Orthognathic versus Camouflage Treatment of Class III Malocclusion: A Systematic Review and Meta-Analysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Search Strategy
2.2. Quality Analysis
2.3. Quantitative Analysis
2.4. Statistical Analysis
3. Results
3.1. Selection of Studies
3.2. Quality Assessment
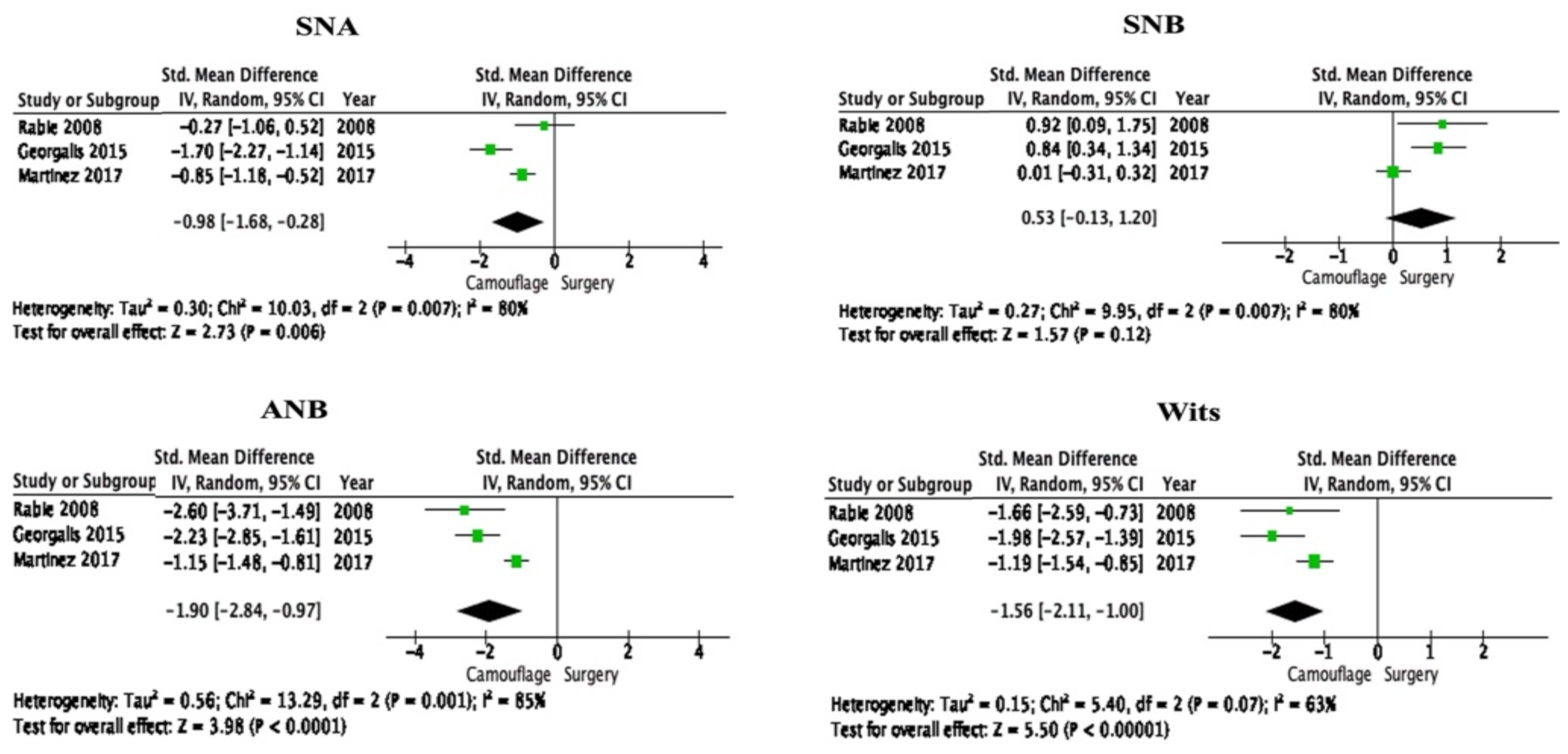
3.3. Meta-Analysis from Selected Studies
3.4. Publication Bias
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Poulton, D.; Ware, W. The American academy of oral roentgenology joins our journal. Oral Surg. Oral Med. Oral Pathol. 1959, 12, 389–390. [Google Scholar]
- Trauner, R.; Obwegeser, H. The surgical correction of mandibular prognathism and retrognathia with consideration of genioplasty: Part I. Surgical procedures to correct mandibular prognathism and reshaping of the chin. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 1957, 10, 677–689. [Google Scholar]
- Obwegeser, H.L. Surgical correction of small or retrodisplaced maxillae the “dish-face” deformity. Plast. Reconstr. Surg. 1969, 43, 351–365. [Google Scholar]
- Proffit, W.; Fields, H.; Sarver, D. Biomechanics, Mechanics, and Contemporary Orthodontic Appliances, Contemporary Orthodontics; Mosby, Elsevier: St. Louis, MO, USA, 2007; pp. 689–693. [Google Scholar]
- Troy, B.A.; Shanker, S.; Fields, H.W.; Vig, K.; Johnston, W. Comparison of incisor inclination in patients with Class III malocclusion treated with orthognathic surgery or orthodontic camouflage. Am. J. Orthod. Dentofac. Orthop. 2009, 135, 146. [Google Scholar]
- Burns, N.R.; Musich, D.R.; Martin, C.; Razmus, T.; Gunel, E.; Ngan, P. Class III camouflage treatment: What are the limits? Am. J. Orthod. Dentofac. Orthop. 2010, 137, 9–13. [Google Scholar]
- Araujo, M.T.D.S.; Squeff, L.R. Orthodontic camouflage as a treatment alternative for skeletal Class III. J. Orthod. 2021, 26, e21bbo4. [Google Scholar]
- Proffit, W.R.; Fields, H.; Sarver, D. Diagnosis and Treatment Planning, Contemporary Orthodontics; Mosby, Elsevier: St. Louis, MO, USA, 2007; Volume 160, pp. 207–217. [Google Scholar]
- Kondo, E.; Arai, S. Nonsurgical and non extraction treatment of a skeletal class III adult patient with severe prognathic mandible. World J. Orthod. 2005, 6, 233–247. [Google Scholar]
- Kuroda, Y.; Kuroda, S.; Alexander, R.G.; Tanaka, E. Adult Class III treatment using a J-hook headgear to the mandibular arch. Angle Orthod. 2010, 80, 336–343. [Google Scholar]
- Lübberink, G.; Nienkemper, M.; Wilmes, B.; Ludwig, B.; Drescher, D. Nonsurgical treatment of a mature adult Class III patient. J. Clin. Orthod. 2014, 48, 697–702. [Google Scholar]
- Miguel, J.A.M.; Zanardi, G. Class III camouflage using skeletal anchorage and Pendex appliance. Prog. Orthod. 2011, 12, 73–83. [Google Scholar]
- Nakamura, Y.; Miyamoto, Y.; Kanzaki, H.; Wada, S. Orthodontic Treatment of an Adult Class III Malocclusion with Severe Transverse Dental Compensation by Remaining of Buccal Crossbite. Int. J. Orthod. Milwaukee 2015, 26, 29–35. [Google Scholar] [PubMed]
- Stellzig-Eisenhauer, A.; Lux, C.J.; Schuster, G. Treatment decision in adult patients with Class III malocclusion: Orthodontic therapy or orthognathic surgery? Am. J. Orthod. Dentofac. Orthop. 2002, 122, 27–37. [Google Scholar]
- Rabie, A.-B.M.; Wong, R.W.; Min, G. Treatment in borderline Class III malocclusion: Orthodontic camouflage (extraction) versus orthognathic surgery. Open Dent. J. 2008, 2, 38–48. [Google Scholar] [PubMed] [Green Version]
- Kerr, W.; Miller, S.; Dawber, J. Class III malocclusion: Surgery or orthodontics? Br. J. Orthod. 1992, 19, 21–24. [Google Scholar] [PubMed]
- Hardy, D.K.; Cubas, Y.P.; Orellana, M.F. Prevalence of angle class III malocclusion: A systematic review and meta-analysis. Open J. Epidemiol. 2012, 2, 75–82. [Google Scholar]
- Dehesa-Santos, A.; Iber-Diaz, P.; Iglesias-Linares, A. Genetic factors contributing to skeletal class III malocclusion: A systematic review and meta-analysis. Clin. Oral Investig. 2021, 25, 1587–1612. [Google Scholar]
- Lin, Y.; Guo, R.; Hou, L.; Fu, Z.; Li, W. Stability of maxillary protraction therapy in children with Class III malocclusion: A systematic review and meta-analysis. Clin. Oral Investig. 2018, 22, 2639–2652. [Google Scholar]
- Yang, X.; Li, C.; Bai, D.; Su, N.; Chen, T.; Xu, Y.; Han, X. Treatment effectiveness of Fränkel function regulator on the Class III malocclusion: A systematic review and meta-analysis. Am. J. Orthod. Dent. Orthop. 2014, 146, 143–154. [Google Scholar]
- Chatzoudi, M.I.; Ioannidou-Marathiotou, I.; Papadopoulos, M.A. Clinical effectiveness of chin cup treatment for the management of Class III malocclusion in pre-pubertal patients: A systematic review and meta-analysis. Prog. Orthod. 2014, 15, 62. [Google Scholar]
- Zhang, W.; Qu, H.-C.; Yu, M.; Zhang, Y. The effects of maxillary protraction with or without rapid maxillary expansion and age factors in treating class III malocclusion: A meta-analysis. PLoS ONE 2015, 10, e0130096. [Google Scholar]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, 336–341. [Google Scholar]
- Downs, S.; Black, N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. JECH 1998, 52, 377–384. [Google Scholar]
- Raposo, R.; Peleteiro, B.; Paço, M.; Pinho, T. Orthodontic camouflage versus orthodontic-orthognathic surgical treatment in class II malocclusion: A systematic review and meta-analysis. Int. J. Oral Maxillofac. Surg. 2018, 47, 445–455. [Google Scholar] [PubMed] [Green Version]
- Landis, J.R.; Koch, G.G. The measurement of observer agreement for categorical data. Biometrics 1977, 33, 159–174. [Google Scholar] [PubMed]
- Eslami, S.; Faber, J.; Fateh, A.; Sheikholaemmeh, F.; Grassia, V.; Jamilian, A. Treatment decision in adult patients with class III malocclusion: Surgery versus orthodontics. Prog. Orthod. 2018, 19, 28. [Google Scholar]
- Tseng, Y.-C.; Pan, C.-Y.; Chou, S.-T.; Liao, C.-Y.; Lai, S.-T.; Chen, C.-M.; Chang, H.-P.; Yang, Y.-H. Treatment of adult Class III malocclusions with orthodontic therapy or orthognathic surgery: Receiver operating characteristic analysis. Am. J. Orthod. Dentofac. Orthop. 2011, 139, 485–493. [Google Scholar]
- Xiong, X.; Yu, Y.; Chen, F. Orthodontic camouflage versus orthognathic surgery: A comparative analysis of long-term stability and satisfaction in moderate skeletal Class III. OJST 2013, 3, 89–93. [Google Scholar]
- Georgalis, K.; Woods, M.G. A study of Class III treatment: Orthodontic camouflage vs. orthognathic surgery. Aust. Orthod. J. 2015, 31, 138–148. [Google Scholar]
- Martinez, P.; Bellot-Arcís, C.; Llamas, J.M.; Cibrian, R.; Gandia, J.L.; Paredes-Gallardo, V. Orthodontic camouflage versus orthognathic surgery for class III deformity: Comparative cephalometric analysis. Int. J. Oral Maxillofac. Surg. 2017, 46, 490–505. [Google Scholar]
- Wu, F.; Wang, L.; Huang, Y.; Guo, W.; Liu, C.; Li, S. Interleukin-1β+ 3954 polymorphisms and risk of external apical root resorption in orthodontic treatment: A meta-analysis. Genet. Mol. Res. 2013, 12, 4678–4686. [Google Scholar]
- Nowrin, S.A.; Jaafar, S.; Ab Rahman, N.; Basri, R.; Alam, M.K.; Shahid, F. Association between genetic polymorphisms and external apical root resorption: A systematic review and meta-analysis. Korean J. Orthod. 2018, 48, 395–404. [Google Scholar] [PubMed]
- Higgins, J.P.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V. Cochrane Handbook for Systematic Reviews of Interventions; John Wiley & Sons: Hoboken, NJ, USA, 2019. [Google Scholar]
- Jamilian, A.; Cannavale, R.; Piancino, M.G.; Eslami, S.; Perillo, L. Methodological quality and outcome of systematic reviews reporting on orthopaedic treatment for class III malocclusion: Overview of systematic reviews. J. Orthod. 2016, 43, 102–120. [Google Scholar] [PubMed]
- Kabbur, K.J.; Hemanth, M.; Patil, G.; Sathyadeep, V.; Shamnur, N.; Harieesha, K.; Praveen, G. An esthetic treatment outcome of orthognathic surgery and dentofacial orthopedics in class II treatment: A cephalometric study. J. Contemp. Dent. Pract. 2012, 13, 602–606. [Google Scholar] [PubMed]



| Variables | Description |
|---|---|
| Participants | Class III malocclusion |
| Interventions | Orthognathic surgery |
| Comparisons | Camouflage treatment |
| Outcomes | Skeletal and dental measurements from lateral cephalogram |
| Study designs | Observational and interventional studies |
| Study (Year) | Country | Sample Size | Study Design | Intervention | Outcome | |
|---|---|---|---|---|---|---|
| Camouflage | Surgical | |||||
| Eslami et al. (2018) [27] | Iran | 65 | Retrospective | 36 | 29 | Wits appraisal and Holdway H angle could be utilized to determine the treatment modality in borderline C-III-M. |
| Tseng et al. (2011) [28] | Taiwan | 80 | Retrospective | 40 | 40 | Minimum six cephalometric measurements are required to attain effective diagnosis between nonsurgical and surgical treatment in C-III-M. |
| Xiong et al. (2013) [29] | China | 46 | Retrospective | 25 | 21 | Camouflage treatment could be a choice of treatment for patients who denied orthognathic surgery |
| Georgalis et al. (2015) [30] | Australia | 67 | Retrospective | 31 | 36 | Treatment of C-III-M is expected to complete with slightly proclined upper incisors in both surgery and camouflage treatment. |
| Martinez et al. (2017) [31] | Spain | 156 | Retrospective | 77 | 79 | Three skeletal and two dental measurements showed a significant difference between surgical and camouflage treatment groups. |
| Rabie et al. (2008) [32] | Hong Kong | 25 | Retrospective | 13 | 12 | For patients with borderline C-III-M, the Holdway angle could be a reliable guide to determine the modality of treatment. |
| Assessment | Eslami et al. (2018) [27] | Georgalis et al. (2015) [30] | Martinez et al. (2017) [31] | Rabie et al. (2008) [15] | Tseng et al. 2011 [28] | Xiong et al. (2013) [29] |
|---|---|---|---|---|---|---|
| Reporting (Q1–Q10) | ||||||
| Q1: Aim clearly described | 1 | 1 | 1 | 1 | 1 | 1 |
| Q2: Outcomes clearly described | 1 | 1 | 1 | 1 | 1 | 1 |
| Q3: Patients’ characteristics clearly described | 1 | 1 | 1 | 1 | 1 | 1 |
| Q4: Interventions clearly described | 1 | 1 | 1 | 1 | 1 | 1 |
| Q5: Principal confounders clearly described | 0 | 0 | 1 | 1 | 1 | 1 |
| Q6: Main findings clearly described | 1 | 1 | 1 | 1 | 1 | 1 |
| Q7: Random variability for the main outcome provided | 1 | 1 | 1 | 1 | 1 | 1 |
| Q8: Adverse events reported | 1 | 1 | 1 | 1 | 1 | 1 |
| Q9: Lost to follow up reported | 0 | 0 | 0 | 1 | 1 | 0 |
| Q10: Actual p value reported | 1 | 0 | 1 | 0 | 1 | 0 |
| Score | 8 | 7 | 9 | 8 | 10 | 8 |
| External Validity (Q11–Q13) and Internal Validity-Bias (Q14–Q20) | ||||||
| Q11: Sample asked to participate representative of the population | 0 | 0 | 0 | 1 | 0 | 0 |
| Q12: Sample agreed to participate representative of the population | 0 | 0 | 0 | 0 | 0 | 0 |
| Q13: Staff participating representative to the patient’s environment | 0 | 0 | 0 | 0 | 0 | 0 |
| Q14: Attempt to blind participants | 0 | 0 | 0 | 0 | 0 | 0 |
| Q15: Attempt to blind assessors | 1 | 1 | 0 | 0 | 0 | 0 |
| Q16: Data dredging results stated clearly | 1 | 1 | 1 | 1 | 1 | 1 |
| Q17: Analysis adjusted for length of follow up | 0 | 0 | 0 | 0 | 0 | 1 |
| Q18: Appropriate statistics | 1 | 1 | 1 | 1 | 1 | 1 |
| Q19: Reliable compliance | 1 | 1 | 1 | 1 | 1 | 1 |
| Q20: Accurate outcome | 1 | 1 | 1 | 1 | 1 | 1 |
| Score | 5 | 5 | 4 | 5 | 4 | 5 |
| Internal Validity–Confounding (selection bias) (Q21–Q26) and Power (Q27) | ||||||
| Q21: Same population | 1 | 1 | 1 | 1 | 1 | 1 |
| Q22: Participants recruited at the same time | 0 | 0 | 0 | 0 | 0 | 0 |
| Q23: Randomised? | 0 | 0 | 0 | 0 | 0 | 0 |
| Q24: Adequate allocation concealment? | 0 | 0 | 0 | 0 | 0 | 0 |
| Q25: Adequate adjustment for confounders? | 0 | 0 | 0 | 1 | 0 | 0 |
| Q26: Loss of follow-up reported? | 0 | 0 | 0 | 0 | 0 | 0 |
| Q27: Power calculation | 5 | 0 | 5 | 0 | 0 | 0 |
| Score | 6 | 1 | 6 | 2 | 1 | 1 |
| Total score | 19 | 13 | 19 | 15 | 15 | 14 |
| Variables | Details |
|---|---|
| SNA | The relation between the maxilla and the cranial base. Angle: Sella-Nasion-Point A |
| SNB | The relation between the mandible and the cranial base. Angle: Sella-nasion-Point B |
| ANB | Relation between the maxilla and the mandible. Angle: Point A-Nasion-Point B |
| Wits appraisal | The sagittal disparity in the occlusal plane between Maxilla and Mandible. Distance between projections from points A and B, drawn perpendicular to the Occlusal plane (O) |
| L1-MDP | The angle between the mandibular plane and the axis of the lower incisor. The angle between the lower incisor axes and mandibular plane |
| IIA | The posterior angle between the upper and lower incisor axes |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alam, M.K.; Nowrin, S.A.; Shahid, F.; AlHarby, H.; Abutayyem, H.; Alswairki, H.J.; El-Din Mohamed, S.K. Orthognathic versus Camouflage Treatment of Class III Malocclusion: A Systematic Review and Meta-Analysis. Appl. Sci. 2022, 12, 3314. https://doi.org/10.3390/app12073314
Alam MK, Nowrin SA, Shahid F, AlHarby H, Abutayyem H, Alswairki HJ, El-Din Mohamed SK. Orthognathic versus Camouflage Treatment of Class III Malocclusion: A Systematic Review and Meta-Analysis. Applied Sciences. 2022; 12(7):3314. https://doi.org/10.3390/app12073314
Chicago/Turabian StyleAlam, Mohammad Khursheed, Shifat A Nowrin, Fazal Shahid, Hassan AlHarby, Huda Abutayyem, Haytham Jamil Alswairki, and Sally Kamal El-Din Mohamed. 2022. "Orthognathic versus Camouflage Treatment of Class III Malocclusion: A Systematic Review and Meta-Analysis" Applied Sciences 12, no. 7: 3314. https://doi.org/10.3390/app12073314







