One-Jaw versus Two-Jaw Orthognathic Surgery for Patients with Cleft: A Comparative Study Using 3D Imaging Virtual Surgical Planning
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patient Selection
2.2. Surgical Simulation
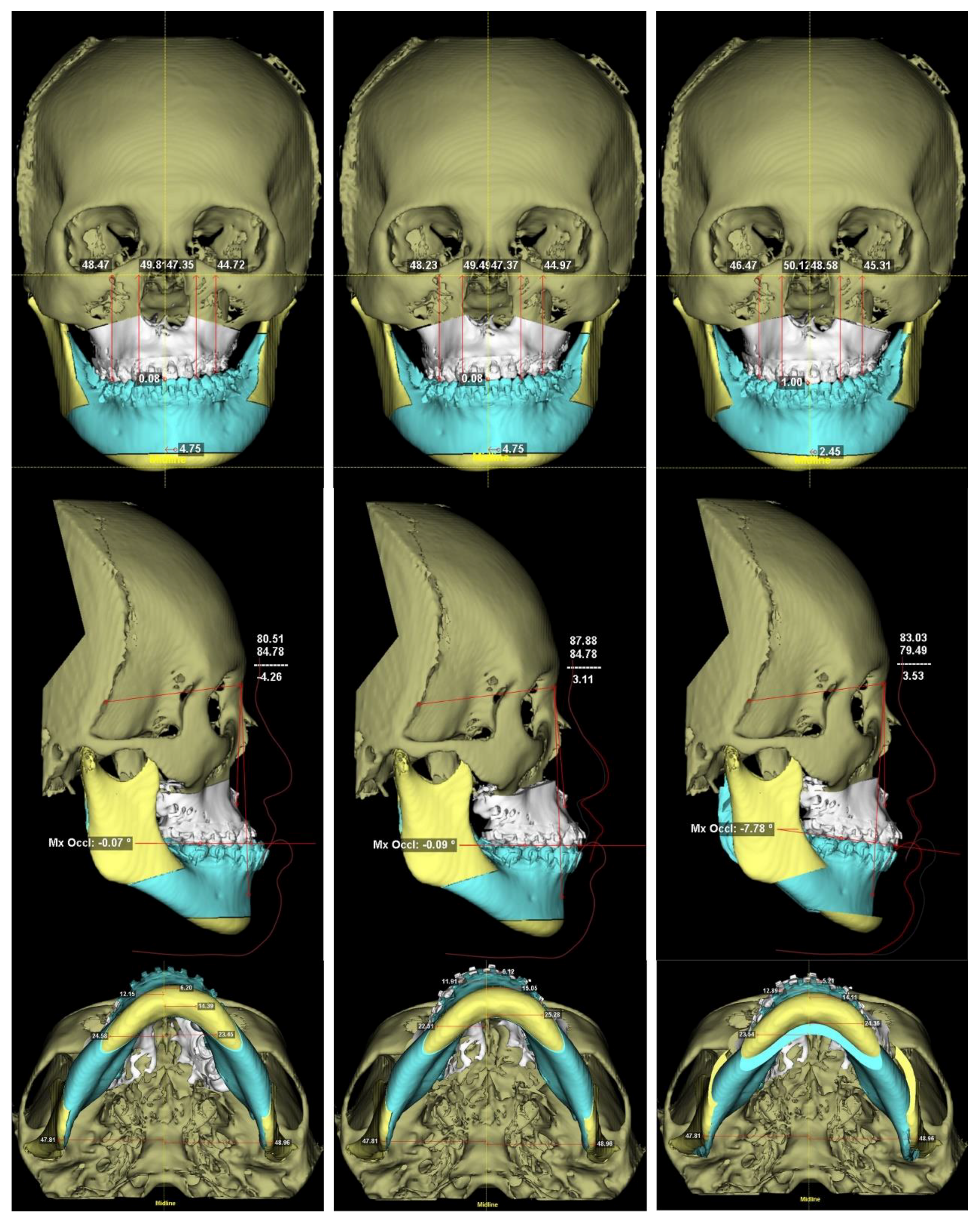
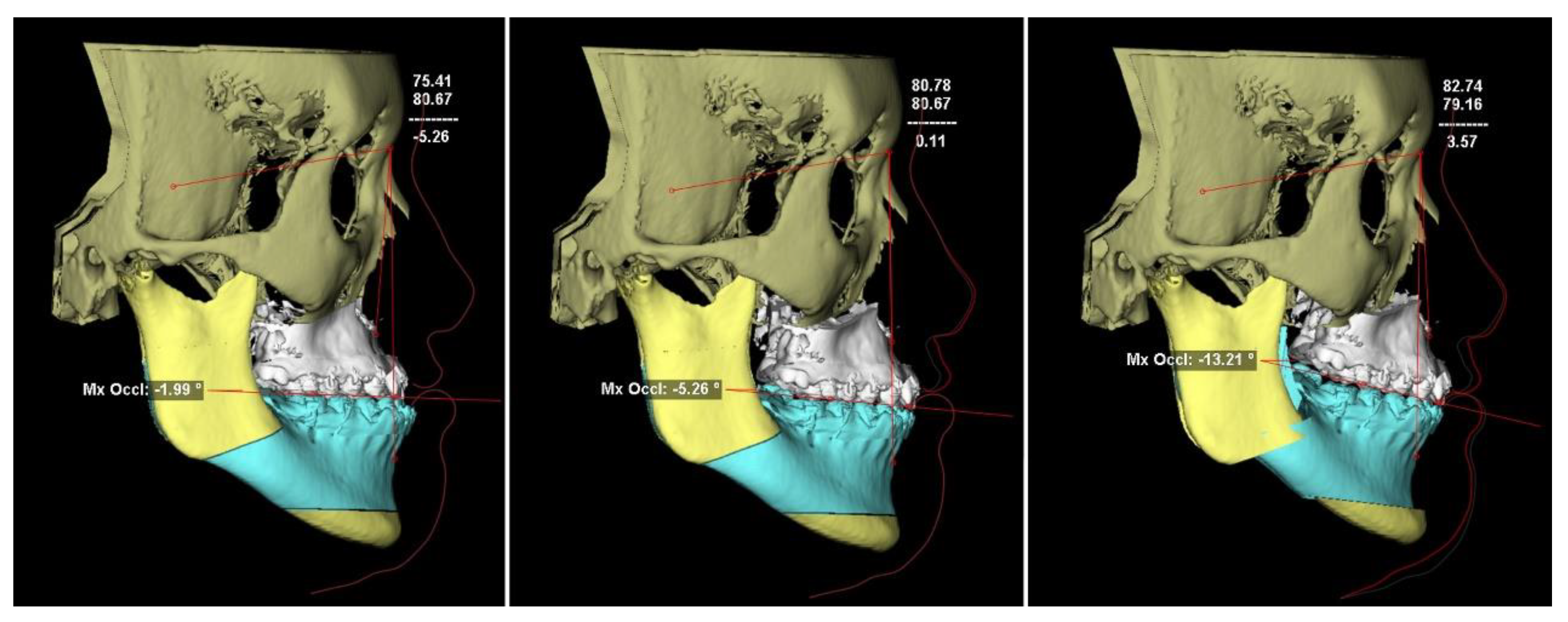
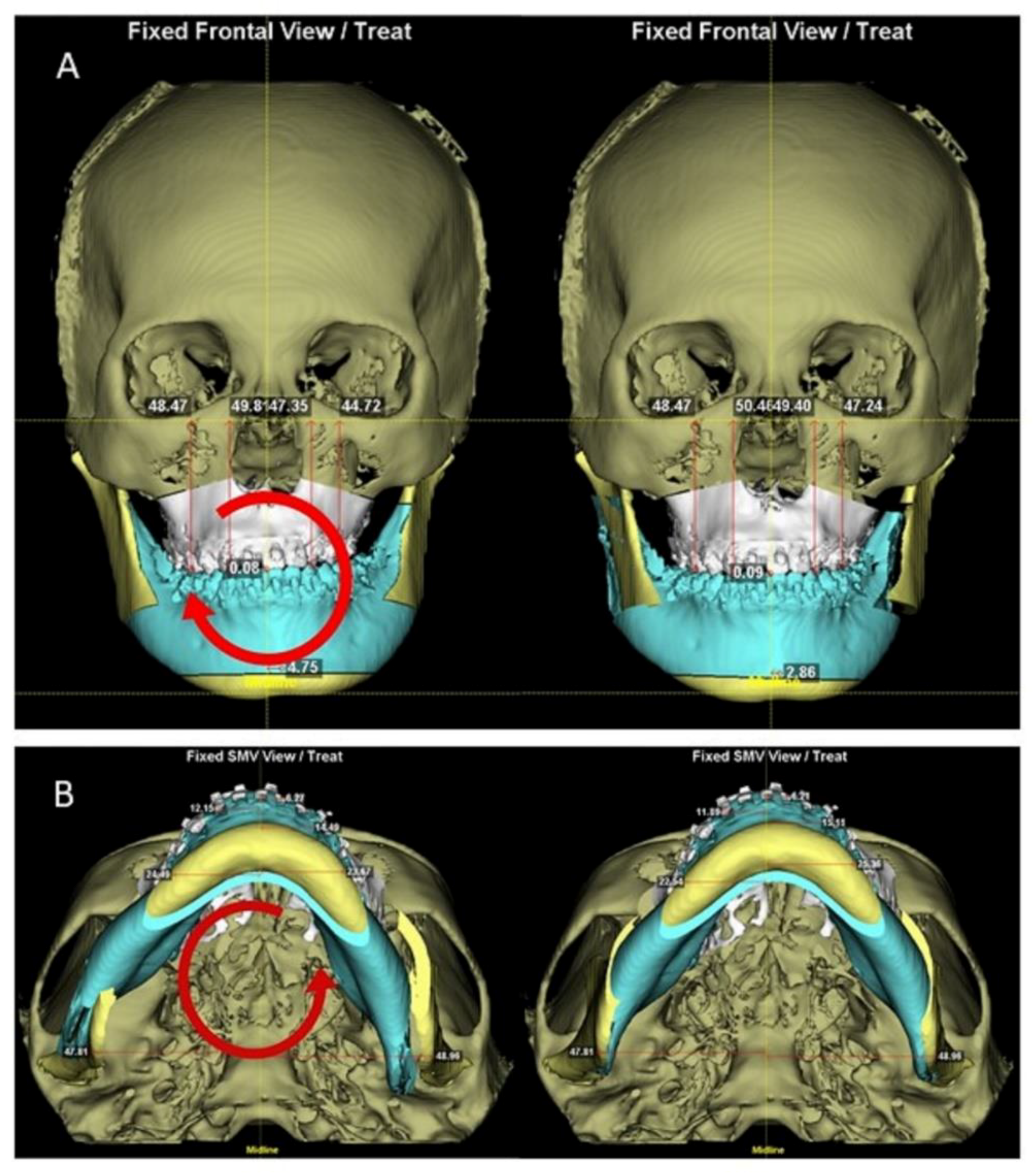
2.3. Two-Jaw Surgical Simulation
2.4. One-Jaw Surgical Simulation
2.5. The 3D Cephalometric Measurement
2.6. Asymmetry Index (ASI)
2.7. Statistical Analysis
3. Results
3.1. The 3D Cephalometric Measurements of T0 Stage
3.2. Comparisons between One-Jaw and Two-Jaw Designs
3.3. Larger versus Regular Maxillary Advancement in the One-Jaw Simulation
3.4. Asymmetry Index
4. Discussion
| Author Year | Country | Patient Number | One-Jaw Surgery (LeFort I) | Two-Jaw Surgery |
|---|---|---|---|---|
| Posnick et al., 1996 [45] | USA | 116 | 72.4% | 27.6% |
| Iannetti et al., 2004 [46] | Italy | 93 | 40.0% | 60.0% |
| Chong et al., 2009 [47] | USA | 103 | 50.5% | 49.5% |
| Broome et al., 2010 [48] | Switzerland | 58 | 84.5% | 15.5% |
| Watts et al., 2014 [49] | Canada | 30 | 46.7% | 53.3% |
| Fahradyan et al., 2018 [50] | USA | 136 | 46.3% | 53.7% |
| Impieri et al., 2018 [51] | Norway | 47 | 63.8% | 36.2% |
| Marion et al., 2019 [52] | France | 54 | 68.5% | 31.5% |
| Yatabe-Ioshida et al., 2019 [44] | Brazil | 9 | 22.2% | 77.8% |
| Chung et al., 2019 [53] | Korea | 44 | 0% | 100% |
| Hwang et al., 2019 [22] | Korea | 17 | 0% | 100% |
| Harjunpää et al., 2019 [54] | Finland | 93 | 74.2% | 25.8% |
| Wang et al., 2020 [55] | China | 90 | 52.2% | 47.8% |
| Wangsrimongkol et al., 2021 [56] | USA | 73 | 88.0% | 12.0% |
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Derijcke, A.; Eerens, A.; Carels, C. The incidence of oral clefts: A review. Br. J. Oral Maxillofac. Surg. 1996, 34, 488–494. [Google Scholar] [CrossRef]
- Chang, W.-J.; See, L.-C.; Lo, L.-J. Time trend of incidence rates of cleft lip/palate in Taiwan from 1994 to 2013. Biomed. J. 2016, 39, 150–154. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ross, R.B. Treatment variables affecting facial growth in complete unilateral cleft lip and palate. Cleft Palate J. 1987, 24, 5–77. [Google Scholar] [PubMed]
- DeLuke, D.M.; Marchand, A.; Robles, E.C.; Fox, P. Facial growth and the need for orthognathic surgery after cleft palate repair: Literature review and report of 28 cases. J. Oral Maxillofac. Surg. 1997, 55, 694–697. [Google Scholar] [CrossRef]
- Daskalogiannakis, J.; Mehta, M. The Need for Orthognathic Surgery in Patients with Repaired Complete Unilateral and Complete Bilateral Cleft Lip and Palate. Cleft Palate-Craniofacial J. 2009, 46, 498–502. [Google Scholar] [CrossRef]
- Oberoi, S.; Hoffman, W.Y.; Chigurupati, R.; Vargervik, K. Frequency of Surgical Correction for Maxillary Hypoplasia in Cleft Lip and Palate. J. Craniofacial Surg. 2012, 23, 1665–1667. [Google Scholar] [CrossRef]
- Dalle Ore, C.; Schoenbrunner, A.; Brandel, M.; Kronstadt, N.; McIntyre, J.; Jones, M.; Gosman, A. Incidence of Le Fort Surgery in a Mature Cohort of Patients With Cleft Lip and Palate. Ann. Plast. Surg. 2017, 78 (Suppl. S4), S199–S203. [Google Scholar] [CrossRef]
- Pai, B.C.J.; Hung, Y.T.; Wang, R.S.H.; Lo, L.J. Outcome of patients with complete unilateral cleft lip and palate: 20-year follow-up of a treatment protocol. Plast. Reconstr. Surg. 2019, 143, 359e–367e. [Google Scholar] [CrossRef]
- Phillips, J.H.; Nish, I.; Daskalogiannakis, J. Orthognathic Surgery in Cleft Patients. Plast. Reconstr. Surg. 2012, 129, 535e–548e. [Google Scholar] [CrossRef]
- James, J.N.; Costello, B.J.; Ruiz, R.L. Management of Cleft Lip and Palate and Cleft Orthognathic Considerations. Oral Maxillofac. Surg. Clin. N. Am. 2014, 26, 565–572. [Google Scholar] [CrossRef]
- Wong, F.; Heggie, A.; Shand, J.; Schneider, P. Skeletal stability of maxillary advancement with and without a mandibular reduction in the cleft lip and palate patient. Int. J. Oral Maxillofac. Surg. 2016, 45, 1501–1507. [Google Scholar] [CrossRef] [PubMed]
- Roy, A.-A.; Rtshiladze, M.A.; Stevens, K.; Phillips, J. Orthognathic Surgery for Patients with Cleft Lip and Palate. Clin. Plast. Surg. 2019, 46, 157–171. [Google Scholar] [CrossRef]
- Denadai, R.; Chou, P.Y.; Pai, B.C.; Chen, C.; Lin, C.C.H.; Huang, C.S.; Chen, Y.R.; Lo, L.J. Skeletofacial reconstruction for cleft-related deformities: Four decades of evolving cleft care. Ann. Plast. Surg. 2020, 85, 3–11. [Google Scholar] [CrossRef] [PubMed]
- Ho, C.T.; Lin, H.H.; Lo, L.J. Intraoral scanning and setting up the digital final occlusion in three-dimensional planning of orthognathic surgery: Its comparison with the dental model approach. Plast. Reconstr. Surg. 2019, 143, 1027e–1036e. [Google Scholar] [CrossRef]
- Seo, H.J.; Denadai, R.; Pai, B.C.-J.; Lo, L.-J. Modern Surgery-First Approach Concept in Cleft-Orthognathic Surgery: A Comparative Cohort Study with 3D Quantitative Analysis of Surgical-Occlusion Setup. J. Clin. Med. 2019, 8, 2116. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Denadai, R.; Chen, Y.-R.; Lo, L.-J. Three-Dimensional Computer-Assisted Single-Splint 2-Jaw Cleft Orthognathic Surgery: Toward Patient-Centered Surgical Rationale. Cleft Palate-Craniofacial J. 2020, 57, 1428–1433. [Google Scholar] [CrossRef]
- Wang, R.H.; Ho, C.-T.; Lin, H.-H.; Lo, L.-J. Three-dimensional cephalometry for orthognathic planning: Normative data and analyses. J. Formos. Med. Assoc. 2020, 119 Pt 2, 191–203. [Google Scholar] [CrossRef]
- Habets, L.L.M.H.; Bezuur, J.N.; Naeiji, M.; Hansson, T.L. The Orthopantomogram, an aid in diagnosis of temporomandibular joint problems. II. The vertical symmetry. J. Oral Rehabil. 1988, 15, 465–471. [Google Scholar] [CrossRef]
- Katsumata, A.; Fujishita, M.; Maeda, M.; Ariji, Y.; Ariji, E.; Langlais, R.P. 3D-CT evaluation of facial asymmetry. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2005, 99, 212–220. [Google Scholar] [CrossRef]
- Patel, D.S.; Jacobson, R.; Duan, Y.; Zhao, L.; Morris, D.; Cohen, M.N. Cleft skeletal asymmetry: Asymmetry index, classification and application. Cleft Palate-Craniofacial J. 2018, 55, 348–355. [Google Scholar] [CrossRef]
- Hochban, W.; Ganß, C.; Austermann, K.H. Long-term results after maxillary advancement in patients with clefts. Cleft Palate-Craniofacial J. 1993, 30, 237–243. [Google Scholar] [CrossRef] [PubMed]
- Hwang, D.; Choi, H.S.; Kim, U.K.; Song, J.-M. Complications Following Orthognathic Surgery for Patients with Cleft Lip/Palate. J. Craniofacial Surg. 2019, 30, 1815–1819. [Google Scholar] [CrossRef] [PubMed]
- Polley, J.W.; Figueroa, A.A. Management of Severe Maxillary Deficiency in Childhood and Adolescence through Distraction Osteogenesis With an External, Adjustable, Rigid Distraction Device. J. Craniofacial Surg. 1997, 8, 181–185. [Google Scholar] [CrossRef] [PubMed]
- Yamaji, K.E.; Gateno, J.; Xia, J.J.; Teichgraeber, J.F. New Internal Le Fort I Distractor for the Treatment of Midface Hypoplasia. J. Craniofacial Surg. 2004, 15, 124–127. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.X.; Wang, X.; Yi, B.; Li, Z.L.; Liang, C.; Lin, Y. Internal midface distraction in correction of severe maxillary hypoplasia secondary to cleft lip and palate. Plast. Reconstr. Surg. 2005, 116, 51–60. [Google Scholar] [CrossRef]
- Cheung, L.K.; Chua, H.D.P.; Hägg, M.B. Cleft maxillary distraction versus orthognathic surgery: Clinical morbidities and surgical relapse. Plast. Reconstr. Surg. 2006, 118, 996–1008. [Google Scholar] [CrossRef]
- Scolozzi, P. Distraction osteogenesis in the management of severe maxillary hypoplasia in cleft lip and palate patients. J. Craniofacial Surg. 2008, 19, 1199–1214. [Google Scholar] [CrossRef] [Green Version]
- Combs, P.D.; Harshbarger, R.J., 3rd. Le fort I maxillary advancement using distraction osteogenesis. Semin. Plast. Surg. 2014, 28, 193–198. [Google Scholar] [CrossRef] [Green Version]
- Laspos, C.P.; Kyrkanides, S.; Tallents, R.H.; E Moss, M.; Subtelny, J.D. Mandibular and maxillary asymmetry in individuals with unilateral cleft lip and palate. Cleft Palate-Craniofacial J. 1997, 34, 232–239. [Google Scholar] [CrossRef]
- Kyrkanides, S.; Klambani, M.; Subtelny, J.D. Cranial base and facial skeleton asymmetries in individuals with unilateral cleft lip and palate. Cleft Palate-Craniofacial J. 2000, 37, 556–561. [Google Scholar] [CrossRef]
- Lin, Y.; Chen, G.; Fu, Z.; Ma, L.; Li, W. Cone-beam computed tomography assessment of lower facial asymmetry in unilateral cleft lip and palate and non-cleft patients with class iii skeletal relationship. PLoS ONE 2015, 10, e0130235. [Google Scholar]
- Choi, Y.-K.; Park, S.-B.; Kim, Y.-I.; Son, W.-S. Three-dimensional evaluation of midfacial asymmetry in patients with nonsyndromic unilateral cleft lip and palate by cone-beam computed tomography. Korean J. Orthod. 2013, 43, 113–119. [Google Scholar] [CrossRef] [PubMed]
- Lonic, D.; Pai, B.C.-J.; Yamaguchi, K.; Chortrakarnkij, P.; Lin, H.-H.; Lo, L.-J. Computer-assisted orthognathic surgery for patients with cleft lip/palate: From traditional planning to three-dimensional surgical simulation. PLoS ONE 2016, 11, e0152014. [Google Scholar] [CrossRef]
- Lew, K.K.; Foong, W.C.; Loh, E. Malocclusion prevalence in an ethnic Chinese population. Aust. Dent. J. 1993, 38, 442–449. [Google Scholar] [CrossRef] [PubMed]
- Zere, E.; Chaudhari, P.K.; Sharan, J.; Dhingra, K.; Tiwari, N. Developing Class III malocclusions: Challenges and solutions. Clin. Cosmet. Investig. Dent. 2018, 10, 99–116. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chan, E.K.; Soh, J.; Petocz, P.; Darendeliler, M.A. Esthetic evaluation of Asian-Chinese profiles from a white perspective. Am. J. Orthod. Dentofac. Orthop. 2008, 133, 532–538. [Google Scholar] [CrossRef] [PubMed]
- Kuroda, S.; Sugahara, T.; Takabatake, S.; Taketa, H.; Ando, R.; Takano-Yamamoto, T. Influence of anteroposterior mandibular positions on facial attractiveness in Japanese adults. Am. J. Orthod. Dentofac. Orthop. 2009, 135, 73–78. [Google Scholar] [CrossRef]
- Lee, L.H.; Jun, J.H.; Danganan, M.; Pogrel, M.A.; Kushner, H.; Lee, J.S. Orthognathic surgery for the Asian patient and the influence of the surgeon’s background on treatment. Int. J. Oral Maxillofac. Surg. 2011, 40, 458–463. [Google Scholar] [CrossRef]
- Chortrakarnkij, P.; Lonic, D.; Lin, H.H.; Yamaguchi, K.; Kim, S.G.; Lo, L.J. A Modified Technique of Mandibular Ramus Sagittal Split Osteotomy for Prevention of Inferior Alveolar Nerve Injury: A Prospective Cohort Study and Outcome Assessment. Ann. Plast. Surg. 2017, 78 (Suppl. S2), S108–S116. [Google Scholar] [CrossRef]
- Choi, B.-K.; Lee, W.; Lo, L.-J.; Yang, E.-J. Is injury to the inferior alveolar nerve still common during orthognathic surgery? Manual twist technique for sagittal split ramus osteotomy. Br. J. Oral Maxillofac. Surg. 2018, 56, 946–951. [Google Scholar] [CrossRef]
- Hsieh, Y.J.; Chen, Y.C.; Chen, Y.A.; Liao, Y.F.; Chen, Y.R. Effect of bimaxillary rotational setback surgery on upper airway structure in skeletal class III deformities. Plast. Reconstr. Surg. 2015, 135, 361e–369e. [Google Scholar] [CrossRef] [PubMed]
- He, J.; Wang, Y.; Hu, H.; Liao, Q.; Zhang, W.; Xiang, X.; Fan, X. Impact on the upper airway space of different types of orthognathic surgery for the correction of skeletal class III malocclusion: A systematic review and meta-analysis. Int. J. Surg. 2017, 38, 31–40. [Google Scholar] [CrossRef] [PubMed]
- Chang, C.-S.; Wallace, C.G.; Hsiao, Y.-C.; Hsieh, Y.-J.; Wang, Y.-C.; Chen, N.-H.; Liao, Y.-F.; Liou, E.J.-W.; Chen, P.K.-T.; Chen, J.-P.; et al. Airway Changes after Cleft Orthognathic Surgery Evaluated by Three-Dimensional Computed Tomography and Overnight Polysomnographic Study. Sci. Rep. 2017, 7, 12260. [Google Scholar] [CrossRef]
- Yatabe-Ioshida, M.S.; Campos, L.D.; Yaedu, R.Y.; Trindade-Suedam, I. Upper Airway 3D Changes of Patients with Cleft Lip and Palate After Orthognathic Surgery. Cleft Palate-Craniofacial J. 2019, 56, 314–320. [Google Scholar] [CrossRef]
- Posnick, J.C. Orthognathic surgery for the cleft lip and palate patient. Semin. Orthod. 1996, 2, 205–214. [Google Scholar] [CrossRef]
- Iannetti, G.; Cascone, P.; Saltarel, A.; Ettaro, G. Le Fort I in cleft patients: 20 years’ experience. J. Craniofacial Surg. 2004, 15, 662–669. [Google Scholar] [CrossRef]
- Chong, D.K.; Portnof, J.E.; Xu, H.; Salyer, K.E. Reviewing the orthognathic surgical care of the patient with cleft lip and palate: The single surgeon experience. J. Craniofacial Surg. 2009, 20 (Suppl. S2), 1895–1904. [Google Scholar] [CrossRef] [Green Version]
- Broome, M.; Herzog, G.; Hohlfeld, J.; Roessingh, A.D.B.; Jaques, B. Influence of the Primary Cleft Palate Closure on the Future Need for Orthognathic Surgery in Unilateral Cleft Lip and Palate Patients. J. Craniofacial Surg. 2010, 21, 1615–1618. [Google Scholar] [CrossRef] [Green Version]
- Watts, G.D.; Antonarakis, G.S.; Forrest, C.R.; Tompson, B.D.; Phillips, J.H. Single Versus Segmental Maxillary Osteotomies and Long-Term Stability in Unilateral Cleft Lip and Palate Related Malocclusion. J. Oral Maxillofac. Surg. 2014, 72, 2514–2521. [Google Scholar] [CrossRef]
- Fahradyan, A.; Wolfswinkel, E.M.; Clarke, N.; Park, S.; Tsuha, M.; Urata, M.M.; Hammoudeh, J.A.; Yamashita, D.-D.R. Impact of the Distance of Maxillary Advancement on Horizontal Relapse After Orthognathic Surgery. Cleft Palate-Craniofacial J. 2018, 55, 546–553. [Google Scholar] [CrossRef]
- Impieri, D.; Tønseth, K.; Hide, Ø.; Brinck, E.; Høgevold, H.; Filip, C. Impact of orthognathic surgery on velopharyngeal function by evaluating speech and cephalometric radiographs. J. Plast. Reconstr. Aesthetic Surg. 2018, 71, 1786–1795. [Google Scholar] [CrossRef] [PubMed]
- Marion, F.; Mercier, J.; Odri, G.-A.; Perrin, J.; Longis, J.; Kün-Darbois, J.-D.; Corre, P.; Bertin, H. Associated relaps factors in Le Fort I osteotomy. A retrospective study of 54 cases. J. Stomatol. Oral Maxillofac. Surg. 2019, 120, 419–427. [Google Scholar] [CrossRef] [PubMed]
- Chung, J.; Lim, J.; Park, H.; Yoo, A.; Kim, S.; Koo, Y. Correlation Between Speech Outcomes and the Amount of Maxillary Advancement After Orthognathic Surgery (Le Fort I Conventional Osteotomy and Distraction Osteogenesis) in Patients With Cleft Lip and Palate. J. Craniofacial Surg. 2019, 30, 1855–1858. [Google Scholar] [CrossRef] [PubMed]
- Harjunpää, R.; Alaluusua, S.; Leikola, J.; Heliövaara, A. Le Fort I osteotomy in cleft patients: Maxillary advancement and velopharyngeal function. J. Cranio-Maxillofacial Surg. 2019, 47, 1868–1874. [Google Scholar] [CrossRef]
- Wang, Y.; Li, J.; Xu, Y.; Huang, N.; Shi, B.; Li, J. Accuracy of virtual surgical planning-assisted management for maxillary hypoplasia in adult patients with cleft lip and palate. J. Plast. Reconstr. Aesthetic Surg. 2020, 73, 134–140. [Google Scholar] [CrossRef] [Green Version]
- Wangsrimongkol, B.; Flores, R.L.; Staffenberg, D.A.; Rodriguez, E.D.; Shetye, P.R. Skeletal and dental correction and stability following LeFort I advancement in patients with cleft lip and palate with mild, moderate, and severe maxillary hypoplasia. Cleft Palate-Craniofacial J. 2021, 59, 98–109, Online ahead of print. [Google Scholar] [CrossRef]

| Landmark | Definition |
|---|---|
| Basion (Ba) | The most anterior point of the great foramen (foramen magnum). |
| Nasion (N) | The midpoint of the frontonasal sutures. |
| Sella (S) | The center of the hypophyseal fossa (sella turcica). |
| Porion (Po) | The most superior point of each external acoustic meatus. |
| Orbitale (Or) | The most inferior point of each infra-orbital rim. |
| Anterior nasal spine (ANS) | The most anterior midpoint of the anterior nasal spine of the maxilla. |
| A point (A) | The point of maximum concavity in the mid-line of the alveolar process of the maxilla. |
| B point (B) | The point of maximum concavity in the mid-line of the alveolar process of the mandible. |
| Pogonion (Pog) | The most anterior midpoint of the chin on the outline of the mandibular symphysis. |
| Menton (Me) | The most inferior midpoint of the chin on the outline of the mandibular symphysis. |
| Gonion (Go) | Dropping a perpendicular from the intersection point of the tangent lines to the posterior margin of the mandibular vertical ramus and inferior margin of the mandibular body or horizontal ramus. |
| Upper incisors (U1) | The midpoint between the crowns of the maxillary central incisors. |
| Lower incisors (L1) | The midpoint between the crowns of the mandibular central incisors. |
| Upper canine (U3R/L) | The cusp tip of the maxillary canine on the right/left side. |
| Lower canine (L3R/L) | The cusp tip of the mandibular canine on the right/left side. |
| Upper first molar (U6R/L) | The mesio-buccal cusp of the maxillary first molar on the right/left side. |
| Lower first molar (L6R/L) | The mesio-buccal cusp of the mandibular first molar on the right/left side. |
| Anterior occlusal cant | Angle between the line of canines and Frankfort horizontal plane. |
| Posterior occlusal cant X axis Y axis Z axis | Angle between the line of first molars and Frankfort horizontal plane. Frankfort horizontal plane. Midsagittal plan. Coronal plane. |
| Parameters | T0 Stage | Norms | p Value | ||
|---|---|---|---|---|---|
| Mean | SD | Mean | SD | ||
| SNA | 75.90 | 4.32 | 83.22 | 2.95 | 0.000 ** |
| SNB | 80.44 | 4.70 | 80.02 | 3.24 | 0.768 |
| ANB | −4.72 | 4.10 | 3.34 | 1.56 | 0.000 ** |
| A-N perpendicular | −4.98 | 3.47 | 1.10 | 2.66 | 0.000 ** |
| Pog-N perpendicular | −0.11 | 7.36 | −3.10 | 6.50 | 0.462 |
| SN/MP | 35.30 | 7.42 | 33.63 | 5.11 | 0.639 |
| The midline discrepancy | |||||
| ANS | 2.87 | 2.09 | 0.73 | 0.50 | 0.000 ** |
| A | 1.57 | 1.99 | 0.67 | 0.43 | 0.000 ** |
| Me | 2.58 | 2.99 | 0.92 | 0.42 | 0.000 ** |
| U1 | 3.01 | 2.97 | 0.59 | 0.26 | 0.000 ** |
| L1 | 2.16 | 2.76 | 0.47 | 0.24 | 0.000 ** |
| Parameters | One-Jaw | Two-Jaw | One-Jaw vs. Two-Jaw | ||
|---|---|---|---|---|---|
| Mean | SD | Mean | SD | p Value | |
| SNA | 83.48 | 5.25 | 80.79 | 3.61 | 0.000 ** |
| SNB | 80.44 | 4.70 | 77.57 | 3.45 | 0.000 ** |
| ANB | 3.12 | 4.22 | 3.37 | 3.44 | 0.706 |
| A-N perpendicular | 2.48 | 4.32 | −0.18 | 3.04 | 0.000 ** |
| Pog-N perpendicular | −0.11 | 7.36 | −1.76 | 4.28 | 0.099 |
| Anterior cant | 4.64 | 3.80 | 3.10 | 2.67 | 0.000 ** |
| Posterior cant | 2.48 | 1.81 | 0.90 | 0.89 | 0.000 ** |
| The midline discrepancy | |||||
| A | 2.27 | 1.60 | 1.75 | 1.19 | 0.039 * |
| Me | 2.52 | 2.20 | 1.51 | 1.01 | 0.012 * |
| U1 | 2.77 | 2.20 | 1.37 | 1.41 | 0.001 ** |
| L1 | 2.16 | 1.88 | 1.45 | 1.06 | 0.038 * |
| Parameters | One-Jaw | Two-Jaw | One-Jaw vs. Two-Jaw | ||
|---|---|---|---|---|---|
| Mean | SD | Mean | SD | p Value | |
| Larger advancement (n = 26) | |||||
| SNA | 85.23 | 4.25 | 80.68 | 2.95 | 0.000 ** |
| SNB | 80.83 | 4.86 | 77.73 | 3.67 | 0.000 ** |
| ANB | 4.67 | 3.41 | 3.20 | 3.12 | 0.050 |
| A-N perpendicular | 3.88 | 3.94 | −0.66 | 2.85 | 0.000 ** |
| Pog-N perpendicular | −0.13 | 8.42 | −1.90 | 4.36 | 0.188 |
| Regular advancement (n = 15) | |||||
| SNA | 80.41 | 5.77 | 80.99 | 4.82 | 0.316 |
| SNB | 79.91 | 4.64 | 77.73 | 3.21 | 0.007 ** |
| ANB | 0.25 | 4.34 | 3.53 | 4.15 | 0.004 ** |
| A-N perpendicular | 0.05 | 4.13 | 0.67 | 3.38 | 0.236 |
| Pog-N perpendicular | 0.14 | 5.42 | −1.32 | 4.94 | 0.441 |
| Landmarks | T0 | One-Jaw | Two-Jaw | T0 vs. One-Jaw | T0 vs. Two-Jaw | One-Jaw vs. Two-Jaw | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | p Value | p Value | p Value | ||
| Maxilla | ||||||||||
| A | 1.58 | 1.19 | 2.27 | 1.60 | 1.75 | 1.19 | 0.010 * | 0.497 | 0.039 * | |
| U1 | 3.06 | 1.90 | 2.77 | 2.20 | 1.37 | 1.41 | 0.299 | 0.000 * | 0.001 * | |
| U3 | 6.28 | 3.87 | 7.68 | 3.73 | 6.53 | 3.87 | 0.013 * | 0.628 | 0.027 * | |
| U6 | 4.36 | 2.05 | 6.40 | 3.55 | 4.98 | 2.94 | 0.000 ** | 0.176 | 0.000 ** | |
| Mandible | ||||||||||
| B | 2.30 | 2.09 | 2.30 | 2.09 | 1.34 | 1.15 | NS | 0.004 ** | 0.012 * | |
| Pog | 2.50 | 2.14 | 2.50 | 2.14 | 1.57 | 1.10 | NS | 0.016 * | 0.017 * | |
| Me | 2.52 | 2.20 | 2.52 | 2.20 | 1.51 | 1.01 | NS | 0.011 * | 0.009 ** | |
| L1 | 2.16 | 1.88 | 2.16 | 1.88 | 1.45 | 1.06 | NS | 0.031 * | 0.038 * | |
| L3 | 5.13 | 3.42 | 5.13 | 3.42 | 3.92 | 2.22 | NS | 0.038 * | 0.038 * | |
| L6 | 4.92 | 3.28 | 4.92 | 3.28 | 3.29 | 1.83 | NS | 0.001 ** | 0.001 ** | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tsai, Y.-H.; Pai, B.C.J.; Lin, H.-H.; Ho, C.-T.; Lo, L.-J. One-Jaw versus Two-Jaw Orthognathic Surgery for Patients with Cleft: A Comparative Study Using 3D Imaging Virtual Surgical Planning. Appl. Sci. 2022, 12, 4461. https://doi.org/10.3390/app12094461
Tsai Y-H, Pai BCJ, Lin H-H, Ho C-T, Lo L-J. One-Jaw versus Two-Jaw Orthognathic Surgery for Patients with Cleft: A Comparative Study Using 3D Imaging Virtual Surgical Planning. Applied Sciences. 2022; 12(9):4461. https://doi.org/10.3390/app12094461
Chicago/Turabian StyleTsai, Yu-Hung, Betty C. J. Pai, Hsiu-Hsia Lin, Cheng-Ting Ho, and Lun-Jou Lo. 2022. "One-Jaw versus Two-Jaw Orthognathic Surgery for Patients with Cleft: A Comparative Study Using 3D Imaging Virtual Surgical Planning" Applied Sciences 12, no. 9: 4461. https://doi.org/10.3390/app12094461
APA StyleTsai, Y.-H., Pai, B. C. J., Lin, H.-H., Ho, C.-T., & Lo, L.-J. (2022). One-Jaw versus Two-Jaw Orthognathic Surgery for Patients with Cleft: A Comparative Study Using 3D Imaging Virtual Surgical Planning. Applied Sciences, 12(9), 4461. https://doi.org/10.3390/app12094461







