1. Introduction
1.1. Smart Healthcare Systems
Smart healthcare systems enable users/patients and related parties in the healthcare sector, such as doctors and nurses, to access, collect, and manage medical data and information quickly and accurately, and to assist in recommending or supporting decisions in the healthcare sector. Still in their early stages of development, smart healthcare systems provide several focused service functions in which software and hardware are integrated to optimize the complete service of the smart healthcare system. Several technological developments in the field of smart healthcare systems help to treat patient illnesses and support the optimization of doctors’ health services, whereas, in general, a smart healthcare system’s architecture consists of software and hardware [
1]. Challenges and supporting technology in a smart healthcare system are indicators that cannot be abandoned. The need (for various types of disease and services) is increasing every day in terms of both hardware and software technology. This, of course, requires appropriate integration so that service needs can be met, assisted by the development of adequate hardware and software technology. Several related studies apply the principles of smart healthcare systems in responding to existing challenges and needs [
2].
1.2. Smart Healthcare Systems
Diabetes mellitus (DM) is a metabolic disorder that leads to high blood sugar levels. In addition to type 2 diabetes, there is also type 1 diabetes. Diabetes causes hyperglycemia because the pancreas cannot produce enough insulin. Under other conditions, the pancreas can produce insulin, but the insulin it produces cannot be used optimally. Both of these conditions can cause blood sugar spikes in diabetics [
3].
Diabetes (DM) is generally divided into type 1 diabetes, or insulin-dependent diabetes mellitus; type 2 diabetes, or non-insulin-dependent diabetes mellitus; other types of diabetes mellitus; and gestational diabetes mellitus (
Table 1). Type 2 diabetes is a metabolic disorder characterized by hyperglycemia due to insulin resistance and/or deficiency. Patients with type 2 diabetes mellitus (T2DM) need DM management to properly and regularly control their blood glucose levels. Blood sugar levels can increase and decrease in an unstable manner if type 2 DM sufferers do not control their blood sugar levels properly, which can trigger complications [
4]. Diabetes mellitus control is carried out using the basic principles of diabetes mellitus control management, including the modification of unhealthy lifestyles to become healthy in the form of diet, physical exercise, and adherence to antidiabetic drug consumption [
5].
Self-management is an integral part of diabetes control. Self-care management of diabetes can effectively reduce the risk of DM (
Table 2) sufferers having coronary heart complications; in addition, self-care can control normal blood sugar levels, reduce the impact of DM problems, and reduce DM mortality [
10,
11]. Self-care performed by DM patients includes diet, eating habits, exercise, monitoring blood sugar levels, medication, and diabetic foot care. Efforts to overcome the weakness of self-care management of type 2 DM in controlling blood glucose levels that develop in the community to minimize DM complications can be assisted by utilizing technological developments [
12].
1.3. Development Mobile Application
ICT (Information and Communication Technology) is a tool that provides added value by generating high-speed, complete, accurate, transparent, and up-to-date information. The era of information and communication technology is being used to increase the provision of health information. Researchers are trying to innovate to develop diabetes care applications that take advantage of technological developments in providing information for self-care management in controlling blood glucose levels. The diabetes care application is expected to be able to answer the problem as a smart solution to minimize complications that arise in Type 2 diabetes mellitus (T2DM) patients [
15].
Android is an operating system for Linux-based mobile devices that appears among other operating systems currently under development with a good set of supported features (
Table 3). However, current development operating systems run in a way that prioritizes internally built core applications without taking into account the significant functionality of third-party applications [
16]. Therefore, there are restrictions on third-party applications that can capture native mobile data and communicate between processes, and there are restrictions on distributing third-party applications to the platform. An application is a special set of instructions on a computer designed for us to complete certain tasks.
1.4. Previous Research
The Android mobile application’s first development efforts were devoted to managing Type 2 diabetes. At this stage, the research team involved 20 people, consisting of 10 people with diabetes and 10 people without diabetes, in the use of diabetes mobile applications with supporting hardware, namely a wearable band, glucose meter, and treadmill [
18]. The results of the initial research were used as reference material for the development of the second stage. At this stage, the researchers evaluated some of the functionality and accessibility of the application by conducting tests involving 40 people, consisting of 20 people with diabetes and 20 people without diabetes. The results of the second stage of research concluded that there was a need for changes and adaptation of applications for users, especially related to user registration for applications and glucometer and wearable band (smartwatch) connectivity with various versions [
19]. Previous researchers have conducted preliminary research through two previous studies (
Table 4).
2. Analysis
2.1. Application in Healthcare
An application in healthcare is a program created by a user that aims to complete a specific task (
Table 5). An application is the storage of data, problems, and work in a container or medium that can be used to implement or implement existing things or problems in a new form without losing the fundamental values of the data, problems, and work itself [
20].
The application can be categorized into three groups in its development, namely [
21]:
- (a)
Desktop applications, namely applications that can only be run on a PC or laptop.
- (b)
Web applications, namely applications that are run using a computer or laptop and an internet connection.
- (c)
Mobile applications, namely applications that run on mobile devices.
2.2. Mobile Technology and Operating System
A mobile phone is a portable electronic device that functions like a regular phone and can be moved over a wide area. While mobile phones currently use a combination of wireless transmission and traditional telephone circuit switching, packet switching is used in parts of the mobile phone network, especially for Internet access and WAP services [
22]. Mobile phones, or “cell phones”, are electronic communication devices that have the same basic functionality as traditional landlines, but they can be carried anywhere (mobile) and do not need to be connected to a phone network using a cable (wireless) [
23].
The mobile operating system is the primary software that directly manages and controls the hardware, and also manages and controls other software so that it can function (
Table 6). Therefore, the mobile operating system is responsible for manipulating the various features and functions available on mobile devices. tasks, keyboards, WAPs, emails, text message scheduling, synchronization with other applications and devices, music playback, cameras, and control features [
24]. In addition to the ability to control mobile phone hardware and software resources such as keyboards, screens, phonebooks, batteries, and network connections, the operating system controls all applications to run consistently and consistently. The operating system needs to be flexible so that software developers can easily create sophisticated new applications [
25].
2.3. Telehealth
Telecare is a part of telehealth. Telecare focuses on the therapeutic side, while telemedicine covers the prophylactic, preventive, and therapeutic aspects [
26]. One of the functions of telehealth, and a major requirement in providing health services, is patient monitoring and scheduling. The coverage of telehealth, telemedicine, and electronic health (e-health), telecare, and m-health is described by Totten AM et al. [
27].
3. Research Methodology
3.1. Research Method
The research was conducted at the Circuit and System Design Laboratory at Kangwon National University. The research was performed by carrying out several systematic stages (
Figure 1) in order to produce research reports and products (Mobile Application) that were in accordance with the objectives of the research implementation. The research method included six stages, starting with identification of the problem, setting the research scope, data and information gathering, software development, analysis, and the final report.
3.2. Software Development Methodology
In developing this application, we used the prototype model [
28] as an approach to mobile application development. We performed three stages: creating and revising the mockup, conducting customer test drives, and listening to customers. All steps in this prototype model were chosen because they were in accordance with the project being developed, which does not have many stages, and the parties or teams involved can also be maximized in the three existing stages [
29,
30].
4. Proposed Architecture
4.1. Mobile Application
The development of the architecture (
Figure 2) for the Type 2 Diabetic Mellitus Mobile Application is broadly divided into three major parts:
Medical sensors in the architecture section include supporting devices (inputs) in the form of wearable bands, glucose meters, and heart rate sensors. The exercise equipment consists of a gym cycle and a treadmill. In this section, the device is Bluetooth- and RFID-compatible. In this section, the device will work for the next stage of data acquisition before going to the transmission section.
Transmission in the architecture section consists of smartphone applications and cloud storage. In this section, the smartphone application receives input data from the Medical Sensor and Exercise Equipment section, which is referred to as the data acquisition process. The processed data are stored in cloud storage, and in this part of the process, the entire process is supported by the Internet network.
Information on the architecture is the final part (output), namely the process after the data are processed in the transmission section. The process at this stage is called “real-time exercise data”, where the processed data can be received at the same time by the user (patient) with an Internet connection as network support.
4.2. Hardware Design and Implementation
The hardware design and implementation for the Type 2 Diabetes Mellitus Mobile Applications are written in block diagram format (
Figure 3). Eight blocks (
Figure 3) consist of RFID, DAQ for Treadmill and Gym Cycle, Heart Rate Sensor, Wearable Band, Glucometer, Signal Integration, Calculation and Memory, Smartphone Application, and Patient. The first five blocks consist of RFID, DAQ for Treadmill and Gym Cycle, Heart Rate Sensor, Wearable Band, and Glucometer, which interact with the Signal Integration, Calculation and Memory block, which in turn send User ID, Exercise Data, Heart Rate, Number of steps, Heart Rate and Blood Glucose Levels, where the data received in the Signal Integration, Calculation, and Memory block will interact with the smartphone application block to send Real-Time Exercise data. The last block is where the patient interacts with the smartphone application block, which is a process of real-time monitoring alerts.
4.3. Sensor
The sensor is one part of the Type 2 Diabetes Mellitus Mobile Application. In
Figure 4, the architecture of sensors is clearly described, starting from the deployment of sensors, active sensors taking measurements, reading RFID tags, and entering mobile applications. Then, in the stage of analyzing the measurement, there will be two choices: namely, updating details in storage with normal or above-normal conditions, or storing the updated data in the database and receiving real-time monitoring alerts.
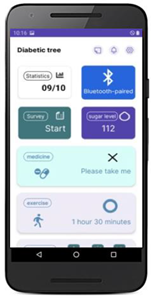
4.4. Sensor User Interface
The user interface (UI) is what the user interacts with as part of an experience (
Table 7). UI is not just about colors and shapes; it is about providing users with the right tools to achieve their goals. In addition, UI is more than just buttons, menus, and forms that the user must fill out. When the system and users can interact with each other through commands such as using content and entering data, this is referred to as a user interface. The user interface is one of the most important parts of application development because it relates to the user and can be seen, heard, and touched. At this stage, the researchers developed a user interface related to the appropriate needs and related to the development of the Type 2 Diabetes Mellitus Mobile Application.
5. Testing
Researchers conducted an evaluation stage on the development of a diabetes mobile application for 40 participants who were users of mobile-based diabetes applications (diabetic patients). Evaluation of user acceptance testing for mobile applications (
Figure 5) adapted five main factors at the application testing stage (
Table 8), which included functionality, ease of use, usefulness, security and privacy, and cost factors. Based on the results of the evaluation using a Likert scale (strongly agree, agree, neutral, disagree, strongly disagree) with an assessment weight of (5, 4, 3, 2, 1), the average value of factor functionality was 4.57, ease of use 4.67, usefulness 4.75, security and privacy 5.0, and cost 4.70. Based on the results of this evaluation, there are two indicators that have an evaluation value with an input value of 3 (neutral), namely the functionality and ease of use factors.
6. Summary and Conclusions
The development of the Type 2 Diabetes Mellitus Mobile Application involves an operational feature that allows an application to run according to specified requirements and can integrate an Android-based mobile application with supporting hardware such as a glucometer, wearable band, heart rate sensor, treadmill, and gym cycle. The provided features in this mobile application include monitoring medication, food intake, exercise, and sleep. Architectural Design for Diabetic Mobile Applications, Hardware Block Diagram Design, and Architecture of Sensors will be useful for the application development team as a benchmark or guideline for what kind of application or product will be produced. Based on the results of the analysis, this study resulted in three proposed architectures: namely, the architecture for mobile applications, the hardware block diagram, and the architecture of sensors, which clearly describe the operational functions that exist in the Type 2 Diabetes Mellitus Mobile Application. On the other hand, the architectural design will support the success rate of application development, so that applications can be useful and optimally utilized both by patients and doctors involved in the treatment of type 2 diabetes (T2DM). This study is also intended to serve as a reference for researchers who are currently conducting or will be conducting research in the field of developing type 2 diabetes mobile applications.
Author Contributions
S.R.J.: project evaluation, methodology, investigation, resources, supervision. W.A.: software developer, functionality evaluation. J.-H.L.: conceptualization, funding acquisition, resources, supervision, writing—original draft, writing—review and editing. All authors have read and agreed to the published version of the manuscript.
Funding
This research was supported by “Regional Innovation Strategy (RIS)” through the National Research Foundation of Korea (NRF), funded by the Ministry of Education (MOE) (2022RIS-005).
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Abd-alrazaq, A.A.; Suleiman, N.; Baagar, K.; Jandali, N.; Alhuwail, D.; Abdalhakam, I.; Shahbal, S.; Abou-Samra, A.; Househ, M. Patients and healthcare workers experience with a mobile application for self-management of diabetes in Qatar: A qualitative study. Comput. Methods Programs Biomed. Update 2021, 1, 100002. [Google Scholar] [CrossRef]
- Adu, M.D.; Malabu, U.H.; Malau-Aduli, A.E.; Malau-Aduli, B.S. Mobile application intervention to promote self-management in insulin-requiring type 1 and type 2 diabetes individuals: Protocol for a mixed methods study and non-blinded randomized controlled trial. Diabetes Metab. Syndr. Obes. 2019, 12, 789–800. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Adu, M.D.; Malabu, U.H.; Malau-Aduli, A.E.; Malau-Aduli, B.S. The development of My Care Hub Mobile-Phone App to Support Self-Management in Australians with Type 1 or Type 2 Diabetes. Sci. Rep. 2020, 10, 7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Höll, B.; Spat, S.; Plank, J.; Schaupp, L.; Neubauer, K.; Beck, P.; Chiarugi, F.; Kontogiannis, V.; Pieber, T.R.; Holzinger, A. Design of a Mobile, Safety-Critical in-Patient Glucose Management System. Stud. Health Technol. Inf. 2011, 169, 950–954. [Google Scholar]
- Jeffrey, B.; Bagala, M.; Creighton, A.; Leavey, A.; Nicholls, S.; Wood, C.; Longman, J.; Barker, J.; Pit, S. Mobile phone applications and their use in the self-management of Type 2 Diabetes Mellitus: A qualitative study among app users and non-app users. Diabetol. Metab. Syndr. 2019, 11, 84. [Google Scholar] [CrossRef]
- Sultan, A.; Murtaza, K.; Mohammed, A. Mobile Health (m-Health) System in the Context of IoT. In Proceedings of the IEEE 4th International Conference on Future Internet of Things and Cloud Workshops (FiCloudW), Vienna, Austria, 22–24 August 2016; pp. 39–42. [Google Scholar]
- Totten, A.M.; Womack, D.M.; Eden, K.B. Telehealth: Mapping the Evidence for Patient Outcomes from Systematic Reviews; Pacific Northwest Evidence-based Practice Center Portland, OR, Technical Briefs, No. 26; Agency for Healthcare Research and Quality: Rockville, MD, USA, 2016; pp. 1–125.
- Hasan, A.M.Y.; Alina, S.; Nor, A. The Role of Different Types of Information Systems in Business Organizations: A Review. Int. J. Res. 2014, 1, 1270–1286. [Google Scholar]
- Naseer, A.; Muhammad, B.W.; Abdul, H.M. Comparative Analysis of Operating System of Different Smart Phones. J. Softw. Eng. Appl. 2015, 8, 114. [Google Scholar]
- Spanakis, E.G.; Chiarugi, F.; Kouroubali, A.; Spat, S.; Beck, P.; Asanin, S.; Rosengren, P.; Gergely, T.; Thestrup, J. Diabetes management using modern information and communication technologies and new care models. Interact. J. Med. Res. 2012, 1, e2193. [Google Scholar] [CrossRef]
- Helen, F.N.C.; Jin, J.D.; Terrence, A.J. Content Analysis: First-Time Patient User Challenges with Top-Rated Commercial Diabetes Apps. Telemed. E-Health 2021, 27, 663–669. [Google Scholar]
- Gunawardena, K.C.; Jackson, R.; Robinett, I.; Dhaniska, L.; Jayamanne, S.; Kalpani, S.; Muthukuda, D. The Influence of the Smart Glucose Manager Mobile Application on Diabetes Management. J. Diabetes Sci. Technol. 2019, 13, 75–81. [Google Scholar] [CrossRef] [Green Version]
- Fernanda, C.F.; Thamiris, L.A.C.; Emerson, P.C.; Adriana, S.P.; Ilka, A.R.; Heloísa, C.T. Mobile applications for adolescents with type 1 diabetes mellitus: Integrative literature review. Acta Paul Enferm. 2017, 30, 565–572. [Google Scholar]
- Kumar, D.S.; Prakash, B.; Chandra, B.J.S.; Shrinivas, K.P.; Vanishri, A.; Jom, T.J.; Praveen, K.; Arun, G.; Murthy, M.R.N. Technological innovations to improve health outcome in type 2 diabetes mellitus: A randomized controlled study. Clin. Epidemiol. Glob. Health 2021, 9, 53–56. [Google Scholar] [CrossRef]
- Slagle, H.B.G.; Hoffman, M.K.; Caplan, R.; Shlossman, P.; Sciscione, A.C. Validation of a novel mobile phone application for type 2 diabetes screening following gestational diabetes mellitus. mHealth 2022, 8, 21–36. [Google Scholar]
- Contreras, I.; Vehi, J. Artificial Intelligence for Diabetes Management and Decision Support: Literature Review. J. Med. Internet Res. 2018, 20, e10775. [Google Scholar] [CrossRef] [PubMed]
- Maryam, J.; Asghar, E.; Shekoufeh, A. Developing “Aryan:” Diabetes self-care mobile application. Int. J. Prev. Med. 2019, 10, 59. [Google Scholar]
- Lee, J.-H.; Park, J.-C.; Kim, S.-B. Therapeutic Exercise Platform for Type-2 Diabetic Mellitus. Electronics 2021, 10, 1820. [Google Scholar] [CrossRef]
- Bults, M.; van Leersum, C.M.; Olthuis, T.J.J.; Bekhuis, R.E.M.; den Ouden, M.E.M. Barriers and Drivers Regarding the Use of Mobile Health Apps Among Patients With Type 2 Diabetes Mellitus in the Netherlands: Explanatory Sequential Design Study. Jmir Diabetes 2022, 7, e31451. [Google Scholar] [CrossRef]
- Christian, M.; Isabel, S.; Stephan, M. User Experience Testing of My ePRO App in a Diabetes Mellitus Type 2 Focus Group. Int. J. Clin. Exp. Med Sci. 2022, 11, 8. [Google Scholar]
- García, M.F.; Porras, Y.; Richmond, D.; Jensen, M.; Madrigal, M.; Zúñiga, G. Designing a Mobile Application to Support Type 2 Diabetes Mellitus Care in Costa Rica: A Qualitative Exploratory Study. J. Acad. Nutr. Diabet. 2016, 116, A75. [Google Scholar] [CrossRef]
- Kebede, M.M.; Pischke, C.R. Popular Diabetes Apps and the Impact of Diabetes App Use on Self-Care Behaviour: A Survey Among the Digital Community of Persons with Diabetes on Social Media. Front. Endocrinol. 2019, 10, 135. [Google Scholar] [CrossRef] [Green Version]
- Michael, O.A.; Taiwo, R.H.; Oluwabukola, A.A.; Joseph, F.O. Mobile phone ownership and willingness to receive mHealth services among patients with diabetes mellitus in South-West, Nigeria. Panafrican Med. J. 2020, 37, 29. [Google Scholar]
- Park, J.C.; Kim, S.; Lee, J.-H. Self-Care IoT Platform for Diabetic Mellitus. Appl. Sci. 2021, 11, 5. [Google Scholar] [CrossRef]
- Więckowska, R.K.; Justyna, D.; Grażyna, D. The usefulness of the nutrition apps in self-control of diabetes mellitus – the review of literature and own experience. Pediatric Endocrinol. Diabetes Metab. 2022, 28, 75–80. [Google Scholar] [CrossRef]
- Joshua, S.R. Analysis and Design of Service Oriented Architecture Based in Public Senior High School Academic Information System. IEEE Xplore 2017, 180–186. [Google Scholar]
- Zeadally, S.; Siddiqui, F.; Baig, Z.; Ibrahim, A. Smart healthcare Challenges and potential solutions using internet of things (IoT) and big data analytics. Psu Res. Rev. 2020, 4, 93–109. [Google Scholar]
- Chomutare, T.; Fernandez-Luque, L.; Årsand, E.; Hartvigsen, G. Features of Mobile Diabetes Applications: Review of the Literature and Analysis of Current Applications Compared Against Evidence-Based Guidelines. J. Med. Internet Res. 2011, 13, e1874. [Google Scholar] [CrossRef] [Green Version]
- Pritee, U.S.; Rani, P.T.; Deepak, D.S.; Umesh, J.P. A Literature Review on Android—A Mobile Operating system. Int. Res. J. Eng. Technol. 2021, 8, 1–6. [Google Scholar]
- Quy, V.K.; Hau, N.V.; Anh, D.V.; Ngoc, L.A. Smart healthcare IoT applications based on fog computing: Architecture, applications and challenges. Complex Intell. Syst. 2022, 8, 3805–3815. [Google Scholar] [CrossRef]
| Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).