Let AI Perform Better Next Time—A Systematic Review of Medical Imaging-Based Automated Diagnosis of COVID-19: 2020–2022
Abstract
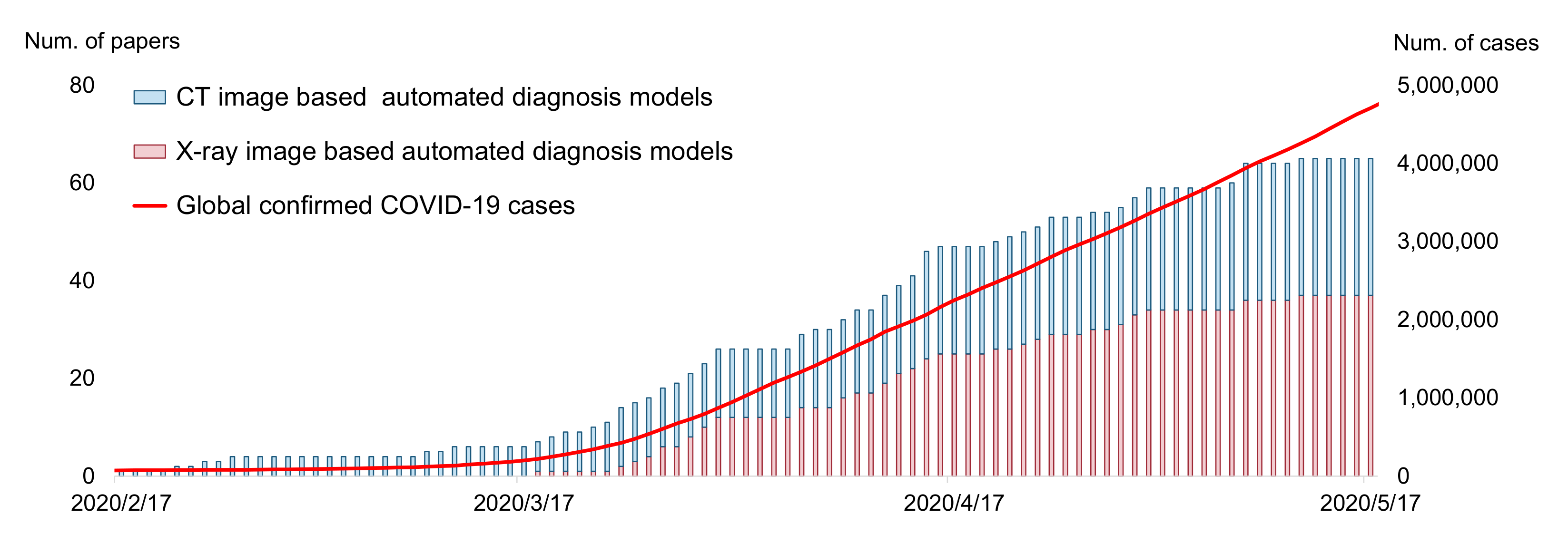
:1. Introduction
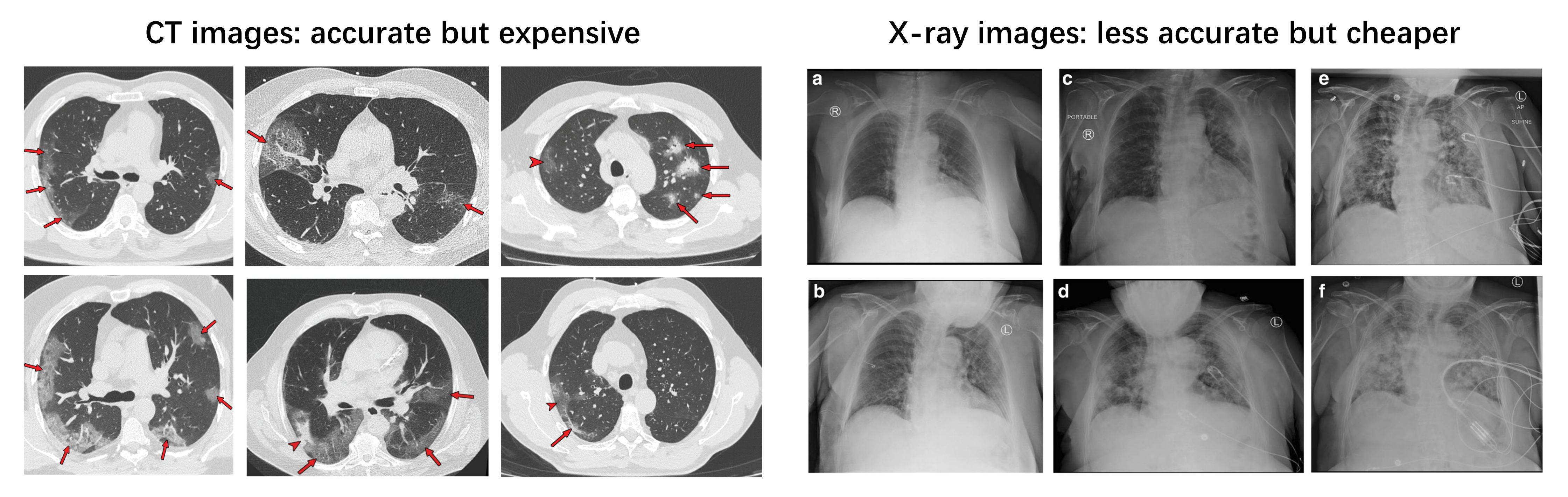
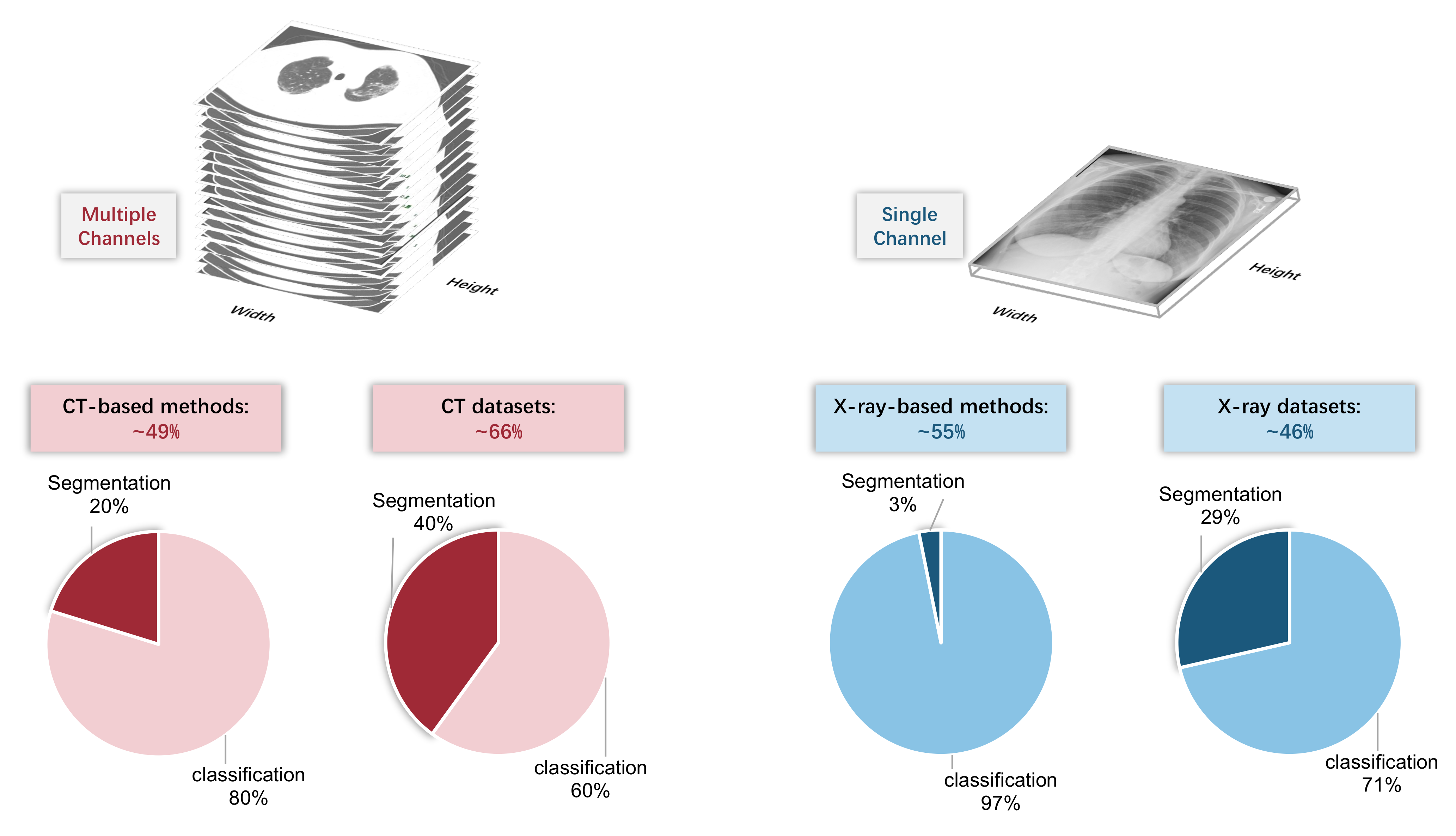
2. Input Modalities: CT or X-ray
2.1. Clinical Perspective
2.2. Artificial Intelligence Perspective
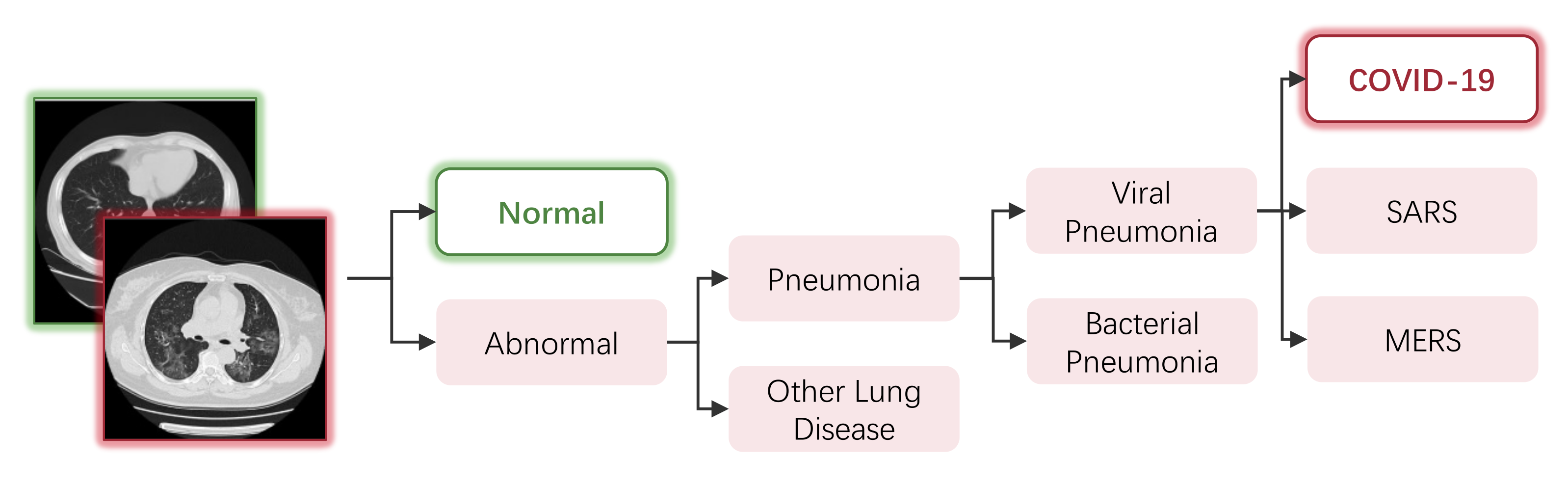
3. Automated Diagnosis of COVID-19
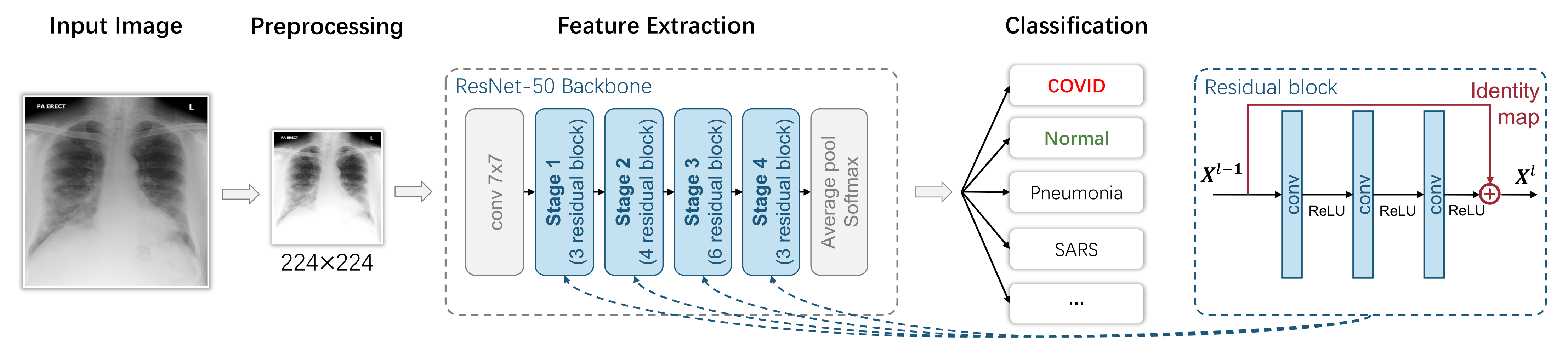
3.1. Image-Level Diagnosis: Classification-Based Models
3.1.1. Overview
3.1.2. Preprocessing
3.1.3. Feature Extraction
3.1.4. Classification
3.1.5. Evaluation
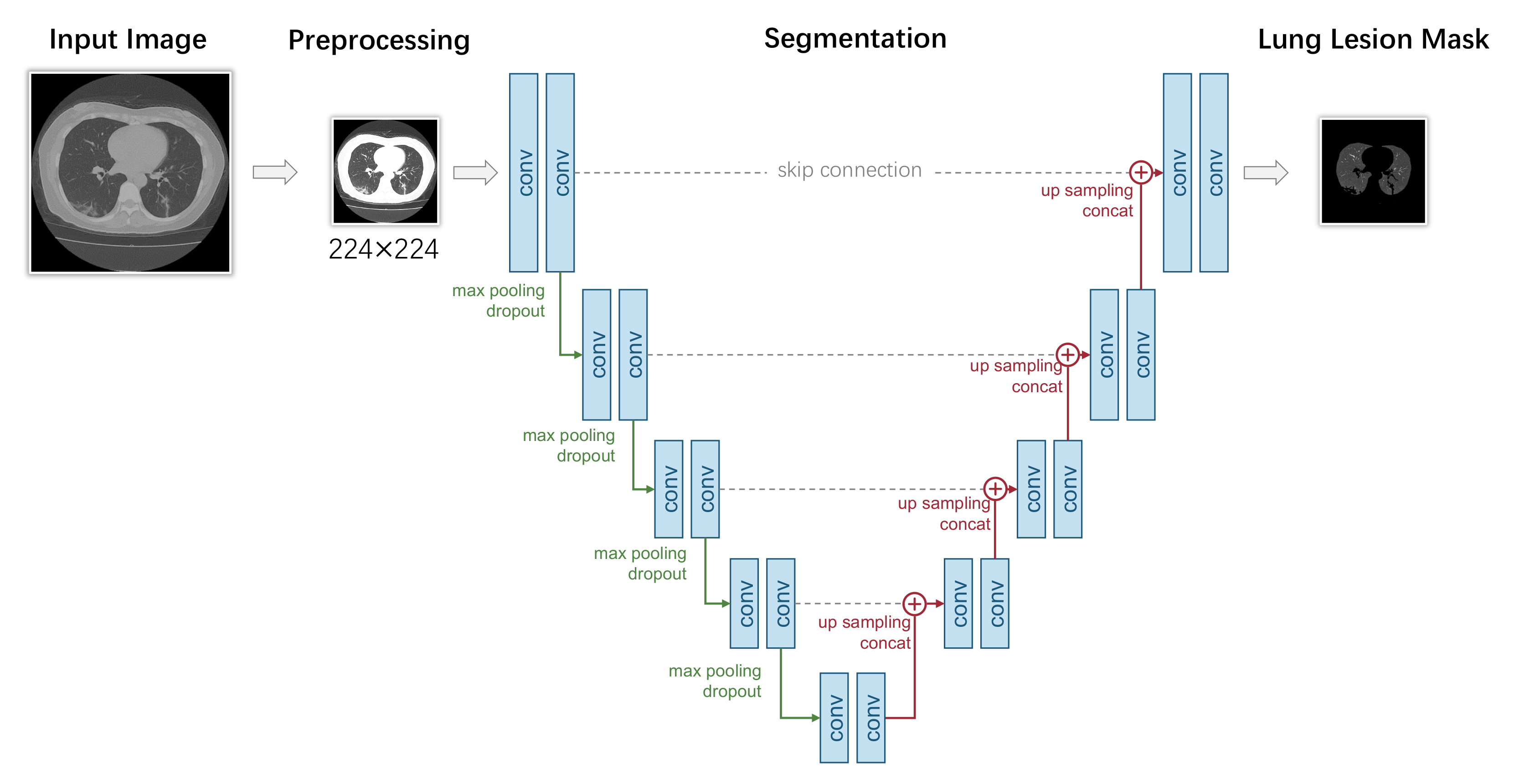
3.2. Pixel-Level Diagnosis: Segmentation-Based Models
3.2.1. Overview
3.2.2. Preprocessing
3.2.3. Segmentation
3.2.4. Evaluation
4. Datasets
4.1. Classification Datasets
- SARS-CoV-2 CT-scan Dataset [201]. These data have been collected from real patients in hospitals from Sao Paulo, Brazil. The aim of this dataset is to encourage the research and development of artificial intelligent methods that are able to identify if a person is infected by SARS-CoV-2 through the analysis of his/her CT scans. There are 2482 images in total, including gender information;
- COVID-CT-Dataset [202]. The COVID-CT-Dataset is a radiologist-confirmed CT image dataset. The images are collected from 760 COVID-19-related preprint PDFs in medRxiv and bioRxiv. The labels are decided according to the associated figure captions, while other information, such as age and gender, are also extracted;
- COVID-CT Dataset [63]. This dataset contains the full original CT scans of 377 persons, including other information, such as age and sex. It was gathered from Negin radiology located in Sari, Iran, between 5 March and 23 April 2020. There are 15,589 and 48,260 CT scan images belonging to 95 COVID-19 and 282 normal persons, respectively. The format of the exported radiology images was a 16-bit grayscale DICOM format with a 512 × 512 pixels resolution;
- CT Scans for COVID-19 Classification [203]. Data were collected from two hospitals: Union Hospital (HUST-UH) and Liyuan hospital (HUST-LH). There are a total of 39,370 CT images, and they are in a JPG format with a resolution of 512 × 512;
- Large COVID-19 CT Scan Slice Dataset [204]. The CT images in this dataset are collected from seven public datasets, which include COVID-CT-Dataset, COVID-CT-MD, Covid-Chestxray-Dataset, MosMedData, COVID-19 CT Lung and Infection Segmentation Dataset, COVID-CTset and COVID-19 CT Segmentation Dataset. There are 17,104 images in total, and all of the CAP images are from the dataset of Afshar et al., in which, 25 cases were previously annotated and their radiologist annotated the remaining 35 volumes. The images are in PNG format with a resolution of 512 × 512. The dataset also contains information such as gender, age and country;
- COVIDx Dataset [155]. The COVIDx Dataset is a combined dataset. The X-ray images in the COVIDx Dataset are collected from more than five different data repositories, which include COVID-19 Image Data Collection, COVID-19 Chest X-ray Dataset Initiative, ActualMed COVID-19 Chest X-ray Dataset Initiative, RSNA Pneumonia Detection Challenge dataset and COVID-19 radiography database; therefore, there are 30,882 images in the dataset. However, the COVIDx Dataset is also a highly imbalanced dataset: the positive samples account for only less than 3% of all samples;
- COVID-19 Radiography Database [43]. The COVID-19 Radiography Database is the winner of the COVID-19 Dataset Award of Kaggle. A team of researchers from Qatar University, Doha, Qatar, and the University of Dhaka, Bangladesh, along with their collaborators from Pakistan and Malaysia in collaboration with medical doctors, has created this dataset. The images are mainly collected from the Italian Society of Medical and Interventional Radiology (SIRM) COVID-19 DATABASE and other databases and publications. All of the images are X-ray images, and in PNG format with a resolution of 299 × 299;
- COVID-19 Detection X-ray Dataset [205]. The 5073 X-ray images are collected from Github user ieee8023 for COVID-19 X-rays and Paul Mooney for Pneumonia Dataset. All images are in JPEG format;
- Augmented COVID-19 X-ray Images Dataset [206]. The Augmented COVID-19 X-ray Images Dataset is modified from two datasets, including Covid-Chestxray-Dataset and Chest-Xray-Pneumonia. There are a total of 3532 X-ray images in PNG format. The images are augmented by basic augmentation methods, such as rotating, flipping, scaling and cropping;
- Covid-Chestxray-Dataset [207]. Data were largely compiled from public databases on websites such as Radiopaedia.org, the Italian Society of Medical and Interventional Radiology2 and the Hannover Medical School. Both X-ray and CT images are involved in the COVID-19 X-ray Images Dataset, where 930 images in total are in JPG format. However, 43 of 45 CT images are COVID-19-positive. The imbalance makes it unsuitable to be used alone. This dataset not only consists of the lung bounding box, but is also annotated with other information, such as sex, age, location, survival, etc.
4.2. Segmentation Datasets
- COVID-19 CT Lung and Infection Segmentation Dataset [208]. The CT images in this dataset are collected from five public datasets, which include StructSeg 2019, NSCLC, MSD Lung Tumor, COVID-19-CT-Seg and MosMed. This dataset contains 20 labeled COVID-19 CT scans. Left lung, right lung and infections are labeled by two radiologists and verified by an experienced radiologist;
- COVID-19 CT Segmentation Dataset [209]. 110 axial CT images from 60 patients with COVID-19 are in this dataset, which is segmented by a radiologist. Three types of objects, including ground-glass, consolidation and pleural effusion, are annotated. Ground-glass opacities are in blue, consolidation is in yellow and pleural effusion is in green. The images are in JPG format, while other information, such as age and sex, are also extracted. This dataset is suitable for the training of both the classification model and detection model;
- MOSMEDDATA [210]. A total of 1110 CT images were provided by municipal hospitals in Moscow, Russia. A small subset of studies (n = 50) has been annotated by the experts of the Research and Practical Clinical Center for Diagnostics and Telemedicine Technologies of the Moscow Health Care Department. During the annotation, for every given image, ground-glass opacifications and regions of consolidation were selected as positive (white) pixels on the corresponding binary pixel mask. This dataset also includes other information, such as age and gender;
- COVIDGR Dataset [211]. COVIDGR Dataset is a balanced X-ray dataset that covered all levels of severity of illness, from normal with positive RT-PCR, mild and moderate to severe. Data were collected from an expert radiologist team of the Hospital Universitario San Cecilio, and there are 852 X-ray images in total;
- BIMCV COVID-19+ [212]. BIMCV COVID-19+ is a 389.27 GB annotated dataset that consists of both X-ray and CT images. Data were collected from public sources, including COVID-CT-Dataset, COVID-19 dataset and COVID-19 RADIOGRAPHY DATABASE. Data were also collected from some private datasets. There are 23,527 images in total, 23 of which were annotated by a team of expert radiologists. Two types of objects, including ground-glass and consolidation, are annotated. Ground-glass opacities are in green, and consolidation is in purple. Images are stored at a high resolution and entities are localized with anatomical labels in a Medical Imaging Data Structure (MIDS) format. The dataset also contains other information, such as sex, age, diagnostics, survival, etc.
5. Discussion
5.1. Biased Model Performance Evaluation
- Recommendation: Well-recognized institutions should establish benchmarks (using baseline models and a high-quality dataset and releasing reproducible codes) as soon as possible.
- Recommendation: The testing set should not be used for validation. In addition, the testing set should be sufficiently large; otherwise, it cannot give an accurate estimation of the model performance.
- Recommendation: When making a new dataset public, researchers should guarantee its quality and provide as much detailed information as possible.
5.2. Inappropriate Implementation Details
- Recommendation: When solving the problem of lacking training data with data augmentation, the ’safety’ of selected data augmentation techniques should be considered.
5.3. Low Reproducibility, Reliability and Explainability
- Recommendation: If possible, upload clean codes accompanying the posted papers. Prepare easy-to-follow documents that describe how to re-implement the proposed method.
- Recommendation: authors should provide sufficient technical details of their proposed methods in order to guarantee the reproducibility.
- Recommendation: Work as a multidisciplinary team. Opinions from domain experts are valuable for evaluating the correctness of AI models.
6. Conclusions
Funding
Conflicts of Interest
References
- Wang, S.; Kang, B.; Ma, J.; Zeng, X.; Xiao, M.; Guo, J.; Cai, M.; Yang, J.; Li, Y.; Meng, X.; et al. A deep learning algorithm using CT images to screen for Corona Virus Disease (COVID-19). Eur. Radiol. 2021, 31, 6096–6104. [Google Scholar] [CrossRef] [PubMed]
- Jemioło, P.; Storman, D.; Orzechowski, P. A Call For Better Methodological Quality Of Reviews On Using Artificial Intelligence For COVID-19 Detection In Medical Imaging—An Umbrella Systematic Review. medRxiv 2021. [Google Scholar] [CrossRef]
- Wynants, L.; van Calster, B.; Bonten, M.J.; Collins, G.S.; Debray, T.P.A.; de Vos, M.; Haller, M.C.; Heinze, G.; Moons, K.G.M.; Riley, R.D.; et al. Systematic review and critical appraisal of prediction models for diagnosis and prognosis of COVID-19 infection. medRxiv 2020. [Google Scholar] [CrossRef]
- Wynants, L.; van Calster, B.; Bonten, M.J.; Collins, G.S.; Debray, T.P.A.; de Vos, M.; Haller, M.C.; Heinze, G.; Moons, K.G.M.; Riley, R.D.; et al. Prediction models for diagnosis and prognosis of covid-19: Systematic review and critical appraisal. BMJ 2020, 369, m1328. [Google Scholar] [CrossRef] [Green Version]
- Moons, K.G.M.; Wolff, R.; Riley, R.D.; Whiting, P.F.; Westwood, M.E.; Collins, G.S.; Reitsma, J.B.; Kleijnen, J.; Mallett, S. PROBAST: A Tool to Assess Risk of Bias and Applicability of Prediction Model Studies: Explanation and Elaboration. Ann. Intern. Med. 2019, 170, W1–W33. [Google Scholar] [CrossRef] [Green Version]
- Summers, R.M. Artificial Intelligence of COVID-19 Imaging: A Hammer in Search of a Nail. Radiology 2020, 298, E162–E164. [Google Scholar] [CrossRef]
- Roberts, M.; Driggs, D.; Thorpe, M.; Gilbey, J.D.; Yeung, M.; Ursprung, S.; Avilés-Rivero, A.I.; Etmann, C.; McCague, C.; Beer, L.; et al. Common pitfalls and recommendations for using machine learning to detect and prognosticate for COVID-19 using chest radiographs and CT scans. Nat. Mach. Intell. 2021, 3, 199–217. [Google Scholar] [CrossRef]
- Born, J.; Beymer, D.J.; Rajan, D.; Coy, A.; Mukherjee, V.V.; Manica, M.; Prasanna, P.; Ballah, D.; Guindy, M.; Shaham, D.; et al. On the Role of Artificial Intelligence in Medical Imaging of COVID-19. medRxiv 2020, 2, 10029. [Google Scholar] [CrossRef]
- Driggs, D.; Selby, I.; Roberts, M.; Gkrania-Klotsas, E.; Rudd, J.H.F.; Yang, G.; Babar, J.L.; Sala, E.; Schönlieb, C.B. Machine Learning for COVID-19 Diagnosis and Prognostication: Lessons for Amplifying the Signal While Reducing the Noise. Radiol. Artif. Intell. 2021, 3, e210011. [Google Scholar] [CrossRef]
- Hryniewska, W.; Bombinski, P.; Szatkowski, P.; Tomaszewska, P.; Przelaskowski, A.; Biecek, P. Checklist for responsible deep learning modeling of medical images based on COVID-19 detection studies. Pattern Recognit. 2021, 118, 108035. [Google Scholar] [CrossRef]
- Cruz, B.G.S.; Bossa, M.N.; Sölter, J.; Husch, A.D. Public Covid-19 X-ray datasets and their impact on model bias—A systematic review of a significant problem. medRxiv 2021, 74, 102225. [Google Scholar] [CrossRef]
- Chen, D.; Ji, S.; Liu, F.; Li, Z.; Zhou, X. A Review of Automated Diagnosis of COVID-19 Based on Scanning Images. In Proceedings of the ICRAI 2020: 6th International Conference on Robotics and Artificial Intelligence, Singapore, 20–22 November 2020; pp. 97–104. [Google Scholar] [CrossRef]
- Bullock, J.; Luccioni, A.S.; Pham, K.H.; Lam, C.S.N.; Luengo-Oroz, M.A. Mapping the landscape of Artificial Intelligence applications against COVID-19. J. Artif. Intell. Res. 2020, 69, 807–845. [Google Scholar] [CrossRef]
- Nguyen, T.T. Artificial Intelligence in the Battle against Coronavirus (COVID-19): A Survey and Future Research Directions. arXiv 2020, arXiv:2008.07343. [Google Scholar]
- Ilyas, M.; Rehman, H.; Naït-Ali, A. Detection of Covid-19 From Chest X-ray Images Using Artificial Intelligence: An Early Review. arXiv 2020, arXiv:2004.05436. [Google Scholar]
- Dong, D.; Tang, Z.; Wang, S.; Hui, H.; Gong, L.; Lu, Y.; Xue, Z.; Liao, H.; Chen, F.; Yang, F.; et al. The Role of Imaging in the Detection and Management of COVID-19: A Review. IEEE Rev. Biomed. Eng. 2021, 14, 16–29. [Google Scholar] [CrossRef]
- Bhargava, A.; Bansal, A. Novel coronavirus (COVID-19) diagnosis using computer vision and artificial intelligence techniques: A review. Multim. Tools Appl. 2021, 80, 19931–19946. [Google Scholar] [CrossRef]
- Islam, M.N.; Inan, T.T.; Rafi, S.; Akter, S.S.; Sarker, I.H.; Islam, A.K.M.N. A Survey on the Use of AI and ML for Fighting the COVID-19 Pandemic. arXiv 2020, arXiv:2008.07449. [Google Scholar]
- McDermott, C.; Lacki, M.; Sainsbury, B.; Henry, J.; Filippov, M.; Rossa, C. Sonographic Diagnosis of COVID-19: A Review of Image Processing for Lung Ultrasound. Front. Big Data 2021, 4, 612561. [Google Scholar] [CrossRef]
- Sun, Y.; Li, C.; Zhang, Q.; Zhou, A.; Zhang, G. Survey of the Detection and Classification of Pulmonary Lesions via CT and X-ray. arXiv 2020, arXiv:2012.15442. [Google Scholar]
- Nabavi, S.; Ejmalian, A.; Moghaddam, M.E.; Abin, A.A.; Frangi, A.F.; Mohammadi, M.; Rad, H.S. Medical imaging and computational image analysis in COVID-19 diagnosis: A review. Comput. Biol. Med. 2021, 135, 104605. [Google Scholar] [CrossRef]
- Hariri, W.; Narin, A. Deep neural networks for COVID-19 detection and diagnosis using images and acoustic-based techniques: A recent review. Soft Comput. 2021, 25, 15345–15362. [Google Scholar] [CrossRef] [PubMed]
- Mondal, M.R.H.; Bharati, S.; Podder, P. Diagnosis of COVID-19 Using Machine Learning and Deep Learning: A review. arXiv 2021, arXiv:2110.14910. [Google Scholar] [CrossRef] [PubMed]
- Li, L.; Huang, T.; qing Wang, Y.; ping Wang, Z.; Liang, Y.; Huang, T.B.; Zhang, H.; Sun, W.; Wang, Y.P. COVID-19 patients’ clinical characteristics, discharge rate, and fatality rate of meta-analysis. J. Med. Virol. 2020, 92, 577–583. [Google Scholar] [CrossRef] [PubMed]
- Buitrago-Garcia, D.; Egli-Gany, D.; Counotte, M.J.; Hossmann, S.; Imeri, H.; Ipekci, A.M.; Salanti, G.; Low, N. Occurrence and transmission potential of asymptomatic and presymptomatic SARS-CoV-2 infections: A living systematic review and meta-analysis. PLoS Medicine 2020, 17, e1003346. [Google Scholar] [CrossRef]
- Byambasuren, O.; Cardona, M.; Bell, K.J.L.; Clark, J.; McLaws, M.L.; Glasziou, P.P. Estimating the extent of asymptomatic COVID-19 and its potential for community transmission: Systematic review and meta-analysis. Off. J. Assoc. Med. Microbiol. Infect. Dis. Can. 2020, 5, 223–234. [Google Scholar]
- Pollock, A.M.; Lancaster, J. Asymptomatic transmission of covid-19. BMJ 2020, 371, m4851. [Google Scholar] [CrossRef]
- Tahamtan, A.; Ardebili, A. Real-time RT-PCR in COVID-19 detection: Issues affecting the results. Expert Rev. Mol. Diagn. 2020, 20, 453–454. [Google Scholar] [CrossRef] [Green Version]
- Xie, X.; Zhong, Z.; Zhao, W.; Zheng, C.; Wang, F.; jing Liu, J. Chest CT for Typical 2019-nCoV Pneumonia: Relationship to Negative RT-PCR Testing. Radiology 2020, 296, 1315–1527. [Google Scholar] [CrossRef] [Green Version]
- Kwee, T.C.; Kwee, R.M. Chest CT in COVID-19: What the Radiologist Needs to Know. Radiographics 2020, 40, 1848–1865. [Google Scholar] [CrossRef]
- Fang, Y.; Zhang, H.; Xie, J.; Lin, M.; Ying, L.; Pang, P.; Ji, W.B. Sensitivity of Chest CT for COVID-19: Comparison to RT-PCR. Radiology 2020, 296, E115–E117. [Google Scholar] [CrossRef]
- Rousan, L.A.; Elobeid, E.; Karrar, M.; Khader, Y.S. Chest X-ray findings and temporal lung changes in patients with COVID-19 pneumonia. BMC Pulm. Med. 2020, 20, 245. [Google Scholar] [CrossRef] [PubMed]
- Cozzi, D.; Albanesi, M.; Cavigli, E.; Moroni, C.; Bindi, A.; Luvarà, S.; Lucarini, S.; Busoni, S.; Mazzoni, L.N.; Miele, V. Chest X-ray in new Coronavirus Disease 2019 (COVID-19) infection: Findings and correlation with clinical outcome. Radiol. Medica 2020, 125, 730–737. [Google Scholar] [CrossRef] [PubMed]
- Dhama, K.; Khan, S.; Tiwari, R.; Sircar, S.; Bhat, S.; Malik, Y.S.; Singh, K.P.; Chaicumpa, W.; Bonilla-Aldana, D.K.; Rodriguez-Morales, A.J. Coronavirus Disease 2019—COVID-19. Clin. Microbiol. Rev. 2020, 33, e00028-20. [Google Scholar] [CrossRef] [PubMed]
- Khatami, F.; Saatchi, M.; Zadeh, S.S.T.; Aghamir, Z.S.; Shabestari, A.N.; Reis, L.O.; Aghamir, S.M.K. A meta-analysis of accuracy and sensitivity of chest CT and RT-PCR in COVID-19 diagnosis. Sci. Rep. 2020, 10, 22402. [Google Scholar] [CrossRef]
- Borakati, A.; Perera, A.; Johnson, J.; Sood, T. Diagnostic accuracy of X-ray versus CT in COVID-19: A propensity-matched database study. BMJ Open 2020, 10, e042946. [Google Scholar] [CrossRef]
- He, K.; Zhang, X.; Ren, S.; Sun, J. Deep Residual Learning for Image Recognition. In Proceedings of the 2016 IEEE Conference on Computer Vision and Pattern Recognition (CVPR), Las Vegas, NV, USA, 27–30 June 2016; pp. 770–778. [Google Scholar]
- Ronneberger, O.; Fischer, P.; Brox, T. U-Net: Convolutional Networks for Biomedical Image Segmentation. In International Conference on Medical Image Computing and Computer-Assisted Intervention; Springer: Berlin/Heidelberg, Germany, 2015. [Google Scholar]
- Li, Z.; Liu, F.; Yang, W.; Peng, S.; Zhou, J. A Survey of Convolutional Neural Networks: Analysis, Applications, and Prospects. IEEE Trans. Neural Netw. Learn. Syst. 2021, 1–21. [Google Scholar] [CrossRef]
- Gozes, O.; Frid-Adar, M.; Greenspan, H.; Browning, P.D.; Zhang, H.; Ji, W.B.; Bernheim, A.; Siegel, E. Rapid AI Development Cycle for the Coronavirus (COVID-19) Pandemic: Initial Results for Automated Detection & Patient Monitoring using Deep Learning CT Image Analysis. arXiv 2020, arXiv:2003.05037. [Google Scholar]
- Zheng, C.; Deng, X.; Fu, Q.; feng Zhou, Q.; Feng, J.; Ma, H.; Liu, W.; Wang, X. Deep Learning-based Detection for COVID-19 from Chest CT using Weak Label. medRxiv 2020. [Google Scholar] [CrossRef] [Green Version]
- Jin, S.; Wang, B.; Xu, H.; Luo, C.; Wei, L.; Zhao, W.; Hou, X.; Ma, W.; Xu, Z.; Zheng, Z.; et al. AI-assisted CT imaging analysis for COVID-19 screening: Building and deploying a medical AI system in four weeks. medRxiv 2020. [Google Scholar] [CrossRef] [Green Version]
- Chowdhury, M.E.H.; Rahman, T.; Khandakar, A.; Mazhar, R.; Kadir, M.A.; Mahbub, Z.B.; Islam, K.R.; Khan, M.S.; Iqbal, A.; Al-Emadi, N.; et al. Can AI Help in Screening Viral and COVID-19 Pneumonia? IEEE Access 2020, 8, 132665–132676. [Google Scholar] [CrossRef]
- Afshar, P.; Heidarian, S.; Naderkhani, F.; Oikonomou, A.; Plataniotis, K.N.; Mohammadi, A. COVID-CAPS: A capsule network-based framework for identification of COVID-19 cases from X-ray images. Pattern Recognit. Lett. 2020, 138, 638–643. [Google Scholar] [CrossRef] [PubMed]
- Ozkaya, U.; Öztürk, S.; Barstugan, M. Coronavirus (COVID-19) Classification using Deep Features Fusion and Ranking Technique. arXiv 2020, arXiv:2004.03698. [Google Scholar]
- Ezzat, D.; Hassanien, A.E.; Ella, H.A. GSA-DenseNet121-COVID-19: A Hybrid Deep Learning Architecture for the Diagnosis of COVID-19 Disease based on Gravitational Search Optimization Algorithm. arXiv 2020, arXiv:2004.05084. [Google Scholar]
- Alom, M.Z.; Rahman, M.M.S.; Nasrin, M.S.; Taha, T.M.; Asari, V.K. COVID_MTNet: COVID-19 Detection with Multi-Task Deep Learning Approaches. arXiv 2020, arXiv:2004.03747. [Google Scholar]
- Khan, A.I.; Shah, J.L.; Bhat, M. CoroNet: A deep neural network for detection and diagnosis of COVID-19 from chest X-ray images. Comput. Methods Programs Biomed. 2020, 196, 105581. [Google Scholar] [CrossRef]
- Minaee, S.; Kafieh, R.; Sonka, M.; Yazdani, S.; Soufi, G.J. Deep-COVID: Predicting COVID-19 from chest X-ray images using deep transfer learning. Med. Image Anal. 2020, 65, 101794. [Google Scholar] [CrossRef]
- Polsinelli, M.; Cinque, L.; Placidi, G. A light CNN for detecting COVID-19 from CT scans of the chest. Pattern Recognit. Lett. 2020, 140, 95–100. [Google Scholar] [CrossRef]
- Goodwin, B.D.; Jaskolski, C.; Zhong, C.; Asmani, H. Intra-model Variability in COVID-19 Classification Using Chest X-ray Images. arXiv 2020, arXiv:2005.02167. [Google Scholar]
- Yamaç, M.; Ahishali, M.; Degerli, A.; Kiranyaz, S.; Chowdhury, M.E.H.; Gabbouj, M. Convolutional Sparse Support Estimator-Based COVID-19 Recognition From X-ray Images. IEEE Trans. Neural Netw. Learn. Syst. 2021, 32, 1810–1820. [Google Scholar] [CrossRef]
- Misra, S.; Jeon, S.; Lee, S.; Managuli, R.; Kim, C. Multi-Channel Transfer Learning of Chest X-ray Images for Screening of COVID-19. arXiv 2020, arXiv:2005.05576. [Google Scholar] [CrossRef]
- Chen, X.; Yao, L.; Zhou, T.; Dong, J.; Zhang, Y. Momentum contrastive learning for few-shot COVID-19 diagnosis from chest CT images. Pattern Recognit. 2021, 113, 107826. [Google Scholar] [CrossRef] [PubMed]
- Nishio, M.; Noguchi, S.; Matsuo, H.; Murakami, T. Automatic classification between COVID-19 pneumonia, non-COVID-19 pneumonia, and the healthy on chest X-ray image: Combination of data augmentation methods. Sci. Rep. 2020, 10, 17532. [Google Scholar] [CrossRef] [PubMed]
- Kumar, R.; Arora, R.; Bansal, V.; Sahayasheela, V.J.; Buckchash, H.; Imran, J.; Narayanan, N.; Pandian, G.N.; Raman, B. Accurate Prediction of COVID-19 using Chest X-ray Images through Deep Feature Learning model with SMOTE and Machine Learning Classifiers. medRxiv 2020. [Google Scholar] [CrossRef]
- Khalifa, N.E.M.; Taha, M.H.N.; Hassanien, A.E.; Elghamrawy, S.M. Detection of Coronavirus (COVID-19) Associated Pneumonia based on Generative Adversarial Networks and a Fine-Tuned Deep Transfer Learning Model using Chest X-ray Dataset. arXiv 2020, arXiv:2004.01184. [Google Scholar]
- Mobiny, A.; Cicalese, P.A.; Zare, S.; Yuan, P.; Abavisani, M.; Wu, C.C.; Ahuja, J.; de Groot, P.M.; Nguyen, H.V. Radiologist-Level COVID-19 Detection Using CT Scans with Detail-Oriented Capsule Networks. arXiv 2020, arXiv:2004.07407. [Google Scholar]
- Goodfellow, I.J.; Pouget-Abadie, J.; Mirza, M.; Xu, B.; Warde-Farley, D.; Ozair, S.; Courville, A.C.; Bengio, Y. Generative Adversarial Nets. In Proceedings of the Advances in Neural Information Processing Systems 2014, Montreal, QC, Canada, 8–13 December 2014. [Google Scholar]
- Mirza, M.; Osindero, S. Conditional Generative Adversarial Nets. arXiv 2014, arXiv:1411.1784. [Google Scholar]
- Wang, J.; Bao, Y.; Wen, Y.; Lu, H.; Luo, H.; Xiang, Y.; Li, X.; Liu, C.; Qian, D. Prior-Attention Residual Learning for More Discriminative COVID-19 Screening in CT Images. IEEE Trans. Med. Imaging 2020, 39, 2572–2583. [Google Scholar] [CrossRef]
- Ismael, A.M.; Şengür, A. Deep learning approaches for COVID-19 detection based on chest X-ray images. Expert Syst. Appl. 2020, 164, 114054. [Google Scholar] [CrossRef]
- Rahimzadeh, M.; Attar, A.; Sakhaei, S.M. A fully automated deep learning-based network for detecting COVID-19 from a new and large lung CT scan dataset. Biomed. Signal Process. Control 2021, 68, 102588. [Google Scholar] [CrossRef]
- Nour, M.K.A.; Cömert, Z.; Polat, K. A Novel Medical Diagnosis model for COVID-19 infection detection based on Deep Features and Bayesian Optimization. Appl. Soft Comput. 2020, 97, 106580. [Google Scholar] [CrossRef]
- Jaiswal, A.; Gianchandani, N.; Singh, D.; Kumar, V.; Kaur, M. Classification of the COVID-19 infected patients using DenseNet201 based deep transfer learning. J. Biomol. Struct. Dyn. 2020, 39, 5682–5689. [Google Scholar] [CrossRef] [PubMed]
- Gifani, P.; Shalbaf, A.; Vafaeezadeh, M. Automated detection of COVID-19 using ensemble of transfer learning with deep convolutional neural network based on CT scans. Int. J. Comput. Assist. Radiol. Surg. 2020, 16, 115–123. [Google Scholar] [CrossRef] [PubMed]
- Tartaglione, E.; Barbano, C.A.; Berzovini, C.; Calandri, M.; Grangetto, M. Unveiling COVID-19 from CHEST X-ray with Deep Learning: A Hurdles Race with Small Data. Int. J. Environ. Res. Public Health 2020, 17, 6933. [Google Scholar] [CrossRef] [PubMed]
- Karakanis, S.; Leontidis, G. Lightweight deep learning models for detecting COVID-19 from chest X-ray images. Comput. Biol. Med. 2021, 130, 104181. [Google Scholar] [CrossRef] [PubMed]
- Schaudt, D.; Kloth, C.; Spaete, C.; Hinteregger, A.; Beer, M.; von Schwerin, R. Improving COVID-19 CXR Detection with Synthetic Data Augmentation. arXiv 2021, arXiv:2112.07529. [Google Scholar]
- Trinh, Q.H.; Nguyen, M.L. Custom Deep Neural Network for 3D Covid Chest CT-scan Classification. arXiv 2021, arXiv:2107.01456. [Google Scholar]
- Aslan, M.F.; Unlersen, M.F.; Sabanci, K.; Durdu, A. CNN-based transfer learning–BiLSTM network: A novel approach for COVID-19 infection detection. Appl. Soft Comput. 2020, 98, 106912. [Google Scholar] [CrossRef]
- Makris, A.; Kontopoulos, I.; Tserpes, K. COVID-19 detection from chest X-ray images using Deep Learning and Convolutional Neural Networks. medRxiv 2020. [Google Scholar] [CrossRef]
- Quan, H.; Xu, X.; Zheng, T.; Li, Z.; Zhao, M.; Cui, X. DenseCapsNet: Detection of COVID-19 from X-ray images using a capsule neural network✩. Comput. Biol. Med. 2021, 133, 104399. [Google Scholar] [CrossRef]
- Ahmad, F.; Khan, M.U.G.; Javed, K. Deep learning model for distinguishing novel coronavirus from other chest related infections in X-ray images. Comput. Biol. Med. 2021, 134, 104401. [Google Scholar] [CrossRef]
- Luz, E.; Silva, P.; Silva, R.; Silva, L.; Guimarães, J.; Miozzo, G.; Menotti, D. Towards an effective and efficient deep learning model for COVID-19 patterns detection in X-ray images. Res. Biomed. Eng. 2021. [Google Scholar] [CrossRef]
- He, X.; Yang, X.; Zhang, S.; Zhao, J.; shan Zhang, Y.; Xing, E.P.; Xie, P. Sample-Efficient Deep Learning for COVID-19 Diagnosis Based on CT Scans. medRxiv 2020. [Google Scholar] [CrossRef]
- Rahimzadeh, M.; Attar, A. A modified deep convolutional neural network for detecting COVID-19 and pneumonia from chest X-ray images based on the concatenation of Xception and ResNet50V2. Inform. Med. Unlocked 2020, 19, 100360. [Google Scholar] [CrossRef] [PubMed]
- Hsu, C.C.; Chen, G.L.; Wu, M.H. Visual Transformer with Statistical Test for COVID-19 Classification. arXiv 2021, arXiv:2107.05334. [Google Scholar]
- Qi, H.; Wang, Y.; Liu, X. 3D RegNet: Deep Learning Model for COVID-19 Diagnosis on Chest CT Image. arXiv 2021, arXiv:2107.04055. [Google Scholar]
- Schlemper, J.; Oktay, O.; Schaap, M.; Heinrich, M.P.; Kainz, B.; Glocker, B.; Rueckert, D. Attention Gated Networks: Learning to Leverage Salient Regions in Medical Images. Med. Image Anal. 2019, 53, 197–207. [Google Scholar] [CrossRef]
- Monshi, M.M.A.; Poon, J.; Chung, Y.Y.; Monshi, F.M. CovidXrayNet: Optimizing data augmentation and CNN hyperparameters for improved COVID-19 detection from CXR. Comput. Biol. Med. 2021, 133, 104375. [Google Scholar] [CrossRef]
- Zhong, Y. Using Deep Convolutional Neural Networks to Diagnose COVID-19 From Chest X-ray Images. arXiv 2020, arXiv:2007.09695. [Google Scholar]
- Nayak, S.R.; Nayak, D.R.; Sinha, U.; Arora, V.; Pachori, R.B. Application of deep learning techniques for detection of COVID-19 cases using chest X-ray images: A comprehensive study. Biomed. Signal Process. Control 2020, 64, 102365. [Google Scholar] [CrossRef]
- Ardakani, A.A.; Kanafi, A.R.; Acharya, U.R.; Khadem, N.; Mohammadi, A. Application of deep learning technique to manage COVID-19 in routine clinical practice using CT images: Results of 10 convolutional neural networks. Comput. Biol. Med. 2020, 121, 103795. [Google Scholar] [CrossRef]
- Maguolo, G.; Nanni, L. A critic evaluation of methods for COVID-19 automatic detection from X-ray images. Int. J. Inf. Fusion 2021, 76, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Liu, B.; Liu, P.; Dai, L.; Yang, Y.; Xie, P.; Tan, Y.X.; Du, J.; Shan, W.; Zhao, C.; Zhong, Q.; et al. Assisting Scalable Diagnosis Automatically via CT Images in the Combat against COVID-19. medRxiv 2020, 11, 4145. [Google Scholar] [CrossRef] [PubMed]
- Li, L.; Qin, L.; Xu, Z.; Yin, Y.; Wang, X.; Kong, B.; Bai, J.; Lu, Y.; Fang, Z.; Song, Q.; et al. Artificial Intelligence Distinguishes COVID-19 from Community Acquired Pneumonia on Chest CT. Radiology 2020. [Google Scholar] [CrossRef] [PubMed]
- Atitallah, S.B.; Driss, M.; Boulila, W.; Gh’ezala, H.B. Randomly initialized convolutional neural network for the recognition of COVID-19 using X-ray images. Int. J. Imaging Syst. Technol. 2021, 32, 55–73. [Google Scholar] [CrossRef] [PubMed]
- Zhong, A.; Li, X.; Wu, D.; Ren, H.; Kim, K.; Kim, Y.; Buch, V.; Neumark, N.; Bizzo, B.C.; Tak, W.Y.; et al. Deep metric learning-based image retrieval system for chest radiograph and its clinical applications in COVID-19. Med. Image Anal. 2021, 70, 101993. [Google Scholar] [CrossRef]
- Goncharov, M.; Pisov, M.; Shevtsov, A.; Shirokikh, B.; Kurmukov, A.; Blokhin, I.A.; Chernina, V.Y.; Solovev, A.V.; Gombolevskiy, V.A.; Morozov, S.P.; et al. CT-Based COVID-19 triage: Deep multitask learning improves joint identification and severity quantification. Med. Image Anal. 2021, 71, 102054. [Google Scholar] [CrossRef]
- Amyar, A.; Modzelewski, R.; Li, H.; Ruan, S. Multi-task deep learning based CT imaging analysis for COVID-19 pneumonia: Classification and segmentation. Comput. Biol. Med. 2020, 126, 104037. [Google Scholar] [CrossRef]
- Gammulle, H.; Fernando, T.; Sridharan, S.; Denman, S.; Fookes, C. Multi-Slice Net: A Novel Light Weight Framework for COVID-19 Diagnosis. In Proceedings of the 2021 IEEE International Conference on Autonomous Systems (ICAS), Montreal, QC, Canada, 11–13 August 2021; pp. 1–5. [Google Scholar]
- Zhang, X.; Han, L.; Sobeih, T.; Han, L.; Dempsey-Hibbert, N.C.; Lechareas, S.; Tridente, A.; Chen, H.; White, S. CXR-Net: An Encoder-Decoder-Encoder Multitask Deep Neural Network for Explainable and Accurate Diagnosis of COVID-19 pneumonia with Chest X-ray Images. arXiv 2021, arXiv:2110.10813. [Google Scholar]
- Henna, S.; Reji, A.P. A Data Augmented Approach to Transfer Learning for Covid-19 Detection. arXiv 2021, arXiv:2108.02870. [Google Scholar]
- Karim, M.R.; Döhmen, T.; Rebholz-Schuhmann, D.; Decker, S.; Cochez, M.; Beyan, O. DeepCOVIDExplainer: Explainable COVID-19 Predictions Based on Chest X-ray Images. arXiv 2020, arXiv:2004.04582. [Google Scholar]
- Oh, Y.; Park, S.; Ye, J.C. Deep Learning COVID-19 Features on CXR Using Limited Training Data Sets. IEEE Trans. Med. Imaging 2020, 39, 2688–2700. [Google Scholar] [CrossRef] [PubMed]
- Kamalaveni, V.; Rajalakshmi, R.; Narayanankutty, K.A. Image Denoising Using Variations of Perona-Malik Model with Different Edge Stopping Functions. Procedia Comput. Sci. 2015, 58, 673–682. [Google Scholar] [CrossRef] [Green Version]
- Lv, D.; Qi, W.; Li, Y.; Sun, L.; Wang, Y. A cascade network for Detecting COVID-19 using chest X-rays. arXiv 2020, arXiv:2005.01468. [Google Scholar]
- Siddhartha, M.; Santra, A. COVIDLite: A depth-wise separable deep neural network with white balance and CLAHE for detection of COVID-19. arXiv 2020, arXiv:2006.13873. [Google Scholar]
- Szegedy, C.; Liu, W.; Jia, Y.; Sermanet, P.; Reed, S.E.; Anguelov, D.; Erhan, D.; Vanhoucke, V.; Rabinovich, A. Going deeper with convolutions. In Proceedings of the 2015 IEEE Conference on Computer Vision and Pattern Recognition (CVPR), Boston, MA, USA, 7–12 June 2015; pp. 1–9. [Google Scholar]
- Huang, G.; Liu, Z.; Weinberger, K.Q. Densely Connected Convolutional Networks. In Proceedings of the 2017 IEEE Conference on Computer Vision and Pattern Recognition (CVPR), Honolulu, HI, USA, 21–26 July 2017; pp. 2261–2269. [Google Scholar]
- Simonyan, K.; Zisserman, A. Very Deep Convolutional Networks for Large-Scale Image Recognition. arXiv 2015, arXiv:1409.1556. [Google Scholar]
- Howard, A.G.; Zhu, M.; Chen, B.; Kalenichenko, D.; Wang, W.; Weyand, T.; Andreetto, M.; Adam, H. MobileNets: Efficient Convolutional Neural Networks for Mobile Vision Applications. arXiv 2017, arXiv:1704.04861. [Google Scholar]
- Iandola, F.N.; Moskewicz, M.W.; Ashraf, K.; Han, S.; Dally, W.J.; Keutzer, K. SqueezeNet: AlexNet-level accuracy with 50x fewer parameters and <1MB model size. arXiv 2016, arXiv:1602.07360. [Google Scholar]
- Krizhevsky, A.; Sutskever, I.; Hinton, G.E. ImageNet classification with deep convolutional neural networks. Commun. ACM 2012, 60, 84–90. [Google Scholar] [CrossRef]
- Sabour, S.; Frosst, N.; Hinton, G.E. Dynamic Routing Between Capsules. arXiv 2017, arXiv:1710.09829. [Google Scholar]
- Xu, X.; Jiang, X.; Ma, C.; Du, P.; Li, X.; Lv, S.; Yu, L.; Chen, Y.; Su, J.; Lang, G.; et al. Deep Learning System to Screen Coronavirus Disease 2019 Pneumonia. arXiv 2020, arXiv:2002.09334. [Google Scholar] [CrossRef]
- Song, Y.; Zheng, S.; Li, L.; Zhang, X.; Huang, Z.; Chen, J.; Zhao, H.; Jie, Y.; Wang, R.; Chong, Y.; et al. Deep learning Enables Accurate Diagnosis of Novel Coronavirus (COVID-19) with CT images. medRxiv 2020, 18, 2775–2780. [Google Scholar] [CrossRef] [PubMed]
- Sethy, P.K.; Behera, S.K.; Ratha, P.K.; Biswas, P. Detection of coronavirus Disease (COVID-19) based on Deep Features and Support Vector Machine. Preprints 2020. [Google Scholar] [CrossRef]
- Jin, C.; Chen, W.; Cao, Y.; Xu, Z.; Zhang, X.; Deng, L.; Zheng, C.; Zhou, J.; Shi, H.; Feng, J. Development and Evaluation of an AI System for COVID-19 Diagnosis. Nat. Commun. 2020, 11, 5088. [Google Scholar] [CrossRef] [PubMed]
- Hemdan, E.E.D.; Shouman, M.A.; Karar, M.E. COVIDX-Net: A Framework of Deep Learning Classifiers to Diagnose COVID-19 in X-ray Images. arXiv 2020, arXiv:2003.11055. [Google Scholar]
- Narin, A.; Kaya, C.; Pamuk, Z. Automatic detection of coronavirus disease (COVID-19) using X-ray images and deep convolutional neural networks. Pattern Anal. Appl. 2021, 24, 1207–1220. [Google Scholar] [CrossRef]
- Zhang, J.; Xie, Y.; Li, Y.; Shen, C.; Xia, Y. COVID-19 Screening on Chest X-ray Images Using Deep Learning based Anomaly Detection. arXiv 2020, arXiv:2003.12338. [Google Scholar]
- Ghoshal, B.; Tucker, A. Estimating Uncertainty and Interpretability in Deep Learning for Coronavirus (COVID-19) Detection. arXiv 2020, arXiv:2003.10769. [Google Scholar]
- Fu, M.; Yi, S.L.; Zeng, Y.L.; Ye, F.; Li, Y.; Dong, X.; Ren, Y.D.; Luo, L.; Pan, J.S.; Zhang, Q. Deep Learning-Based Recognizing COVID-19 and other Common Infectious Diseases of the Lung by Chest CT Scan Images. medRxiv 2020. [Google Scholar] [CrossRef] [Green Version]
- Farooq, M.; Hafeez, A. COVID-ResNet: A Deep Learning Framework for Screening of COVID19 from Radiographs. arXiv 2020, arXiv:2003.14395. [Google Scholar]
- Gozes, O.; Frid-Adar, M.; Sagie, N.; Zhang, H.; Ji, W.; Greenspan, H. Coronavirus Detection and Analysis on Chest CT with Deep Learning. arXiv 2020, arXiv:2004.02640. [Google Scholar]
- Hall, L.O.; Paul, R.; Goldgof, D.B.; Goldgof, G.M. Finding Covid-19 from Chest X-rays using Deep Learning on a Small Dataset. arXiv 2020, arXiv:2004.02060. [Google Scholar]
- Kassani, S.H.; Kassani, P.H.; Wesolowski, M.J.; Schneider, K.A.; Deters, R. Automatic Detection of Coronavirus Disease (COVID-19) in X-ray and CT Images: A Machine Learning Based Approach. Biocybern. Biomed. Eng. 2021, 41, 867–879. [Google Scholar] [CrossRef] [PubMed]
- Punn, N.S.; Agarwal, S. Automated diagnosis of COVID-19 with limited posteroanterior chest X-ray images using fine-tuned deep neural networks. Appl. Intell. 2021, 51, 2689–2702. [Google Scholar] [CrossRef] [PubMed]
- Rahimzadeh, M.; Attar, A. A New Modified Deep Convolutional Neural Network for Detecting COVID-19 from X-ray Images. arXiv 2020, arXiv:2004.08052. [Google Scholar]
- Li, T.; Han, Z.; Wei, B.; Zheng, Y.; Hong, Y.; Cong, J. Robust Screening of COVID-19 from Chest X-ray via Discriminative Cost-Sensitive Learning. arXiv 2020, arXiv:2004.12592. [Google Scholar]
- Ouyang, X.; Huo, J.; Xia, L.; Shan, F.; Liu, J.; Mo, Z.; Yan, F.; Ding, Z.; Yang, Q.; Song, B.; et al. Dual-Sampling Attention Network for Diagnosis of COVID-19 From Community Acquired Pneumonia. IEEE Trans. Med. Imaging 2020, 39, 2595–2605. [Google Scholar] [CrossRef]
- Chatterjee, S.; Saad, F.; Sarasaen, C.; Ghosh, S.; Khatun, R.; Radeva, P.; Rose, G.; Stober, S.; Speck, O.; Nürnberger, A. Exploration of Interpretability Techniques for Deep COVID-19 Classification using Chest X-ray Images. arXiv 2020, arXiv:2006.02570. [Google Scholar]
- Saeedi, A.; Saeedi, M.; Maghsoudi, A. A Novel and Reliable Deep Learning Web-Based Tool to Detect COVID-19 Infection from Chest CT-Scan. arXiv 2020, arXiv:2006.14419. [Google Scholar]
- Shamsi, A.; Asgharnezhad, H.; Jokandan, S.S.; Khosravi, A.; Kebria, P.M.; Nahavandi, D.; Nahavandi, S.; Srinivasan, D. An Uncertainty-Aware Transfer Learning-Based Framework for COVID-19 Diagnosis. IEEE Trans. Neural Netw. Learn. Syst. 2021, 32, 1408–1417. [Google Scholar] [CrossRef]
- Zhou, T.; Lu, H.; Yang, Z.; Qiu, S.; qiang Huo, B.; Dong, Y. The ensemble deep learning model for novel COVID-19 on CT images. Appl. Soft Comput. 2020, 98, 106885. [Google Scholar] [CrossRef]
- Wu, X.; Hui, H.; Niu, M.; Li, L.; Wang, L.; He, B.; Yang, X.; Li, L.; Li, H.; Tian, J.; et al. Deep learning-based multi-view fusion model for screening 2019 novel coronavirus pneumonia: A multicentre study. Eur. J. Radiol. 2020, 128, 109041. [Google Scholar] [CrossRef]
- Horry, M.J.; Chakraborty, S.; Paul, M.; Ulhaq, A.; Pradhan, B.; Saha, M.; Shukla, N. X-ray Image based COVID-19 Detection using Pre-trained Deep Learning Models. 2020. Available online: https://engrxiv.org/index.php/engrxiv/preprint/view/937 (accessed on 5 March 2022).
- Bukhari, S.U.K.; Bukhari, S.U.K.; Syed, A.; Shah, S.S.H. The diagnostic evaluation of Convolutional Neural Network (CNN) for the assessment of chest X-ray of patients infected with COVID-19. medRxiv 2020. [Google Scholar] [CrossRef]
- Moutounet-Cartan, P.G.B. Deep Convolutional Neural Networks to Diagnose COVID-19 and other Pneumonia Diseases from Posteroanterior Chest X-rays. arXiv 2020, arXiv:2005.00845. [Google Scholar]
- Ghassemi, N.; Shoeibi, A.; Khodatars, M.; Heras, J.; Rahimi, A.; Zare, A.; Pachori, R.B.; Górriz, J.M. Automatic Diagnosis of COVID-19 from CT Images using CycleGAN and Transfer Learning. arXiv 2021, arXiv:2104.11949. [Google Scholar]
- Zeiser, F.A.; da Costa, C.A.; de Oliveira Ramos, G.; Bohn, H.C.; dos Santos, I.H.F.; da Rosa Righi, R. Evaluation of Convolutional Neural Networks for COVID-19 Classification on Chest X-rays. In Brazilian Conference on Intelligent Systems; Springer: Berlin/Heidelberg, Germany, 2021. [Google Scholar]
- Anwar, T. COVID19 Diagnosis using AutoML from 3D CT scans. In Proceedings of the 2021 IEEE/CVF International Conference on Computer Vision Workshops (ICCVW), Virtual Conference, 11–17 October 2021; pp. 503–507. [Google Scholar]
- Kollias, D.; Arsenos, A.; Soukissian, L.; Kollias, S.D. MIA-COV19D: COVID-19 Detection through 3-D Chest CT Image Analysis. In Proceedings of the 2021 IEEE/CVF International Conference on Computer Vision Workshops (ICCVW), Virtual Conference, 11–17 October 2021; pp. 537–544. [Google Scholar]
- Apostolopoulos, I.D.; Bessiana, T. Covid-19: Automatic detection from X-ray images utilizing Transfer Learning with Convolutional Neural Networks. arXiv 2020, arXiv:2003.11617. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rajaraman, S.; Siegelman, J.; Alderson, P.O.; Folio, L.S.; Folio, L.R.; Antani, S.K. Iteratively Pruned Deep Learning Ensembles for COVID-19 Detection in Chest X-rays. IEEE Access 2020, 8, 115041–115050. [Google Scholar] [CrossRef]
- Gonz’alez, G.; Bustos, A.; Salinas, J.M.; de la Iglesia-Vayá, M.; Galant, J.; Cano-Espinosa, C.; Barber, X.; Orozco-Beltr’an, D.; Cazorla, M.; Pertusa, A. UMLS-ChestNet: A deep convolutional neural network for radiological findings, differential diagnoses and localizations of COVID-19 in chest X-rays. arXiv 2020, arXiv:2006.05274. [Google Scholar]
- Li, X.; Li, C.; Zhu, D. COVID-MobileXpert: On-Device COVID-19 Screening using Snapshots of Chest X-ray. arXiv 2020, arXiv:2004.03042. [Google Scholar]
- Yeh, C.F.; Cheng, H.T.; Wei, A.; Liu, K.C.; Ko, M.C.; Kuo, P.C.; Chen, R.J.; Lee, P.C.; Chuang, J.H.; Chen, C.M.; et al. A Cascaded Learning Strategy for Robust COVID-19 Pneumonia Chest X-ray Screening. arXiv 2020, arXiv:2004.12786. [Google Scholar]
- Tan, W.; Guo, H. Data Augmentation and CNN Classification For Automatic COVID-19 Diagnosis From CT-Scan Images On Small Dataset. arXiv 2021, arXiv:2108.07148. [Google Scholar]
- Gao, X.; Qian, Y.; Gao, A. COVID-VIT: Classification of COVID-19 from CT chest images based on vision transformer models. arXiv 2021, arXiv:2107.01682. [Google Scholar]
- Nasiri, H.; Alavi, S.A. A novel framework based on deep learning and ANOVA feature selection method for diagnosis of COVID-19 cases from chest X-ray Images. arXiv 2021, arXiv:2110.06340. [Google Scholar] [CrossRef] [PubMed]
- Heidari, M.; Mirniaharikandehei, S.; Khuzani, A.Z.; Danala, G.; Qiu, Y.; Zheng, B. Improving the performance of CNN to predict the likelihood of COVID-19 using chest X-ray images with preprocessing algorithms. Int. J. Med. Inform. 2020, 144, 104284. [Google Scholar] [CrossRef] [PubMed]
- Gour, M.; Jain, S. Stacked Convolutional Neural Network for Diagnosis of COVID-19 Disease from X-ray Images. arXiv 2020, arXiv:2006.13817. [Google Scholar]
- Brunese, L.; Mercaldo, F.; Reginelli, A.; Santone, A. Explainable Deep Learning for Pulmonary Disease and Coronavirus COVID-19 Detection from X-rays. Comput. Methods Programs Biomed. 2020, 196, 105608. [Google Scholar] [CrossRef]
- Shah, V.; Keniya, R.; Shridharani, A.; Punjabi, M.; Shah, J.; Mehendale, N.D. Diagnosis of COVID-19 using CT scan images and deep learning techniques. Emerg. Radiol. 2021, 28, 497–505. [Google Scholar] [CrossRef] [PubMed]
- Menon, S.; Mangalagiri, J.; Galita, J.; Morris, M.; Saboury, B.; Yesha, Y.; Yesha, Y.; Nguyen, P.; Gangopadhyay, A.; Chapman, D. CCS-GAN: COVID-19 CT-scan classification with very few positive training images. arXiv 2021, arXiv:2110.01605. [Google Scholar]
- Teli, M.N. TeliNet: Classifying CT scan images for COVID-19 diagnosis. In Proceedings of the 2021 IEEE/CVF International Conference on Computer Vision Workshops (ICCVW), Virtual Conference, 11–17 October 2021; pp. 496–502. [Google Scholar]
- Apostolopoulos, I.D.; Aznaouridis, S.; Tzani, M. Extracting Possibly Representative COVID-19 Biomarkers from X-ray Images with Deep Learning Approach and Image Data Related to Pulmonary Diseases. J. Med. Biol. Eng. 2020, 40, 462–469. [Google Scholar] [CrossRef]
- Abbas, A.; Abdelsamea, M.M.; Gaber, M.M. Classification of COVID-19 in chest X-ray images using DeTraC deep convolutional neural network. Appl. Intell. 2021, 51, 854–864. [Google Scholar] [CrossRef]
- Maghdid, H.S.; Asaad, A.; Ghafoor, K.Z.; Sadiq, A.S.; Khan, M.K. Diagnosing COVID-19 pneumonia from X-ray and CT images using deep learning and transfer learning algorithms. In Multimodal Image Exploitation and Learning 2021; International Society for Optics and Photonics: Bellingham, WA, USA, 2021. [Google Scholar]
- Loey, M.; Smarandache, F.; Khalifa, N.E.M. Within the Lack of Chest COVID-19 X-ray Dataset: A Novel Detection Model Based on GAN and Deep Transfer Learning. Symmetry 2020, 12, 651. [Google Scholar] [CrossRef] [Green Version]
- Jin, W.; Dong, S.; Dong, C.; Ye, X. Hybrid ensemble model for differential diagnosis between COVID-19 and common viral pneumonia by chest X-ray radiograph. Comput. Biol. Med. 2021, 131, 104252. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Lin, Z.Q.; Wong, A. COVID-Net: A tailored deep convolutional neural network design for detection of COVID-19 cases from chest X-ray images. Sci. Rep. 2020, 10, 19549. [Google Scholar] [CrossRef] [PubMed]
- Pereira, R.M.; Bertolini, D.; Teixeira, L.O.; Silla, C.N., Jr.; Costa, Y.M.G. COVID-19 identification in chest X-ray images on flat and hierarchical classification scenarios. Comput. Methods Programs Biomed. 2020, 194, 105532. [Google Scholar] [CrossRef] [PubMed]
- Goel, C.; Kumar, A.; Dubey, S.; Srivastava, V. Efficient Deep Network Architecture for COVID-19 Detection Using Computed Tomography Images. medRxiv 2020. [Google Scholar] [CrossRef]
- Hu, S.; Gao, Y.; Niu, Z.; Jiang, Y.; Li, L.; Xiao, X.; Wang, M.; Fang, E.F.; Menpes-Smith, W.; Xia, J.; et al. Weakly Supervised Deep Learning for COVID-19 Infection Detection and Classification From CT Images. IEEE Access 2020, 8, 118869–118883. [Google Scholar] [CrossRef]
- Lin, T.Y.; Dollár, P.; Girshick, R.B.; He, K.; Hariharan, B.; Belongie, S.J. Feature Pyramid Networks for Object Detection. In Proceedings of the 2017 IEEE Conference on Computer Vision and Pattern Recognition (CVPR), Honolulu, HI, USA, 21–26 July 2017; pp. 936–944. [Google Scholar]
- Han, Z.; Wei, B.; Hong, Y.; Li, T.; Cong, J.; Zhu, X.; Wei, H.; Zhang, W. Accurate Screening of COVID-19 Using Attention-Based Deep 3D Multiple Instance Learning. IEEE Trans. Med. Imaging 2020, 39, 2584–2594. [Google Scholar] [CrossRef]
- Wang, S.; Zha, Y.; Li, W.; Wu, Q.; Li, X.; Niu, M.; Wang, M.; Qiu, X.; Li, H.; Yu, H.; et al. A Fully Automatic Deep Learning System for COVID-19 Diagnostic and Prognostic Analysis. medRxiv 2020, 56, 2000775. [Google Scholar] [CrossRef]
- Shi, F.; Xia, L.; Shan, F.; Wu, D.; Wei, Y.; Yuan, H.; Jiang, H.; Gao, Y.; Sui, H.; Shen, D. Large-Scale Screening of COVID-19 from Community Acquired Pneumonia using Infection Size-Aware Classification. arXiv 2020, arXiv:2003.09860. [Google Scholar]
- Sun, L.; Mo, Z.; Yan, F.; Xia, L.; Shan, F.; Ding, Z.; Song, B.; Gao, W.; Shao, W.; Shi, F.; et al. Adaptive Feature Selection Guided Deep Forest for COVID-19 Classification With Chest CT. IEEE J. Biomed. Health Inform. 2020, 24, 2798–2805. [Google Scholar] [CrossRef]
- Hassanien, A.E.; Mahdy, L.N.; Ezzat, K.A.; Elmousalami, H.H.; Ella, H.A. Automatic X-ray COVID-19 Lung Image Classification System based on Multi-Level Thresholding and Support Vector Machine. medRxiv 2020. [Google Scholar] [CrossRef]
- Ke, G.; Meng, Q.; Finley, T.; Wang, T.; Chen, W.; Ma, W.; Ye, Q.; Liu, T.Y. LightGBM: A Highly Efficient Gradient Boosting Decision Tree. NIPS. 2017. Available online: https://papers.nips.cc/paper/2017/file/6449f44a102fde848669bdd9eb6b76fa-Paper.pdf (accessed on 5 March 2022).
- Tibshirani, R. Regression Shrinkage and Selection via the Lasso. J. R. Stat. Soc. Ser. Methodol. 1996, 58, 267–288. [Google Scholar] [CrossRef]
- Zhou, Z.H.; Feng, J. Deep Forest: Towards An Alternative to Deep Neural Networks. arXiv 2017, arXiv:1702.08835. [Google Scholar]
- Chen, J.; lian Wu, L.; Zhang, J.; Zhang, L.; Gong, D.; lin Zhao, Y.; Hu, S.; Wang, Y.; Hu, X.; Zheng, B.; et al. Deep learning-based model for detecting 2019 novel coronavirus pneumonia on high-resolution computed tomography: A prospective study. medRxiv 2020, 10, 19196. [Google Scholar] [CrossRef]
- Zhang, Y.; Niu, S.; Qiu, Z.; Wei, Y.; Zhao, P.; Yao, J.; Huang, J.; Wu, Q.; Tan, M. COVID-DA: Deep Domain Adaptation from Typical Pneumonia to COVID-19. arXiv 2020, arXiv:2005.01577. [Google Scholar]
- Mei, X.; Lee, H.C.; Diao, K.; Huang, M.; Lin, B.; Liu, C.; Xie, Z.; Ma, Y.; Robson, P.M.; Chung, M.S.; et al. Artificial intelligence–enabled rapid diagnosis of patients with COVID-19. Nat. Med. 2020, 26, 1224–1228. [Google Scholar] [CrossRef]
- De Melo e Sousa, A.; Reis, F.; Zerbini, R.; Comba, J.L.D.; Falcão, A.X. CNN Filter Learning from Drawn Markers for the Detection of Suggestive Signs of COVID-19 in CT Images. In Proceedings of the 2021 43rd Annual International Conference of the IEEE Engineering in Medicine & Biology Society (EMBC), Guadalajara, Mexico, 31 October–4 November 2021; pp. 3169–3172. [Google Scholar]
- Ali, A.R.; Budka, M. An Automated Approach for Timely Diagnosis and Prognosis of Coronavirus Disease. In Proceedings of the 2021 International Joint Conference on Neural Networks (IJCNN), Shenzhen, China, 18–22 July 2021; pp. 1–8. [Google Scholar]
- Hussain, M.G.; Ye, S. Recognition of COVID-19 Disease Utilizing X-ray Imaging of the Chest Using CNN. In Proceedings of the 2021 International Conference on Computing, Electronics & Communications Engineering (iCCECE), Southend, UK, 16–17 August 2021; pp. 71–76. [Google Scholar]
- Hasan, M.K.; Alam, M.A.; Elahi, M.T.E.; Roy, S.; Wahid, S.R. CVR-Net: A deep convolutional neural network for coronavirus recognition from chest radiography images. arXiv 2020, arXiv:2007.11993. [Google Scholar]
- Mahmud, T.; Rahman, M.A.; Fattah, S.A. CovXNet: A multi-dilation convolutional neural network for automatic COVID-19 and other pneumonia detection from chest X-ray images with transferable multi-receptive feature optimization. Comput. Biol. Med. 2020, 122, 103869. [Google Scholar] [CrossRef]
- Pathari, S. Automatic Detection of COVID-19 and Pneumonia from Chest X-ray using Deep Learning. arXiv 2021, arXiv:2110.09384. [Google Scholar]
- Zhou, J.; Jing, B.; Wang, Z. SODA: Detecting Covid-19 in Chest X-rays with Semi-supervised Open Set Domain Adaptation. IEEE/ACM Trans. Comput. Biol. Bioinform. 2021. [Google Scholar] [CrossRef]
- Yousefzadeh, M.; Esfahanian, P.; Movahed, S.M.S.; Gorgin, S.; Rahmati, D.; Kiani, A.; Nadji, S.A.; Haseli, S.; Hoseinyazdi, M.; Roshandel, J.; et al. ai-corona: Radiologist-Assistant Deep Learning Framework for COVID-19 Diagnosis in Chest CT Scans. medRxiv 2020. [Google Scholar] [CrossRef]
- Singh, D.; Kumar, V.; Vaishali; Kaur, M. Classification of COVID-19 patients from chest CT images using multi-objective differential evolution–based convolutional neural networks. Eur. J. Clin. Microbiol. Infect. Dis. 2020, 39, 1379–1389. [Google Scholar] [CrossRef] [PubMed]
- Mukherjee, H.; Ghosh, S.; Dhar, A.; Obaidullah, S.M.; Santosh, K.C.; Roy, K. Shallow Convolutional Neural Network for COVID-19 Outbreak Screening Using Chest X-rays. Cogn. Comput. 2021. [Google Scholar] [CrossRef] [PubMed]
- Barstugan, M.; Ozkaya, U.; Şaban, Ö. Coronavirus (COVID-19) Classification using CT Images by Machine Learning Methods. arXiv 2021, arXiv:2003.09424. [Google Scholar]
- Morani, K.; Ünay, D. Deep Learning Based Automated COVID-19 Classification from Computed Tomography Images. arXiv 2021, arXiv:2111.11191. [Google Scholar]
- Tan, W.; Liu, J. A 3D CNN Network with BERT For Automatic COVID-19 Diagnosis From CT-Scan Images. In Proceedings of the 2021 IEEE/CVF International Conference on Computer Vision Workshops (ICCVW), Montreal, BC, Canada, 11–17 October 2021; pp. 439–445. [Google Scholar]
- Liang, S. A hybrid deep learning framework for Covid-19 detection via 3D Chest CT Images. arXiv 2021, arXiv:2107.03904. [Google Scholar]
- Das, D.; Santosh, K.C.; Pal, U. Truncated inception net: COVID-19 outbreak screening using chest X-rays. Phys. Eng. Sci. Med. 2020, 43, 915–925. [Google Scholar] [CrossRef]
- Antonchuk, J.; Prescott, B.; Melanchthon, P.; Singh, R. COVID-19 Pneumonia and Influenza Pneumonia Detection Using Convolutional Neural Networks. arXiv 2021, arXiv:2112.07102. [Google Scholar]
- Ucar, F.; Korkmaz, D. COVIDiagnosis-Net: Deep Bayes-SqueezeNet based diagnosis of the coronavirus disease 2019 (COVID-19) from X-ray images. Med. Hypotheses 2020, 140, 109761. [Google Scholar] [CrossRef]
- Sarkar, A.; Vandenhirtz, J.; Nagy, J.B.; Bacsa, D.; Riley, M. Detection of COVID-19 from Chest X-rays using Deep Learning: Comparing COGNEX VisionPro Deep Learning 1.0 Software with Open Source Convolutional Neural Networks. 2020. Available online: https://www.researchgate.net/publication/343414434_Detection_of_COVID-19_from_Chest_X-rays_using_Deep_Learning_Comparing_COGNEX_VisionPro_Deep_Learning_10_Software_with_Open_Source_Convolutional_Neural_Networks (accessed on 5 March 2022).
- Miron, R.; Moisii, C.; Dinu, S.A.; Breaban, M. COVID Detection in Chest CTs: Improving the Baseline on COV19-CT-DB. arXiv 2021, arXiv:2107.04808. [Google Scholar]
- Elghamrawy, S.M.; ell Hassanien, A. Diagnosis and Prediction Model for COVID19 Patients Response to Treatment based on Convolutional Neural Networks and Whale Optimization Algorithm Using CT Images. medRxiv 2020. [Google Scholar] [CrossRef] [Green Version]
- Kang, H.; Xia, L.; Yan, F.; Wan, Z.; Shi, F.; Yuan, H.; Jiang, H.; Wu, D.; Sui, H.; Zhang, C.; et al. Diagnosis of Coronavirus Disease 2019 (COVID-19) With Structured Latent Multi-View Representation Learning. IEEE Trans. Med. Imaging 2020, 39, 2606–2614. [Google Scholar] [CrossRef] [PubMed]
- Banerjee, I.; Sinha, P.; Purkayastha, S.; Mashhaditafreshi, N.; Tariq, A.; Jeong, J.J.; Trivedi, H.; Gichoya, J.W. Was there COVID-19 back in 2012? Challenge for AI in Diagnosis with Similar Indications. arXiv 2020, arXiv:2006.13262. [Google Scholar]
- Mohammed, M.A.; Abdulkareem, K.H.; Al-Waisy, A.S.; Mostafa, S.A.; Al-Fahdawi, S.; Dinar, A.M.; Alhakami, W.; Baz, A.; Al-Mhiqani, M.N.; Alhakami, H.; et al. Benchmarking Methodology for Selection of Optimal COVID-19 Diagnostic Model Based on Entropy and TOPSIS Methods. IEEE Access 2020, 8, 99115–99131. [Google Scholar] [CrossRef]
- Chen, X.; Yao, L.; Zhang, Y. Residual Attention U-Net for Automated Multi-Class Segmentation of COVID-19 Chest CT Images. arXiv 2020, arXiv:2004.05645. [Google Scholar]
- Lokwani, R.; Gaikwad, A.; Kulkarni, V.; Pant, A.; Kharat, A. Automated Detection of COVID-19 from CT Scans Using Convolutional Neural Networks. Int. J. Comput. Assist. Radiol. Surg. 2021, 16, 115–123. [Google Scholar]
- Wu, Y.; Gao, S.; Mei, J.; Xu, J.; Fan, D.; Zhang, R.; Cheng, M. JCS: An Explainable COVID-19 Diagnosis System by Joint Classification and Segmentation. IEEE Trans. Image Process. 2021, 30, 3113–3126. [Google Scholar] [CrossRef]
- Fan, D.P.; Zhou, T.; Ji, G.P.; Zhou, Y.; Chen, G.; Fu, H.B.; Shen, J.; Shao, L. Inf-Net: Automatic COVID-19 Lung Infection Segmentation from CT Scans. arXiv 2020, arXiv:2004.14133. [Google Scholar]
- Gao, K.; Su, J.; biao Jiang, Z.; Zeng, L.; Feng, Z.; Shen, H.; Rong, P.; Xu, X.; Qin, J.; Yang, Y.; et al. Dual-branch combination network (DCN): Towards accurate diagnosis and lesion segmentation of COVID-19 using CT images. Med. Image Anal. 2020, 67, 101836. [Google Scholar] [CrossRef]
- Yang, D.; Xu, Z.; Li, W.; Myronenko, A.; Roth, H.R.; Harmon, S.A.; Xu, S.; Turkbey, B.; Turkbey, E.B.; Wang, X.; et al. Federated semi-supervised learning for COVID region segmentation in chest CT using multi-national data from China, Italy, Japan. Med. Image Anal. 2021, 70, 101992. [Google Scholar] [CrossRef]
- Qiu, Y.; Liu, Y.; Xu, J. MiniSeg: An Extremely Minimum Network for Efficient COVID-19 Segmentation. Proc. AAAI Conf. Artif. Intell. 2020, 35, 4846–4854. [Google Scholar]
- Soares, E.A.; Angelov, P.P.; Biaso, S.; Froes, M.H.; Abe, D.K. SARS-CoV-2 CT-scan dataset:A large dataset of real patients CT scans for SARS-CoV-2 identification. medRxiv 2020. [Google Scholar] [CrossRef]
- Yang, X.; Zhao, J.; Zhang, Y.; He, X.; Xie, P. COVID-CT-Dataset: A CT Scan Dataset about COVID-19. arXiv 2020, arXiv:2003.13865. [Google Scholar]
- Ning, W.; Lei, S.; Yang, J.; Cao, Y.; Jiang, P.; Yang, Q.; Zhang, J.; Wang, X.; Chen, F.H.; Geng, Z.; et al. iCTCF: An integrative resource of chest computed tomography images and clinical features of patients with COVID-19 pneumonia. Res. Square 2020. [Google Scholar] [CrossRef] [Green Version]
- Maftouni, M.; Law, A.C.C.; Shen, B.; Zhou, Y.; Ayoobi Yazdi, N.; Kong, Z. A Robust Ensemble-Deep Learning Model for COVID-19 Diagnosis based on an Integrated CT Scan Images Database. In IIE Annual Conference; Ayoobi Yazdi, N.; Institute of Industrial and Systems Engineers (IISE): Norcross, Georgia, 2021; pp. 632–637. [Google Scholar]
- Covid-19-Detection-X-ray-Dataset. Available online: https://www.kaggle.com/darshan1504/covid19-detection-xray-dataset (accessed on 5 March 2022).
- Alqudah, A.M. Augmented COVID-19 X-ray Images Dataset. 2020. Available online: https://data.mendeley.com/datasets/2fxz4px6d8/4 (accessed on 5 March 2022).
- Cohen, J.P.; Morrison, P.; Dao, L. COVID-19 Image Data Collection. arXiv 2020, arXiv:2003.11597. [Google Scholar]
- COVID-19 CT Lung and Infection Segmentation Dataset. Available online: https://zenodo.org/record/3757476 (accessed on 6 March 2022).
- COVID-19 CT Segmentation Dataset. 2020. Available online: http://medicalsegmentation.com/covid19/ (accessed on 5 March 2022).
- Morozov, S.P.; Andreychenko, A.E.; Pavlov, N.A.; Vladzymyrskyy, A.V.; Ledikhova, N.V.; Gombolevsky, V.A.; Blokhin, I.A.; Gelezhe, P.B.; Gonchar, A.V.; Chernina, V.Y. MosMedData: Chest CT Scans with COVID-19 Related Findings. arXiv 2020, arXiv:2005.06465. [Google Scholar]
- Tabik, S.; G’omez-R’ios, A.; Mart’in-Rodr’iguez, J.L.; Sevillano-Garc’ia, I.; Rey-Area, M.; Charte, D.; Guirado, E.; Su’arez, J.L.; Luengo, J.; Valero-Gonz’alez, M.A.; et al. COVIDGR Dataset and COVID-SDNet Methodology for Predicting COVID-19 Based on Chest X-ray Images. IEEE J. Biomed. Health Inform. 2020, 24, 3595–3605. [Google Scholar] [CrossRef] [PubMed]
- De la Iglesia-Vayá, M.; Saborit, J.M.; Montell, J.A.; Pertusa, A.; Bustos, A.; Cazorla, M.; Galant, J.; Barber, X.; Orozco-Beltrán, D.; García-García, F.; et al. BIMCV COVID-19+: A large annotated dataset of RX and CT images from COVID-19 patients. arXiv 2020, arXiv:2006.01174. [Google Scholar]
- Deng, J.; Dong, W.; Socher, R.; Li, L.; Li, K.; Fei-Fei, L. ImageNet: A large-scale hierarchical image database. In Proceedings of the 2009 IEEE Computer Society Conference on Computer Vision and Pattern Recognition (CVPR 2009), Miami, FL, USA, 20–25 June 2009; pp. 248–255. [Google Scholar] [CrossRef] [Green Version]
- Lin, T.; Maire, M.; Belongie, S.J.; Hays, J.; Perona, P.; Ramanan, D.; Dollár, P.; Zitnick, C.L. Microsoft COCO: Common Objects in Context. In Proceedings of the Computer Vision-ECCV 2014—13th European Conference, Proceedings, Part V. Zurich, Switzerland, 6–12 September 2014; Fleet, D.J., Pajdla, T., Schiele, B., Tuytelaars, T., Eds.; Springer: Berlin/Heidelberg, Germany, 2014; Volume 8693, pp. 740–755. [Google Scholar] [CrossRef] [Green Version]
- Cordts, M.; Omran, M.; Ramos, S.; Rehfeld, T.; Enzweiler, M.; Benenson, R.; Franke, U.; Roth, S.; Schiele, B. The Cityscapes Dataset for Semantic Urban Scene Understanding. In Proceedings of the 2016 IEEE Conference on Computer Vision and Pattern Recognition, CVPR 2016, Las Vegas, NV, USA, 27–30 June 2016; pp. 3213–3223. [Google Scholar] [CrossRef] [Green Version]
- Wang, M.; Deng, W. Deep Visual Domain Adaptation: A Survey. Neurocomputing 2018, 312, 135–153. [Google Scholar] [CrossRef] [Green Version]
- Selvaraju, R.R.; Das, A.; Vedantam, R.; Cogswell, M.; Parikh, D.; Batra, D. Grad-CAM: Why did you say that? arXiv 2016, arXiv:1611.07450. [Google Scholar]
- Basu, S.; Mitra, S.; Saha, N. Deep Learning for Screening COVID-19 using Chest X-ray Images. arXiv 2020, arXiv:2004.10507. [Google Scholar]



| Special Issue on | Submission Deadline | Journal | Publisher | Impact Factor |
|---|---|---|---|---|
| Artificial Intelligence and Information Technologies for COVID-19 | April 2020 | Computers, Materials & Continua | Tech Science | 3.772 |
| https://techscience.com/cmc/special_detail/COVID-19 | ||||
| Bioengineering Techniques and Applications Against COVID-19 | April 2020 | Bioengineering | MDPI | 4.673 |
| https://www.mdpi.com/journal/bioengineering/special_issues/against_COVID-19 | ||||
| Intelligent Analysis of COVID-19 Imaging Data | June 2020 | Medical Image Analysis | Elsevier | 19.116 |
| https://www.sciencedirect.com/journal/medical-image-analysis/special-issue/10W9DDB50B2 | ||||
| AI for COVID-19 | July 2020 | IEEE Transactions on Big Data | IEEE | 3.344 |
| https://www.computer.org/digital-library/journals/bd/call-for-papers-special-issue-on-ai-for-covid-19 | ||||
| Artificial Intelligence Techniques for COVID-19 Imaging Data—Recent Advances | January 2021 | Health Informatics Journal | SAGE | 2.681 |
| https://journals.sagepub.com/page/jhi/call-for-papers/special-collections/artificial-intelligence | ||||
| Deep Learning: AI Steps Up in Battle against COVID-19 | May 2021 | International Journal of Environmental Research and Public Health | MDPI | 3.531 |
| https://www.mdpi.com/journal/ijerph/special_issues/AI_against_COVID-19 | ||||
| AI and Data Science in COVID-19 | August 2021 | International Journal of Data Science and Analytics | Springer | 3.239 |
| https://www.springer.com/journal/41060/updates/19117582 | ||||
| Artificial Intelligence for COVID-19 Diagnosis | October 2021 | Diagnostics | MDPI | 3.24 |
| https://www.mdpi.com/journal/diagnostics/special_issues/AI_COVID-19 | ||||
| COVID-19: Diagnostic Imaging and Beyond | February 2022 | Journal of Clinical Medicine | MDPI | 4.242 |
| https://www.mdpi.com/journal/jcm/special_issues/COVID-19_Diagnostic_Imaging_and_Beyond | ||||
| Multidisciplinary Approaches to Manage COVID-19: From Surveillance to Diagnosis | February 2022 | Diagnostics | MDPI | 3.24 |
| https://www.mdpi.com/journal/diagnostics/special_issues/COVID_surveillance_diagnosis | ||||
| Artificial Intelligence Computing and Applications for COVID-19 | March 2022 | Applied Sciences | MDPI | 2.679 |
| https://www.mdpi.com/journal/applsci/special_issues/Computing_and_Applications_for_COVID_19 | ||||
| Surveillance Strategies and Diagnostic Procedures: Integrated Approaches to Manage the COVID-19 Outbreak | April 2022 | Diagnostics | MDPI | 3.24 |
| https://www.mdpi.com/journal/diagnostics/special_issues/COVID-19_diagnostic_strategies | ||||
| COVID-19 | No submission deadline | Healthcare Informatics Research | Springer | 3.261 |
| https://www.springer.com/journal/41666/updates/17947710 | ||||
| Reference | Date | Covered Methods | Covered Datasets |
|---|---|---|---|
| Systematic review and critical appraisal of prediction models for diagnosis and prognosis of COVID-19 infection [3] | March 2020 | 6 | - |
| Mapping the landscape of artificial intelligence applications against COVID-19 [13] | March 2020 | 6 | - |
| Artificial Intelligence in the Battle against Coronavirus (COVID-19): A Survey and Future Research Directions [14] | April 2020 | 12 | - |
| Detection of Covid-19 From Chest X-ray Images Using Artificial Intelligence: An Early Review [15] | April 2020 | 5 | - |
| The Role of Imaging in the Detection and Management of COVID-19: A Review [16] | April 2020 | 23 | - |
| Novel coronavirus (COVID-19) diagnosis using computer vision and artificial intelligence techniques: a review [17] | June 2020 | 21 | 7 |
| A Survey on the Use of AI and ML for Fighting the COVID-19 Pandemic [18] | August 2020 | 35 | - |
| Sonographic Diagnosis of COVID-19: A Review of Image Processing for Lung Ultrasound [19] | September 2020 | 12 | - |
| Survey of the Detection and Classification of Pulmonary Lesions via CT and X-ray [20] | December 2020 | 39 | 26 |
| Medical imaging and computational image analysis in COVID-19 diagnosis: A review [21] | June 2021 | 51 | - |
| Deep neural networks for COVID-19 detection and diagnosis using images and acoustic-based techniques: a recent review [22] | August 2021 | 27 | 10 |
| Diagnosis of COVID-19 Using Machine Learning and Deep Learning: A review [23] | October 2021 | 52 | - |
| (Ours) Let AI Perform Better Next Time—A Systematic Review of Medical Imaging-based Automated Diagnosis of COVID-19: 2020–2022 | April 2022 | 179 | 15 |
| Paper | Rotating or Flipping | Scaling or Cropping | Brightness Adjusting | Contrast Adjusting |
|---|---|---|---|---|
| [47,49,52,61,62,63,64,65,66,67,68,69,70,71] | √ | - | - | - |
| [40,42,43,44,50,53,72,73,74,75,76,77,78,79,80] | √ | √ | - | - |
| [45,51,81] | √ | √ | √ | - |
| [41,82] | √ | √ | √ | √ |
| [54,56,83,84,85,86,87,88,89] | - | √ | - | - |
| [90,91] | - | √ | - | √ |
| [92] | √ | - | √ | √ |
| [48] | √ | √ | - | √ |
| [46,79,93,94] | - | - | - | √ |
| Total | 36 | 32 | 6 | 10 |
| CNN Structure | Paper | Total |
|---|---|---|
| ResNet [37] | [40,42,43,49,51,53,55,56,57,62,63,67,70,75,77,83,84,87,92,94,95,96,98,107,108,109,110,111,112,113,114,115,116,117,118,119,120,121,122,123,124,125,126,127,128,129,130,131,132,133,134,135,135] | 54 |
| GoogLeNet [100] | [1,42,48,57,109,111,112,121,124,125,126,127,136,137,138] | 18 |
| DenseNet [101] | [43,49,51,52,55,65,67,70,73,86,95,96,98,108,111,119,120,124,125,126,132,133,134,137,139,140,141,142,143] | 29 |
| VGG [102] | [55,62,75,82,83,84,94,95,108,109,111,118,119,122,124,126,129,131,133,134,136,137,144,145,146,147,148,149] | 28 |
| MobileNet [103] | [51,55,74,83,84,111,119,125,134,136,137,139,150] | 13 |
| SqueezeNet [104] | [43,49,50,57,83,84,109] | 7 |
| AlexNet [105] | [43,57,83,84,85,94,109,127,148,151,152,153,154] | 13 |
| Capsule [106] | [44,58,73] | 3 |
| [99,107,115,154,186] | [68,108,153,187,187] | [44,48,52,74,93,95,114,116,118,122,124,133,155,174,175,176] | [87,92,117,141] | [55,70,75,79,82,136,139,144,160,188,189,79] | [1,190] | [151,162,191] | [41,57,66,69,76,79,84,86,94,110,134,135,142,149,177,178,179,180,181,182,183,184] | |
|---|---|---|---|---|---|---|---|---|
| COVID-19 | √ | √ | √ | √ | √ | √ | √ | √ |
| Normal | √ | √ | √ | √ | √ | - | - | - |
| VP | √ | - | √ | - | - | √ | - | - |
| BP | - | √ | √ | - | - | - | - | - |
| CAP | - | - | - | √ | - | - | √ | - |
| NCP | - | - | - | - | √ | - | - | √ |
| Total | 5 | 5 | 16 | 4 | 12 | 2 | 3 | 23 |
| Dataset | Modality | #COVID-19 | #Total | Size | Format |
|---|---|---|---|---|---|
| SARS-CoV-2 CT-scan dataset | CT | 1252 | 2482 | 242 MB | PNG |
| COVID-CT-Dataset | CT | 349 | 749 | 474 MB | JPG |
| COVID-CTset | CT | 15,589 | 63,849 | 61.6 GB | DICOM |
| CT Scans for COVID-19 Classification | CT | 4001 | 39,370 | 3.68 GB | JPG |
| Large COVID-19 CT scan slice dataset | CT | 7593 | 17,104 | 2.12 GB | PNG |
| COVIDx Dataset | X-ray | 18,490 | 30,882 | 12.9 GB | PNG |
| COVID-19 Radiography Database | X-ray | 3616 | 21,165 | 744 MB | PNG |
| COVID-19 Detection X-ray Dataset | X-ray | 129 | 5073 | 188 MB | JPEG |
| Augmented COVID-19 X-ray Images | X-ray | 878 | 3532 | 173 MB | PNG |
| Covid-Chestxray-Dataset | CT + X-ray | 563 | 930 | 529 MB | JPG |
| Dataset | Modality | #COVID-19 | #Total | Size | Format |
|---|---|---|---|---|---|
| COVID-19 CT Lung and Infection Segmentation | CT | - | - | 1.05 GB | - |
| COVID-19 CT Segmentation Dataset | CT | 110 | 110 | 367 MB | JPG |
| MOSMEDDATA | CT | - | 1110 | - | NIFTI |
| COVIDGR Dataset | X-ray | 426 | 852 | 949 MB | JPG |
| BIMCV COVID-19+ | CT + X-ray | - | 23,527 | 389.27 GB | MIDS |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liu, F.; Chen, D.; Zhou, X.; Dai, W.; Xu, F. Let AI Perform Better Next Time—A Systematic Review of Medical Imaging-Based Automated Diagnosis of COVID-19: 2020–2022. Appl. Sci. 2022, 12, 3895. https://doi.org/10.3390/app12083895
Liu F, Chen D, Zhou X, Dai W, Xu F. Let AI Perform Better Next Time—A Systematic Review of Medical Imaging-Based Automated Diagnosis of COVID-19: 2020–2022. Applied Sciences. 2022; 12(8):3895. https://doi.org/10.3390/app12083895
Chicago/Turabian StyleLiu, Fan, Delong Chen, Xiaocong Zhou, Wenwen Dai, and Feng Xu. 2022. "Let AI Perform Better Next Time—A Systematic Review of Medical Imaging-Based Automated Diagnosis of COVID-19: 2020–2022" Applied Sciences 12, no. 8: 3895. https://doi.org/10.3390/app12083895
APA StyleLiu, F., Chen, D., Zhou, X., Dai, W., & Xu, F. (2022). Let AI Perform Better Next Time—A Systematic Review of Medical Imaging-Based Automated Diagnosis of COVID-19: 2020–2022. Applied Sciences, 12(8), 3895. https://doi.org/10.3390/app12083895







