Old and Novel Predictors for Cardiovascular Risk in Diabetic Foot Syndrome—A Narrative Review
Abstract
:1. Diabetes Mellitus and the Cardiovascular Continuum
2. Materials and Methods
3. Past, Present and Future in Assessing the Cardiovascular Risk
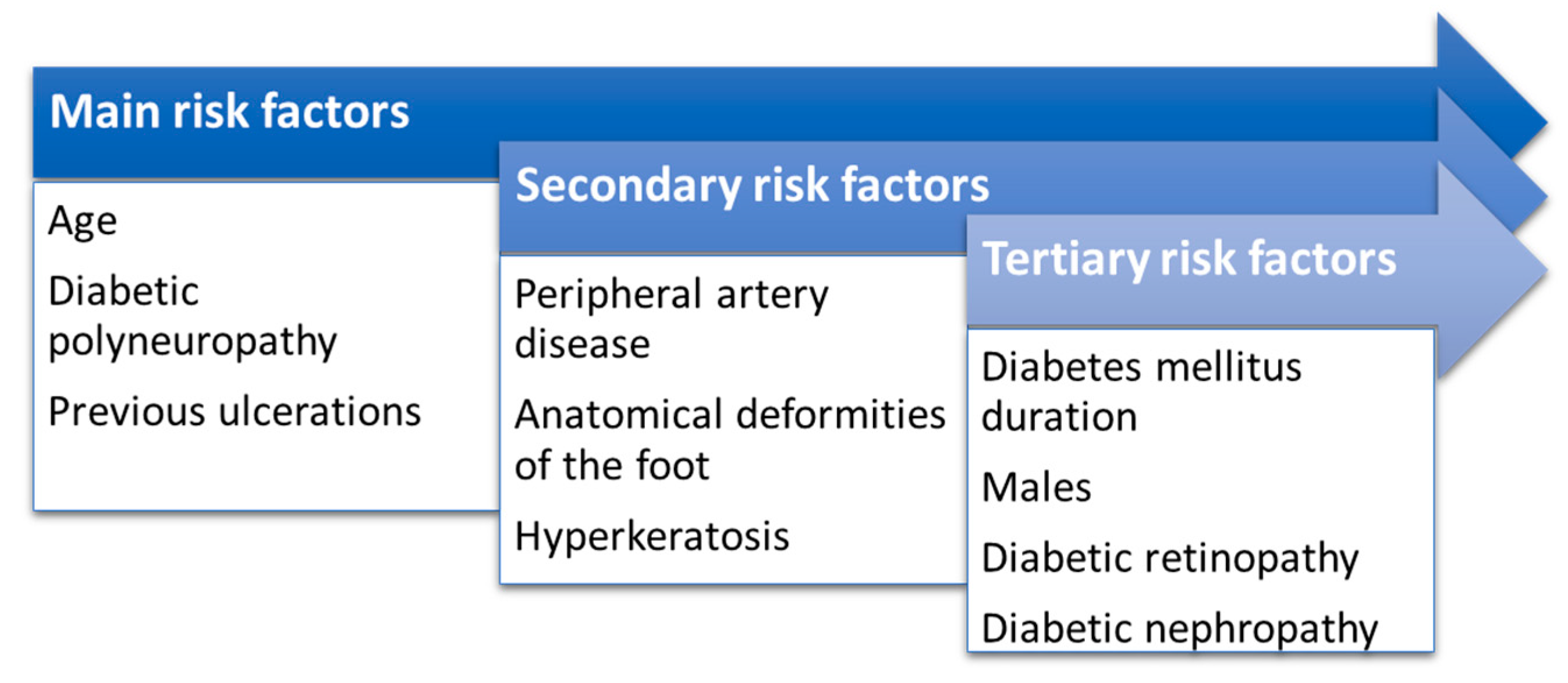
4. Diabetic Foot Syndrome
5. Discussions
5.1. Cardio-Diabetology: The Role of Biomarkers and Inflammatory Molecules
5.2. Diabetic Foot Syndrome and Diabetic Cardiomyopathy
6. Future Directions
6.1. The Role of Artificial Intelligence in Assessing CVD Risk in DM
6.2. Predictive Risk Models for CVD Events in DM
6.3. Novel Therapeutic Targets
7. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Sakran, N.; Graham, Y.; Pintar, T.; Yang, W.; Kassir, R.; Willigendael, E.M.; Singhal, R.; Kooreman, Z.E.; Ramnarain, D.; Mahawar, K.; et al. The Many Faces of Diabetes. Is There a Need for Re-Classification? A Narrative Review. BMC Endocr. Disord. 2022, 22, 9. [Google Scholar] [CrossRef] [PubMed]
- Zhang, G.Q.; Canner, J.K.; Haut, E.; Sherman, R.L.; Abularrage, C.J.; Hicks, C.W. Impact of Geographic Socioeconomic Disadvantage on Minor Amputation Outcomes in Patients with Diabetes. J. Surg. Res. 2021, 258, 38–46. [Google Scholar] [CrossRef] [PubMed]
- Sharma, A.; Mittal, S.; Aggarwal, R.; Chauhan, M.K. Diabetes and Cardiovascular Disease: Inter-Relation of Risk Factors and Treatment. Future J. Pharm. Sci. 2020, 6, 130. [Google Scholar] [CrossRef]
- Jalilian, M.; Ahmadi Sarbarzeh, P.; Oubari, S. Factors Related to Severity of Diabetic Foot Ulcer: A Systematic Review. Diabetes Metab. Syndr. Obes. Targets Ther. 2020, 13, 1835–1842. [Google Scholar] [CrossRef]
- Awasthi, A.; Singh, S.K.; Kumar, B.; Gulati, M.; Kumar, R.; Wadhwa, S.; Khursheed, R.; Corrie, L.; Kr, A.; Kumar, R.; et al. Treatment Strategies Against Diabetic Foot Ulcer: Success so Far and the Road Ahead. Curr. Diabetes Rev. 2021, 17, 421–436. [Google Scholar] [CrossRef]
- Rosinha, P.; Saraiva, M.; Ferreira, L.; Garrido, S.; Carvalho, A.; Freitas, C.; Amaral, C.; Costa, L.; Loureiro, L.; Carvalho, R. A Retrospective Cohort Study on Diabetic Foot Disease: Ascertainment of Ulcer Locations by Age Group. Cureus 2022, 14, e28189. [Google Scholar] [CrossRef]
- Roglic WHO Global Report on Diabetes: A Summary. Available online: https://www.ijncd.org/article.asp?issn=2468-8827;year=2016;volume=1;issue=1;spage=3;epage=8;aulast=Roglic (accessed on 20 December 2022).
- Saeedi, P.; Petersohn, I.; Salpea, P.; Malanda, B.; Karuranga, S.; Unwin, N.; Colagiuri, S.; Guariguata, L.; Motala, A.A.; Ogurtsova, K.; et al. Global and Regional Diabetes Prevalence Estimates for 2019 and Projections for 2030 and 2045: Results from the International Diabetes Federation Diabetes Atlas, 9th Edition. Diabetes Res. Clin. Pract. 2019, 157, 107843. [Google Scholar] [CrossRef]
- Shrestha, N.; Karki, K.; Poudyal, A.; Aryal, K.K.; Mahato, N.K.; Gautam, N.; Kc, D.; Gyanwali, P.; Dhimal, M.; Jha, A.K. Prevalence of Diabetes Mellitus and Associated Risk Factors in Nepal: Findings from a Nationwide Population-Based Survey. BMJ Open 2022, 12, e060750. [Google Scholar] [CrossRef]
- Costa, D.; Ielapi, N.; Caprino, F.; Giannotta, N.; Sisinni, A.; Abramo, A.; Ssempijja, L.; Andreucci, M.; Bracale, U.M.; Serra, R. Social Aspects of Diabetic Foot: A Scoping Review. Soc. Sci. 2022, 11, 149. [Google Scholar] [CrossRef]
- Yan, R.; Yu, F.; Strandlund, K.; Han, J.; Lei, N.; Song, Y. Analyzing Factors Affecting Quality of Life in Patients Hospitalized with Chronic Wound. Wound Repair Regen. 2021, 29, 70–78. [Google Scholar] [CrossRef]
- Shankar, P.; Grewal, V.S.; Agrawal, S.; Nair, S.V. A Study on Quality of Life among Lower Limb Amputees at a Tertiary Prosthetic Rehabilitation Center. Med. J. Armed Forces India 2020, 76, 89–94. [Google Scholar] [CrossRef] [PubMed]
- Pedras, S.; Vilhena, E.; Carvalho, R.; Pereira, M.G. Quality of Life Following a Lower Limb Amputation in Diabetic Patients: A Longitudinal and Multicenter Study. Psychiatry 2020, 83, 47–57. [Google Scholar] [CrossRef] [PubMed]
- Yogal, C.; Shakya, S.; Karmarcharya, B.; Koju, R.; Stunes, A.K.; Mosti, M.P.; Gustafsson, M.K.; Åsvold, B.O.; Schei, B.; Syversen, U. Diabetes Prevalence and Associated Risk Factors among Women in a Rural District of Nepal Using HbA1c as a Diagnostic Tool: A Population-Based Study. Int. J. Environ. Res. Public Health 2022, 19, 7011. [Google Scholar] [CrossRef] [PubMed]
- Manicardi, V.; Russo, G.; Napoli, A.; Torlone, E.; Li Volsi, P.; Giorda, C.B.; Musacchio, N.; Nicolucci, A.; Suraci, C.; Lucisano, G.; et al. Gender-Disparities in Adults with Type 1 Diabetes: More Than a Quality of Care Issue. A Cross-Sectional Observational Study from the AMD Annals Initiative. PLoS ONE 2016, 11, e0162960. [Google Scholar] [CrossRef] [PubMed]
- Ciarambino, T.; Crispino, P.; Leto, G.; Mastrolorenzo, E.; Para, O.; Giordano, M. Influence of Gender in Diabetes Mellitus and Its Complication. Int. J. Mol. Sci. 2022, 23, 8850. [Google Scholar] [CrossRef]
- Kautzky-Willer, A.; Harreiter, J.; Abrahamian, H.; Weitgasser, R.; Fasching, P.; Hoppichler, F.; Lechleitner, M. [Sex and gender-specific aspects in prediabetes and diabetes mellitus-clinical recommendations (Update 2019)]. Wien. Klin. Wochenschr. 2019, 131, 221–228. [Google Scholar] [CrossRef]
- Huebschmann, A.G.; Huxley, R.R.; Kohrt, W.M.; Zeitler, P.; Regensteiner, J.G.; Reusch, J.E.B. Sex Differences in the Burden of Type 2 Diabetes and Cardiovascular Risk across the Life Course. Diabetologia 2019, 62, 1761–1772. [Google Scholar] [CrossRef]
- Zhang, H.; Ni, J.; Yu, C.; Wu, Y.; Li, J.; Liu, J.; Tu, J.; Ning, X.; He, Q.; Wang, J. Sex-Based Differences in Diabetes Prevalence and Risk Factors: A Population-Based Cross-Sectional Study among Low-Income Adults in China. Front. Endocrinol. 2019, 10, 658. [Google Scholar] [CrossRef]
- Yeo, J.L.; Brady, E.M.; McCann, G.P.; Gulsin, G.S. Sex and Ethnic Differences in the Cardiovascular Complications of Type 2 Diabetes. Ther. Adv. Endocrinol. Metab. 2021, 12, 20420188211034296. [Google Scholar] [CrossRef]
- Einarson, T.R.; Acs, A.; Ludwig, C.; Panton, U.H. Prevalence of Cardiovascular Disease in Type 2 Diabetes: A Systematic Literature Review of Scientific Evidence from across the World in 2007–2017. Cardiovasc. Diabetol. 2018, 17, 83. [Google Scholar] [CrossRef]
- Einarson, T.R.; Acs, A.; Ludwig, C.; Panton, U.H. Economic Burden of Cardiovascular Disease in Type 2 Diabetes: A Systematic Review. Value Health J. Int. Soc. Pharm. Outcomes Res. 2018, 21, 881–890. [Google Scholar] [CrossRef]
- López-Díez, R.; Egaña-Gorroño, L.; Senatus, L.; Shekhtman, A.; Ramasamy, R.; Schmidt, A.M. Diabetes and Cardiovascular Complications: The Epidemics Continue. Curr. Cardiol. Rep. 2021, 23, 74. [Google Scholar] [CrossRef]
- Peters, S.A.E.; Huxley, R.R.; Woodward, M. Diabetes as Risk Factor for Incident Coronary Heart Disease in Women Compared with Men: A Systematic Review and Meta-Analysis of 64 Cohorts Including 858,507 Individuals and 28,203 Coronary Events. Diabetologia 2014, 57, 1542–1551. [Google Scholar] [CrossRef] [PubMed]
- Montarello, N.; Chan, W.P.A. Coronary Artery Disease in Women. Aust. Prescr. 2022, 45, 193–199. [Google Scholar] [CrossRef] [PubMed]
- Gnatiuc, L.; Herrington, W.; Halsey, J.; Tuomilehto, J.; Fang, X.; Kim, H.; De Bacquer, D.; Dobson, A.; Criqui, M.; Jacobs, D.; et al. Sex-Specific Relevance of Diabetes to Occlusive Vascular and Other Mortality: A Collaborative Meta-Analysis of Individual Data from 980,793 Adults from 68 Prospective Studies. Lancet Diabetes Endocrinol. 2018, 6, 538–546. [Google Scholar] [CrossRef] [PubMed]
- Taskinen, M.-R. Diabetic Dyslipidaemia: From Basic Research to Clinical Practice. Diabetologia 2003, 46, 733–749. [Google Scholar] [CrossRef]
- Miura, Y.; Suzuki, H. Hypertriglyceridemia and Atherosclerotic Carotid Artery Stenosis. Int. J. Mol. Sci. 2022, 23, 16224. [Google Scholar] [CrossRef]
- Josloff, K.; Beiriger, J.; Khan, A.; Gawel, R.J.; Kirby, R.S.; Kendrick, A.D.; Rao, A.K.; Wang, R.X.; Schafer, M.M.; Pearce, M.E.; et al. Comprehensive Review of Cardiovascular Disease Risk in Nonalcoholic Fatty Liver Disease. J. Cardiovasc. Dev. Dis. 2022, 9, 419. [Google Scholar] [CrossRef]
- Kaze, A.D.; Santhanam, P.; Musani, S.K.; Ahima, R.; Echouffo-Tcheugui, J.B. Metabolic Dyslipidemia and Cardiovascular Outcomes in Type 2 Diabetes Mellitus: Findings from the Look AHEAD Study. J. Am. Heart Assoc. Cardiovasc. Cerebrovasc. Dis. 2021, 10, e016947. [Google Scholar] [CrossRef]
- Ray, K.K.; Seshasai, S.R.K.; Wijesuriya, S.; Sivakumaran, R.; Nethercott, S.; Preiss, D.; Erqou, S.; Sattar, N. Effect of Intensive Control of Glucose on Cardiovascular Outcomes and Death in Patients with Diabetes Mellitus: A Meta-Analysis of Randomised Controlled Trials. Lancet 2009, 373, 1765–1772. [Google Scholar] [CrossRef]
- Control Group; Turnbull, F.M.; Abraira, C.; Anderson, R.J.; Byington, R.P.; Chalmers, J.P.; Duckworth, W.C.; Evans, G.W.; Gerstein, H.C.; Holman, R.R.; et al. Intensive Glucose Control and Macrovascular Outcomes in Type 2 Diabetes. Diabetologia 2009, 52, 2288–2298. [Google Scholar] [CrossRef] [PubMed]
- Lupsa, B.C.; Inzucchi, S.E. Diabetes Medications and Cardiovascular Disease: At Long Last Progress. Curr. Opin. Endocrinol. Diabetes Obes. 2018, 25, 87–93. [Google Scholar] [CrossRef]
- Kalyani, R.R.; Lazo, M.; Ouyang, P.; Turkbey, E.; Chevalier, K.; Brancati, F.; Becker, D.; Vaidya, D. Sex Differences in Diabetes and Risk of Incident Coronary Artery Disease in Healthy Young and Middle-Aged Adults. Diabetes Care 2014, 37, 830–838. [Google Scholar] [CrossRef]
- Khanal, M.K.; Bhandari, P.; Dhungana, R.R.; Gurung, Y.; Rawal, L.B.; Pandey, G.; Bhandari, M.; Devkota, S.; de Courten, M.; de Courten, B. Poor Glycemic Control, Cardiovascular Disease Risk Factors and Their Clustering among Patients with Type 2 Diabetes Mellitus: A Cross-Sectional Study from Nepal. PLoS ONE 2022, 17, e0271888. [Google Scholar] [CrossRef] [PubMed]
- Sattar, N.; Rawshani, A.; Franzén, S.; Rawshani, A.; Svensson, A.-M.; Rosengren, A.; McGuire, D.K.; Eliasson, B.; Gudbjörnsdottir, S. Age at Diagnosis of Type 2 Diabetes Mellitus and Associations with Cardiovascular and Mortality Risks. Circulation 2019, 139, 2228–2237. [Google Scholar] [CrossRef] [PubMed]
- Wright, A.K.; Kontopantelis, E.; Emsley, R.; Buchan, I.; Mamas, M.A.; Sattar, N.; Ashcroft, D.M.; Rutter, M.K. Cardiovascular Risk and Risk Factor Management in Type 2 Diabetes Mellitus. Circulation 2019, 139, 2742–2753. [Google Scholar] [CrossRef]
- del-Sueldo, M.A.; Mendonça-Rivera, M.A.; Sánchez-Zambrano, M.B.; Zilberman, J.; Múnera-Echeverri, A.G.; Paniagua, M.; Campos-Alcántara, L.; Almonte, C.; Paix-Gonzales, A.; Anchique-Santos, C.V.; et al. Guía de práctica clínica de la Sociedad Interamericana de Cardiología sobre prevención primaria de enfermedad cardiovascular en la mujer. Arch. Cardiol. México 2022, 92, 8672. [Google Scholar] [CrossRef]
- Hu, G.; Liu, H.; Leng, J.; Wang, L.; Li, W.; Zhang, S.; Li, W.; Liu, G.; Tian, H.; Yang, S.; et al. Effects of a Lifestyle Intervention in Young Women with GDM and Subsequent Diabetes. Nutrients 2022, 14, 5232. [Google Scholar] [CrossRef]
- Millett, E.R.C.; Peters, S.A.E.; Woodward, M. Sex Differences in Risk Factors for Myocardial Infarction: Cohort Study of UK Biobank Participants. BMJ 2018, 363, k4247. [Google Scholar] [CrossRef]
- Engelen, S.E.; van der Graaf, Y.; Stam-Slob, M.C.; Grobbee, D.E.; Cramer, M.J.; Kappelle, L.J.; de Borst, G.J.; Visseren, F.L.J.; Westerink, J.; SMART Study Group. Incidence of Cardiovascular Events and Vascular Interventions in Patients with Type 2 Diabetes. Int. J. Cardiol. 2017, 248, 301–307. [Google Scholar] [CrossRef]
- Wang, Y.; O’Neil, A.; Jiao, Y.; Wang, L.; Huang, J.; Lan, Y.; Zhu, Y.; Yu, C. Sex Differences in the Association between Diabetes and Risk of Cardiovascular Disease, Cancer, and All-Cause and Cause-Specific Mortality: A Systematic Review and Meta-Analysis of 5,162,654 Participants. BMC Med. 2019, 17, 136. [Google Scholar] [CrossRef]
- Lopez-de-Andres, A.; Jimenez-Garcia, R.; Hernández-Barrera, V.; de Miguel-Yanes, J.M.; Albaladejo-Vicente, R.; Villanueva-Orbaiz, R.; Carabantes-Alarcon, D.; Zamorano-Leon, J.J.; Lopez-Herranz, M.; de Miguel-Diez, J. Are There Sex Differences in the Effect of Type 2 Diabetes in the Incidence and Outcomes of Myocardial Infarction? A Matched-Pair Analysis Using Hospital Discharge Data. Cardiovasc. Diabetol. 2021, 20, 81. [Google Scholar] [CrossRef] [PubMed]
- Wargny, M.; Croyal, M.; Ragot, S.; Gand, E.; Jacobi, D.; Trochu, J.-N.; Prieur, X.; Le May, C.; Goronflot, T.; Cariou, B.; et al. Nutritional Biomarkers and Heart Failure Requiring Hospitalization in Patients with Type 2 Diabetes: The SURDIAGENE Cohort. Cardiovasc. Diabetol. 2022, 21, 101. [Google Scholar] [CrossRef]
- Liang, B.; Li, R.; Zhang, P.; Gu, N. Empagliflozin for Patients with Heart Failure and Type 2 Diabetes Mellitus: Clinical Evidence in Comparison with Other Sodium-Glucose Co-Transporter-2 Inhibitors and Potential Mechanism. J Cardiovasc. Transl. Res. 2022, 16, 327–340. [Google Scholar] [CrossRef] [PubMed]
- Ohkuma, T.; Komorita, Y.; Peters, S.A.E.; Woodward, M. Diabetes as a Risk Factor for Heart Failure in Women and Men: A Systematic Review and Meta-Analysis of 47 Cohorts Including 12 Million Individuals. Diabetologia 2019, 62, 1550–1560. [Google Scholar] [CrossRef] [PubMed]
- Chase-Vilchez, A.Z.; Chan, I.H.Y.; Peters, S.A.E.; Woodward, M. Diabetes as a Risk Factor for Incident Peripheral Arterial Disease in Women Compared to Men: A Systematic Review and Meta-Analysis. Cardiovasc. Diabetol. 2020, 19, 151. [Google Scholar] [CrossRef]
- Pabon, M.; Cheng, S.; Altin, S.E.; Sethi, S.S.; Nelson, M.D.; Moreau, K.L.; Hamburg, N.; Hess, C.N. Sex Differences in Peripheral Artery Disease. Circ. Res. 2022, 130, 496–511. [Google Scholar] [CrossRef] [PubMed]
- Shatnawi, N.J.; Al-Zoubi, N.A.; Hawamdeh, H.M.; Khader, Y.S.; Heis, M.; Al Omari, M.; Bataineh, B. The Relation of Anatomical Distribution of Symptomatic Peripheral Arterial Disease (PAD) with HbA1c Level in Patients with Type 2 Diabetes Mellitus. Ther. Adv. Endocrinol. Metab. 2021, 12, 20420188211000504. [Google Scholar] [CrossRef]
- Althouse, A.D.; Abbott, J.D.; Forker, A.D.; Bertolet, M.; Barinas-Mitchell, E.; Thurston, R.C.; Mulukutla, S.; Aboyans, V.; Brooks, M.M.; BARI 2D Study Group. Risk Factors for Incident Peripheral Arterial Disease in Type 2 Diabetes: Results from the Bypass Angioplasty Revascularization Investigation in Type 2 Diabetes (BARI 2D) Trial. Diabetes Care 2014, 37, 1346–1352. [Google Scholar] [CrossRef]
- Selvin, E.; Erlinger, T.P. Prevalence of and Risk Factors for Peripheral Arterial Disease in the United States: Results from the National Health and Nutrition Examination Survey, 1999–2000. Circulation 2004, 110, 738–743. [Google Scholar] [CrossRef]
- Thiruvoipati, T.; Kielhorn, C.E.; Armstrong, E.J. Peripheral Artery Disease in Patients with Diabetes: Epidemiology, Mechanisms, and Outcomes. World J. Diabetes 2015, 6, 961–969. [Google Scholar] [CrossRef]
- Jalkanen, J.M.; Wickström, J.-E.; Venermo, M.; Hakovirta, H.H. The Extent of Atherosclerotic Lesions in Crural Arteries Predicts Survival of Patients with Lower Limb Peripheral Artery Disease: A New Classification of Crural Atherosclerosis. Atherosclerosis 2016, 251, 328–333. [Google Scholar] [CrossRef]
- Jude, E.B.; Oyibo, S.O.; Chalmers, N.; Boulton, A.J.M. Peripheral Arterial Disease in Diabetic and Nondiabetic Patients. Diabetes Care 2001, 24, 1433–1437. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Z.-Y.; Liu, Y.-K.; Chen, H.-L.; Yang, H.-L.; Liu, F. HbA1c and Lower Extremity Amputation Risk in Patients with Diabetes: A Meta-Analysis. Int. J. Low. Extrem. Wounds 2015, 14, 168–177. [Google Scholar] [CrossRef]
- Arya, S.; Binney, Z.O.; Khakharia, A.; Long, C.A.; Brewster, L.P.; Wilson, P.W.; Jordan, W.D.; Duwayri, Y. High Hemoglobin A1c Associated with Increased Adverse Limb Events in Peripheral Arterial Disease Patients Undergoing Revascularization. J. Vasc. Surg. 2018, 67, 217–228.e1. [Google Scholar] [CrossRef]
- McGill, H.C.; McMahan, C.A.; Malcom, G.T.; Oalmann, M.C.; Strong, J.P. Effects of Serum Lipoproteins and Smoking on Atherosclerosis in Young Men and Women. The PDAY Research Group. Pathobiological Determinants of Atherosclerosis in Youth. Arterioscler. Thromb. Vasc. Biol. 1997, 17, 95–106. [Google Scholar] [CrossRef]
- Diehm, N.; Shang, A.; Silvestro, A.; Do, D.-D.; Dick, F.; Schmidli, J.; Mahler, F.; Baumgartner, I. Association of Cardiovascular Risk Factors with Pattern of Lower Limb Atherosclerosis in 2659 Patients Undergoing Angioplasty. Eur. J. Vasc. Endovasc. Surg. 2006, 31, 59–63. [Google Scholar] [CrossRef] [PubMed]
- Lowry, D.; Saeed, M.; Narendran, P.; Tiwari, A. A Review of Distribution of Atherosclerosis in the Lower Limb Arteries of Patients with Diabetes Mellitus and Peripheral Vascular Disease. Vasc. Endovasc. Surg. 2018, 52, 535–542. [Google Scholar] [CrossRef]
- Ozkan, U.; Oguzkurt, L.; Tercan, F. Atherosclerotic Risk Factors and Segmental Distribution in Symptomatic Peripheral Artery Disease. J. Vasc. Interv. Radiol. JVIR 2009, 20, 437–441. [Google Scholar] [CrossRef] [PubMed]
- Wickström, J.-E.; Jalkanen, J.M.; Venermo, M.; Hakovirta, H.H. Crural Index and Extensive Atherosclerosis of Crural Vessels Are Associated with Long-Term Cardiovascular Mortality in Patients with Symptomatic Peripheral Artery Disease. Atherosclerosis 2017, 264, 44–50. [Google Scholar] [CrossRef]
- Cannavale, A.; Santoni, M.; Gazzetti, M.; Catalano, C.; Fanelli, F. Updated Clinical and Radiological Classification of Lower Limb Atherosclerotic Disease. Ann. Vasc. Surg. 2019, 55, 272–284. [Google Scholar] [CrossRef]
- Koivunen, V.; Juonala, M.; Mikkola, K.; Hakovirta, H. Chronic Limb Threatening Ischemia and Diabetes Mellitus: The Severity of Tibial Atherosclerosis and Outcome after Infrapopliteal Revascularization. Scand. J. Surg. SJS Off. Organ Finn. Surg. Soc. Scand. Surg. Soc. 2021, 110, 472–482. [Google Scholar] [CrossRef] [PubMed]
- Karayiannides, S.; Djupsjö, C.; Kuhl, J.; Hofman-Bang, C.; Norhammar, A.; Holzmann, M.J.; Lundman, P. Long-Term Prognosis in Patients with Acute Myocardial Infarction and Newly Detected Glucose Abnormalities: Predictive Value of Oral Glucose Tolerance Test and HbA1c. Cardiovasc. Diabetol. 2021, 20, 122. [Google Scholar] [CrossRef]
- Currie, C.J.; Peters, J.R.; Tynan, A.; Evans, M.; Heine, R.J.; Bracco, O.L.; Zagar, T.; Poole, C.D. Survival as a Function of HbA(1c) in People with Type 2 Diabetes: A Retrospective Cohort Study. Lancet 2010, 375, 481–489. [Google Scholar] [CrossRef]
- Yu, D.; Simmons, D. Relationship between HbA1c and Risk of All-Cause Hospital Admissions among People with Type 2 Diabetes. Diabet. Med. J. Br. Diabet. Assoc. 2013, 30, 1407–1411. [Google Scholar] [CrossRef]
- Nozawa, K.; Ikeda, M.; Kikuchi, S. Association Between HbA1c Levels and Diabetic Peripheral Neuropathy: A Case-Control Study of Patients with Type 2 Diabetes Using Claims Data. Drugs-Real World Outcomes 2022, 9, 403–414. [Google Scholar] [CrossRef]
- Arnold, L.W.; Wang, Z. The HbA1c and All-Cause Mortality Relationship in Patients with Type 2 Diabetes Is J-Shaped: A Meta-Analysis of Observational Studies. Rev. Diabet. Stud. RDS 2014, 11, 138–152. [Google Scholar] [CrossRef] [PubMed]
- Zoungas, S.; Chalmers, J.; Ninomiya, T.; Li, Q.; Cooper, M.E.; Colagiuri, S.; Fulcher, G.; de Galan, B.E.; Harrap, S.; Hamet, P.; et al. Association of HbA1c Levels with Vascular Complications and Death in Patients with Type 2 Diabetes: Evidence of Glycaemic Thresholds. Diabetologia 2012, 55, 636–643. [Google Scholar] [CrossRef]
- van Hateren, K.J.J.; Landman, G.W.D.; Kleefstra, N.; Drion, I.; Groenier, K.H.; Houweling, S.T.; Bilo, H.J.G. Glycaemic Control and the Risk of Mortality in Elderly Type 2 Diabetic Patients (ZODIAC-20). Int. J. Clin. Pract. 2011, 65, 415–419. [Google Scholar] [CrossRef]
- Djupsjö, C.; Kuhl, J.; Andersson, T.; Lundbäck, M.; Holzmann, M.J.; Nyström, T. Admission Glucose as a Prognostic Marker for All-Cause Mortality and Cardiovascular Disease. Cardiovasc. Diabetol. 2022, 21, 258. [Google Scholar] [CrossRef] [PubMed]
- Amin, N.; Doupis, J. Diabetic Foot Disease: From the Evaluation of the “Foot at Risk” to the Novel Diabetic Ulcer Treatment Modalities. World J. Diabetes 2016, 7, 153–164. [Google Scholar] [CrossRef] [PubMed]
- Rossboth, S.; Lechleitner, M.; Oberaigner, W. Risk Factors for Diabetic Foot Complications in Type 2 Diabetes—A Systematic Review. Endocrinol. Diabetes Metab. 2021, 4, e00175. [Google Scholar] [CrossRef] [PubMed]
- Jeffcoate, W.J.; Macfarlane, R.M.; Fletcher, E.M. The Description and Classification of Diabetic Foot Lesions. Diabet. Med. J. Br. Diabet. Assoc. 1993, 10, 676–679. [Google Scholar] [CrossRef] [PubMed]
- Dietrich, I.; Braga, G.A.; de Melo, F.G.; da Costa Silva Silva, A.C.C. The Diabetic Foot as a Proxy for Cardiovascular Events and Mortality Review. Curr. Atheroscler. Rep. 2017, 19, 44. [Google Scholar] [CrossRef]
- Noor, S.; Khan, R.U.; Ahmad, J. Understanding Diabetic Foot Infection and Its Management. Diabetes Metab. Syndr. 2017, 11, 149–156. [Google Scholar] [CrossRef]
- Wang, Z.; Hazlehurst, J.; Subramanian, A.; Tahrani, A.A.; Hanif, W.; Thomas, N.; Singh, P.; Wang, J.; Sainsbury, C.; Nirantharakumar, K.; et al. Diabetic Foot Risk Classification at the Time of Type 2 Diabetes Diagnosis and Subsequent Risk of Mortality: A Population-Based Cohort Study. Front. Endocrinol. 2022, 13, 888924. [Google Scholar] [CrossRef]
- American Diabetes Association. Consensus Development Conference on Diabetic Foot Wound Care: 7–8 April 1999, Boston, Massachusetts. American Diabetes Association. Diabetes Care 1999, 22, 1354–1360. [Google Scholar] [CrossRef]
- Khanolkar, M.P.; Bain, S.C.; Stephens, J.W. The Diabetic Foot. QJM Mon. J. Assoc. Physicians 2008, 101, 685–695. [Google Scholar] [CrossRef]
- Wang, J.; Xue, T.; Li, H.; Guo, S. Nomogram Prediction for the Risk of Diabetic Foot in Patients with Type 2 Diabetes Mellitus. Front. Endocrinol. 2022, 13, 890057. [Google Scholar] [CrossRef]
- Polikandrioti, M.; Vasilopoulos, G.; Koutelekos, I.; Panoutsopoulos, G.; Gerogianni, G.; Babatsikou, F.; Zartaloudi, A.; Toulia, G. Quality of Life in Diabetic Foot Ulcer: Associated Factors and the Impact of Anxiety/Depression and Adherence to Self-Care. Int. J. Low. Extrem. Wounds 2020, 19, 165–179. [Google Scholar] [CrossRef]
- Volmer-Thole, M.; Lobmann, R. Neuropathy and Diabetic Foot Syndrome. Int. J. Mol. Sci. 2016, 17, 917. [Google Scholar] [CrossRef]
- Jiang, Y.; Wang, X.; Xia, L.; Fu, X.; Xu, Z.; Ran, X.; Yan, L.; Li, Q.; Mo, Z.; Yan, Z.; et al. A Cohort Study of Diabetic Patients and Diabetic Foot Ulceration Patients in China. Wound Repair Regen. Off. Publ. Wound Health Soc. Eur. Tissue Repair Soc. 2015, 23, 222–230. [Google Scholar] [CrossRef] [PubMed]
- Lai, Y.-J.; Hu, H.-Y.; Lin, C.-H.; Lee, S.-T.; Kuo, S.-C.; Chou, P. Incidence and Risk Factors of Lower Extremity Amputations in People with Type 2 Diabetes in Taiwan, 2001–2010. J. Diabetes 2015, 7, 260–267. [Google Scholar] [CrossRef] [PubMed]
- Robinson, T.E.; Kenealy, T.; Garrett, M.; Bramley, D.; Drury, P.L.; Elley, C.R. Ethnicity and Risk of Lower Limb Amputation in People with Type 2 Diabetes: A Prospective Cohort Study. Diabet. Med. J. Br. Diabet. Assoc. 2016, 33, 55–61. [Google Scholar] [CrossRef] [PubMed]
- Sarfo-Kantanka, O.; Sarfo, F.S.; Kyei, I.; Agyemang, C.; Mbanya, J.C. Incidence and Determinants of Diabetes-Related Lower Limb Amputations in Ghana, 2010–2015—A Retrospective Cohort Study. BMC Endocr. Disord. 2019, 19, 27. [Google Scholar] [CrossRef]
- Lin, J.; Song, H.; Liang, M.; Cai, Z.; Chen, T.; Lin, Z.; Zhang, J. Advances in the Study of OSA and Diabetic Foot. Diabetol. Metab. Syndr. 2022, 14, 70. [Google Scholar] [CrossRef]
- Reis, J.M.C.D.; Wanzeller, R.R.M.; Meireles, W.M.; Andrade, M.C.D.; Gomes, V.H.G.A.; Arrais, J.A.A.; Ishak, G. Demographic and Socioeconomic Profiles of Patients Admitted with Diabetic Foot Complications in a Tertiary Hospital in Belem—Para. Rev. Colégio Bras. Cir. 2020, 47, e20202606. [Google Scholar] [CrossRef]
- Rahman, M.H.; Kamrul-Hasan, A.B.; Islam, M.R.; Hasan, A.Y.; Chowdhury, F.Q.; Miah, O.F.; Islam, M.F.; Wadud, S.A.; Akhanda, A.H. Frequency and Risk Factors of Diabetic Retinopathy among Patients with Type 2 Diabetes Mellitus: A Single-Center Study from Bangladesh. Mymensingh Med. J. MMJ 2020, 29, 807–814. [Google Scholar]
- Dekker, R.G.; Qin, C.; Ho, B.S.; Kadakia, A.R. The Effect of Cumulative Glycemic Burden on the Incidence of Diabetic Foot Disease. J. Orthop. Surg. 2016, 11, 143. [Google Scholar] [CrossRef]
- Kress, S.; Anderten, H.; Borck, A.; Freckmann, G.; Heinemann, L.; Holzmüller, U.; Kulzer, B.; Portele, A.; Schnell, O.; Varlemann, H.; et al. Preulcerous Risk Situation in Diabetic Foot Syndrome: Proposal for a Simple Ulcer Prevention Score. J. Diabetes Sci. Technol. 2021, 15, 816–826. [Google Scholar] [CrossRef]
- Shahbazian, H.; Yazdanpanah, L.; Latifi, S.M. Risk Assessment of Patients with Diabetes for Foot Ulcers according to Risk Classification Consensus of International Working Group on Diabetic Foot (IWGDF). Pak. J. Med. Sci. 2013, 29, 730–734. [Google Scholar] [CrossRef] [PubMed]
- Papanas, N.; Steiropoulos, P. Obstructive Sleep Apnea and Diabetic Foot: New Responsibilities? Angiology 2016, 67, 605–606. [Google Scholar] [CrossRef]
- Kannel, W.B.; McGee, D.L. Diabetes and Cardiovascular Disease. The Framingham Study. JAMA 1979, 241, 2035–2038. [Google Scholar] [CrossRef]
- Roper, N.A.; Bilous, R.W.; Kelly, W.F.; Unwin, N.C.; Connolly, V.M. Excess Mortality in a Population with Diabetes and the Impact of Material Deprivation: Longitudinal, Population Based Study. BMJ 2001, 322, 1389–1393. [Google Scholar] [CrossRef] [PubMed]
- Tuttolomondo, A.; Maida, C.; Pinto, A. Diabetic Foot Syndrome as a Possible Cardiovascular Marker in Diabetic Patients. J. Diabetes Res. 2015, 2015, 268390. [Google Scholar] [CrossRef]
- Walters, D.P.; Gatling, W.; Mullee, M.A.; Hill, R.D. The Distribution and Severity of Diabetic Foot Disease: A Community Study with Comparison to a Non-Diabetic Group. Diabet. Med. J. Br. Diabet. Assoc. 1992, 9, 354–358. [Google Scholar] [CrossRef]
- Tahrani, A.A.; Ali, A.; Raymond, N.T.; Begum, S.; Dubb, K.; Mughal, S.; Jose, B.; Piya, M.K.; Barnett, A.H.; Stevens, M.J. Obstructive Sleep Apnea and Diabetic Neuropathy: A Novel Association in Patients with Type 2 Diabetes. Am. J. Respir. Crit. Care Med. 2012, 186, 434–441. [Google Scholar] [CrossRef] [PubMed]
- Shen, H.; Zhao, J.; Liu, Y.; Sun, G. Interactions between and Shared Molecular Mechanisms of Diabetic Peripheral Neuropathy and Obstructive Sleep Apnea in Type 2 Diabetes Patients. J. Diabetes Res. 2018, 2018, 3458615. [Google Scholar] [CrossRef]
- Altaf, Q.-A.A.; Ali, A.; Piya, M.K.; Raymond, N.T.; Tahrani, A.A. The Relationship between Obstructive Sleep Apnea and Intra-Epidermal Nerve Fiber Density, PARP Activation and Foot Ulceration in Patients with Type 2 Diabetes. J. Diabetes Its Complicat. 2016, 30, 1315–1320. [Google Scholar] [CrossRef]
- Xue, P.; Covassin, N.; Ran, X.; Zhou, J.; Zhang, X.; Yan, D.; Li, X.; Gao, Y.; Tang, X. Association of Parameters of Nocturnal Hypoxemia with Diabetic Microvascular Complications: A Cross-Sectional Study. Diabetes Res. Clin. Pract. 2020, 170, 108484. [Google Scholar] [CrossRef]
- Paschou, S.A.; Bletsa, E.; Saltiki, K.; Kazakou, P.; Kantreva, K.; Katsaounou, P.; Rovina, N.; Trakada, G.; Bakakos, P.; Vlachopoulos, C.V.; et al. Sleep Apnea and Cardiovascular Risk in Patients with Prediabetes and Type 2 Diabetes. Nutrients 2022, 14, 4989. [Google Scholar] [CrossRef] [PubMed]
- Begun, A.; Morbach, S.; Rümenapf, G.; Icks, A. Study of Disease Progression and Relevant Risk Factors in Diabetic Foot Patients Using a Multistate Continuous-Time Markov Chain Model. PLoS ONE 2016, 11, e0147533. [Google Scholar] [CrossRef] [PubMed]
- Pinto, A.; Tuttolomondo, A.; Di Raimondo, D.; Fernandez, P.; La Placa, S.; Di Gati, M.; Licata, G. Cardiovascular Risk Profile and Morbidity in Subjects Affected by Type 2 Diabetes Mellitus with and without Diabetic Foot. Metabolism 2008, 57, 676–682. [Google Scholar] [CrossRef]
- Pinto, A.; Tuttolomondo, A.; Di Raimondo, D.; La Placa, S.; Di Sciacca, R.; Fernandez, P.; Di Gati, M.; Raffa, A.; Licata, G. Ischemic Stroke in Patients with Diabetic Foot. Int. Angiol. J. Int. Union Angiol. 2007, 26, 266–269. [Google Scholar]
- Ranachowska, C.; Lass, P.; Korzon-Burakowska, A.; Dobosz, M. Diagnostic Imaging of the Diabetic Foot. Nucl. Med. Rev. 2010, 13, 18–22. [Google Scholar]
- Low, K.T.; Peh, W.C. Magnetic Resonance Imaging of Diabetic Foot Complications. Singap. Med. J. 2015, 56, 23–34. [Google Scholar] [CrossRef]
- Ledermann, H.P.; Morrison, W.B. Differential Diagnosis of Pedal Osteomyelitis and Diabetic Neuroarthropathy: MR Imaging. Semin. Musculoskelet. Radiol. 2005, 9, 272–283. [Google Scholar] [CrossRef] [PubMed]
- Daneshvar, K.; Anwander, H. Diagnostic Imaging of Diabetic Foot Disorders. Foot Ankle Clin. 2022, 27, 513–527. [Google Scholar] [CrossRef]
- Kapoor, A.; Page, S.; Lavalley, M.; Gale, D.R.; Felson, D.T. Magnetic Resonance Imaging for Diagnosing Foot Osteomyelitis: A Meta-Analysis. Arch. Intern. Med. 2007, 167, 125–132. [Google Scholar] [CrossRef] [PubMed]
- Lipsky, B.A.; Berendt, A.R.; Deery, H.G.; Embil, J.M.; Joseph, W.S.; Karchmer, A.W.; LeFrock, J.L.; Lew, D.P.; Mader, J.T.; Norden, C.; et al. Diagnosis and Treatment of Diabetic Foot Infections. Clin. Infect. Dis. 2004, 39, 885–910. [Google Scholar] [CrossRef]
- El-Maghraby, T.A.F.; Moustafa, H.M.; Pauwels, E.K.J. Nuclear Medicine Methods for Evaluation of Skeletal Infection among Other Diagnostic Modalities. Q. J. Nucl. Med. Mol. Imaging 2006, 50, 167–192. [Google Scholar]
- Smith, C.D.; Bilmen, J.G.; Iqbal, S.; Robey, S.; Pereira, M. Medial Artery Calcification as an Indicator of Diabetic Peripheral Vascular Disease. Foot Ankle Int. 2008, 29, 185–190. [Google Scholar] [CrossRef]
- Herbst, S.A.; Jones, K.B.; Saltzman, C.L. Pattern of Diabetic Neuropathic Arthropathy Associated with the Peripheral Bone Mineral Density. J. Bone Joint Surg. 2004, 86, 378–383. [Google Scholar] [CrossRef]
- Gielen, J.; Vael, L. Imaging of the Diabetic Foot. J. Belg. Soc. Radiol. 2021, 105, 73. [Google Scholar] [CrossRef]
- Morrison, W.B.; Schweitzer, M.E.; Bock, G.W.; Mitchell, D.G.; Hume, E.L.; Pathria, M.N.; Resnick, D. Diagnosis of Osteomyelitis: Utility of Fat-Suppressed Contrast-Enhanced MR Imaging. Radiology 1993, 189, 251–257. [Google Scholar] [CrossRef]
- Palestro, C.J.; Love, C. Nuclear Medicine and Diabetic Foot Infections. Semin. Nucl. Med. 2009, 39, 52–65. [Google Scholar] [CrossRef] [PubMed]
- Pieruzzi, L.; Napoli, V.; Goretti, C.; Adami, D.; Iacopi, E.; Cicorelli, A.; Piaggesi, A. Ultrasound in the Modern Management of the Diabetic Foot Syndrome: A Multipurpose Versatile Toolkit. Int. J. Low. Extrem. Wounds 2020, 19, 315–333. [Google Scholar] [CrossRef] [PubMed]
- Plekhanov, A.N.; Markevich, P.S. Syndrome of diabetic foot: Modern diagnostic methods. Klin. Med. 2014, 92, 29–33. [Google Scholar]
- Rastogi, A.; Bhansali, A.; Ramachandran, S. Efficacy and Safety of Low-Frequency, Noncontact Airborne Ultrasound Therapy (Glybetac) For Neuropathic Diabetic Foot Ulcers: A Randomized, Double-Blind, Sham-Control Study. Int. J. Low. Extrem. Wounds 2019, 18, 81–88. [Google Scholar] [CrossRef] [PubMed]
- Ennis, W.J.; Foremann, P.; Mozen, N.; Massey, J.; Conner-Kerr, T.; Meneses, P. Ultrasound Therapy for Recalcitrant Diabetic Foot Ulcers: Results of a Randomized, Double-Blind, Controlled, Multicenter Study. Ostomy. Wound Manag. 2005, 51, 24–39. [Google Scholar]
- Yao, M.; Hasturk, H.; Kantarci, A.; Gu, G.; Garcia-Lavin, S.; Fabbi, M.; Park, N.; Hayashi, H.; Attala, K.; French, M.A.; et al. A Pilot Study Evaluating Non-Contact Low-Frequency Ultrasound and Underlying Molecular Mechanism on Diabetic Foot Ulcers. Int. Wound J. 2014, 11, 586–593. [Google Scholar] [CrossRef]
- Lim, J.Z.M.; Ng, N.S.L.; Thomas, C. Prevention and Treatment of Diabetic Foot Ulcers. J. R. Soc. Med. 2017, 110, 104–109. [Google Scholar] [CrossRef]
- Colen, L.B.; Kim, C.J.; Grant, W.P.; Yeh, J.-T.; Hind, B. Achilles Tendon Lengthening: Friend or Foe in the Diabetic Foot? Plast. Reconstr. Surg. 2013, 131, 37e–43e. [Google Scholar] [CrossRef]
- Dallimore, S.M.; Kaminski, M.R. Tendon Lengthening and Fascia Release for Healing and Preventing Diabetic Foot Ulcers: A Systematic Review and Meta-Analysis. J. Foot Ankle Res. 2015, 8, 33. [Google Scholar] [CrossRef]
- Foote, G.A.; Belis, A.M. Radiographic Correction of Achilles Tendon Lengthening in Diabetic Patients with High Risk for Foot Ulceration. Foot Ankle Surg. Tech. Rep. Cases 2022, 2, 100146. [Google Scholar] [CrossRef]
- Schirmer, S.; Ritter, R.-G.; Fansa, H. Vascular Surgery, Microsurgery and Supramicrosurgery for Treatment of Chronic Diabetic Foot Ulcers to Prevent Amputations. PLoS ONE 2013, 8, e74704. [Google Scholar] [CrossRef]
- Zil-E-Ali, A.; Shafi, S.; Ali, M.H. Think Before Chopping a Diabetic Foot: Insight to Vascular Intervention. Cureus 2017, 9, e1194. [Google Scholar] [CrossRef]
- Hutting, K.H.; aan de Stegge, W.B.; van Netten, J.J.; ten Cate, W.A.; Smeets, L.; Welten, G.M.J.M.; Scharn, D.M.; de Vries, J.-P.P.M.; van Baal, J.G. Surgical Treatment of Diabetic Foot Ulcers Complicated by Osteomyelitis with Gentamicin-Loaded Calcium Sulphate-Hydroxyapatite Biocomposite. J. Clin. Med. 2021, 10, 371. [Google Scholar] [CrossRef]
- Rani, V.; Deep, G.; Singh, R.K.; Palle, K.; Yadav, U.C.S. Oxidative Stress and Metabolic Disorders: Pathogenesis and Therapeutic Strategies. Life Sci. 2016, 148, 183–193. [Google Scholar] [CrossRef] [PubMed]
- Pop-Busui, R.; Ang, L.; Holmes, C.; Gallagher, K.; Feldman, E.L. Inflammation as a Therapeutic Target for Diabetic Neuropathies. Curr. Diabetes Rep. 2016, 16, 29. [Google Scholar] [CrossRef] [PubMed]
- Gómez-Marcos, M.Á.; Recio-Rodríguez, J.I.; Patino-Alonso, M.C.; Agudo-Conde, C.; Rodríguez-Sanchez, E.; Maderuelo-Fernandez, J.A.; Gómez-Sánchez, L.; Gomez-Sanchez, M.; García-Ortiz, L.; LOD-DIABETES Group. Evolution of Target Organ Damage and Haemodynamic Parameters over 4 Years in Patients with Increased Insulin Resistance: The LOD-DIABETES Prospective Observational Study. BMJ Open 2016, 6, e010400. [Google Scholar] [CrossRef]
- De Favari Signini, É.; Castro, A.; Rehder-Santos, P.; Cristina Millan-Mattos, J.; Magalhães de Oliveira, J.; Minatel, V.; Bianca Falasco Pantoni, C.; Sobreiro Selistre de Araújo, H.; Fabrizzi, F.; Porta, A.; et al. Integrative Perspective of the Healthy Aging Process Considering the Metabolome, Cardiac Autonomic Modulation and Cardiorespiratory Fitness Evaluated in Age Groups. Sci. Rep. 2022, 12, 21314. [Google Scholar] [CrossRef]
- Lanting, S.M.; Twigg, S.M.; Johnson, N.A.; Baker, M.K.; Caterson, I.D.; Chuter, V.H. Non-Invasive Lower Limb Small Arterial Measures Co-Segregate Strongly with Foot Complications in People with Diabetes. J. Diabetes Its Complicat. 2017, 31, 589–593. [Google Scholar] [CrossRef] [PubMed]
- Tun, H.N. Cardio-Diabetology: New Subspecialty and Collaborative Work to Defeat the Burden of Deadly Duo. J. Cardiovasc. Med. Cardiol. 2018, 5, 081–084. [Google Scholar]
- Deedwania, P.; Kosiborod, M.; Barrett, E.; Ceriello, A.; Isley, W.; Mazzone, T.; Raskin, P. Hyperglycemia and Acute Coronary Syndrome: A Scientific Statement from the American Heart Association Diabetes Committee of the Council on Nutrition, Physical Activity, and Metabolism. Circulation 2008, 117, 1610–1619. [Google Scholar] [CrossRef] [PubMed]
- Miric, D.J.; Kisic, B.M.; Filipovic-Danic, S.; Grbic, R.; Dragojevic, I.; Miric, M.B.; Puhalo-Sladoje, D. Xanthine Oxidase Activity in Type 2 Diabetes Mellitus Patients with and without Diabetic Peripheral Neuropathy. J. Diabetes Res. 2016, 2016, 4370490. [Google Scholar] [CrossRef]
- Razzaghi, R.; Pourbagheri, H.; Momen-Heravi, M.; Bahmani, F.; Shadi, J.; Soleimani, Z.; Asemi, Z. The Effects of Vitamin D Supplementation on Wound Healing and Metabolic Status in Patients with Diabetic Foot Ulcer: A Randomized, Double-Blind, Placebo-Controlled Trial. J. Diabetes Its Complicat. 2017, 31, 766–772. [Google Scholar] [CrossRef]
- Baltzis, D.; Roustit, M.; Grammatikopoulou, M.G.; Katsaboukas, D.; Athanasiou, V.; Iakovou, I.; Veves, A.; Manes, C.; Trakatelli, M.-C. Diabetic Peripheral Neuropathy as a Predictor of Asymptomatic Myocardial Ischemia in Type 2 Diabetes Mellitus: A Cross-Sectional Study. Adv. Ther. 2016, 33, 1840–1847. [Google Scholar] [CrossRef]
- Callaghan, B.C.; Xia, R.; Banerjee, M.; de Rekeneire, N.; Harris, T.B.; Newman, A.B.; Satterfield, S.; Schwartz, A.V.; Vinik, A.I.; Feldman, E.L.; et al. Metabolic Syndrome Components Are Associated with Symptomatic Polyneuropathy Independent of Glycemic Status. Diabetes Care 2016, 39, 801–807. [Google Scholar] [CrossRef]
- Smith, S.; Normahani, P.; Lane, T.; Hohenschurz-Schmidt, D.; Oliver, N.; Davies, A.H. Prevention and Management Strategies for Diabetic Neuropathy. Life 2022, 12, 1185. [Google Scholar] [CrossRef]
- Afshinnia, F.; Reynolds, E.L.; Rajendiran, T.M.; Soni, T.; Byun, J.; Savelieff, M.G.; Looker, H.C.; Nelson, R.G.; Michailidis, G.; Callaghan, B.C.; et al. Serum Lipidomic Determinants of Human Diabetic Neuropathy in Type 2 Diabetes. Ann. Clin. Transl. Neurol. 2022, 9, 1392–1404. [Google Scholar] [CrossRef] [PubMed]
- Ziegler, D.; Strom, A.; Straßburger, K.; Knebel, B.; Bönhof, G.J.; Kotzka, J.; Szendroedi, J.; Roden, M.; German Diabetes Study Group. Association of Cardiac Autonomic Dysfunction with Higher Levels of Plasma Lipid Metabolites in Recent-Onset Type 2 Diabetes. Diabetologia 2021, 64, 458–468. [Google Scholar] [CrossRef] [PubMed]
- Semba, R.D.; Gonzalez-Freire, M.; Moaddel, R.; Sun, K.; Fabbri, E.; Zhang, P.; Carlson, O.D.; Khadeer, M.; Chia, C.W.; Salem, N.; et al. Altered Plasma Amino Acids and Lipids Associated with Abnormal Glucose Metabolism and Insulin Resistance in Older Adults. J. Clin. Endocrinol. Metab. 2018, 103, 3331–3339. [Google Scholar] [CrossRef] [PubMed]
- Zhao, J.; Deng, W.; Zhang, Y.; Zheng, Y.; Zhou, L.; Boey, J.; Armstrong, D.G.; Yang, G.; Liang, Z.; Chen, B. Association between Serum Cystatin C and Diabetic Foot Ulceration in Patients with Type 2 Diabetes: A Cross-Sectional Study. J. Diabetes Res. 2016, 2016, e8029340. [Google Scholar] [CrossRef] [PubMed]
- Herder, C.; Schamarek, I.; Nowotny, B.; Carstensen-Kirberg, M.; Straßburger, K.; Nowotny, P.; Kannenberg, J.M.; Strom, A.; Püttgen, S.; Müssig, K.; et al. Inflammatory Markers Are Associated with Cardiac Autonomic Dysfunction in Recent-Onset Type 2 Diabetes. Heart Br. Card. Soc. 2017, 103, 63–70. [Google Scholar] [CrossRef]
- Herder, C.; Færch, K.; Carstensen-Kirberg, M.; Lowe, G.D.; Haapakoski, R.; Witte, D.R.; Brunner, E.J.; Roden, M.; Tabák, A.G.; Kivimäki, M.; et al. Biomarkers of Subclinical Inflammation and Increases in Glycaemia, Insulin Resistance and Beta-Cell Function in Non-Diabetic Individuals: The Whitehall II Study. Eur. J. Endocrinol. 2016, 175, 367–377. [Google Scholar] [CrossRef]
- Sudo, S.Z.; Montagnoli, T.L.; Rocha, B.D.S.; Santos, A.D.; de Sá, M.P.L.; Zapata-Sudo, G. Diabetes-Induced Cardiac Autonomic Neuropathy: Impact on Heart Function and Prognosis. Biomedicines 2022, 10, 3258. [Google Scholar] [CrossRef]
- Shah, A.S.; El Ghormli, L.; Vajravelu, M.E.; Bacha, F.; Farrell, R.M.; Gidding, S.S.; Levitt Katz, L.E.; Tryggestad, J.B.; White, N.H.; Urbina, E.M. Heart Rate Variability and Cardiac Autonomic Dysfunction: Prevalence, Risk Factors, and Relationship to Arterial Stiffness in the Treatment Options for Type 2 Diabetes in Adolescents and Youth (TODAY) Study. Diabetes Care 2019, 42, 2143–2150. [Google Scholar] [CrossRef]
- Benichou, T.; Pereira, B.; Mermillod, M.; Tauveron, I.; Pfabigan, D.; Maqdasy, S.; Dutheil, F. Heart Rate Variability in Type 2 Diabetes Mellitus: A Systematic Review and Meta-Analysis. PLoS ONE 2018, 13, e0195166. [Google Scholar] [CrossRef]
- Hansen, C.S.; Vistisen, D.; Jørgensen, M.E.; Witte, D.R.; Brunner, E.J.; Tabák, A.G.; Kivimäki, M.; Roden, M.; Malik, M.; Herder, C. Adiponectin, Biomarkers of Inflammation and Changes in Cardiac Autonomic Function: Whitehall II Study. Cardiovasc. Diabetol. 2017, 16, 153. [Google Scholar] [CrossRef]
- Aljafary, M.A.; Al-Suhaimi, E.A. Adiponectin System (Rescue Hormone): The Missing Link between Metabolic and Cardiovascular Diseases. Pharmaceutics 2022, 14, 1430. [Google Scholar] [CrossRef]
- Menzaghi, C.; Trischitta, V. The Adiponectin Paradox for All-Cause and Cardiovascular Mortality. Diabetes 2018, 67, 12–22. [Google Scholar] [CrossRef]
- Zhou, Z.; Liu, C.; Xu, S.; Wang, J.; Guo, F.; Duan, S.; Deng, Q.; Sun, J.; Yu, F.; Zhou, Y.; et al. Metabolism Regulator Adiponectin Prevents Cardiac Remodeling and Ventricular Arrhythmias via Sympathetic Modulation in a Myocardial Infarction Model. Basic Res. Cardiol. 2022, 117, 34. [Google Scholar] [CrossRef] [PubMed]
- Zhu, T.; Wang, Z.; Wang, S.; Hu, W.; Chen, H.; Xie, J.; Wang, M.; Ma, K.; Jiang, H. Association between Serum Adiponectin and Atrial Fibrillation: A Case-Control Study Stratified by Age and Gender. Cardiol. Res. Pract. 2021, 2021, 6633948. [Google Scholar] [CrossRef] [PubMed]
- Jeffcoate, W.J.; Rasmussen, L.M.; Hofbauer, L.C.; Game, F.L. Medial Arterial Calcification in Diabetes and Its Relationship to Neuropathy. Diabetologia 2009, 52, 2478–2488. [Google Scholar] [CrossRef] [PubMed]
- Jhamb, S.; Vangaveti, V.N.; Malabu, U.H. Genetic and Molecular Basis of Diabetic Foot Ulcers: Clinical Review. J. Tissue Viability 2016, 25, 229–236. [Google Scholar] [CrossRef]
- Wang, Z.; Li, L.; Du, R.; Yan, J.; Liu, N.; Yuan, W.; Jiang, Y.; Xu, S.; Ye, F.; Yuan, G.; et al. CML/RAGE Signal Induces Calcification Cascade in Diabetes. Diabetol. Metab. Syndr. 2016, 8, 83. [Google Scholar] [CrossRef]
- Allman, K.C.; Stevens, M.J.; Wieland, D.M.; Hutchins, G.D.; Wolfe, E.R.; Greene, D.A.; Schwaiger, M. Noninvasive Assessment of Cardiac Diabetic Neuropathy by Carbon-11 Hydroxyephedrine and Positron Emission Tomography. J. Am. Coll. Cardiol. 1993, 22, 1425–1432. [Google Scholar] [CrossRef]
- Hamano, K.; Nakadaira, I.; Suzuki, J.; Gonai, M. N-Terminal Fragment of Probrain Natriuretic Peptide Is Associated with Diabetes Microvascular Complications in Type 2 Diabetes. Vasc. Health Risk Manag. 2014, 10, 585–589. [Google Scholar] [CrossRef]
- Jouni, H.; Rodeheffer, R.J.; Kullo, I.J. Increased Serum N-Terminal Pro–B-Type Natriuretic Peptide Levels in Patients with Medial Arterial Calcification and Poorly Compressible Leg Arteries. Arterioscler. Thromb. Vasc. Biol. 2011, 31, 197–202. [Google Scholar] [CrossRef]
- Yan, P.; Wan, Q.; Zhang, Z.; Xu, Y.; Miao, Y.; Chen, P.; Gao, C. Association between Circulating B-Type Natriuretic Peptide and Diabetic Peripheral Neuropathy: A Cross-Sectional Study of a Chinese Type 2 Diabetic Population. J. Diabetes Res. 2020, 2020, 3436549. [Google Scholar] [CrossRef] [PubMed]
- Ramzi, Z.S. N-Terminal Prohormone Brain Natriuretic Peptide as a Prognostic Biomarker for the Risk of Complications in Type 2 Diabetes: A Systematic Review and Meta-Analysis. Lab. Med. 2022, lmac119. [Google Scholar] [CrossRef] [PubMed]
- Ghanem, S.E.; Abdel-Samiee, M.; Torky, M.H.; Gaafar, A.; Mohamed, S.M.; Eldin, G.M.M.S.; Awad, S.M.; Diab, K.A.; ELsabaawy, D.M.; Yehia, S.A.; et al. Role of Resistin, IL-6 and NH2-Terminal Portion ProBNP in the Pathogenesis of Cardiac Disease in Type 2 Diabetes Mellitus. BMJ Open Diabetes Res. Care 2020, 8, e001206. [Google Scholar] [CrossRef]
- Demirtas, D.; Kucukosmanoglu, M. In Patients with Diabetic Foot, Improved Left Ventricular Functions Are Detected by Strain Echocardiography after the Diabetic Foot Treatment: A Cross-Sectional Study. Medicine 2019, 98, e17217. [Google Scholar] [CrossRef] [PubMed]
- Cameli, M.; Lisi, M.; Mondillo, S.; Padeletti, M.; Ballo, P.; Tsioulpas, C.; Bernazzali, S.; Maccherini, M. Left Atrial Longitudinal Strain by Speckle Tracking Echocardiography Correlates Well with Left Ventricular Filling Pressures in Patients with Heart Failure. Cardiovasc. Ultrasound 2010, 8, 14. [Google Scholar] [CrossRef] [PubMed]
- Marwick, T.H.; Gimelli, A.; Plein, S.; Bax, J.J.; Charron, P.; Delgado, V.; Donal, E.; Lancellotti, P.; Levelt, E.; Maurovich-Horvat, P.; et al. Multimodality Imaging Approach to Left Ventricular Dysfunction in Diabetes: An Expert Consensus Document from the European Association of Cardiovascular Imaging. Eur. Heart J.-Cardiovasc. Imaging 2022, 23, e62–e84. [Google Scholar] [CrossRef] [PubMed]
- Rubler, S.; Dlugash, J.; Yuceoglu, Y.Z.; Kumral, T.; Branwood, A.W.; Grishman, A. New Type of Cardiomyopathy Associated with Diabetic Glomerulosclerosis. Am. J. Cardiol. 1972, 30, 595–602. [Google Scholar] [CrossRef]
- Kannel, W.B.; Hjortland, M.; Castelli, W.P. Role of Diabetes in Congestive Heart Failure: The Framingham Study. Am. J. Cardiol. 1974, 34, 29–34. [Google Scholar] [CrossRef]
- Dandamudi, S.; Slusser, J.; Mahoney, D.W.; Redfield, M.M.; Rodeheffer, R.J.; Chen, H.H. The Prevalence of Diabetic Cardiomyopathy: A Population-Based Study in Olmsted County, Minnesota. J. Card. Fail. 2014, 20, 304–309. [Google Scholar] [CrossRef]
- Klajda, M.D.; Scott, C.G.; Rodeheffer, R.J.; Chen, H.H. Diabetes Mellitus Is an Independent Predictor for the Development of Heart Failure: A Population Study. Mayo Clin. Proc. 2020, 95, 124–133. [Google Scholar] [CrossRef]
- Khan, S.; Ahmad, S.S.; Kamal, M.A. Diabetic Cardiomyopathy: From Mechanism to Management in a Nutshell. Endocr. Metab. Immune Disord. Drug Targets 2021, 21, 268–281. [Google Scholar] [CrossRef] [PubMed]
- Jia, G.; Hill, M.A.; Sowers, J.R. Diabetic Cardiomyopathy: An Update of Mechanisms Contributing to This Clinical Entity. Circ. Res. 2018, 122, 624–638. [Google Scholar] [CrossRef] [PubMed]
- Marwick, T.H.; Ritchie, R.; Shaw, J.E.; Kaye, D. Implications of Underlying Mechanisms for the Recognition and Management of Diabetic Cardiomyopathy. J. Am. Coll. Cardiol. 2018, 71, 339–351. [Google Scholar] [CrossRef] [PubMed]
- Jia, G.; Whaley-Connell, A.; Sowers, J.R. Diabetic Cardiomyopathy: A Hyperglycaemia- and Insulin-Resistance-Induced Heart Disease. Diabetologia 2018, 61, 21–28. [Google Scholar] [CrossRef]
- Levelt, E.; Gulsin, G.; Neubauer, S.; McCann, G.P. MECHANISMS IN ENDOCRINOLOGY: Diabetic Cardiomyopathy: Pathophysiology and Potential Metabolic Interventions State of the Art Review. Eur. J. Endocrinol. 2018, 178, R127–R139. [Google Scholar] [CrossRef] [PubMed]
- Finck, B.N.; Lehman, J.J.; Leone, T.C.; Welch, M.J.; Bennett, M.J.; Kovacs, A.; Han, X.; Gross, R.W.; Kozak, R.; Lopaschuk, G.D.; et al. The Cardiac Phenotype Induced by PPARα Overexpression Mimics That Caused by Diabetes Mellitus. J. Clin. Investig. 2002, 109, 121–130. [Google Scholar] [CrossRef]
- Huynh, K.; Bernardo, B.C.; McMullen, J.R.; Ritchie, R.H. Diabetic Cardiomyopathy: Mechanisms and New Treatment Strategies Targeting Antioxidant Signaling Pathways. Pharmacol. Ther. 2014, 142, 375–415. [Google Scholar] [CrossRef]
- Wang, J.; Song, Y.; Wang, Q.; Kralik, P.M.; Epstein, P.N. Causes and Characteristics of Diabetic Cardiomyopathy. Rev. Diabet. Stud. 2006, 3, 108. [Google Scholar] [CrossRef]
- Grubić Rotkvić, P.; Planinić, Z.; Liberati Pršo, A.-M.; Šikić, J.; Galić, E.; Rotkvić, L. The Mystery of Diabetic Cardiomyopathy: From Early Concepts and Underlying Mechanisms to Novel Therapeutic Possibilities. Int. J. Mol. Sci. 2021, 22, 5973. [Google Scholar] [CrossRef]
- Favot, M.; Courage, C.; Ehrman, R.; Khait, L.; Levy, P. Strain Echocardiography in Acute Cardiovascular Diseases. West. J. Emerg. Med. 2016, 17, 54–60. [Google Scholar] [CrossRef]
- Negishi, K. Echocardiographic Feature of Diabetic Cardiomyopathy: Where Are We Now? Cardiovasc. Diagn. Ther. 2018, 8, 47–56. [Google Scholar] [CrossRef] [PubMed]
- Kristensen, S.L.; Mogensen, U.M.; Jhund, P.S.; Petrie, M.C.; Preiss, D.; Win, S.; Køber, L.; McKelvie, R.S.; Zile, M.R.; Anand, I.S.; et al. Clinical and Echocardiographic Characteristics and Cardiovascular Outcomes according to Diabetes Status in Patients with Heart Failure and Preserved Ejection Fraction: A Report from the I-Preserve Trial (Irbesartan in Heart Failure with Preserved Ejection Fraction). Circulation 2017, 135, 724–735. [Google Scholar] [CrossRef] [PubMed]
- Zhao, X.; Liu, S.; Wang, X.; Chen, Y.; Pang, P.; Yang, Q.; Lin, J.; Deng, S.; Wu, S.; Fan, G.; et al. Diabetic Cardiomyopathy: Clinical Phenotype and Practice. Front. Endocrinol. 2022, 13, 1032268. [Google Scholar] [CrossRef] [PubMed]
- Wamil, M.; Goncalves, M.; Rutherford, A.; Borlotti, A.; Pellikka, P.A. Multi-Modality Cardiac Imaging in the Management of Diabetic Heart Disease. Front. Cardiovasc. Med. 2022, 9, 1043711. [Google Scholar] [CrossRef] [PubMed]
- Fang, Z.Y.; Leano, R.; Marwick, T.H. Relationship between Longitudinal and Radial Contractility in Subclinical Diabetic Heart Disease. Clin. Sci. 2004, 106, 53–60. [Google Scholar] [CrossRef]
- Ernande, L.; Rietzschel, E.R.; Bergerot, C.; De Buyzere, M.L.; Schnell, F.; Groisne, L.; Ovize, M.; Croisille, P.; Moulin, P.; Gillebert, T.C.; et al. Impaired Myocardial Radial Function in Asymptomatic Patients with Type 2 Diabetes Mellitus: A Speckle-Tracking Imaging Study. J. Am. Soc. Echocardiogr. Off. Publ. Am. Soc. Echocardiogr. 2010, 23, 1266–1272. [Google Scholar] [CrossRef]
- Ernande, L.; Audureau, E.; Jellis, C.L.; Bergerot, C.; Henegar, C.; Sawaki, D.; Czibik, G.; Volpi, C.; Canoui-Poitrine, F.; Thibault, H.; et al. Clinical Implications of Echocardiographic Phenotypes of Patients with Diabetes Mellitus. J. Am. Coll. Cardiol. 2017, 70, 1704–1716. [Google Scholar] [CrossRef]
- Ernande, L.; Bergerot, C.; Girerd, N.; Thibault, H.; Davidsen, E.S.; Gautier Pignon-Blanc, P.; Amaz, C.; Croisille, P.; De Buyzere, M.L.; Rietzschel, E.R.; et al. Longitudinal Myocardial Strain Alteration Is Associated with Left Ventricular Remodeling in Asymptomatic Patients with Type 2 Diabetes Mellitus. J. Am. Soc. Echocardiogr. Off. Publ. Am. Soc. Echocardiogr. 2014, 27, 479–488. [Google Scholar] [CrossRef]
- Vukomanovic, V.; Suzic-Lazic, J.; Celic, V.; Cuspidi, C.; Grassi, G.; Galderisi, M.; Djukic, V.; Tadic, M. Is There Association between Left Atrial Function and Functional Capacity in Patients with Uncomplicated Type 2 Diabetes? Int. J. Cardiovasc. Imaging 2020, 36, 15–22. [Google Scholar] [CrossRef]
- Tadic, M.; Vukomanovic, V.; Cuspidi, C.; Suzic-Lazic, J.; Stanisavljevic, D.; Celic, V. Left Atrial Phasic Function and Heart Rate Variability in Asymptomatic Diabetic Patients. Acta Diabetol. 2017, 54, 301–308. [Google Scholar] [CrossRef]
- Tadic, M.; Cuspidi, C. Left Atrial Function in Diabetes: Does It Help? Acta Diabetol. 2021, 58, 131–137. [Google Scholar] [CrossRef] [PubMed]
- Tadic, M.; Suzic-Lazic, J.; Vukomanovic, V.; Cuspidi, C.; Ilic, S.; Celic, V. Functional Capacity and Left Ventricular Diastolic Function in Patients with Type 2 Diabetes. Acta Diabetol. 2021, 58, 107–113. [Google Scholar] [CrossRef] [PubMed]
- Bytyçi, I.; Bajraktari, G. Left Atrial Changes in Early Stages of Heart Failure with Preserved Ejection Fraction. Echocardiography 2016, 33, 1479–1487. [Google Scholar] [CrossRef]
- Moulik, P.K.; Mtonga, R.; Gill, G.V. Amputation and Mortality in New-Onset Diabetic Foot Ulcers Stratified by Etiology. Diabetes Care 2003, 26, 491–494. [Google Scholar] [CrossRef] [PubMed]
- Löndahl, M.; Katzman, P.; Fredholm, O.; Nilsson, A.; Apelqvist, J. Is Chronic Diabetic Foot Ulcer an Indicator of Cardiac Disease? J. Wound Care 2008, 17, 12–16. [Google Scholar] [CrossRef]
- Jia, Y.; Li, D.; Yu, J.; Liu, Y.; Li, F.; Li, W.; Zhang, Q.; Gao, Y.; Zhang, W.; Zeng, Z.; et al. Subclinical Cardiovascular Disease and Frailty Risk: The Atherosclerosis Risk in Communities Study. BMC Geriatr. 2022, 22, 321. [Google Scholar] [CrossRef]
- Scognamiglio, R.; Avogaro, A.; Casara, D.; Crepaldi, C.; Marin, M.; Palisi, M.; Mingardi, R.; Erle, G.; Fasoli, G.; Dalla Volta, S. Myocardial Dysfunction and Adrenergic Cardiac Innervation in Patients with Insulin-Dependent Diabetes Mellitus. J. Am. Coll. Cardiol. 1998, 31, 404–412. [Google Scholar] [CrossRef] [PubMed]
- Kuehl, M.; Stevens, M.J. Cardiovascular Autonomic Neuropathies as Complications of Diabetes Mellitus. Nat. Rev. Endocrinol. 2012, 8, 405–416. [Google Scholar] [CrossRef] [PubMed]
- Alfuhied, A.; Gulsin, G.S.; Athithan, L.; Brady, E.M.; Parke, K.; Henson, J.; Redman, E.; Marsh, A.-M.; Yates, T.; Davies, M.J.; et al. The Impact of Lifestyle Intervention on Left Atrial Function in Type 2 Diabetes: Results from the DIASTOLIC Study. Int. J. Cardiovasc. Imaging 2022, 38, 2013–2023. [Google Scholar] [CrossRef]
- Gulsin, G.S.; Swarbrick, D.J.; Athithan, L.; Brady, E.M.; Henson, J.; Baldry, E.; Argyridou, S.; Jaicim, N.B.; Squire, G.; Walters, Y.; et al. Effects of Low-Energy Diet or Exercise on Cardiovascular Function in Working-Age Adults with Type 2 Diabetes: A Prospective, Randomized, Open-Label, Blinded End Point Trial. Diabetes Care 2020, 43, 1300–1310. [Google Scholar] [CrossRef]
- Waheed, F.N.M.; Vangaveti, V.N.; Malabu, U.H. Ischemic Heart Disease and Its Risk Factors in Patients with Diabetic Foot Ulcers: A Systematic Review and Meta-Analysis. Diabetes Metab. Syndr. Clin. Res. Rev. 2022, 16, 102414. [Google Scholar] [CrossRef]
- Emerging Risk Factors Collaboration; Sarwar, N.; Gao, P.; Seshasai, S.R.K.; Gobin, R.; Kaptoge, S.; Di Angelantonio, E.; Ingelsson, E.; Lawlor, D.A.; Selvin, E.; et al. Diabetes Mellitus, Fasting Blood Glucose Concentration, and Risk of Vascular Disease: A Collaborative Meta-Analysis of 102 Prospective Studies. Lancet 2010, 375, 2215–2222. [Google Scholar] [CrossRef]
- Jupiter, D.C.; Thorud, J.C.; Buckley, C.J.; Shibuya, N. The Impact of Foot Ulceration and Amputation on Mortality in Diabetic Patients. I: From Ulceration to Death, a Systematic Review. Int. Wound J. 2016, 13, 892–903. [Google Scholar] [CrossRef] [PubMed]
- Truslow, J.G.; Goto, S.; Homilius, M.; Mow, C.; Higgins, J.M.; MacRae, C.A.; Deo, R.C. Cardiovascular Risk Assessment Using Artificial Intelligence-Enabled Event Adjudication and Hematologic Predictors. Circ. Cardiovasc. Qual. Outcomes 2022, 15, e008007. [Google Scholar] [CrossRef] [PubMed]
- Saba, L.; Biswas, M.; Kuppili, V.; Cuadrado Godia, E.; Suri, H.S.; Edla, D.R.; Omerzu, T.; Laird, J.R.; Khanna, N.N.; Mavrogeni, S.; et al. The Present and Future of Deep Learning in Radiology. Eur. J. Radiol. 2019, 114, 14–24. [Google Scholar] [CrossRef]
- Anaya-Isaza, A.; Zequera-Diaz, M. Fourier Transform-Based Data Augmentation in Deep Learning for Diabetic Foot Thermograph Classification. Biocybern. Biomed. Eng. 2022, 42, 437–452. [Google Scholar] [CrossRef]
- Goyal, M.; Reeves, N.D.; Davison, A.K.; Rajbhandari, S.; Spragg, J.; Yap, M.H. DFUNet: Convolutional Neural Networks for Diabetic Foot Ulcer Classification. IEEE Trans. Emerg. Top. Comput. Intell. 2020, 4, 728–739. [Google Scholar] [CrossRef]
- Mishra, S.C.; Chhatbar, K.C.; Kashikar, A.; Mehndiratta, A. Diabetic Foot. BMJ 2017, 359, j5064. [Google Scholar] [CrossRef] [PubMed]
- Maniruzzaman, M.; Kumar, N.; Menhazul Abedin, M.; Shaykhul Islam, M.; Suri, H.S.; El-Baz, A.S.; Suri, J.S. Comparative Approaches for Classification of Diabetes Mellitus Data: Machine Learning Paradigm. Comput. Methods Programs Biomed. 2017, 152, 23–34. [Google Scholar] [CrossRef]
- Maniruzzaman, M.; Rahman, M.J.; Al-MehediHasan, M.; Suri, H.S.; Abedin, M.M.; El-Baz, A.; Suri, J.S. Accurate Diabetes Risk Stratification Using Machine Learning: Role of Missing Value and Outliers. J. Med. Syst. 2018, 42, 92. [Google Scholar] [CrossRef]
- Khanna, N.N.; Maindarkar, M.A.; Viswanathan, V.; Puvvula, A.; Paul, S.; Bhagawati, M.; Ahluwalia, P.; Ruzsa, Z.; Sharma, A.; Kolluri, R.; et al. Cardiovascular/Stroke Risk Stratification in Diabetic Foot Infection Patients Using Deep Learning-Based Artificial Intelligence: An Investigative Study. J. Clin. Med. 2022, 11, 6844. [Google Scholar] [CrossRef] [PubMed]
- Rajkomar, A.; Dean, J.; Kohane, I. Machine Learning in Medicine. N. Engl. J. Med. 2019, 380, 1347–1358. [Google Scholar] [CrossRef]
- El-Baz, A.; Suri, J.S. Big Data in Multimodal Medical Imaging; CRC Press: Boca Raton, FL, USA, 2019; ISBN 978-1-351-38073-7. [Google Scholar]
- Goldstein, B.A.; Navar, A.M.; Carter, R.E. Moving beyond Regression Techniques in Cardiovascular Risk Prediction: Applying Machine Learning to Address Analytic Challenges. Eur. Heart J. 2017, 38, 1805–1814. [Google Scholar] [CrossRef]
- Ming, C.; Viassolo, V.; Probst-Hensch, N.; Chappuis, P.O.; Dinov, I.D.; Katapodi, M.C. Machine Learning Techniques for Personalized Breast Cancer Risk Prediction: Comparison with the BCRAT and BOADICEA Models. Breast Cancer Res. 2019, 21, 75. [Google Scholar] [CrossRef] [PubMed]
- Khanna, N.N.; Maindarkar, M.; Puvvula, A.; Paul, S.; Bhagawati, M.; Ahluwalia, P.; Ruzsa, Z.; Sharma, A.; Munjral, S.; Kolluri, R.; et al. Vascular Implications of COVID-19: Role of Radiological Imaging, Artificial Intelligence, and Tissue Characterization: A Special Report. J. Cardiovasc. Dev. Dis. 2022, 9, 268. [Google Scholar] [CrossRef]
- Jamthikar, A.; Gupta, D.; Khanna, N.N.; Saba, L.; Laird, J.R.; Suri, J.S. Cardiovascular/Stroke Risk Prevention: A New Machine Learning Framework Integrating Carotid Ultrasound Image-Based Phenotypes and Its Harmonics with Conventional Risk Factors. Indian Heart J. 2020, 72, 258–264. [Google Scholar] [CrossRef] [PubMed]
- Jamthikar, A.D.; Gupta, D.; Saba, L.; Khanna, N.N.; Viskovic, K.; Mavrogeni, S.; Laird, J.R.; Sattar, N.; Johri, A.M.; Pareek, G.; et al. Artificial Intelligence Framework for Predictive Cardiovascular and Stroke Risk Assessment Models: A Narrative Review of Integrated Approaches Using Carotid Ultrasound. Comput. Biol. Med. 2020, 126, 104043. [Google Scholar] [CrossRef]
- Derevitskii, I.V.; Kovalchuk, S.V. Machine Learning-Based Predictive Modeling of Complications of Chronic Diabetes. Procedia Comput. Sci. 2020, 178, 274–283. [Google Scholar] [CrossRef]
- Jamthikar, A.D.; Gupta, D.; Mantella, L.E.; Saba, L.; Laird, J.R.; Johri, A.M.; Suri, J.S. Multiclass Machine Learning vs. Conventional Calculators for Stroke/CVD Risk Assessment Using Carotid Plaque Predictors with Coronary Angiography Scores as Gold Standard: A 500 Participants Study. Int. J. Cardiovasc. Imaging 2021, 37, 1171–1187. [Google Scholar] [CrossRef]
- Chemello, G.; Salvatori, B.; Morettini, M.; Tura, A. Artificial Intelligence Methodologies Applied to Technologies for Screening, Diagnosis and Care of the Diabetic Foot: A Narrative Review. Biosensors 2022, 12, 985. [Google Scholar] [CrossRef]
- Howard, T.; Ahluwalia, R.; Papanas, N. The Advent of Artificial Intelligence in Diabetic Foot Medicine: A New Horizon, a New Order, or a False Dawn? Int. J. Low. Extrem. Wounds 2021. [Google Scholar] [CrossRef] [PubMed]
- Kaselimi, M.; Protopapadakis, E.; Doulamis, A.; Doulamis, N. A Review of Non-Invasive Sensors and Artificial Intelligence Models for Diabetic Foot Monitoring. Front. Physiol. 2022, 13, 924546. [Google Scholar] [CrossRef]
- Yap, M.H.; Hachiuma, R.; Alavi, A.; Brüngel, R.; Cassidy, B.; Goyal, M.; Zhu, H.; Rückert, J.; Olshansky, M.; Huang, X.; et al. Deep Learning in Diabetic Foot Ulcers Detection: A Comprehensive Evaluation. Comput. Biol. Med. 2021, 135, 104596. [Google Scholar] [CrossRef] [PubMed]
- Young, J.B.; Gauthier-Loiselle, M.; Bailey, R.A.; Manceur, A.M.; Lefebvre, P.; Greenberg, M.; Lafeuille, M.-H.; Duh, M.S.; Bookhart, B.; Wysham, C.H. Development of Predictive Risk Models for Major Adverse Cardiovascular Events among Patients with Type 2 Diabetes Mellitus Using Health Insurance Claims Data. Cardiovasc. Diabetol. 2018, 17, 118. [Google Scholar] [CrossRef]
- Wilson, P.W.F.; D’Agostino, R.B.; Levy, D.; Belanger, A.M.; Silbershatz, H.; Kannel, W.B. Prediction of Coronary Heart Disease Using Risk Factor Categories. Circulation 1998, 97, 1837–1847. [Google Scholar] [CrossRef]
- D’Agostino, R.B.; Vasan, R.S.; Pencina, M.J.; Wolf, P.A.; Cobain, M.; Massaro, J.M.; Kannel, W.B. General Cardiovascular Risk Profile for Use in Primary Care: The Framingham Heart Study. Circulation 2008, 117, 743–753. [Google Scholar] [CrossRef] [PubMed]
- Coleman, R.L.; Stevens, R.J.; Retnakaran, R.; Holman, R.R. Framingham, SCORE, and DECODE Risk Equations Do Not Provide Reliable Cardiovascular Risk Estimates in Type 2 Diabetes. Diabetes Care 2007, 30, 1292–1293. [Google Scholar] [CrossRef]
- Kengne, A.P.; Patel, A.; Colagiuri, S.; Heller, S.; Hamet, P.; Marre, M.; Pan, C.Y.; Zoungas, S.; Grobbee, D.E.; Neal, B.; et al. The Framingham and UK Prospective Diabetes Study (UKPDS) Risk Equations Do Not Reliably Estimate the Probability of Cardiovascular Events in a Large Ethnically Diverse Sample of Patients with Diabetes: The Action in Diabetes and Vascular Disease: Preterax and Diamicron-MR Controlled Evaluation (ADVANCE) Study. Diabetologia 2010, 53, 821–831. [Google Scholar] [CrossRef]
- Kothari, V.; Stevens, R.J.; Adler, A.I.; Stratton, I.M.; Manley, S.E.; Neil, H.A.; Holman, R.R. UKPDS 60: Risk of Stroke in Type 2 Diabetes Estimated by the UK Prospective Diabetes Study Risk Engine. Stroke 2002, 33, 1776–1781. [Google Scholar] [CrossRef]
- Stevens, R.J.; Kothari, V.; Adler, A.I.; Stratton, I.M.; United Kingdom Prospective Diabetes Study (UKPDS) Group. The UKPDS Risk Engine: A Model for the Risk of Coronary Heart Disease in Type II Diabetes (UKPDS 56). Clin. Sci. 2001, 101, 671–679. [Google Scholar] [CrossRef]
- Mu, X.; Wu, A.; Hu, H.; Zhou, H.; Yang, M. Assessment of QRISK3 as a Predictor of Cardiovascular Disease Events in Type 2 Diabetes Mellitus. Front. Endocrinol. 2022, 13, 1077632. [Google Scholar] [CrossRef]
- Hippisley-Cox, J.; Coupland, C.; Brindle, P. Development and Validation of QRISK3 Risk Prediction Algorithms to Estimate Future Risk of Cardiovascular Disease: Prospective Cohort Study. BMJ 2017, 357, j2099. [Google Scholar] [CrossRef]
- Livingstone, S.J.; Guthrie, B.; Donnan, P.T.; Thompson, A.; Morales, D.R. Predictive Performance of a Competing Risk Cardiovascular Prediction Tool CRISK Compared to QRISK3 in Older People and Those with Comorbidity: Population Cohort Study. BMC Med. 2022, 20, 152. [Google Scholar] [CrossRef] [PubMed]
- Khera, A.V.; Chaffin, M.; Aragam, K.G.; Haas, M.E.; Roselli, C.; Choi, S.H.; Natarajan, P.; Lander, E.S.; Lubitz, S.A.; Ellinor, P.T.; et al. Genome-Wide Polygenic Scores for Common Diseases Identify Individuals with Risk Equivalent to Monogenic Mutations. Nat. Genet. 2018, 50, 1219–1224. [Google Scholar] [CrossRef] [PubMed]
- Khera, A.V.; Emdin, C.A.; Drake, I.; Natarajan, P.; Bick, A.G.; Cook, N.R.; Chasman, D.I.; Baber, U.; Mehran, R.; Rader, D.J.; et al. Genetic Risk, Adherence to a Healthy Lifestyle, and Coronary Disease. N. Engl. J. Med. 2016, 375, 2349–2358. [Google Scholar] [CrossRef] [PubMed]
- Rezaee, M.; Putrenko, I.; Takeh, A.; Ganna, A.; Ingelsson, E. Development and Validation of Risk Prediction Models for Multiple Cardiovascular Diseases and Type 2 Diabetes. PLoS ONE 2020, 15, e0235758. [Google Scholar] [CrossRef] [PubMed]
- Ruiz-Canela, M.; Hruby, A.; Clish, C.B.; Liang, L.; Martínez-González, M.A.; Hu, F.B. Comprehensive Metabolomic Profiling and Incident Cardiovascular Disease: A Systematic Review. J. Am. Heart Assoc. 2017, 6, e005705. [Google Scholar] [CrossRef] [PubMed]
- Ganna, A.; Salihovic, S.; Sundström, J.; Broeckling, C.D.; Hedman, A.K.; Magnusson, P.K.E.; Pedersen, N.L.; Larsson, A.; Siegbahn, A.; Zilmer, M.; et al. Large-Scale Metabolomic Profiling Identifies Novel Biomarkers for Incident Coronary Heart Disease. PLoS Genet. 2014, 10, e1004801. [Google Scholar] [CrossRef]
- Galbete, A.; Tamayo, I.; Librero, J.; Enguita-Germán, M.; Cambra, K.; Ibáñez-Beroiz, B. Cardiovascular Risk in Patients with Type 2 Diabetes: A Systematic Review of Prediction Models. Diabetes Res. Clin. Pract. 2022, 184, 109089. [Google Scholar] [CrossRef]
- Westermann, D.; Rutschow, S.; Van Linthout, S.; Linderer, A.; Bücker-Gärtner, C.; Sobirey, M.; Riad, A.; Pauschinger, M.; Schultheiss, H.-P.; Tschöpe, C. Inhibition of P38 Mitogen-Activated Protein Kinase Attenuates Left Ventricular Dysfunction by Mediating pro-Inflammatory Cardiac Cytokine Levels in a Mouse Model of Diabetes Mellitus. Diabetologia 2006, 49, 2507–2513. [Google Scholar] [CrossRef]
- Barbati, S.A.; Colussi, C.; Bacci, L.; Aiello, A.; Re, A.; Stigliano, E.; Isidori, A.M.; Grassi, C.; Pontecorvi, A.; Farsetti, A.; et al. Transcription Factor CREM Mediates High Glucose Response in Cardiomyocytes and in a Male Mouse Model of Prolonged Hyperglycemia. Endocrinology 2017, 158, 2391–2405. [Google Scholar] [CrossRef]
- Zhang, Z.; Wang, S.; Zhou, S.; Yan, X.; Wang, Y.; Chen, J.; Mellen, N.; Kong, M.; Gu, J.; Tan, Y.; et al. Sulforaphane Prevents the Development of Cardiomyopathy in Type 2 Diabetic Mice Probably by Reversing Oxidative Stress-Induced Inhibition of LKB1/AMPK Pathway. J. Mol. Cell. Cardiol. 2014, 77, 42–52. [Google Scholar] [CrossRef]
- Wang, X.; Gu, H.; Huang, W.; Peng, J.; Li, Y.; Yang, L.; Qin, D.; Essandoh, K.; Wang, Y.; Peng, T.; et al. Hsp20-Mediated Activation of Exosome Biogenesis in Cardiomyocytes Improves Cardiac Function and Angiogenesis in Diabetic Mice. Diabetes 2016, 65, 3111–3128. [Google Scholar] [CrossRef] [PubMed]
- Bastin, M.; Andreelli, F. The Gut Microbiota and Diabetic Cardiomyopathy in Humans. Diabetes Metab. 2020, 46, 197–202. [Google Scholar] [CrossRef] [PubMed]
- Katare, R.; Caporali, A.; Zentilin, L.; Avolio, E.; Sala-Newby, G.; Oikawa, A.; Cesselli, D.; Beltrami, A.P.; Giacca, M.; Emanueli, C.; et al. Intravenous Gene Therapy with PIM-1 Via a Cardiotropic Viral Vector Halts the Progression of Diabetic Cardiomyopathy Through Promotion of Prosurvival Signaling. Circ. Res. 2011, 108, 1238–1251. [Google Scholar] [CrossRef]
- Jeffcoate, W.J.; Game, F.; Cavanagh, P.R. The Role of Proinflammatory Cytokines in the Cause of Neuropathic Osteoarthropathy (Acute Charcot Foot) in Diabetes. Lancet 2005, 366, 2058–2061. [Google Scholar] [CrossRef] [PubMed]
- Marmolejo, V.S.; Arnold, J.F.; Ponticello, M.; Andersen, C.A. Charcot Foot: Clinical Clues, Diagnostic Strategies, and Treatment Principles. Am. Fam. Physician 2018, 97, 594–599. [Google Scholar] [PubMed]
- Schweitzer, M.; Rockhill, S. Conservative Management of Charcot Neuroarthropathy. Clin. Podiatr. Med. Surg. 2022, 39, 585–594. [Google Scholar] [CrossRef]
- Greco, T.; Mascio, A.; Comisi, C.; Polichetti, C.; Caravelli, S.; Mosca, M.; Mondanelli, N.; Troiano, E.; Maccauro, G.; Perisano, C. RANKL-RANK-OPG Pathway in Charcot Diabetic Foot: Pathophysiology and Clinical-Therapeutic Implications. Int. J. Mol. Sci. 2023, 24, 3014. [Google Scholar] [CrossRef]
- Carvès, S.; Bourgeon-Ghittori, M.; Henry, J.; Belkhir, R.; Besson, F.L.; Levante, S.; Mariette, X.; Seror, R. Denosumab in Active Charcot Neuro-Osteoarthropathy of the Foot. Jt. Bone Spine 2021, 88, 105241. [Google Scholar] [CrossRef]
- Busch-Westbroek, T.E.; Delpeut, K.; Balm, R.; Bus, S.A.; Schepers, T.; Peters, E.J.; Smithuis, F.F.; Maas, M.; Nieuwdorp, M. Effect of Single Dose of RANKL Antibody Treatment on Acute Charcot Neuro-Osteoarthropathy of the Foot. Diabetes Care 2018, 41, e21–e22. [Google Scholar] [CrossRef]
- Shofler, D.; Hamedani, E.; Seun, J.; Sathananthan, A.; Katsaros, E.; Liggan, L.; Kang, S.; Pham, C. Investigating the Use of Denosumab in the Treatment of Acute Charcot Neuroarthropathy. J. Foot Ankle Surg. 2021, 60, 354–357. [Google Scholar] [CrossRef] [PubMed]
- Golledge, J.; Thanigaimani, S. Novel Therapeutic Targets for Diabetes-Related Wounds or Ulcers: An Update on Preclinical and Clinical Research. Expert Opin. Ther. Targets 2021, 25, 1061–1075. [Google Scholar] [CrossRef] [PubMed]
- Serban, D.; Papanas, N.; Dascalu, A.M.; Kempler, P.; Raz, I.; Rizvi, A.A.; Rizzo, M.; Tudor, C.; Silviu Tudosie, M.; Tanasescu, D.; et al. Significance of Neutrophil to Lymphocyte Ratio (NLR) and Platelet Lymphocyte Ratio (PLR) in Diabetic Foot Ulcer and Potential New Therapeutic Targets. Int. J. Low. Extrem. Wounds 2021. [Google Scholar] [CrossRef]
- Chen, W.; Chen, K.; Xu, Z.; Hu, Y.; Liu, Y.; Liu, W.; Hu, X.; Ye, T.; Hong, J.; Zhu, H.; et al. Neutrophil-to-Lymphocyte Ratio and Platelet-to-Lymphocyte Ratio Predict Mortality in Patients with Diabetic Foot Ulcers Undergoing Amputations. Diabetes Metab. Syndr. Obes. Targets Ther. 2021, 14, 821–829. [Google Scholar] [CrossRef] [PubMed]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Adam, C.A.; Marcu, D.T.M.; Mitu, O.; Roca, M.; Aursulesei Onofrei, V.; Zabara, M.L.; Tribuș, L.C.; Cumpăt, C.; Crișan Dabija, R.; Mitu, F. Old and Novel Predictors for Cardiovascular Risk in Diabetic Foot Syndrome—A Narrative Review. Appl. Sci. 2023, 13, 5990. https://doi.org/10.3390/app13105990
Adam CA, Marcu DTM, Mitu O, Roca M, Aursulesei Onofrei V, Zabara ML, Tribuș LC, Cumpăt C, Crișan Dabija R, Mitu F. Old and Novel Predictors for Cardiovascular Risk in Diabetic Foot Syndrome—A Narrative Review. Applied Sciences. 2023; 13(10):5990. https://doi.org/10.3390/app13105990
Chicago/Turabian StyleAdam, Cristina Andreea, Dragos Traian Marius Marcu, Ovidiu Mitu, Mihai Roca, Viviana Aursulesei Onofrei, Mihai Lucian Zabara, Laura Carina Tribuș, Carmen Cumpăt, Radu Crișan Dabija, and Florin Mitu. 2023. "Old and Novel Predictors for Cardiovascular Risk in Diabetic Foot Syndrome—A Narrative Review" Applied Sciences 13, no. 10: 5990. https://doi.org/10.3390/app13105990
APA StyleAdam, C. A., Marcu, D. T. M., Mitu, O., Roca, M., Aursulesei Onofrei, V., Zabara, M. L., Tribuș, L. C., Cumpăt, C., Crișan Dabija, R., & Mitu, F. (2023). Old and Novel Predictors for Cardiovascular Risk in Diabetic Foot Syndrome—A Narrative Review. Applied Sciences, 13(10), 5990. https://doi.org/10.3390/app13105990








