. Influence of 2% Chlorhexidine on the Bond Strength of Three Adhesive Systems on Primary Molars: An In Vitro Study. Appl. Sci. 2022, 12, 2964. https://doi.org/10.3390/app12062964
Velayos-Galán L, Molinero-Mourelle P, Sevilla P, Fonseca M, Mourelle-Martínez MR, Vera-González V. Influence of 2% Chlorhexidine on the Bond Strength of Three Adhesive Systems on Primary Molars: An In Vitro Study. Applied Sciences. 2022; 12(6):2964. https://doi.org/10.3390/app12062964
Chicago/Turabian StyleVelayos-Galán, Laura, Pedro Molinero-Mourelle, Pablo Sevilla, Manrique Fonseca, María Rosa Mourelle-Martínez, and Vicente Vera-González. 2022. "Influence of 2% Chlorhexidine on the Bond Strength of Three Adhesive Systems on Primary Molars: An In Vitro Study" Applied Sciences 12, no. 6: 2964. https://doi.org/10.3390/app12062964






