Abstract
The aim of this study was to evaluate the clinical application of fixed screw-retained complete-arch rehabilitations supported by four narrow-diameter implants (NDIs). The records of patients treated with complete-arch prostheses screwed onto four NDIs treated with an immediate loading protocol between 2010 and 2020 with at least 1 year of follow-up after the positioning of the definitive restoration were reviewed. The implants were placed according to the final prosthetic design and were immediately loaded. The interim prostheses were replaced after the healing period by definitive acrylic resin titanium-supported prostheses. Patients were followed to evaluate treatment success, the implant survival rate (ISR), and the prosthetic survival rate (PSR). A total of 121 NDIs were positioned in 30 patients to restore 30 complete arches (18 maxilla and 12 mandible). One implant did not achieve osseointegration, resulting in an overall ISR of 99.2%. No prosthetic or implant failures occurred during the 1 to 11 years of follow-up. Three biological and four prosthetic complications occurred, resulting in a treatment rehabilitation survival of 94.1% and a PSR of 86.7%. Despite the limitations of the present retrospective study, such as the use of one single type of dental implant and patients treated in a single rehabilitation center, complete-arch rehabilitation with fixed prostheses supported by four NDIs seems to be a reliable treatment in the medium to long term.
1. Introduction
Before the arrival of dental implants, removable dentures were the only possibility to rehabilitate complete edentulous patients [1]. From the first years of the 21st century, tilting dental implants up to 30° distally in the distal parts of the jaws to avoid contact with the maxillary sinus or the inferior alveolar canals in atrophic jaws, avoiding bone augmentation procedures, became a well-documented and reliable treatment option. Malo et al. developed the “All-on-4” concept to restore edentulous jaws with two implants positioned axial in the anterior zone and two tilted in the posterior zone of both jaws [2]. The idea was to place the implants in a geometric manner that was as regular and symmetric as possible to make the interimplant position as large as possible, reducing the distal cantilever lengths of prostheses with 12 teeth [3,4,5,6].
However, patients that were edentate for a long time or the presence of terminal dentitions may increase the need for horizontal and/or vertical augmentation of the alveolar bones in both jaws [2,7,8]. Moreover, trauma, malformation, neoplasms, the use of removable prostheses, and periodontal disease may increase the reduction in bone width [9,10,11].
Different types of vertical and horizontal augmentation techniques were proposed to overcome these dimensional changes, such as maxillary sinus elevation and/or vertical ridge augmentation in combination with contour augmentation [12,13,14]. However, these procedures should be performed only by expert clinicians to minimize possible intraoperative complications and postoperative morbidity. The combination of several augmentation procedures with dental implant placement may influence the overall surgery outcomes, such as early graft or membrane exposure [15,16,17,18,19,20]. Narrow-diameter dental implants (NDIs) were introduced to reduce or eliminate the need for horizontal bone augmentation procedures, reducing the implant diameter in the most coronal part [21,22,23,24]. NDIs can be classified in three categories according to the ITI consensus report [25]:
- Implants < 2.5 mm Ø (“Mini-implants”);
- Implants 2.5 mm to <3.3 mm Ø;
- Implants 3.3 mm to 3.5 mm Ø.
In certain clinical scenarios, NDIs provide prosthetic flexibility in patients with a reduced mesiodistal width or reduced bone thickness. Moreover, NDIs can be used for single-tooth rehabilitations, such as lateral incisors in the upper jaw or incisors in the lower jaw [26,27,28,29]. However, reducing the implant diameter may increase the risk of implant or component fracture in patients with heavy chewing function or parafunction. NDIs positioned to replace missing teeth in the posterior zone are still not well investigated in the literature. In these cases, it is mandatory to use caution in patients with parafunctional habits and malocclusion. As a matter of fact, for NDIs in the anterior zone there are different biomechanical forces that can overload the implants compared to the posterior zone [25,28,30,31,32,33].
The aim of this retrospective study was to evaluate the clinical survival of fixed screw-retained complete-arch rehabilitations supported by four NDIs.
2. Materials and Methods
The analysis was conducted in a retrospective manner that included all patients treated with a single operative protocol in a single dental office between 2010 and 2020. The patients included in the analysis needed to be followed up for a minimum of 1 year after the positioning of the definitive restoration. The study was conducted in accordance with the Helsinki Declaration of 1964 and the revision in 2013 for ethical principles regarding human experimentation and with the written informed consent of the patients. The study was approved by the institutional review board of Sapienza University of Rome with protocol number 0000212 and was registered with protocol number ISRCTN16104700 (date: 10/02/2022). The study was conducted following the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines (http://www.strobe-statement.org (accessed on 20 December 2022)) [34]. The medical status of the patients was documented. The patients included in the retrospective study were treated if they were in good health and did not need any bone augmentation procedures to place four implants with minimum dimensions of 3.3 mm of diameter and 10 mm of length. Patients were not treated if they did not have suitable bones for such measures of implants, had diseases, or smoked. All patients gave their written informed consent for immediate implant loading.
2.1. Clinical Protocol
Each treated patient received a comprehensive evaluation of function and esthetic in order to re-establish correct tooth positions. Patients were included in this treatment protocol if they were fully edentulous or partially edentulous with terminal dentitions in one or both jaws. Moreover, the periodontal status was screened, and only patients with plaque scores (PS) < 25% and bleeding on probing (BoP) < 20% could receive the treatment. For edentulous patients, brand-new removable dentures were fabricated and worn by patients to re-establish function, aesthetic, and correct tooth positions until the patients felt comfortable with the new disposition. For terminal dentition patients, partial dentures were fabricated if stable teeth were present, otherwise extractions were performed and immediate dentures were fabricated. Diagnoses were made clinically and radiographically with preoperative panoramic radiographs and CBCT scans with radiographic templates in place. Radiographic templates were made from duplications of the interim prostheses (Figure 1, Figure 2 and Figure 3).
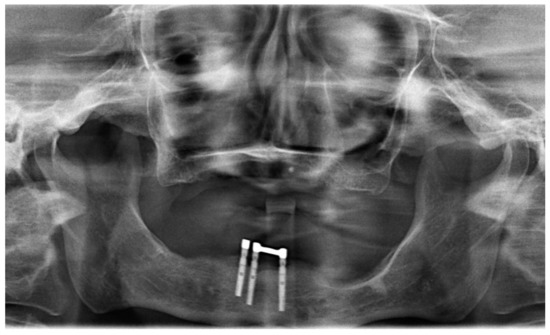
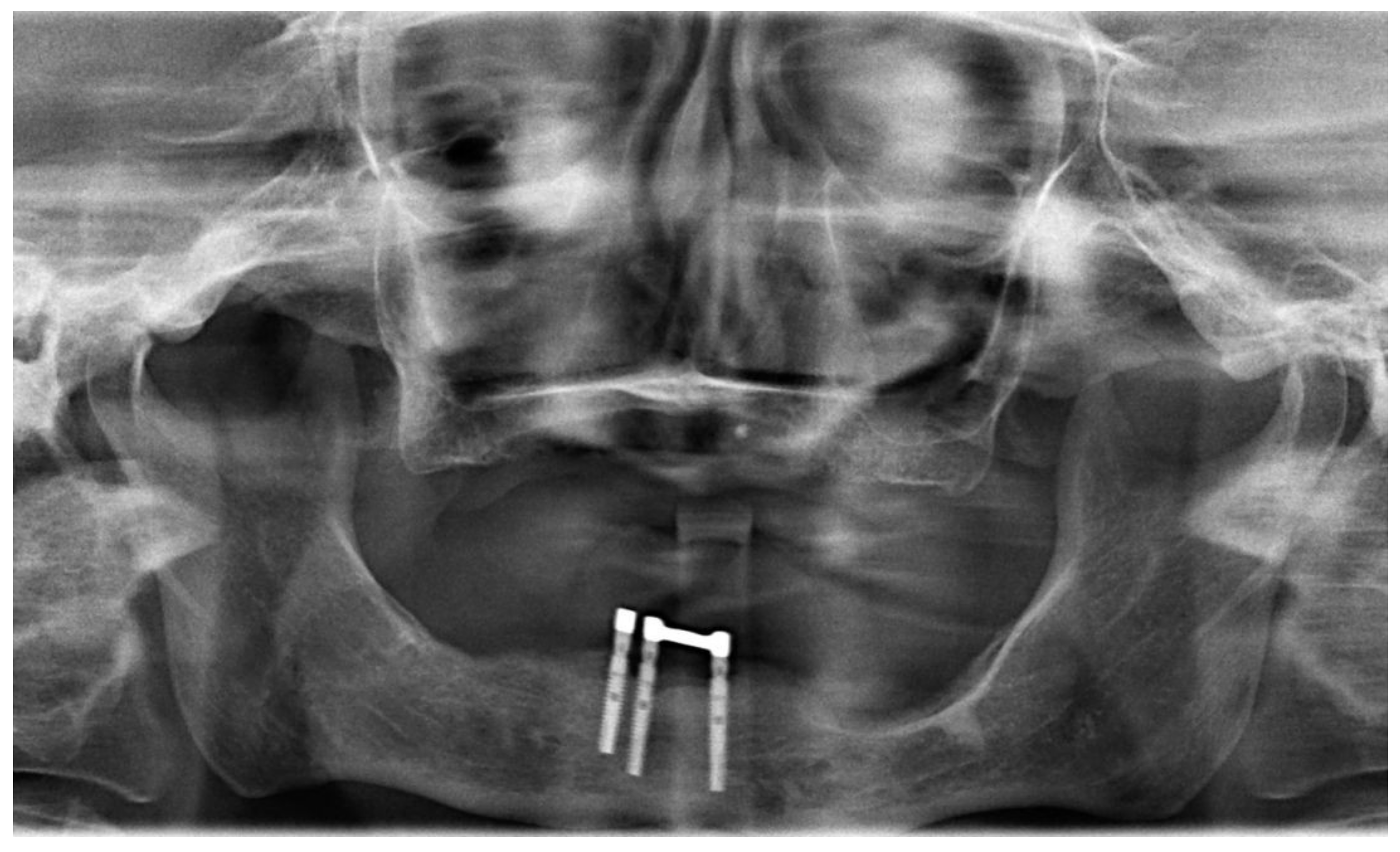
Figure 1.
Preoperative panoramic radiograph with complete edentulism in the maxilla and failing implants in the mandible.
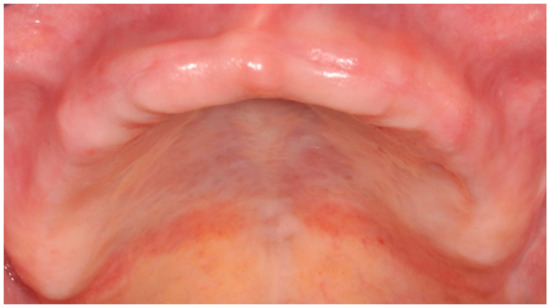
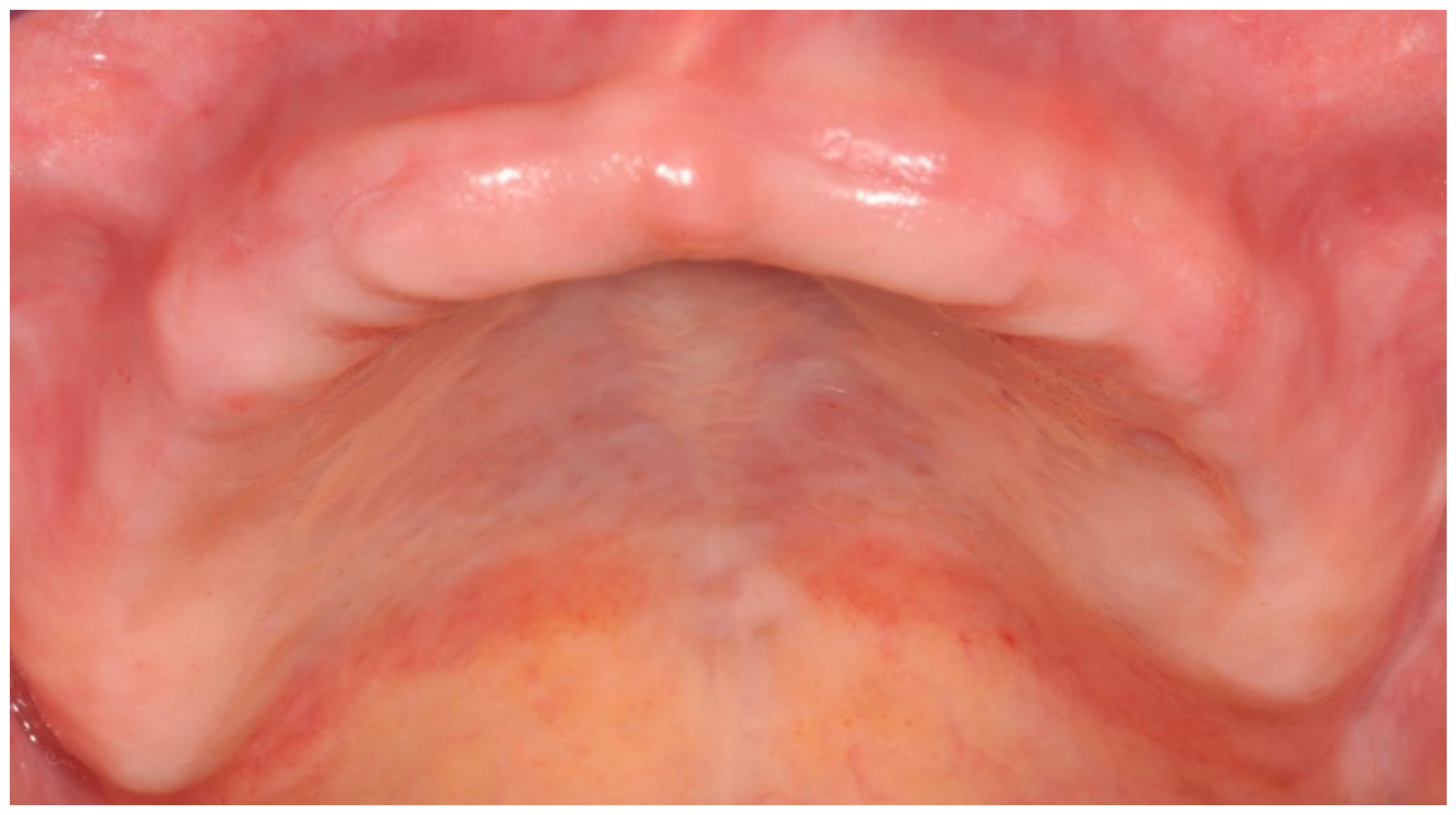
Figure 2.
Clinical view of an edentulous maxilla before treatment.

Figure 3.
Radiographic template with radiopaque landmarks made from a duplicate of the denture.
From 2010 to 2015, implants were positioned free-hand using the radiographic templates to prepare implant recipient sites; from 2016 to the conclusion of the report, fully computer-guided surgery with static templates was used to place the implants. Platform-switched implants with round apexes (Bone Level Implant, Straumann, Straumann AG, Basel, Switzerland) or tapered apexes (Bone Level Tapered Implant, Straumann) with a narrow neck diameter of 3.3 mm were used in the treated patients. A specific drill set was used to prepare each implant recipient site (Surgical Kit, Straumann). The sequence of the drills was carefully respected in order to underprepare the implant recipient site, enhancing primary stability. The first drill was a needle drill that had to create a hole in the cortical zone. Then, the pilot drill (2.2 Ø mm) was used to create a pathway in the hole made by the needle drill. These two drills were used under copious irrigation at 800 rpm. The last drill was the 2.8 Ø mm drill, which followed the pilot drill pathway. The drill was used without irrigation at 40 rpm in order to recover bone chips along the drill. Then, the profile drill (3.3 Ø mm) was used only in the crestal zone to reduce stress on the cortical zone during implant positioning. The flaps were limited to the implant recipient zone and were not overextended in order to reduce the invasiveness. The insertion torque was confirmed with a torque wrench (Straumann AG). After implant placement, angulated or straight screw-retained abutments (SRA, Straumann) were positioned to enhance the parallelism between the tilted and vertical implants with titanium copings screwed onto them. The SRAs could correct the emergence profile from 0° to 30° with different gingival heights to create an appropriate transmucosal tunnel and an axial support for the occlusal load. Sutures were used if necessary and were made by polyglycolic acid (PGA). Chlorhexidine (0.1%) was recommended for patients twice daily for one week for plaque control. For pain control, the patients were prescribed analgesics. The sutures were removed 14 days after surgery. The interim prostheses based on the prosthetic plans were milled from blocks of polymethyl methacrylate (PMMA, dima Mill temp, Kulzer) and merged with a self-curing resin (Enamel Plus, Micerium) to the titanium copings. The correct position of the interim prosthesis was determined by occlusal contacts with the opposite dentition. The interim prostheses had no cantilevers and were screwed to 15 Ncm onto the SRAs (Figure 4 and Figure 5).

Figure 4.
Interim prosthesis without cantilevers.

Figure 5.
Interim prosthesis after implant placement.
Occlusion was verified with 40 μm articulating paper to avoid heavy contacts in order to uniformly distribute in centric occlusion and light lateral contacts. Patients were recalled 7 days after the surgery and every 15 days to check the occlusal contacts for the first 3 months. Moreover, maxillary occlusal nightguards were delivered to every patient to minimize the parafunction stress on the implants. They were designed to be applied only on the occlusal part of the prostheses and were realized from acrylic resin discs (Erkodent, Pfalzgrafenweile, Germany). The interim prostheses were not removed for at least 6 weeks from the immediate loading. At the end of the healing period, panoramic radiographs were taken, and the prostheses removed to check the implant stability. If an implant showed mobility, pain, or suppuration, it was removed, recorded as a failure, and replaced after 3 months. The SRA screws were torqued to 35 Ncm, and if the implants showed an absence of mobility, pain, and suppuration, they were considered osseointegrated and ready for the final prosthetic part of the protocol. A definitive plaster impression was taken to obtain a master cast of the patient. The definitive prosthesis workflow followed the principles of the removable complete denture. The main difference was that the definitive prostheses had a titanium framework with an acrylic resin denture base material and denture teeth and was screwed to the implants. The frameworks were digitally designed with titanium retentive pins for each tooth and were milled at a specialized milling center (Createch Medical Milling Center, Createch Medical S.L., Mendaro, Spain). Moreover, they had cantilevers to support the first molars. The cantilever length was determined following the prosthetic plan of the rehabilitation in combination with the final distal implant position including only the first molar (Figure 6 and Figure 7).

Figure 6.
Definitive prosthesis with cantilevers after 7 years of use.

Figure 7.
Occlusal view of definitive prosthesis after 7 years of use.
On the day of definitive prosthesis placement, new maxillary acrylic resin occlusal nightguards were delivered to each patient and screw access openings were restored with a provisional material (Fermit, Ivoclar Vivadent, Naturno, Bolzano, Italy). The patients were recalled every 4 months for professional oral hygiene and peri-implant parameter recording (BoP and PS) and every 12 months for annual radiographic and clinical examinations, following the EAO guidelines [35] (Figure 8).

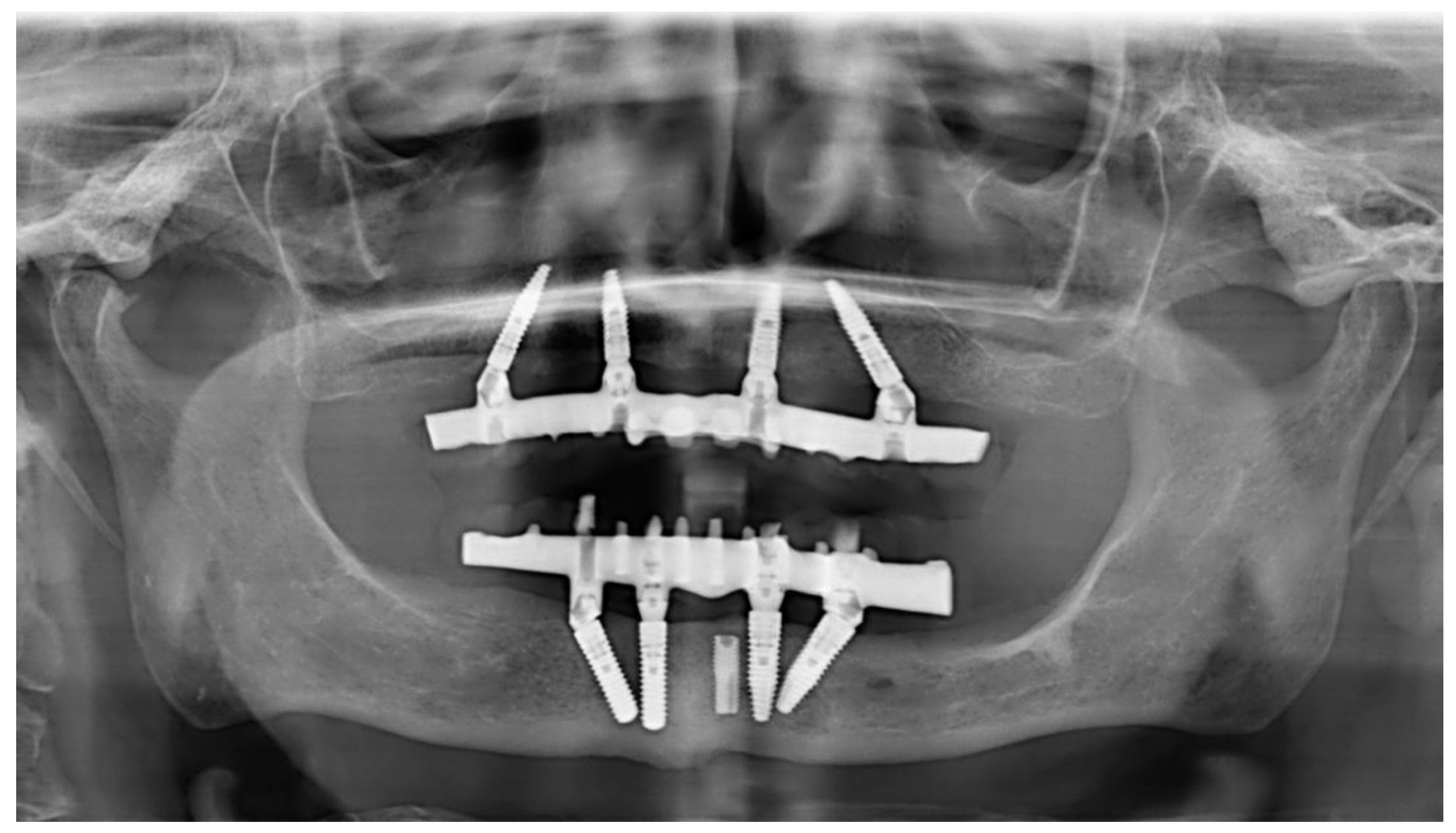
Figure 8.
Panoramic radiograph after 7 years of use in maxillary-implant-supported rehabilitation. In the mandible, the same treatment was performed with standard-diameter implants. One previously placed implant had fractured and was left in the subgingival region. It was not included in the rehabilitation treatment.
2.2. Follow-Up Protocol
Each patient was enrolled in a specific maintenance protocol. Every 4 months, one expert dental hygienist performed a professional hygiene session. A clinical check of the implant and the prosthesis was performed annually. An independent operator who was not involved in the study performed panoramic radiographs to assess the radiographic peri-implant bone quality in accordance with the European Association for Osseointegration (EAO) guidelines. Implant success and survival were assessed according to the criteria accepted at the International Congress of Oral Implantologists Consensus Conference for Implant Success [36]. Biological (i.e., mucositis and peri-implantitis) as well as technical complications (i.e., screw loosening, acrylic veneering fractures, and tooth detachment) were also recorded at each planned visit. Moreover, peri-implant values were recorded at the four sites/implants by one experienced dental hygienist.
2.3. Outcomes
2.3.1. Rehabilitation Treatment Survival
The rehabilitation treatment was survival in the absence of biologic or prosthetic complications after definitive prosthesis delivery.
2.3.2. Implant Survival Rate
The implants were recorded as successfully integrated implants after clinical and radiographic examinations in accordance with the criteria of Albrektsson [37]. A “surviving implant” was an implant in the absence of biologic complications, without bleeding and/or suppuration on probing, with an absence of pain, mobility, or suppuration when the peri-implant mucosa was pressed. Moreover, the combination of one of the previous clinical signs with radiographic bone loss of more than 2 mm were the criteria to be used for the diagnosis of peri-implantitis [38,39].
2.3.3. Prosthetic Survival Rate
Definitive prosthesis survival was defined as an absence of technical complications. A “surviving prosthesis” was a prosthetic reconstruction that was stable and in good function [1].
2.3.4. Soft Tissue Parameters
Soft tissue values were assessed at the implant–SRA interfaces at each follow-up visit using a periodontal probe (Hu-Friedy PGF-GFS, Hu-Friedy), following the protocol previously published by the authors of [40].
2.4. Statistical Analysis
The data of the involved patients were anonymized and imported into a master spreadsheet. A descriptive analysis was performed using means and standard deviations. The implant was used as the unit in the statistical analysis.
3. Results
The results from 30 patients of both genders (13 men and 17 women, mean age: 69.2, ranging from 54 to 87 years) were collected and analyzed (Table 1).

Table 1.
Main characteristics of included patients (mean age in years).
A total of 30 complete arches (18 maxilla and 12 mandible) were restored using four NDIs that were loaded immediately to support screw-retained fixed prostheses. In total, 121 NDIs were positioned, and 120 were reviewed at least 1 year after definitive prosthesis positioning (Table 2).

Table 2.
Life table analysis at the implant level (n = implants placed per year; follow-up in years).
In total, 40 implants (33.3%) were positioned flapless, while 80 implants (66.7%) were positioned with flaps, and 68 implants were positioned in healed sites (56.7%), while 52 implants were positioned in postextraction sockets (43.3%). Two types of NDIs were used: 70 Ø3.3 mm Narrow Crossfit® Bone Level implants (BL NC, Straumann) and 50 Ø3.3 Narrow Crossfit Bone Level Tapered implants (BLT NC, Straumann). The implants lengths were 14 mm (50.8%), 12 mm (45%), and 10 mm (4.2%) (Table 3).

Table 3.
Characteristics of positioned implants.
All implants were inserted with insertion torque values of at least 35 Ncm. Twelve arches were treated using prosthetically driven free-hand surgery while the other eighteen arches were treated using fully guided template-driven static computer-guided surgery. In the opposite dentitions, 11 patients presented with natural teeth and fixed restorations, 10 patients had removable dentures, 7 patients had implants supporting complete-arch fixed prostheses, and 2 had natural dentitions. No dropouts occurred during the follow-up period, and no deviations occurred from the original protocol. No prosthetic complications occurred to the interim prosthesis during the healing period. One implant did not achieve osseointegration during the healing period, resulting in an implant survival rate of 99.2%. The failed implant (BLT NC 12 mm) was placed in a healed site, removed at the osseointegration check after the healing period, and replaced via a computer-guided surgery procedure after a healing period of 3 months. After the healing period, a total of 30 definitive prostheses with cantilevers were positioned. No prosthetic or implant failures (i.e., framework fracture, abutment fracture, or screw fracture) occurred during the entire observation period. BoP was recorded for three implants (2.5%), and plaque was detected around seven implants (5.8%). No mucositis or peri-implantitis were recorded at the last follow-up visits. Three biological and four prosthetic complications occurred, resulting in a treatment rehabilitation success of 94.1%. Three implants showed mucositis in two patients after 4 and 6 years of use. The patients skipped two professional maintenance sessions. The implants were debrided, chlorhexidine was prescribed twice a day for 15 days, and the complications resolved [41]. Four prosthetic complications occurred in three patients, resulting in a prosthetic survival rate of 86.7%. Two patients had chipping of acrylic resin veneers, and one patient had chipping and screw loosening on two implants after 5 and 8 years of use, respectively. The patients did not wear the nightguards for 6 months. The prostheses were repaired and screwed to 15 Ncm to the SRAs, and the patients were encouraged to wear the nightguards.
4. Discussion
The aim of this study was to analyze the clinical outcomes of complete arch restored with complete-arch prostheses that were screwed onto four NDIs and loaded immediately. The main limitations of this study were the lack of a control group and its retrospective nature. Nevertheless, 120 NDIs were positioned, restoring 30 complete arches. Only one implant did not achieve osteointegration after the healing period, and it was successfully replaced, resulting in an ISR of 99.2% after an observation period ranging from one to eleven years. Several studies investigated the clinical performance of NDIs [22,23,24]. Two systematic reviews by Gonzalez-Valls et al. [10] and Valente et al. [11] reported that the clinical outcomes of NDIs can be comparable to the standard dental implant outcomes, especially when significative bone augmentation procedures are needed to place standard implants. The meta-analysis showed an overall NDI ISR of 97.80% over 3.5 years of follow up, while the ISR for implants placed with horizontal bone augmentation procedures reported an overall ISR of 97.22% after 3.22 years of follow-up [11]. In recent years, NDIs were investigated in clinical scenarios of partially edentulous patients when supporting fixed prostheses in the aesthetic and posterior zones [9,15,25], providing high ISR values and a low incidence of biologic and/or prosthetic complications. Moreover, NDIs may be useful when wide bone augmentation procedures are required, such as after trauma, malformation, neoplasms, the use of removable prostheses, and periodontal disease. Reconstructive surgeries are always related to greater morbidity, leading to multiple surgeries and higher economic costs for the patients. In complete edentulous patients, NDIs were mostly used to support two-implant mandibular overdentures, providing encouraging clinical results in terms of ISR, marginal bone loss (MBL), and patient satisfaction [16,17,18,26]. The main limitation of this treatment option is the hybrid support of the prostheses. The mandibular overdenture can be attached to two implants and can have a mucosa support. In this sense, the comfort for the patients could decrease because of the load on the posterior region of the mucosa in the mandible. For fixed prostheses, four implants are considered to be the minimum number to give support and to reduce overload. One study conducted by Coskunses [27] reported clinical data of 67 NDIs supporting fixed complete-arch prostheses in combination with standard dental implants, with a maximum of 2 years of follow-up. In these terms, the present study reported clinical data of 30 complete arches from 1 to 11 years of use restored with complete-arch prostheses screwed onto four NDIs. Complete-arch restorations with four implants could be considered a valid treatment option in the medium to long term. As a matter of fact, the last systematic review with a meta-analysis by Valente et al. [11] indicated that “NDIs do not seem suitable for ‘all-on-four’ rehabilitations due to the increased load stress during occlusal function”. The present study goes the opposite way and shows favorable results for the all-on-four technique with NDIs. The incidence of implant–prosthetic failures and biological and/or prosthetic complications were mostly related to smoking and/or the frequency of maintenance sessions [1,3,4,5]. In the present study, the overall treatment success was 94.1% due to three biological complications and four prosthetic complications that were successfully solved. The low incidence of complications could be related to the high motivation of the patients included in this retrospective study. Moreover, the reinforcement of oral hygiene instructions was constantly delivered to each patient at each professional hygiene session. Biological complications can occur in every implant-based rehabilitation, from a single tooth gap to complete arches. The need for bone augmentation procedures could increase the risk of early complications such as graft failures, membrane exposure, and infections of graft sites, adding a variable to the surgical phase. Moreover, late complications could also be reported after several years because of the stability of the regenerated bone over time [11]. These unfaithful events could determine a longer “time-to-teeth” for the patients, enhancing pain, discomfort, and the overall rehabilitation time [42]. Complications such as chipping or screw loosening could be frequent events with complete-arch implant-supported prostheses [6,19,20]. However, due to a lack of data in the literature, no other study investigated complete-arch rehabilitations supported by NDIs. The prosthetic complications reported in the current literature are only related to single-tooth replacements. In order to reduce technical and/or biological complications, the prosthetic manufacturing had to be carefully made to obtain long-term survival and success. In addition, constant maintenance sessions, including professional hygiene sessions, occlusion checks, and radiographic checks of the implant status, and the use of nightguards are mandatory to decrease the risk of complications. In addition, some biomechanical aspects have to be analyzed. NDIs in vitro showed a higher possibility of fracture in load tests. Türker et al. [29] reported in a finite element analysis that the coronal part of the implant is the most likely to receive high stress in maximum intercuspation. In this sense, the peri-implant bone on the most coronal part of the implant could be overstressed if the clenching of the jaws was observed while the patient was sleeping, which may lead to loss of osseointegration [28]. Osseointegration was quantified by calculating the bone to implant contact (BIC) and the bone area fraction occupancy (BAFO). These indexes are considered essential for implant stability and indications of successful osseointegration. Jimbo et al. [32] demonstrated that when the implant diameter increased, the histomorphometry values of BIC and BAFO inversely decreased. In these terms, standard and wide implants showed significantly lower values compared with narrow implants in a longer healing period without occlusal loading. However, it must be pointed out that increasing the diameter of the implants increases their ability to withstand bending and torsional forces and loading [33]. It seems that the overload on NDIs could be significantly reduced if they are splinted together compared to NDIs replacing a single-tooth gap. In the present study, only NDIs were positioned to perform complete-arch rehabilitations on four dental implants and fixed prostheses with titanium frameworks and acrylic teeth. The overload on the implants could have been reduced in the study sample because of the light load of the definitive prosthesis, in combination with several occlusal checks and the use of nightguards. The use of metal-based and ceramic heavy frameworks may increase the risk of overload, which may negatively influence the crestal parts of the dental implants. More RCTs are needed to improve the scientific data on complete-arch restorations supported only by NDIs. As a matter of fact, clinical investigations should focus on the differences between NDIs placed in native bone and standard-diameter implants placed in augmented bone in order to clarify and better understand the possibilities of NDIs.
5. Conclusions
The results of this retrospective study including patients treated with complete-arch restorations with screw-retained fixed prostheses supported by four NDIs showed encouraging results, and this protocol appears to be a possible alternative when extensive bone augmentation procedures are needed to place standard dental implants.
Author Contributions
Conceptualization, C.L. and F.L.; methodology, P.P.; software, A.L. and V.M.; validation, C.A., C.L. and P.P.; formal analysis, F.L. and V.M.; investigation, C.L.; resources, A.L.; data curation, A.L.; writing—original draft preparation, C.L.; writing—review and editing, F.L.; visualization, P.P.; supervision, C.A.; project administration, C.L. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Helsinki Declaration of 1964 and the revision in 2013 for ethical principles regarding human experimentation and with the written informed consent of the patients. The study was approved by the institutional review board of Sapienza University of Rome with protocol number 0000212 and was registered with protocol number ISRCTN16104700 (date 10/02/2022). The study was conducted following the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines (URL: http://www.strobe-statement.org (accessed on 20 December 2022)).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data from the present study can be obtained upon reasonable request from the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Pozzi, A.; Arcuri, L.; Fabbri, G.; Singer, G.; Londono, J. Long-term survival and success of zirconia screw-retained implant-supported prostheses for up to 12 years: A retrospective multicenter study. J Prosthet. Dent. 2021. [Google Scholar] [CrossRef] [PubMed]
- Maló, P.; Rangert, B.; Nobre, M. All-on-Four Immediate-Function Concept with Brånemark System® Implants for Completely Edentulous Mandibles: A Retrospective Clinical Study. Clin. Implant Dent. Relat. R. 2003, 5, 2–9. [Google Scholar] [CrossRef] [PubMed]
- Maló, P.; de Araújo Nobre, M.; Lopes, A.; Ferro, A.; Nunes, M. The All-on-4 concept for full-arch rehabilitation of the edentulous maxillae: A longitudinal study with 5–13 years of follow-up. Clin. Implant Dent. Relat. R. 2018, 21, 538–549. [Google Scholar] [CrossRef] [PubMed]
- Maló, P.; de Araújo Nobre, M.; Lopes, A.; Ferro, A.; Botto, J. The All-on-4 treatment concept for the rehabilitation of the completely edentulous mandible: A longitudinal study with 10 to 18 years of follow-up. Clin. Implant Dent. Relat. R. 2019, 21, 565–577. [Google Scholar] [CrossRef]
- Carosi, P.; Ferrigno, N.; Arcuri, C.; Laureti, M. Computer-Aided Surgery and Immediate Loading to Rehabilitate Complete Arch with Four Dental Implants and Fixed Screw-Retained Prosthesis Up to 4 Years in Function: A Retrospective Study. Int. J. Oral Max. Implant. 2021, 36, 1180–1187. [Google Scholar] [CrossRef]
- Pozzi, A.; Mura, P. Clinical and radiologic experience with moderately rough oxidized titanium implants: Up to 10 years of retrospective follow-up. Int. J. Oral Max. Implant. 2014, 29, 152–161. [Google Scholar] [CrossRef]
- Malo, P.; Rangert, B.; Nobre, M. All-on-4 Immediate-Function Concept with Branemark SystemR Implants for Completely Edentulous Maxillae: A 1-Year Retrospective Clinical Study. Clin. Implant Dent. Relat. R. 2005, 7, s88–s94. [Google Scholar] [CrossRef]
- Papi, P.; Carlo, S.D.; Rosella, D.; Angelis, F.D.; Capogreco, M.; Pompa, G. Peri-implantitis and extracellular matrix antibodies: A case-control study. Eur. J. Dent. 2017, 11, 340–344. [Google Scholar] [CrossRef]
- Storelli, S.; Caputo, A.; Palandrani, G.; Peditto, M.; Fabbro, M.D.; Romeo, E.; Oteri, G. Use of Narrow-Diameter Implants in Completely Edentulous Patients as a Prosthetic Option: A Systematic Review of the Literature. Biomed. Res. Int. 2021, 2021, 5571793. [Google Scholar] [CrossRef]
- González-Valls, G.; Roca-Millan, E.; Céspedes-Sánchez, J.M.; González-Navarro, B.; Torrejon-Moya, A.; López-López, J. Narrow Diameter Dental Implants as an Alternative Treatment for Atrophic Alveolar Ridges. Systematic Review and Meta-Analysis. Materials 2021, 14, 3234. [Google Scholar] [CrossRef]
- Valente, N.A.; Marchio, V.; Troiano, G.; Gasparro, R.; Balice, P.; Marenzi, G.; Laino, L.; Sammartino, G.; Lezzi, G.; Barone, A. Narrow-diameter versus standard-diameter implants placed in horizontally regenerated bone in the rehabilitation of partially and completely edentulous patients: A systematic review. Int. J. Oral Implant. 2022, 15, 11–33. [Google Scholar]
- Pozzi, A.; Arcuri, L.; Carosi, P.; Nardi, A.; Kan, J. Clinical and radiological outcomes of novel digital workflow and dynamic navigation for single-implant immediate loading in aesthetic zone: 1-year prospective case series. Clin. Oral Implant. Res. 2021, 32, 1397–1410. [Google Scholar] [CrossRef]
- Carosi, P.; Lorenzi, C.; Lio, F.; Cardelli, P.; Pinto, A.; Laureti, A.; Pozzi, A. Accuracy of Computer-Assisted Flapless Implant Placement by Means of Mucosa-Supported Templates in Complete-Arch Restorations: A Systematic Review. Materials 2022, 15, 1462. [Google Scholar] [CrossRef]
- Pozzi, A.; Moy, P.K. Minimally invasive transcrestal guided sinus lift (TGSL): A clinical prospective proof-of-concept cohort study up to 52 months. Clin. Implant. Dent. Relat. Res. 2014, 16, 582–593. [Google Scholar] [CrossRef]
- Cruz, R.S.; Lemos, C.A.A.; de Batista, V.E.S.; Yogui, F.C.; Oliveira, H.F.F.; Verri, F.R. Narrow-diameter implants versus regular-diameter implants for rehabilitation of the anterior region: A systematic review and meta-analysis. Int. J. Oral Max. Surg. 2021, 50, 674–682. [Google Scholar] [CrossRef]
- Bielemann, A.M.; Schuster, A.J.; da Rosa Possebon, A.P.; Schinestsck, A.R.; Chagas-Junior, O.L.; Faot, F. Clinical performance of narrow-diameter implants with hydrophobic and hydrophilic surfaces with mandibular implant overdentures: 1-year results of a randomized clinical trial. Clin. Oral Implant. Res. 2021, 33, 21–32. [Google Scholar] [CrossRef]
- Bielemann, A.M.; Marcello-Machado, R.M.; Schuster, A.J.; Júnior, O.L.C.; Cury, A.A.D.B.; Faot, F. Healing differences in narrow diameter implants submitted to immediate and conventional loading in mandibular overdentures: A randomized clinical trial. J. Periodontal Res. 2018, 54, 241–250. [Google Scholar] [CrossRef]
- Marcello-Machado, R.M.; Faot, F.; Schuster, A.J.; Bielemann, A.M.; Júnior, O.L.C.; Cury, A.A.D.B. One-year clinical outcomes of locking taper Equator attachments retaining mandibular overdentures to narrow diameter implants. Clin. Implant. Dent. R. 2017, 20, 483–492. [Google Scholar] [CrossRef]
- Papaspyridakos, P.; Bordin, T.B.; Kim, Y.J.; El-Rafie, K.; Pagni, S.E.; Natto, Z.S.; Teixeira, E.R.; Chochlidakis, k.; Weber, H.-P. Technical Complications and Prosthesis Survival Rates with Implant-Supported Fixed Complete Dental Prostheses: A Retrospective Study with 1- to 12-Year Follow-Up. J. Prosthodont. Off. J. Am. Coll. Prosthodont. 2019, 29, 3–11. [Google Scholar] [CrossRef]
- Chochlidakis, K.; Einarsdottir, E.; Tsigarida, A.; Papaspyridakos, P.; Romeo, D.; Barmak, A.B.; Ercoli, C. Survival rates and prosthetic complications of implant fixed complete dental prostheses: An up to 5-year retrospective study. J. Prosthet. Dent. 2020, 124, 539–546. [Google Scholar] [CrossRef]
- Jung, R.E.; Al-Nawas, B.; Araujo, M.; Bartner, S.; Brodala, N.; Chappuis, V.; Chen, B.; De Souza, A.; Almeida, R.F.; Fickl, S.; et al. Group 1 ITI Consensus Report: The influence of implant length and design and medications on clinical and patient-reported outcomes. Clin. Oral Implant. Res. 2018, 29, 69–77. [Google Scholar] [CrossRef] [PubMed]
- Roccuzzo, A.; Imber, J.; Jensen, S.S. Need for lateral bone augmentation at two narrow-diameter implants: A prospective, controlled, clinical study. Clin. Oral Implant. Res. 2021, 32, 511–520. [Google Scholar] [CrossRef] [PubMed]
- Antiua, E.; Escuer, V.; Alkhraisat, M.H. Short Narrow Dental Implants versus Long Narrow Dental Implants in Fixed Prostheses: A Prospective Clinical Study. Dent. J. 2022, 10, 39. [Google Scholar] [CrossRef] [PubMed]
- Parize, H.N.; Bohner, L.O.L.; Gama, L.T.; Porporatti, A.L.; Mezzomo, L.A.M.; Christopher, W.; Gonçalves, T.M.S.V. Narrow-diameter implants in the anterior region: A meta-analysis. Int. J. Oral Max. Implant. 2019, 34, 1347–1358. [Google Scholar] [CrossRef] [PubMed]
- Schiegnitz, E.; Al-Nawas, B. Narrow-diameter implants: A systematic review and meta-analysis. Clin. Oral Implant. Res. 2018, 29, 21–40. [Google Scholar] [CrossRef]
- Reis, R.; Nicolau, P.; Calha, N.; Messias, A.; Guerra, F. Immediate versus early loading protocols of titanium-zirconium narrow-diameter implants for mandibular overdentures in edentulous patients: 1-year results from a randomized controlled trial. Clin. Oral Implant. Res. 2019, 30, 953–961. [Google Scholar] [CrossRef]
- Coskunses, F.M.; Tak, Ö. Clinical performance of narrow-diameter titanium–zirconium implants in immediately loaded fixed full-arch prostheses: A 2-year clinical study. Int. J. Implant. Dent. 2021, 7, 30. [Google Scholar] [CrossRef]
- Beddis, H.; Pemberton, M.; Davies, S. Sleep bruxism: An overview for clinicians. Brit. Dent. J. 2018, 225, 497–501. [Google Scholar] [CrossRef]
- Türker, N.; Büyükkaplan, U.S.; Sadowsky, S.J.; Özarslan, M.M. Finite Element Stress Analysis of Applied Forces to Implants and Supporting Tissues Using the All-on-Four Concept with Different Occlusal Schemes. J. Prosthodont. Off. J. Am. Coll. Prosthodont. 2018, 28, 185–194. [Google Scholar] [CrossRef]
- Klein, M.; Schiegnitz, E.; Al-Nawas, B. Systematic Review on Success of Narrow-Diameter Dental Implants. Int. J. Oral Max. Implant. 2014, 29, 43–54. [Google Scholar] [CrossRef]
- Tsigarida, A.; Chochlidakis, K.; Fraser, D.; Lampraki, E.; Einarsdottir, E.R.; Barmak, A.B.; Papaspyridakos, P.; Ercoli, C. Peri-Implant Diseases and Biologic Complications at Implant-Supported Fixed Dental Prostheses in Partially Edentulous Patients. J. Prosthodont. Off. J. Am. Coll. Prosthodont. 2020, 29, 429–435. [Google Scholar] [CrossRef]
- Jimbo, R.; Janal, M.N.; Marin, C.; Giro, G.; Tovar, N.; Coelho, P.G. The effect of implant diameter on osseointegration utilizing simplified drilling protocols. Clin. Oral Implant. Res. 2013, 25, 1295–1300. [Google Scholar] [CrossRef]
- Do Carmo Filho, L.C.; Faot, F.; de Matos Madruga, M.; Machado, R.M.M.; Bordin, D.; Cury, A.A.D.B. Effect of implant macrogeometry on peri-implant healing outcomes: A randomized clinical trial. Clin. Oral Investig. 2018, 23, 567–575. [Google Scholar] [CrossRef]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vanderbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for reporting observational studies. Int. J. Surg. 2014, 12, 1495–1499. [Google Scholar] [CrossRef]
- Harris, D.; Horner, K.; Gröndahl, K.; Jacobs, R.; Helmrot, E.; Benic, G.I.; Bornstein, M.M.; Dawood, A.; Quirynen, M.E.A.O. guidelines for the use of diagnostic imaging in implant dentistry A consensus workshop organized by the European Association for Osseointegration at the Medical University of Warsaw. Clin. Oral Implant. Res. 2012, 23, 1243–1253. [Google Scholar] [CrossRef]
- Misch, C.E.; Perel, M.L.; Wang, H.L.; Sammartino, G.; Galindo-Moreno, P.; Trisi, P.; Steigmann, M.; Rebaudi, A.; Palti, A.; Pikos, M.A.; et al. Implant Success, Survival, and Failure: The International Congress of Oral Implantologists (ICOI) Pisa Consensus Conference. Implant. Dent. 2008, 17, 5–15. [Google Scholar] [CrossRef]
- Albrektsson, T.; Johansson, C. Osteoinduction, osteoconduction and osseointegration. Eur. Spine J. 2001, 10, S96–S101. [Google Scholar]
- Heitz-Mayfield, L.; Needleman, I.; Salvi, G.E.; Pjetursson, B.E. Consensus statements and clinical recommendations for prevention and management of biologic and technical implant complications. Int. J. Oral Max. Implant. 2014, 29, 346–350. [Google Scholar] [CrossRef]
- Papaspyridakos, P.; Bordin, T.B.; Kim, Y.J.; Defuria, C.; Pagni, S.E.; Chochlidakis, K.; Teixeira, E.R.; Weber, H.-P. Implant survival rates and biologic complications with implant-supported fixed complete dental prostheses: A retrospective study with up to 12-year follow-up. Clin. Oral Implant. Res. 2018, 29, 881–893. [Google Scholar] [CrossRef]
- Carosi, P.; Ottria, L.; Lio, F.; Laureti, A.; Papi, P. The health of soft tissues around four dental implants loaded immediately supporting a 4-year-old fixed screw-retained prosthesis. J. Biol. Regul. Homeost. Agents 2021, 35, 57–66. [Google Scholar] [CrossRef]
- Ravida, A.; Siqueira, R.; Di Gianfilippo, R.; Kaur, G.; Giannobile, A.; Galindo Moreno, P.; Wang, C.-W.; Wang, H.-L. Prognostic factors associated with implant loss, disease progression or favorable outcomes after peri-implantitis surgical therapy. Clin. Implant. Dent. Relat. Res. 2022, 24, 222–232. [Google Scholar] [CrossRef] [PubMed]
- Papi, P.; Di Murro, B.; Penna, D.; Pompa, G. Digital prosthetic workflow during COVID-19 pandemic to limit infection risk in dental practice. Oral Dis. 2021, 27, 723–726. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).