Evaluation of the Predictability and Accuracy of Orthognathic Surgery in the Era of Virtual Surgical Planning
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patient Data Collection
2.2. Surgical Protocol
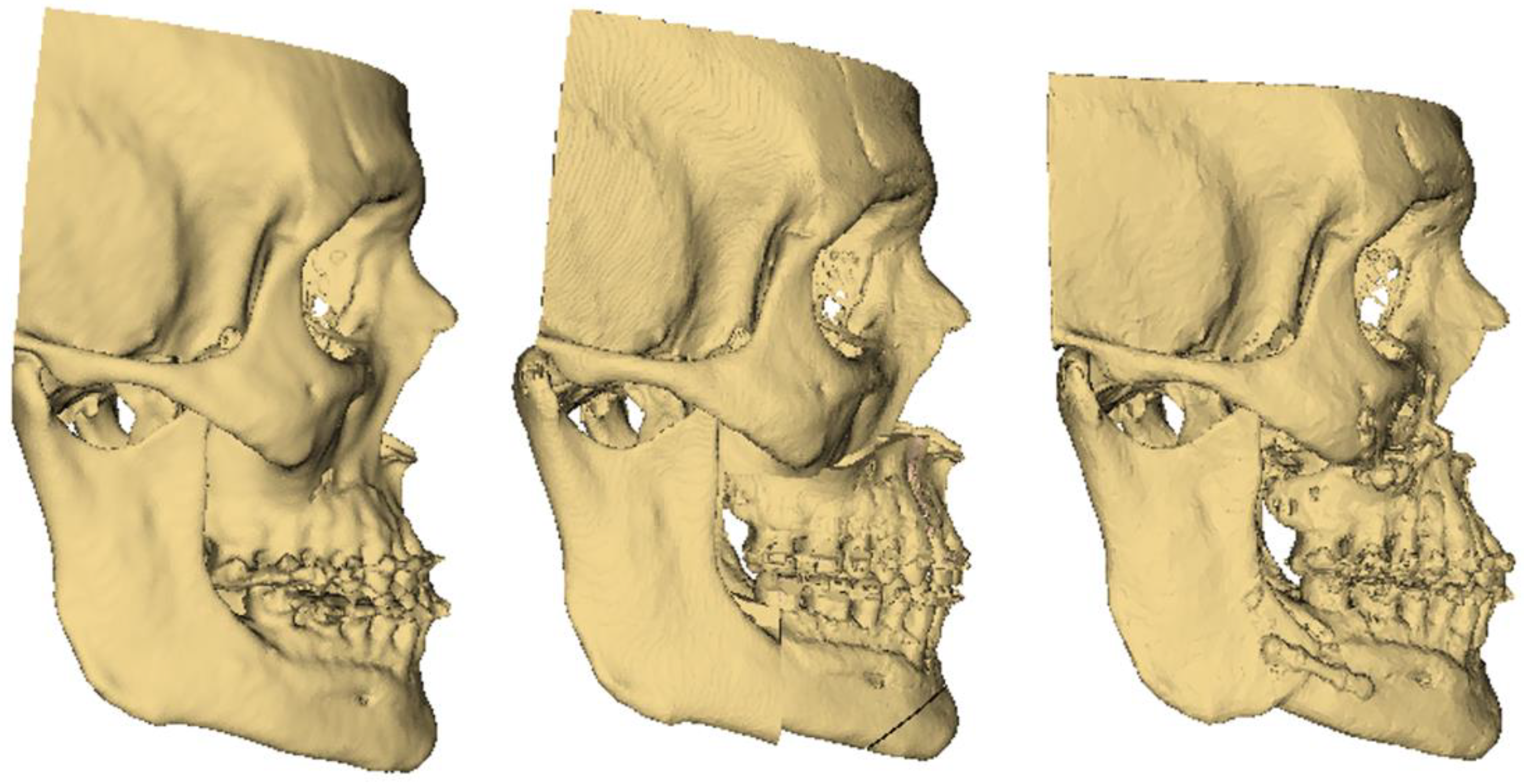
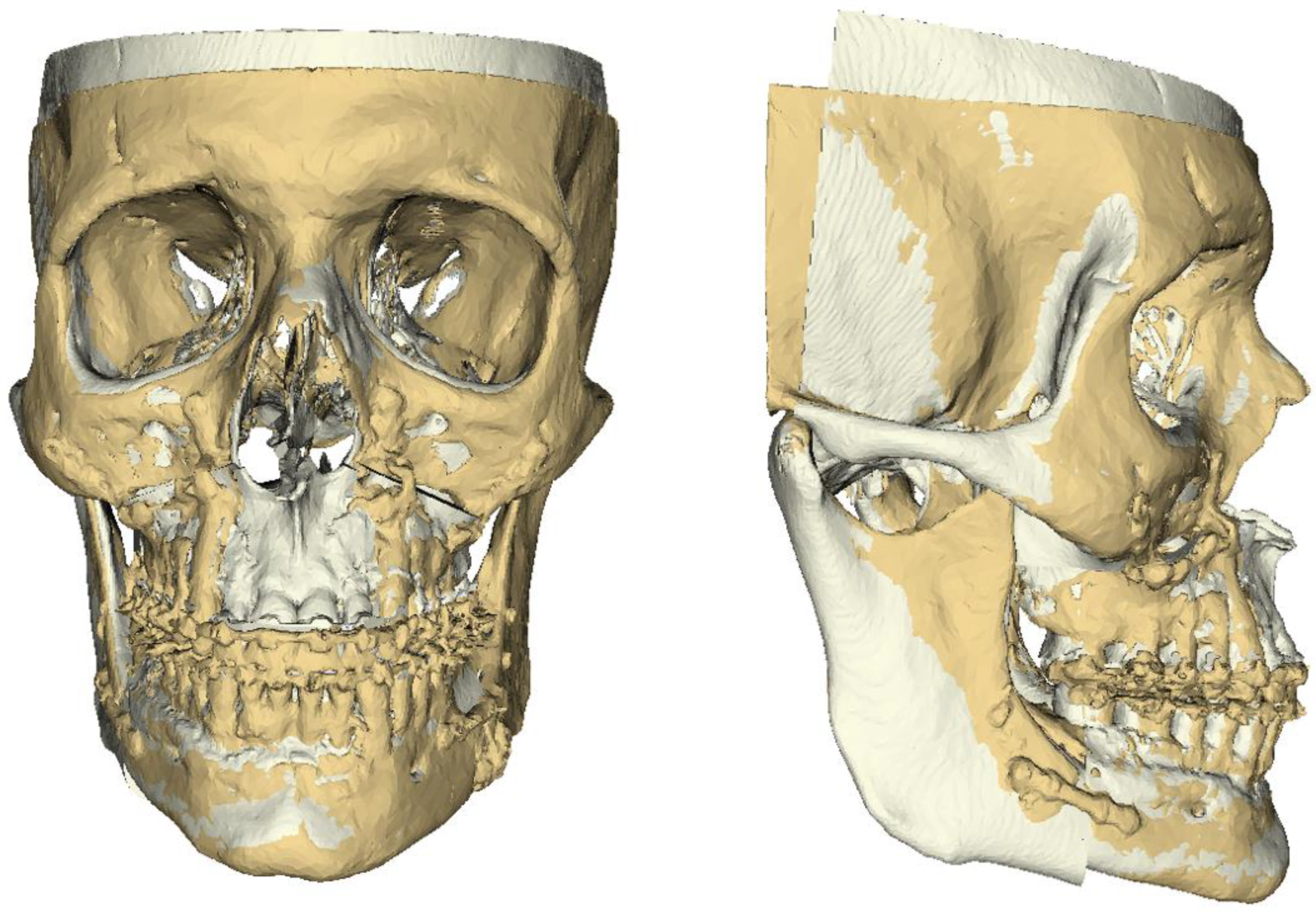
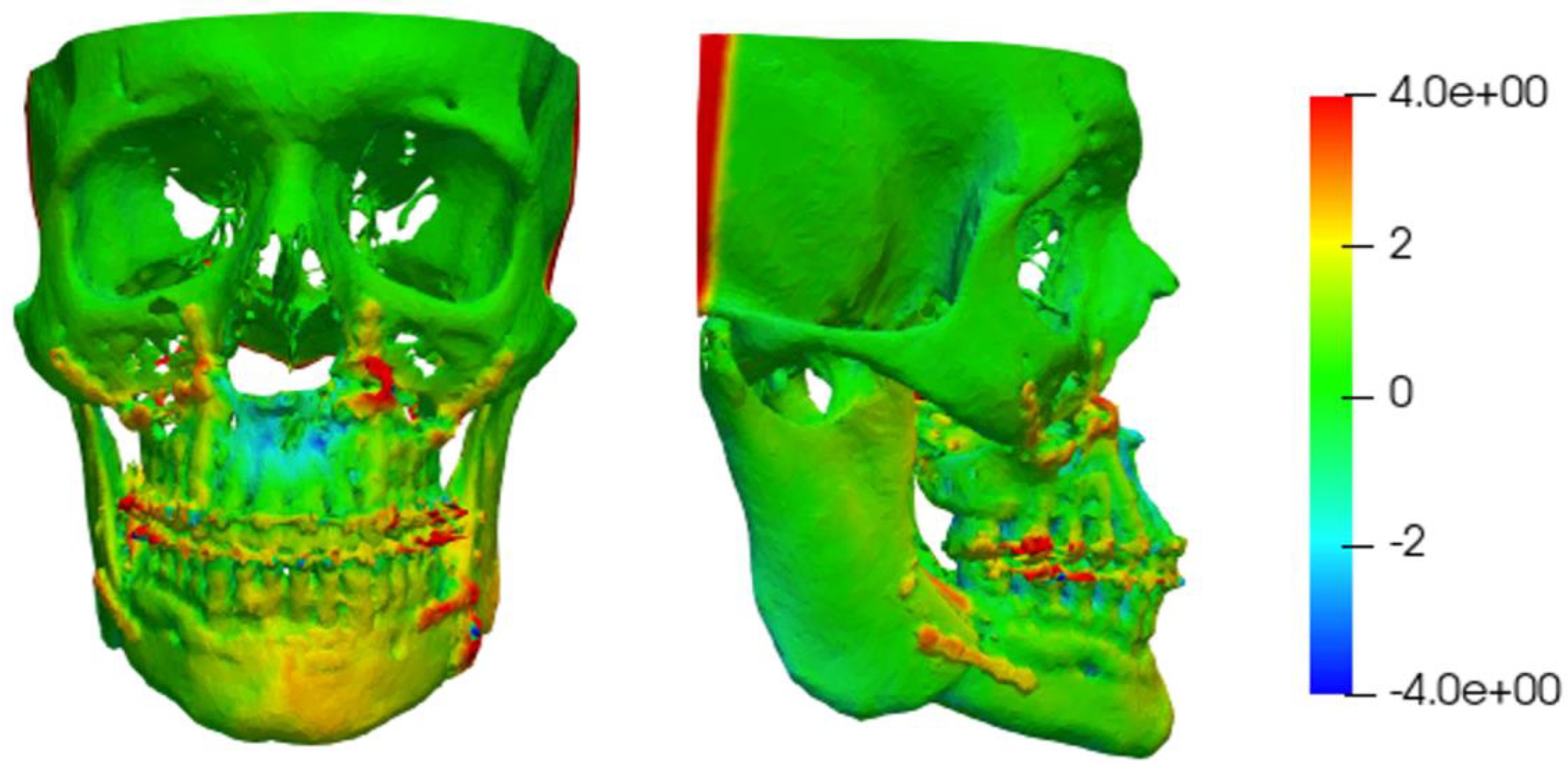
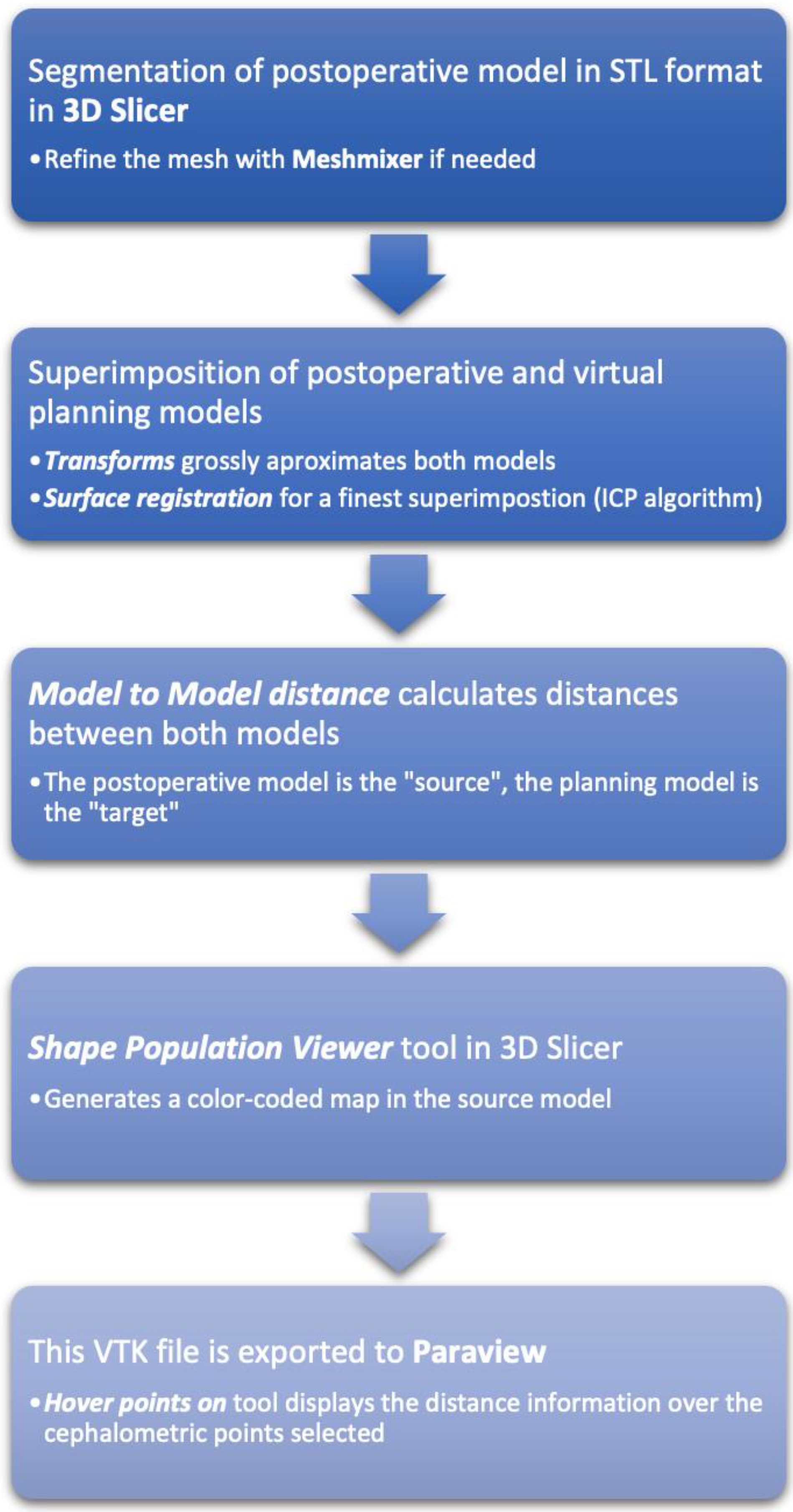
2.3. Distance Measurement
2.4. Statistical Analysis
2.5. Ethics Committee
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Quereshy, F.A.; Baur, D.A.; Levintov, N.; Altay, M.A.; Bazina, M. Role of Virtual Surgical Planning in Increased Predictability of Orthognathic Surgery. J. Oral Maxillofac. Surg. 2015, 73, e63–e64. [Google Scholar] [CrossRef]
- Seo, H.J.; Choi, H.J.Y.K. Current trends in orthognathic surgery. Curr. Trends Orthognath. Surg. 2021, 22, 287–295. [Google Scholar] [CrossRef] [PubMed]
- Lin, H.H.; Lonic, D.; Lo, L.J. 3D printing in orthognathic surgery—A literature review. J. Formos. Med. Assoc. 2018, 117, 547–558. [Google Scholar] [CrossRef] [PubMed]
- Stokbro, K.; Aagaard, E.; Torkov, P.; Bell, R.B.; Thygesen, T. Surgical accuracy of three-dimensional virtual planning: A pilot study of bimaxillary orthognathic procedures including maxillary segmentation. J. Oral Maxillofac. Surg. 2016, 45, 8–18. [Google Scholar] [CrossRef]
- Aboul-Hosn Centenero, S.; Hernández-Alfaro, F. 3D planning in orthognathic surgery: CAD/CAM surgical splints and prediction of the soft and hard tissues results—Our experience in 16 cases. J. Cranio-Maxillofac. Surg. 2012, 40, 162–168. [Google Scholar] [CrossRef]
- De Riu, G.; Virdis, P.I.; Meloni, S.M.; Lumbau, A.; Vaira, L.A. Accuracy of computer-assisted orthognathic surgery. J. Cranio-Maxillofac. Surg. 2018, 46, 293–298. [Google Scholar] [CrossRef]
- Baan, F.; Liebregts, J.; Xi, T.; Schreurs, R.; de Koning, M.; Bergé, S.; Maal, T. A new 3D tool for assessing the accuracy of bimaxillary surgery: The Ortho Gnathican Alyser. PLoS ONE 2016, 11, e0149625. [Google Scholar] [CrossRef] [Green Version]
- Hsu, S.S.-P.; Gateno, J.; Bell, R.B.; Hirsch, D.L.; Markiewicz, M.R.; Teichgraeber, J.F.; Zhou, X.; Xia, J.J. Accuracy of a Computer-Aided Surgical Simulation Protocol for Orthognathic Surgery: A Prospective Multicenter Study. J. Oral Maxillofac. Surg. 2013, 71, 128–142. [Google Scholar] [CrossRef] [Green Version]
- Xia, J.J.; Gateno, J.; Teichgraeber, J.F.; Christensen, A.M.; Lasky, R.E.; Lemoine, J.J.; Liebschner, M.A. Accuracy of the Computer-Aided Surgical Simulation (CASS) System in the Treatment of Patients with Complex Craniomaxillofacial Deformity: A Pilot Study. J. Oral Maxillofac. Surg. 2007, 65, 248–254. [Google Scholar] [CrossRef]
- Fedorov, A.; Beichel, R.; Kalpathy-Cramer, J.; Finet, J.; Fillion-Robin, J.-C.; Pujol, S.; Bauer, C.; Jennings, D.; Fennessy, F.; Sonka, M.; et al. 3D Slicer as an image computing platform for the Quantitative Imaging Network. Magn. Reson. Imaging 2012, 30, 1323–1341. [Google Scholar] [CrossRef] [Green Version]
- Wang, L.C.; Lee, Y.H.; Tsai, C.Y.; Wu, T.J.; Teng, Y.Y.; Lai, J.P.; Lin, S.S.; Chang, Y.J. Postsurgical Stability of Temporomandibular Joint of Skeletal Class III Patients Treated with 2-Jaw Orthognathic Surgery via Computer-Aided Three-Dimensional Simulation and Navigation in Orthognathic Surgery (CASNOS). BioMed Res. Int. 2021, 2021, 1563551. [Google Scholar] [CrossRef] [PubMed]
- Sendyk, M.; Cevidanes, L.; Ruellas, A.; Fattori, L.; Mendes, F.M.; Paiva, J.B.; Rino Neto, J. Three-dimensional evaluation of dental decompensation and mandibular symphysis remodeling on orthodontic-surgical treatment of Class III malocclusion. Am. J. Orthod. Dentofac. Orthop. 2021, 159, 175–183.e3. [Google Scholar] [CrossRef] [PubMed]
- McAllister, P.; Watson, M.; Burke, E. A Cost-Effective, In-House, Positioning and Cutting Guide System for Orthognathic Surgery. J. Maxillofac. Oral Surg. 2018, 17, 112–114. [Google Scholar] [CrossRef] [PubMed]
- Cevidanes, L.H.C.; Oliveira, A.E.F.; Grauer, D.; Styner, M.; Proffit, W.R. Clinical Application of 3D Imaging for Assessment of Treatment Outcomes. Semin. Orthod. 2011, 17, 72–80. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Marlière, D.A.A.; Demétrio, M.S.; Verner, F.S.; Asprino, L.; Netto, H.D.D.M.C. Feasibility of iterative closest point algorithm for accuracy between virtual surgical planning and orthognathic surgery outcomes. J. Cranio-Maxillofac. Surg. 2019, 47, 1031–1040. [Google Scholar] [CrossRef]
- Tucker, S.; Cevidanes, L.H.S.; Styner, M.; Kim, H.; Reyes, M.; Proffit, W.; Turvey, T. Comparison of actual surgical outcomes and 3-dimensional surgical simulations. J. Oral Maxillofac. Surg. 2010, 68, 2412–2421. [Google Scholar] [CrossRef] [Green Version]
- Ahrens, J.P.; Geveci, B.; Law, C.C. Paraview: An End-User Tool for Large Data Visualization; The Visualization Handbook; Hansen, C.D., Johnson, C.R., Eds.; Butterworth-Heinemann: Oxford, UK, 2005; pp. 717–731. Available online: https://www.sciencedirect.com/science/article/pii/B9780123875822500381?via%3Dihub (accessed on 17 March 2022).
- Baker, S.B.; Goldstein, J.A.; Seruya, M. Outcomes in Computer-Assisted Surgical Simulation for Orthognathic Surgery. J. Craniofac. Surg. 2012, 23, 509–513. [Google Scholar] [CrossRef]
- Swennen, G.R.J.; Mollemans, W.; Schutyser, F. Three-Dimensional Treatment Planning of Orthognathic Surgery in the Era of Virtual Imaging. J. Oral Maxillofac. Surg. 2009, 67, 2080–2092. [Google Scholar] [CrossRef]
- Tran, N.H.; Tantidhnazet, S.; Raocharernporn, S.; Kiattavornchareon, S.; Pairuchvej, V.; Wongsirichat, N. Accuracy of Three-Dimensional Planning in Surgery-First Orthognathic Surgery: Planning Versus Outcome. J. Clin. Med. Res. 2018, 10, 429–436. [Google Scholar] [CrossRef] [Green Version]
- Alcañiz, P.; Pérez, J.; Gutiérrez, A.; Barreiro, H.; Villalobos, Á.; Miraut, D.; Illana, C.; Guiñales, J.; Otaduy, M.A. Soft-Tissue Simulation for Computational Planning of Orthognathic Surgery. J. Pers. Med. 2021, 11, 982. [Google Scholar] [CrossRef] [PubMed]
- Hernandez-Alfaro, F.; Guijarro-Martinez, R. New protocol for threedimensional surgical planning and CAD/CAM splint generation in orthognathic surgery: An in vitro and in vivo study. Int. J. Oral Maxillofac. Surg. 2013, 42, 1547–1556. [Google Scholar] [CrossRef] [PubMed]
- Makram, M.; Kamel, H. Reeb graph for automatic 3D cephalometry. IJIP 2014, 8, 17–29. [Google Scholar]
- Zhang, N.; Liu, S.; Hu, Z.; Hu, J.; Zhu, S.; Li, Y. Accuracy of virtual surgical planning in two-jaw orthognathic surgery: Comparison of planned and actual results. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2016, 122, 143–151. [Google Scholar] [CrossRef]
- Cevidanes, L.H.S.; Bailey, L.J.; Tucker, G.R.; Styner, M.A.; Mol, A.; Phillips, C.L.; Proffit, W.R.; Turvey, T. Superimposition of 3D cone-beam CT models of orthognathic surgery patients. Dentomaxillofac. Radiol. 2005, 34, 369–375. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hajeer, M.Y.; Ayoub, A.F.; Millett, D.T.; Bock, M.; Siebert, J.P. Three-dimensional imaging in orthognathic surgery: The clinical application of a new method. Int. J. Adult Orthod. Orthognath. Surg. 2002, 17, 318–330. [Google Scholar]
- Kawamata, A.; Fujishita, M.; Nagahara, K.; Kanematu, N.; Niwa, K.; Langlais, R.P. Three-dimensional computed tomography evaluation of postsurgical condylar displacement after mandibular osteotomy. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 1998, 85, 371–376. [Google Scholar] [CrossRef]
- Lee, C.-Y.; Jang, C.-S.; Kim, J.-W.; Kim, J.-Y.; Yang, B.-E. Condylar repositioning using centric relation bite in bimaxillary surgery. Korean J. Orthod. 2013, 43, 74–82. [Google Scholar] [CrossRef] [Green Version]
- Alkhayer, A.; Piffkó, J.; Lippold, C.; Segatto, E. Accuracy of virtual planning in orthognathic surgery: A systematic review. Head Face Med. 2020, 16, 1–9. [Google Scholar] [CrossRef]
- Chin, S.J.; Wilde, F.; Neuhaus, M.; Schramm, A.; Gellrich, N.C.; Rana, M. Accuracy of virtual surgical planning of orthognathic surgery with aid of CAD/CAM fabricated surgical splint—A novel 3D analyzing algorithm. J. Cranio-Maxillofac. Surg. 2017, 45, 1962–1970. [Google Scholar] [CrossRef]
- Jabar, N.; Robinson, W.; Goto, T.K.; Khambay, B.S. The validity of using surface meshes for evaluation of three-dimensional maxillary and mandibular surgical changes. Int. J. Oral Maxillofac. Surg. 2015, 44, 914–920. [Google Scholar] [CrossRef]

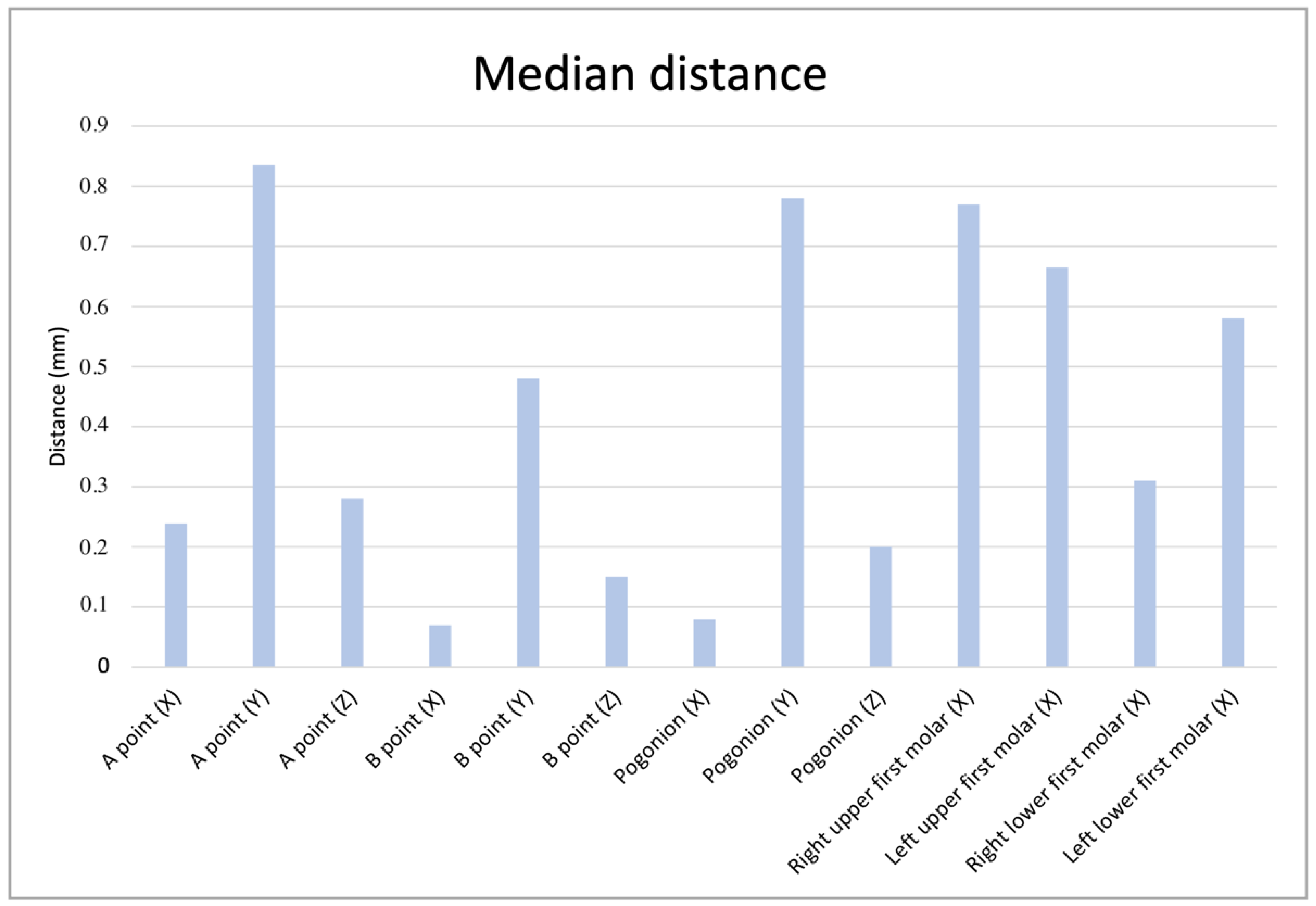

| Landmark (Measured Axis) | Percentile 25 (mm) | Median (mm) | Percentile 75 (mm) |
|---|---|---|---|
| A point (X) | 0.077 | 0.239 | 0.360 |
| A point (Y) | 0.297 | 0.835 | 0.400 |
| A point (Z) | 0.075 | 0.280 | 0.600 |
| B point (X) | 0.020 | 0.070 | 0.330 |
| B point (Y) | 0,162 | 0.480 | 0.885 |
| B point (Z) | 0.036 | 0.150 | 0.292 |
| Pogonion (X) | 0.013 | 0.079 | 0.190 |
| Pogonion (Y) | 0.175 | 0.780 | 1.160 |
| Pogonion (Z) | 0.070 | 0.200 | 0.625 |
| Right upper first molar (X) | 0.257 | 0.770 | 1.445 |
| Left upper first molar (X) | 0.186 | 0.665 | 1.222 |
| Right lower first molar (X) | 0.100 | 0.310 | 0.370 |
| Left lower first molar (X) | 0.150 | 0.580 | 0.850 |
| Landmark (3D Absolute Measure) | Percentile 25 (mm) | Median (mm) | Percentile 75 (mm) |
|---|---|---|---|
| A point | 0.344 | 0.934 | 1.719 |
| B point | 0.367 | 0.613 | 1.107 |
| Pog | 0.405 | 1.034 | 1.513 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pampín Martínez, M.M.; Gutiérrez Venturini, A.; Guiñales Díaz de Cevallos, J.; Barajas Blanco, M.; Aragón Niño, I.; Moreiras Sánchez, A.; del Castillo Pardo de Vera, J.L.; Cebrián Carretero, J.L. Evaluation of the Predictability and Accuracy of Orthognathic Surgery in the Era of Virtual Surgical Planning. Appl. Sci. 2022, 12, 4305. https://doi.org/10.3390/app12094305
Pampín Martínez MM, Gutiérrez Venturini A, Guiñales Díaz de Cevallos J, Barajas Blanco M, Aragón Niño I, Moreiras Sánchez A, del Castillo Pardo de Vera JL, Cebrián Carretero JL. Evaluation of the Predictability and Accuracy of Orthognathic Surgery in the Era of Virtual Surgical Planning. Applied Sciences. 2022; 12(9):4305. https://doi.org/10.3390/app12094305
Chicago/Turabian StylePampín Martínez, Marta María, Alessandro Gutiérrez Venturini, Jorge Guiñales Díaz de Cevallos, María Barajas Blanco, Iñigo Aragón Niño, Alvaro Moreiras Sánchez, José Luis del Castillo Pardo de Vera, and José Luis Cebrián Carretero. 2022. "Evaluation of the Predictability and Accuracy of Orthognathic Surgery in the Era of Virtual Surgical Planning" Applied Sciences 12, no. 9: 4305. https://doi.org/10.3390/app12094305
APA StylePampín Martínez, M. M., Gutiérrez Venturini, A., Guiñales Díaz de Cevallos, J., Barajas Blanco, M., Aragón Niño, I., Moreiras Sánchez, A., del Castillo Pardo de Vera, J. L., & Cebrián Carretero, J. L. (2022). Evaluation of the Predictability and Accuracy of Orthognathic Surgery in the Era of Virtual Surgical Planning. Applied Sciences, 12(9), 4305. https://doi.org/10.3390/app12094305








