Fast-Track-Protocol for Optimization of Presurgical Planning in Acute Surgical Treatment of Acetabular Quadrilateral Plate Fractures Using 3D Printing Technology and Pre-Contoured Reconstruction Plates
Abstract
:1. Introduction
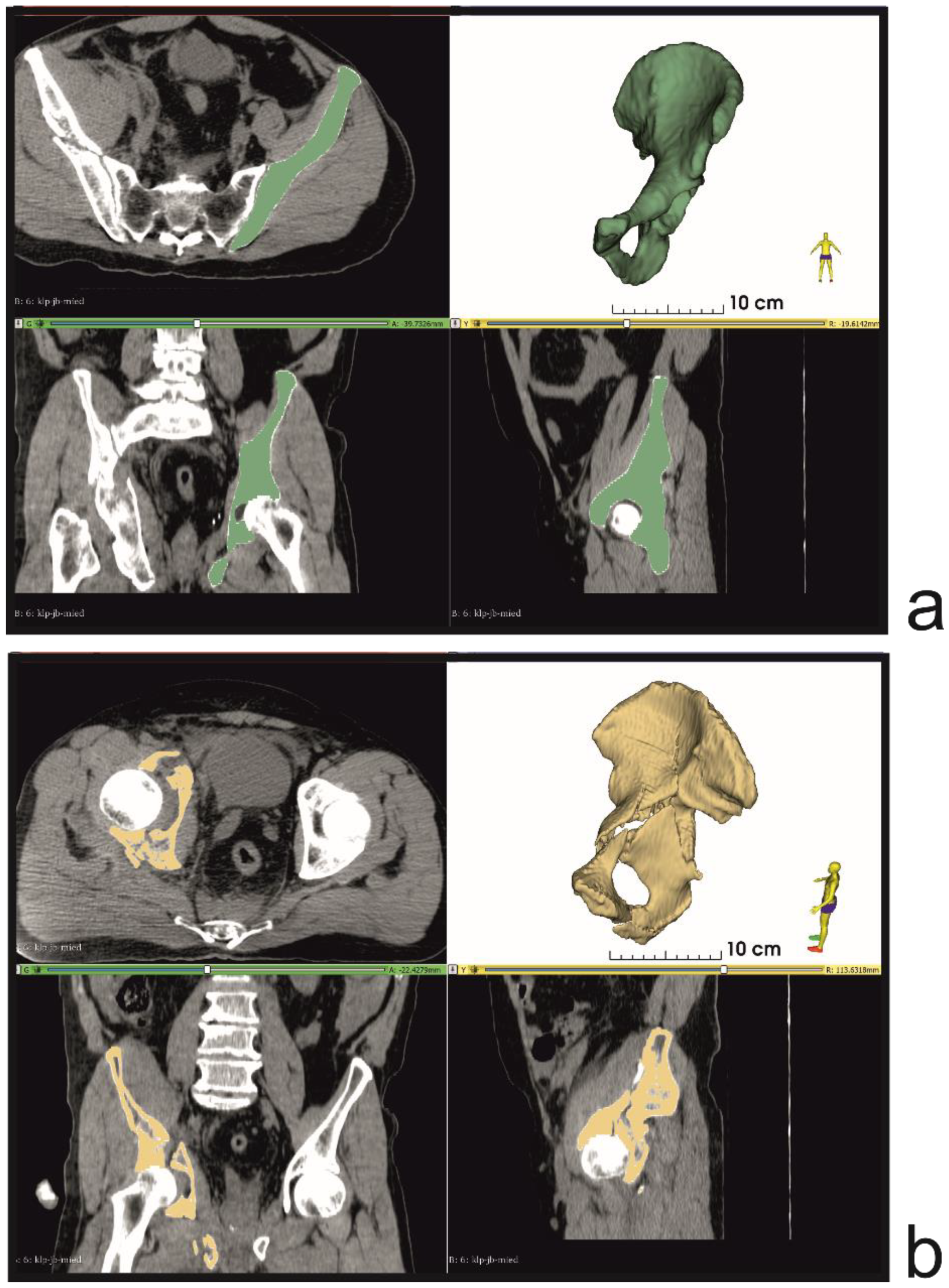
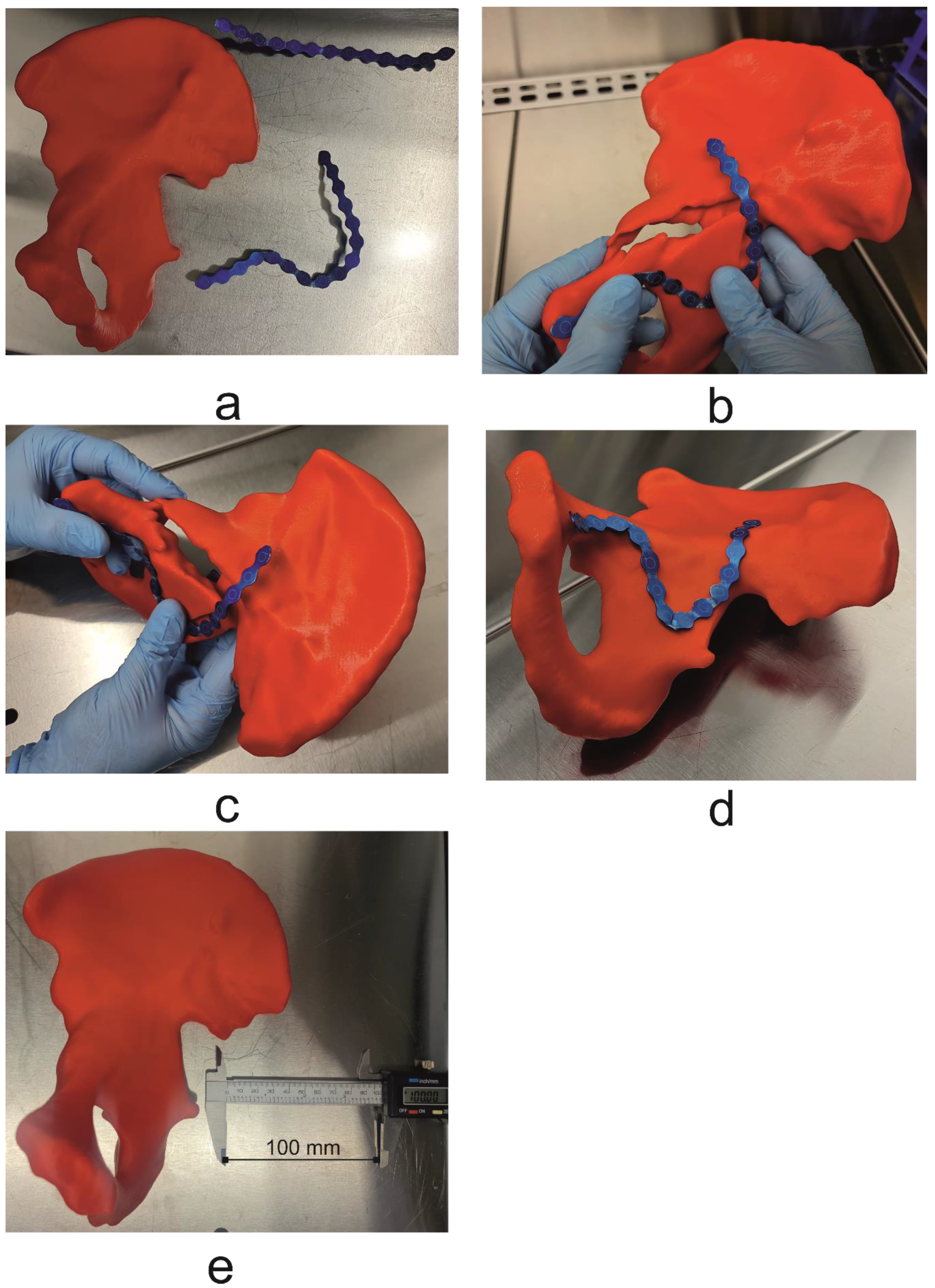
2. Materials and Methods
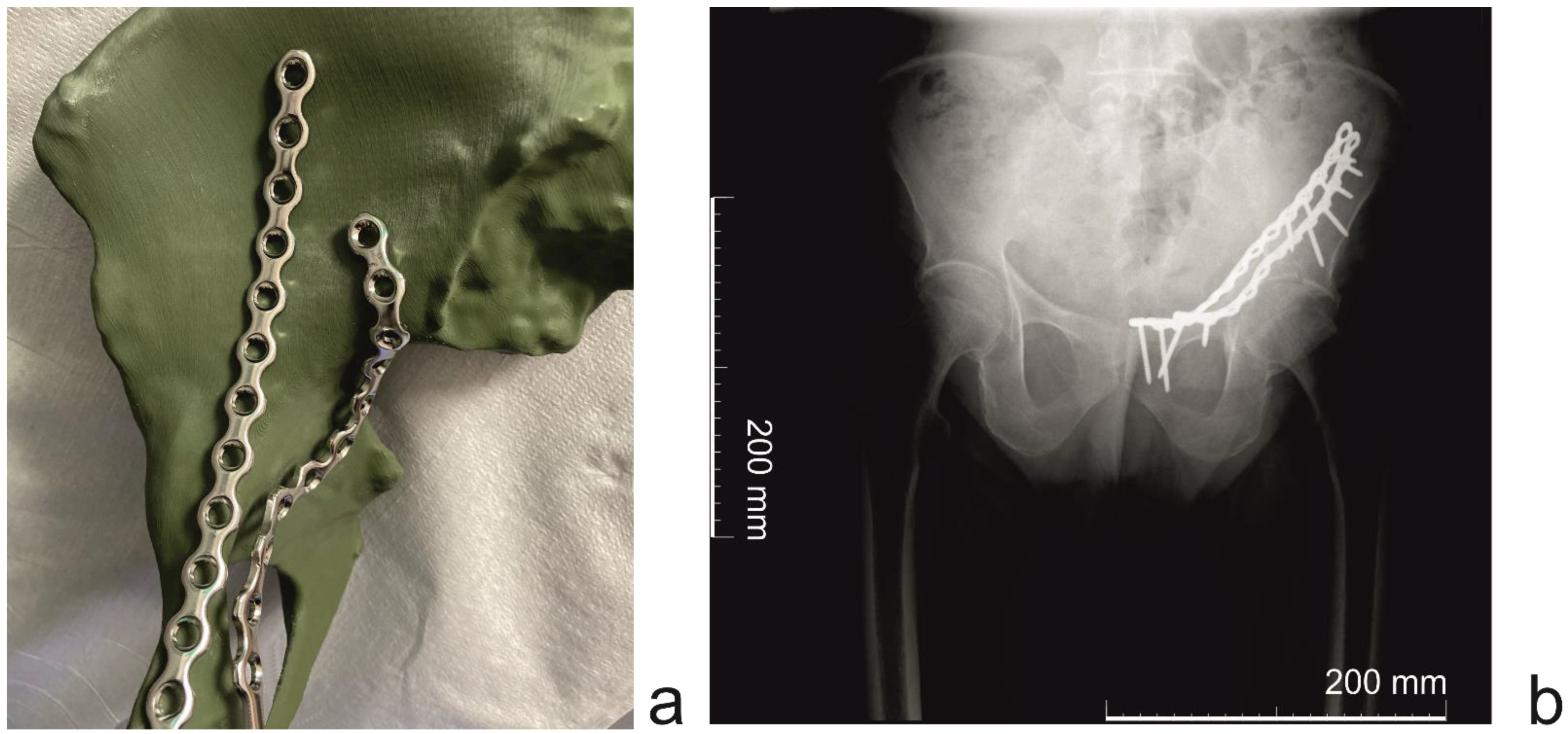
3. Results
- Day 1:
- ○
- Patient CT study
- ○
- Segmentation and virtual planning;
- ○
- 3D printing;
- Day 2:
- ○
- Support material removal;
- ○
- Surgical plate pre-contouring;
- ○
- Sterilization of pre-contoured plates;
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Rodríguez, F.C.; Mañanes, R.P.; Cárceles, F.N.; Gil Martínez, P. 3D printing utility for surgical treatment of acetabular fractures. Rev. Esp. Cir. Ortop. Traumatol. (Engl. Ed.) 2018, 62, 231–239. [Google Scholar] [CrossRef]
- Khorasani, M.; Ghasemi, A.; Rolfe, B.; Gibson, I. Additive manufacturing a powerful tool for the aerospace industry. Rapid Prototyp. J. 2022, 28, 87–100. [Google Scholar] [CrossRef]
- Hu, Y.; Li, H.; Qiao, G.; Liu, H.; Ji, A.; Ye, F. Computer-assisted virtual surgical procedure for acetabular fractures based on real CT data. Injury 2011, 42, 1121–1124. [Google Scholar] [CrossRef] [PubMed]
- Merema, B.J.; Kraeima, J.; ten Duis, K.; Wendt, K.W.; Warta, R.; Vos, E.; Schepers, R.H.; Witjes, M.J.H.; Ijpma, F.F.A. The design, production and clinical application of 3D patient-specific implants with drilling guides for acetabular surgery. Injury 2017, 48, 2540–2547. [Google Scholar] [CrossRef]
- Boudissa, M.; Oliveri, H.; Chabanas, M.; Tonetti, J. Computer-assisted surgery in acetabular fractures: Virtual reduction of acetabular fracture using the first patient-specific biomechanical model simulator. Orthop. Traumatol. Surg. Res. 2018, 104, 359–362. [Google Scholar] [CrossRef]
- Tostain, O.; Debuyzer, E.; Benad, K.; Putman, S.; Pierache, A.; Girard, J.; Pasquier, G. Ten-year outcomes of cementless anatomical femoral implants after 3D computed tomography planning. Follow-up note. Orthop. Traumatol. Surg. Res. 2019, 105, 937–942. [Google Scholar] [CrossRef]
- IMDRP Management Committee. IMDRF Strategic Plan 2021–2025; International Medical Device Regulators Forum, 25 September 2020. Available online: https://www.hsa.gov.sg/medical-devices/international-collaboration-medical-devices/imdrf (accessed on 16 January 2022).
- Rashed, K.; Kafi, A.; Simons, R.; Bateman, S. Fused filament fabrication of nylon 6/66 copolymer: Parametric study comparing full factorial and Taguchi design of experiments. Rapid Prototyp. J. 2022. ahead-of-print. [Google Scholar] [CrossRef]
- Nahar, C.; Gurrala, P.K. Transient thermal finite-element analysis of fused filament fabrication process. Rapid Prototyp. J. 2022. ahead-of-print. [Google Scholar] [CrossRef]
- Herzog, T.; Schnell, G.; Tille, C.; Seitz, H. Investigation of suitable material and adhesion promoter combinations for fused filament fabrication on flexible silicone build plates. Rapid Prototyp. J. 2022. ahead-of-print. [Google Scholar] [CrossRef]
- Chand, R.; Sharma, V.S.; Trehan, R.; Gupta, M.K. A physical investigation of dimensional and mechanical characteristics of 3D printed nut and bolt for industrial applications. Rapid Prototyp. J. 2022. ahead-of-print. [Google Scholar] [CrossRef]
- Mishra, P.K.; Ponnusamy, S.; Nallamilli, M.S.R. The influence of process parameters on the impact resistance of 3D printed PLA specimens under water-absorption and heat-treated conditions. Rapid Prototyp. J. 2021, 27, 1108–1123. [Google Scholar] [CrossRef]
- Durastanti, G.; Belvedere, C.; Ruggeri, M.; Donati, D.M.; Spazzoli, B.; Leardini, A. A Pelvic Reconstruction Procedure for Custom-Made Prosthesis Design of Bone Tumor Surgical Treatments. Appl. Sci. 2022, 12, 1654. [Google Scholar] [CrossRef]
- Chana-Rodríguez, F.; Mañanes, R.P.; Rojo-Manaute, J.; Gil, P.; Martínez-Gómiz, J.M.; Vaquero-Martín, J. 3D surgical printing and pre contoured plates for acetabular fractures. Injury 2016, 47, 2507–2511. [Google Scholar] [CrossRef] [PubMed]
- Zeng, C.; Xing, W.; Wu, Z.; Huang, H.; Huang, W. A combination of three-dimensional printing and computer-assisted virtual surgical procedure for preoperative planning of acetabular fracture reduction. Injury 2016, 47, 2223–2227. [Google Scholar] [CrossRef]
- Wang, H.; Wang, F.; Newman, S.; Lin, Y.; Chen, X.; Xu, L.; Wang, Q. Application of an innovative computerized virtual planning system in acetabular fracture surgery: A feasibility study. Injury 2016, 47, 1698–1701. [Google Scholar] [CrossRef]
- Citak, M.; Gardner, M.J.; Kendoff, D.; Tarte, S.; Krettek, C.; Nolte, L.-P.; Hüfner, T. Virtual 3D planning of acetabular fracture reduction. J. Orthop. Res. 2008, 26, 547–552. [Google Scholar] [CrossRef]
- Oberkircher, L.; Ruchholtz, S.; Rommens, P.M.; Hofmann, A.; Bücking, B.; Krüger, A. Osteoporotic Pelvic Fractures. Dtsch. Ärztebl. Int. 2018, 115, 70–80. [Google Scholar] [CrossRef] [Green Version]
- Marinescu, R.; Popescu, D.; Laptoiu, D. A Review on 3D-Printed Templates for Precontouring Fixation Plates in Orthopedic Surgery. J. Clin. Med. 2020, 9, 2908. [Google Scholar] [CrossRef]
- Fedorov, A.; Beichel, R.; Kalpathy-Cramer, J.; Finet, J.; Fillion-Robin, J.-C.; Pujol, S.; Bauer, C.; Jennings, D.; Fennessy, F.; Sonka, M.; et al. 3D Slicer as an image computing platform for the Quantitative Imaging Network. Magn. Reson. Imaging 2012, 30, 1323–1341. [Google Scholar] [CrossRef] [Green Version]
- Sánchez-Pérez, C.; Rodríguez-Lozano, G.; Rojo-Manaute, J.; Vaquero-Martín, J.; Chana-Rodríguez, F. 3D surgical printing for preoperative planning of trabecular augments in acetabular fracture sequel. Injury 2018, 49, S36–S43. [Google Scholar] [CrossRef]
- Li, L.; Gao, J. Comparison of three-dimensional printing and conventional imaging in surgical treatment of Tile C pelvic fractures: A long-term follow-up study. Int. J. Clin. Exp. Med. 2017, 10, 12433–12439. [Google Scholar]
- Ead, M.S.; Duke, K.K.; Jaremko, J.L.; Westover, L. Investigation of pelvic symmetry using CAD software. Med Biol. Eng. Comput. 2019, 58, 75–82. [Google Scholar] [CrossRef] [PubMed]
- Chen, K.; Yang, F.; Yao, S.; Xiong, Z.; Sun, T.; Zhu, F.; Telemacque, D.; Drepaul, D.; Ren, Z.; Guo, X. Application of computer-assisted virtual surgical procedures and three-dimensional printing of patient-specific pre-contoured plates in bicolumnar acetabular fracture fixation. Orthop. Traumatol. Surg. Res. 2019, 105, 877–884. [Google Scholar] [CrossRef] [PubMed]
- Pierannunzii, L.; Fischer, F.; Tagliabue, L.; Calori, G.M.; D’Imporzano, M. Acetabular both-column fractures: Essentials of operative management. Injury 2010, 41, 1145–1149. [Google Scholar] [CrossRef]
- Chen, X.; Chen, X.; Zhang, G.; Lin, H.; Yu, Z.; Wu, C.; Li, X.; Lin, Y.; Huang, W. Accurate fixation of plates and screws for the treatment of acetabular fractures using 3D-printed guiding templates: An experimental study. Injury 2017, 48, 1147–1154. [Google Scholar] [CrossRef]
- Damon, A.; Clifton, W.; Valero-Moreno, F.; Quinones-Hinojosa, A. Cost-Effective Method for 3-Dimensional Printing Dynamic Multiobject and Patient-Specific Brain Tumor Models: Technical Note. World Neurosurg. 2020, 140, 173–179. [Google Scholar] [CrossRef]
- Virzì, A.; Muller, C.O.; Marret, J.-B.; Mille, E.; Berteloot, L.; Grévent, D.; Boddaert, N.; Gori, P.; Sarnacki, S.; Bloch, I. Comprehensive Review of 3D Segmentation Software Tools for MRI usable for pelvic surgery planning. J. Digit. Imaging 2020, 33, 99–110. [Google Scholar] [CrossRef]
- Czeibert, K.; Sommese, A.; Petneházy, Ö.; Csörgő, T.; Kubinyi, E. Digital endocasting in comparatirve canine brain morphology. Front. Vet. Sci. 2020, 7, 749. [Google Scholar] [CrossRef]
- Kikinis, R.; Pieper, S. 3D Slicer as a tool for interactive brain tumor segmentation. In Proceedings of the 2011 Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Boston, MA, USA, 30 August–3 September 2011; pp. 6982–6984. [Google Scholar] [CrossRef] [Green Version]
- Bianchi, J.; Paniagua, B.; Oliveira Ruellas, A.C.; Fillion-Robin, J.C.; Prietro, J.C.; Gonçalves, J.R.; Hoctor, J.; Yatabe, M.; Styner, M.; Li, T.; et al. 3D Slicer craniomaxillofacial moduler support patient-specific decision-making for personalized healthcare in dental research. In Multimodal Learning for Clinical Decision Support and Clinical Image-Based Procedures; Springer: Cham, Switzerland, 2020; pp. 44–53. [Google Scholar] [CrossRef]
- Shetty, H.; Shetty, S.; Kakade, A.; Shetty, A.; Karobari, M.I.; Pawar, A.M.; Marya, A.; Heboyan, A.; Venugopal, A.; Nguyen, T.H.; et al. Three-dimensional semi-automated volumetric assessment of the pulp space of teeth following regenerative dental procedures. Sci. Rep. 2021, 11, 21914. [Google Scholar] [CrossRef]
- Velazquez, E.R.; Parmar, C.; Jermoumi, M.; Mak, R.H.; Van Baardwijk, A.; Fennessy, F.M.; Lewis, J.H.; De Ruysscher, D.; Kikinis, R.; Lambin, P.; et al. Volumetric CT-based segmentation of NSCLC using 3D-Slicer. Sci. Rep. 2013, 3, 3529. [Google Scholar] [CrossRef] [Green Version]
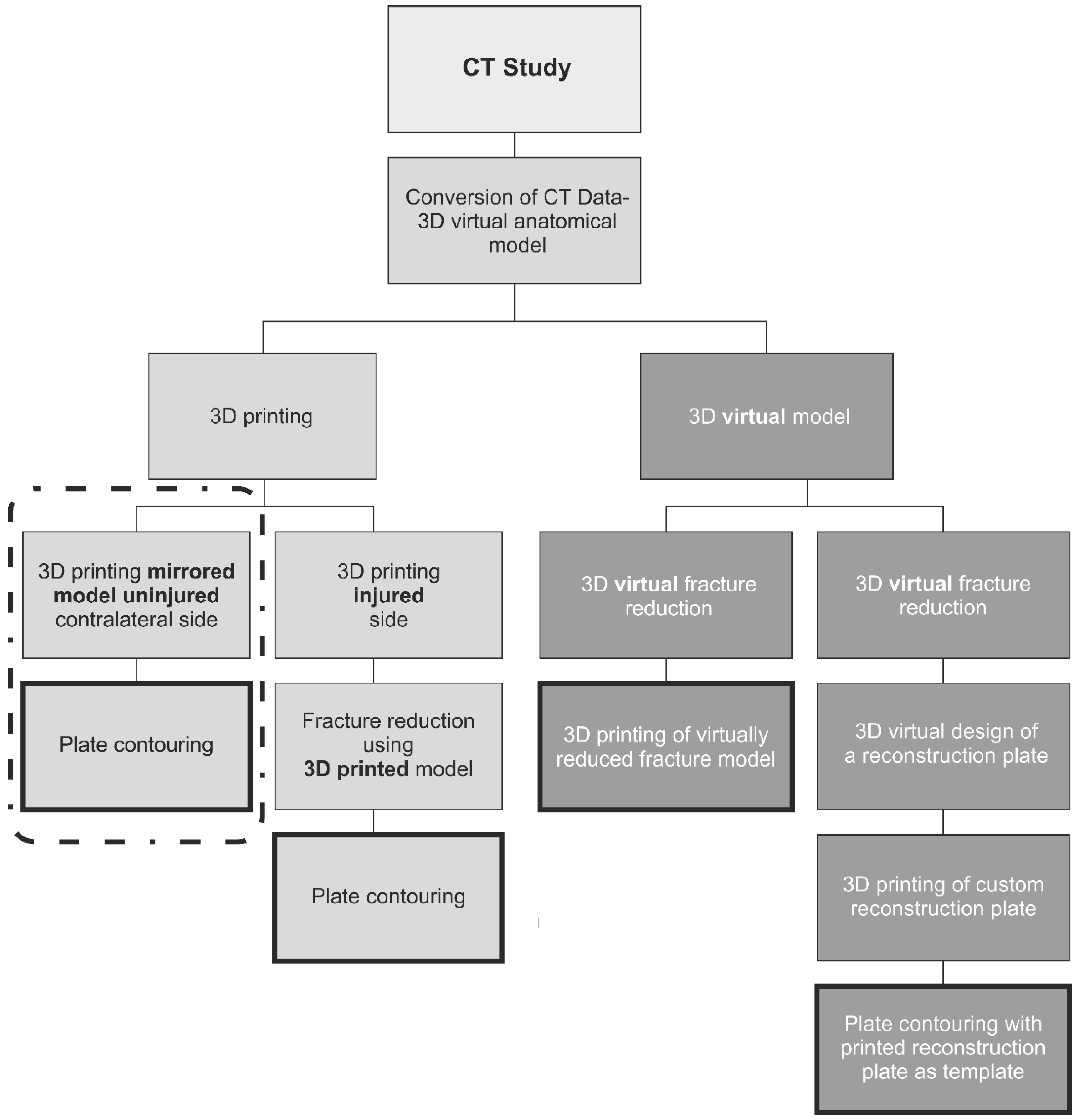

| 3D Printed Model | 3D Virtual Fracture Reduction |
|---|---|
| 3D printed mirrored (rotated 180 degrees) hemipelvis of the uninjured side, resulting in a model that represents pre-morbid anatomy of the injured side, assuming body symmetry. Model is then used to shape surgical plates. 3D printed model of the injured side, which is manually reduced and next used to contour surgical plates | 3D printed model of the injured side with virtually reduced fracture, which is used to shape surgical plates. 3D virtual design of a reconstruction plate, designed to fit the shape of the virtually reconstructed fracture. The plate is then 3D printed and used as a template |
| Computed Tomography Scanning Protocol | |
|---|---|
| NECT | Non-contrast Enhanced Computed Tomography |
| Region | Pelvis |
| Image reconstruction | Reconstruction algorithms (Kernels): Used in the study GE: Standard, Bone, Bone Plus; Siemens: B30f, B30s, B60s, B70s; Recommended for other CT scanners Philips: Standard, Sharp, Detail (B, C, D, E, L); Toshiba: FC08, FC18, FC30, Fc35; |
| Slice Thickness | ≤1.0 mm (isometric voxel) |
| Resolution | 512 × 512 |
| Pitch | ≤1.0 |
| Gantry Tilt Angle | 0 |
| Data Format | Uncompressed DICOM files |
| 3D Printing Parameters | |
|---|---|
| Printing temperature | 205 °C |
| Build plate temperature | 60 °C |
| Layer high | 0.2 mm |
| Infill | 60% |
| Support material | Polyvinyl alcohol (PVA) (Ultimaker B.V, Utrecht, The Netherlands) |
| Activity | Patient 1 | Patient 2 | Patient 3 | Patient 4 | Patient 5 | Mean | Sd |
|---|---|---|---|---|---|---|---|
| CT scan | 25 min | 25 min | 30 min | 35 min | 30 min | 30 min | 5 |
| Segmentation | 180 min | 170 min | 185 min | 195 min | 170 min | 180 min | 11 |
| 3D printing | 600 min | 540 min | 660 min | 660 min | 540 min | 600 min | 60 |
| Removal of support materials | 190 min | 170 min | 190 min | 180 min | 170 min | 180 min | 10 |
| Pre-contouring of plates | 35 min | 25 min | 35 min | 30 min | 25 min | 30 min | 5 |
| Cleaning and sterilization | 120 min | 120 min | 120 min | 120 min | 120 min | 120 min | 0 |
| Total time of preparing of the model | 1150 min (19.16 h) | 1050 min (17.5 h) | 1220 min (20.33 h) | 1220 min (20.33 h) | 1060 min (17.66 h) | 1140 min (19.0 h) | 83 min (1.38 h) |
| Fast Track Protocol | |
|---|---|
| Advantages | Disadvantages |
| A Do-It-Yourself approach that greatly reduces any potential costs and makes it possible for a multidisciplinary team to create 3D printed models, which can be used to shape and form custom implants Free open-source software for converting CT data and creating 3D anatomical models, with an active community of users and numerous freely available guides and tutorials CT study protocol that can be implemented on any modern multidetector scanner. 3D model production using budget desktop 3D printers using relatively low-cost materials | The necessity to learn and implement the entire process of converting CT data, 3D printing, and model preparation Software is relatively easy to learn. However, some users may find it difficult to grasp, particularly in the early stages, if no prior experience of segmenting CT data. Cost of purchasing a dual extruder 3D printer that has an adequate level of precision and accuracy Budget 3D printers can be fickle and usually require regular maintenance |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Andrzejewski, K.; Elgalal, M.; Komorowski, P.; Poszepczyński, J.; Rokita, B.; Domżalski, M. Fast-Track-Protocol for Optimization of Presurgical Planning in Acute Surgical Treatment of Acetabular Quadrilateral Plate Fractures Using 3D Printing Technology and Pre-Contoured Reconstruction Plates. Appl. Sci. 2022, 12, 3492. https://doi.org/10.3390/app12073492
Andrzejewski K, Elgalal M, Komorowski P, Poszepczyński J, Rokita B, Domżalski M. Fast-Track-Protocol for Optimization of Presurgical Planning in Acute Surgical Treatment of Acetabular Quadrilateral Plate Fractures Using 3D Printing Technology and Pre-Contoured Reconstruction Plates. Applied Sciences. 2022; 12(7):3492. https://doi.org/10.3390/app12073492
Chicago/Turabian StyleAndrzejewski, Krzysztof, Marcin Elgalal, Piotr Komorowski, Jan Poszepczyński, Bożena Rokita, and Marcin Domżalski. 2022. "Fast-Track-Protocol for Optimization of Presurgical Planning in Acute Surgical Treatment of Acetabular Quadrilateral Plate Fractures Using 3D Printing Technology and Pre-Contoured Reconstruction Plates" Applied Sciences 12, no. 7: 3492. https://doi.org/10.3390/app12073492
APA StyleAndrzejewski, K., Elgalal, M., Komorowski, P., Poszepczyński, J., Rokita, B., & Domżalski, M. (2022). Fast-Track-Protocol for Optimization of Presurgical Planning in Acute Surgical Treatment of Acetabular Quadrilateral Plate Fractures Using 3D Printing Technology and Pre-Contoured Reconstruction Plates. Applied Sciences, 12(7), 3492. https://doi.org/10.3390/app12073492






