Abstract
It is common to detect a gap between the apical portion of the post and the most coronal part of gutta-percha in a root canal during post and core treatment in endodontically treated teeth. It may compromise the seal that gutta-percha material provides in the root canal filling, leading to apical leakage, which is often thought to be one of the most common causes for failure of endodontic treatment. The prevention of apical leakage to achieve a complete apical seal and its effect on periapical health of endodontically treated teeth of post and core in long term clinical research remains unanswered. Post and core treatment were provided to 100 patients by undergraduate students in the year 2016–2017. A total of 70 patients in all were called back to the Prosthodontic Clinic for follow-up care after 4 years to assess the clinical result in terms of the gap between the post-operative and residual gutta-percha. The cemented posts were divided into three groups depending on the space between the cemented post end and the remaining gutta-percha: group I revealed no gaps, group II revealed gaps between >0.1 and 1 mm, and group III revealed gaps more than 1 mm. The periapical index (PAI) was used to determine the apical condition of each tooth. Chi-square test was used for evaluating the data, and a p-value of 0.05 was considered statistically significant. A total of 28.6% post and core treated teeth were found diseased while 71.4% teeth were found normal. In group I, 90% of the teeth and in group II, 66.7% of teeth were evaluated as normal; however, in group III, 41.2% teeth were found diseased. In endodontically treated teeth restored with a post and core, a gap between the apical end of the post and the coronal section of the residual gutta-percha was associated with a greater prevalence of disease. The post and core treatment by undergraduate students achieved a clinically acceptable outcome in terms of the gap between the post end and the remaining gutta-percha.
1. Introduction
In the era of modern dentistry, where dental implants are constantly on the rise, post and core treatment procedures play an important role by retaining grossly decayed teeth for a longer period of time [1]. The use of post and core restorations makes it possible to reconstruct the severely decayed teeth that have undergone endodontic therapy rather than extracting and replacing them, allowing patients to keep their own teeth [2]. After undergoing root canal therapy, teeth with severe coronal tooth structural loss are more susceptible to fracture. Following the fundamental concepts of retention and resistance form for an artificial crown for coronal restoration, a post is put in the root canal space of such teeth to support the core which provides the appropriate coronal structure [3,4]. The core part can be fabricated separately and fixed mechanically or chemically onto the post as in a prefabricated post and core system, or it can be cast along with the post as in the conventional custom cast post and core system [5]. The standard preparation for a post space constitutes parallel sides and radicular dentine walls that can be up to 1 mm thick [6]. Underneath the post space preparation, 3 to 5 mm of gutta-percha remains intact as endodontic filling material in the apical third region [7]. The required post length and the root form of teeth that have undergone endodontic treatment determine the ideal depth for post space preparation. Longer posts have greater retention of posts [8]. Typically, the teeth that need post and core restorations have minimum residual sound tooth structure. Before considering a post-core restoration, it is necessary to assess the amount of remaining tooth structure, its location, and if an adequate ferrule is available [9]. While creating the post space, attention must be exercised to prevent compromising the integrity of the apical seal [10]. When the apical seal fails to remain intact, the tooth may get reinfected and require retreatment [11]. The penetration of bacteria or other infectious materials or exudates into the root canal and vice versa from the peri-radicular spaces can be reduced by an effective apical seal [12]. Numerous studies suggest maintaining 4–5 mm of apical gutta-percha to maintain an effective apical seal [13,14].
Endodontically treated teeth with loss of significant tooth structure require sophisticated treatments that require a high level of skill and competence to restore the compromised teeth with post and core. In consideration of this, it is crucial that dentistry undergraduate students acquire adequate training prior to carrying out the post and core treatment on patients. The post and core basic procedures are provided in the preclinical training in the fixed prosthodontic curriculum at dental schools. Preclinical training has been shown to be an essential factor for ensuring a seamless transition to the clinical environment for undergraduate students [15]. In fixed prosthodontics, there is a well-established positive association between preclinical and clinical grades [16]. It has been demonstrated that teaching in dental simulation clinics is vital for preclinical education so that students may gain practical skills [17]. In preclinical fixed prosthodontic teaching methods, simulation clinic teaching has been widely employed. In these methods, students often complete a series of formative practical activities that conclude with a summative practical assessment [18].
The space between the apical portion of the post and the most coronal section of the gutta-percha that typically remains after the post has been inserted into the root canal of a tooth that has undergone endodontic therapy, can be a crucial determining factor in the prognosis of the treatment due to the presence of microorganisms. Only a few research studies have investigated how this gap may impact the clinical outcome of teeth that have undergone post and core treatment after endodontic therapy. The effectiveness of preclinical training for undergraduate students to assess the clinical success of endodontically treated teeth rebuilt with post and core in terms of the space between post and residual gutta-percha with 4 years of follow up has not been studied in a clinical trial as of yet. The null-hypothesis is that the gap between the cemented post end and any remaining gutta-percha would have an unfavorable effect on the periapical health of teeth with post and core restorations that had received endodontic therapy.
2. Materials and Methods
The current study used a cross-sectional retrospective research approach. A total of 100 patients received post and core treatment after endodontic therapy in 2016–2017 from final year undergraduate dental students at Jazan University in Saudi Arabia. The same undergraduate students had already been trained to execute the post and core basic procedures on typodont teeth as part of their preclinical training in fixed prosthodontics. Prior to the commencement of the study, an ethical clearance with the approval reference number REC42/1/051 was received. The sample size was estimated using R statistical software, version 3.3.1 (R Core Team 2016; R Foundation for Statistical Computing, Vienna, Austria). The optimal sample size was determined using a one-way analysis of variance power calculation for more than two groups. The findings indicated that a sample size of 75 endodontically treated teeth would be sufficient to reject the null-hypothesis with a power of 90% and a two-sided significance level of 5%.
According to the following inclusion criteria, subjects were included in the study:
- Patients who had received post and core treatment after root canal therapy by undergraduate students.
- After the post-and-core therapy, digital periapical radiographs had been acquired and were included in the patient records.
Subjects were disqualified from the research based on the following criteria:
- Post and core treatment executed by specialists or interns.
- Any variable that could affect the result of root-canal therapy. For example, a broken instrument or file in the root canal, or overextended or underextended root canal fillings, calcified canals, or root fractures.
- Any distortions in the radiographs.
Final year undergraduate students performed the post and core treatment on the endodontically treated teeth with compromised tooth structure. Diagnostic preparation was performed to evaluate the remaining tooth structure and ferrule. An intraoral periapical radiograph was made to evaluate the post space preparation. Depending on the shape, diameter, length, and curvature of the root canal, Gates Glidden drills and peeso reamers (MANI, Utsunomiya, Japan, size #1 to #6) were used in the sequence to prepare the post space. In order to maintain the periapical seal, the root canal was prepared in such a way that the remaining 5 mm of gutta-percha was left to maintain the apical seal. An intraoral periapical radiograph was made to confirm the post space preparation and remaining gutta-percha. Based on the diameter and length of the prepared post space, the length and diameter of the prefabricated glass fiber post (3M RelyX, St. Paul, MN, USA) was selected. A universal twist drill, supplied by the manufacturer, corresponding to the selected prefabricated post was used to shape the canal before cementation. The entire procedure was carried out under rubber dam isolation. The prefabricated glass fiber post was cemented with self-adhesive resin cement (3M RelyX Unicem 2 Automix, St. Paul, MN, USA). Custom cast posts were fabricated using an indirect method. The separating media was applied to the prepared post space with paper points. The plastic posts (Spee-Dee plastic pins, Pulpdent corporation, Watertown, MA, USA) were used to make the post space impression using pattern resin (Pattern Resin LS, GC America Inc., Alsip, IL, USA). After the initial set, the pattern was moved up and down to assure that it came out passively. After that, the core component of the crown was shaped with the pattern resin according to the shape of the future abutment. The manufacturer’s instructions were followed while spruing, investing, and casting. The retrieved castings were evaluated intraorally for their fit and minor adjustments were performed. The metal cast posts were cemented with zinc phosphate cement (Primedent, St. Paul, MN, USA). The canal may be recontaminated in various ways such as contact between the oral bacterial flora and root canal tubule inlets. However, it most frequently occurs due to loss of temporary filling material or inadequate endodontic permanent restoration or crown sealing. A contra bevel was prepared to produce a cast core with a collar of metal that encircles the tooth and acts as secondary ferrule and provides the adequate coronal seal to the metal post.
A total of 100 patients who received post and core treatments from undergraduate students in 2016–2017, were contacted four years later for follow-up evaluation. A total of 70 patients reported to the clinic in 2020–2021. To assess the endodontically treated teeth restored with glass fiber posts and cast posts in the maxillary and mandibular arches, clinical and radiographic examinations were carried out. Intraoral peri-apical radiographs of the cemented posts were taken using the paralleling approach technique to reduce the chances of distortion. The digital periapical radiographs were assessed using the CS-R4 program (CSR4 with Practice Management Software version 4, Carestream Dental LLC, Atlanta, GA, USA).
All subjects were categorized into three groups based on the gap present between the apical portion of the cemented post and the residual remaining gutta-percha in the radiograph [19].
Group I: There was no gap between the remaining gutta-percha and cemented post end.
Group II: The remaining gutta-percha and the cemented post end were separated by a gap that measured more than 0 mm but less than 1 mm.
Group III: The remaining gutta-percha and the cemented post end were separated by a gap that measured more than 1 mm.
The same participants were divided into three groups as well, in order to determine how much gutta-percha was still present after the post- and core-procedure [10,20,21,22].
Group IV: The amount of gutta-percha left was less than 3 mm.
Group V: The amount of gutta-percha left was between 3 to 5 mm.
Group VI: The amount of gutta-percha left was more than 5 mm.
The periapical index (PAI) was used to determine the apical condition of each tooth as follows [23]:
- Normal periapical region present
- Minor changes in bone structure present
- Moderate changes in the bone structure present
- Periodontitis with well-defined radiolucent area present
- Severe periodontitis with exacerbating features present
A healthy periapex was designated as PAI 1, showing a normal width of periodontal ligament space and a normal look of the surrounding bone. All other PAI score (2,3,4,5) values were indicated as apical periodontitis. In order to prevent bias, the coronal portion of every radiograph was covered with cardboard. The radiographs were assessed according to the following criteria:
Normal: The periodontal ligament was intact and the periapical region was free of radiolucency. (PAI 1)
Disease: Periapical radiolucency or a widening of the PDL gap was present. (PAI 2,3,4,5)
All clinical and radiographic examinations were evaluated independently by two examiners. Both examiners went through a calibration phase before performing the clinical and radiographic evaluation. During the calibration phase, the examiners received clear explanations of the study approach. Ten teeth were initially examined in order to calibrate both examiners, and Cohen’s kappa (kappa 0.91) was used to find inter-examiner agreement. The examination room was made darker to regulate the ambient light and provide the best radiographic image quality and radiographic contrast. Whenever there was a disagreement between the first two examiners, a prosthodontist with ten years of professional experience, the third observer, was asked to make a final decision. Each radiographic measurement was triple recorded by one experienced investigator after software calibration for linear measurement. The average of three values was obtained in order to reduce the intra-observer error. Between December 2021 and March 2022, clinical and radiological data were gathered. The gaps between the post and remaining gutta-percha were taken into account when grouping all of the qualitative data into three different groups. The post- and core-treated teeth carried out by the male and female undergraduate students were also taken into account when grouping these results. Microsoft Excel software (version 2016) was used to analyze the data and create a tabular summary of the findings. Using the SPSS statistical analysis program, a chi-square test of independence was performed on each result (version 21, SPSS, Chicago, IL, USA) with the level of significance set at p = 0.05.
3. Results
A total of 70 cases were evaluated for the follow up examination.
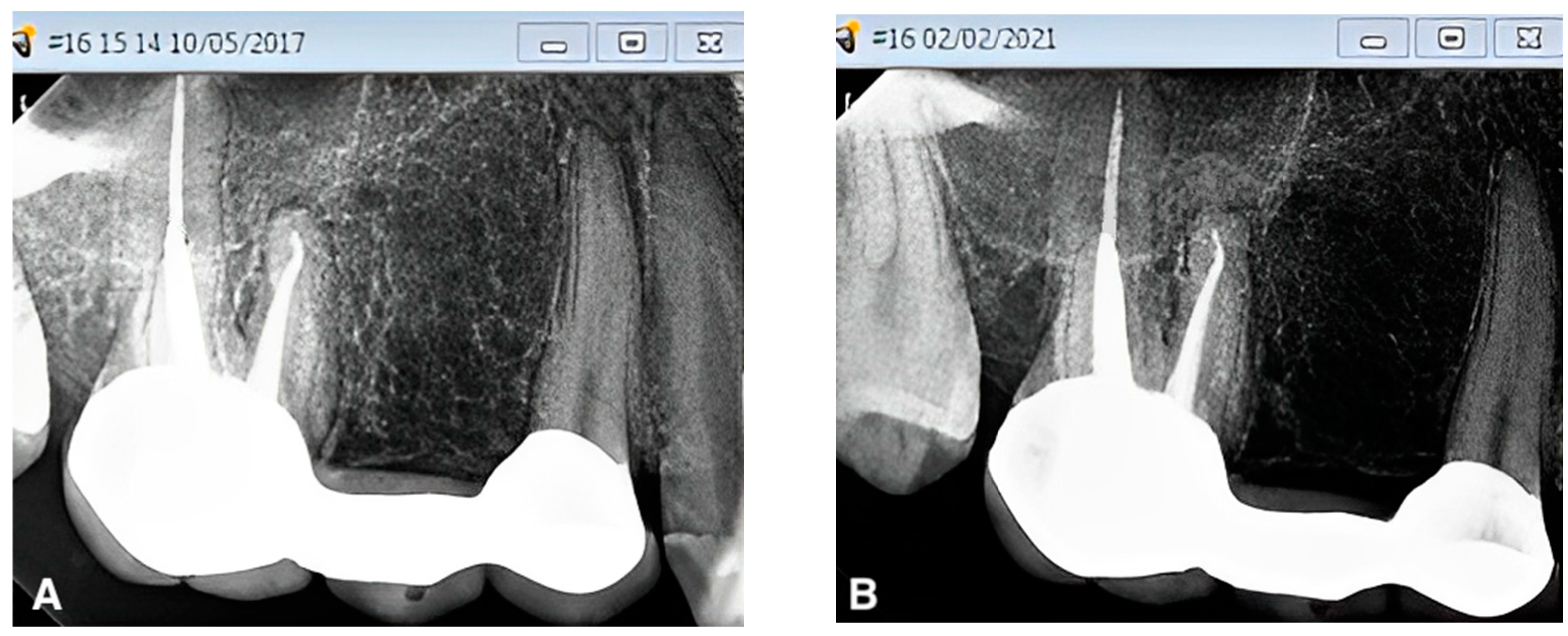
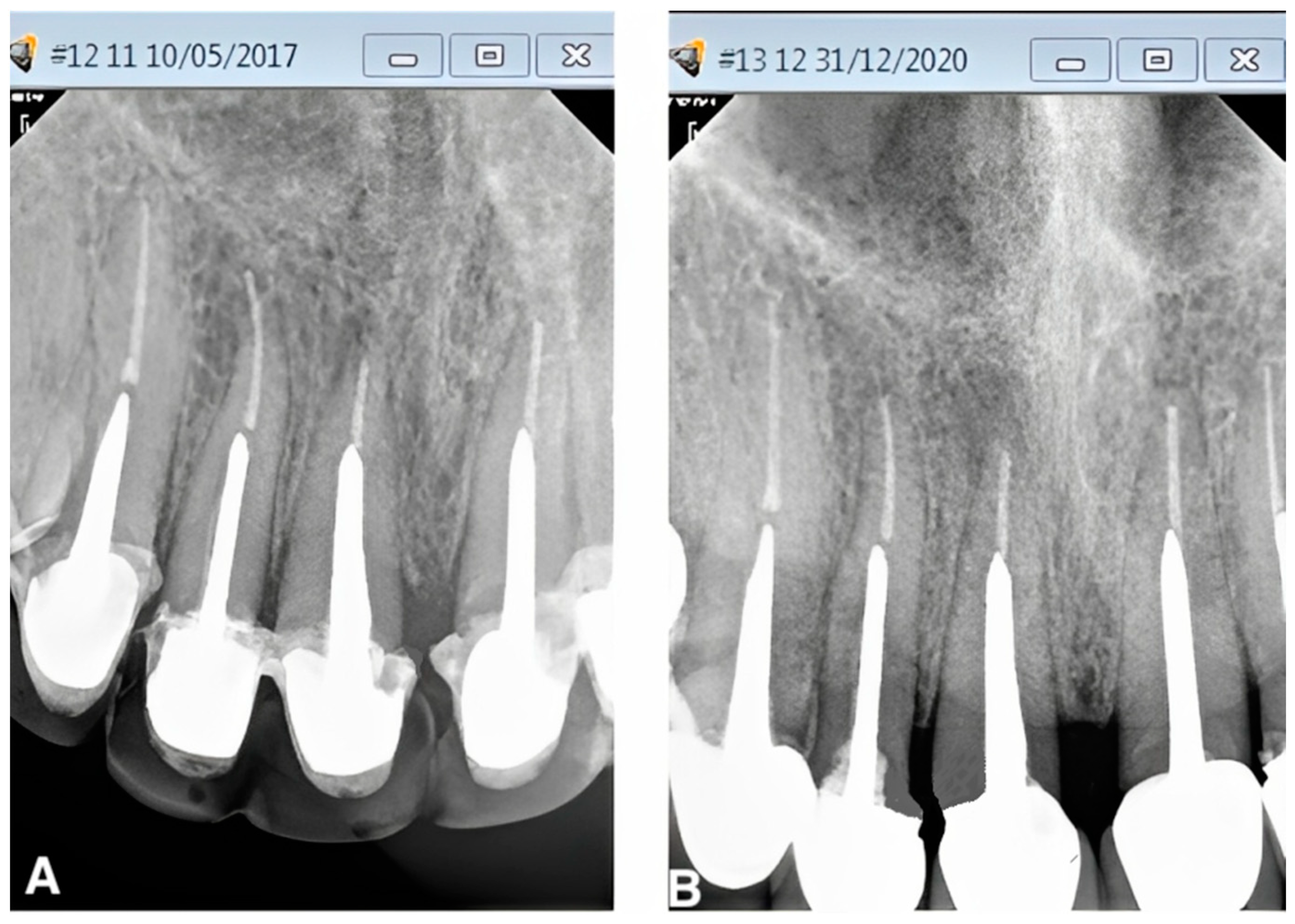
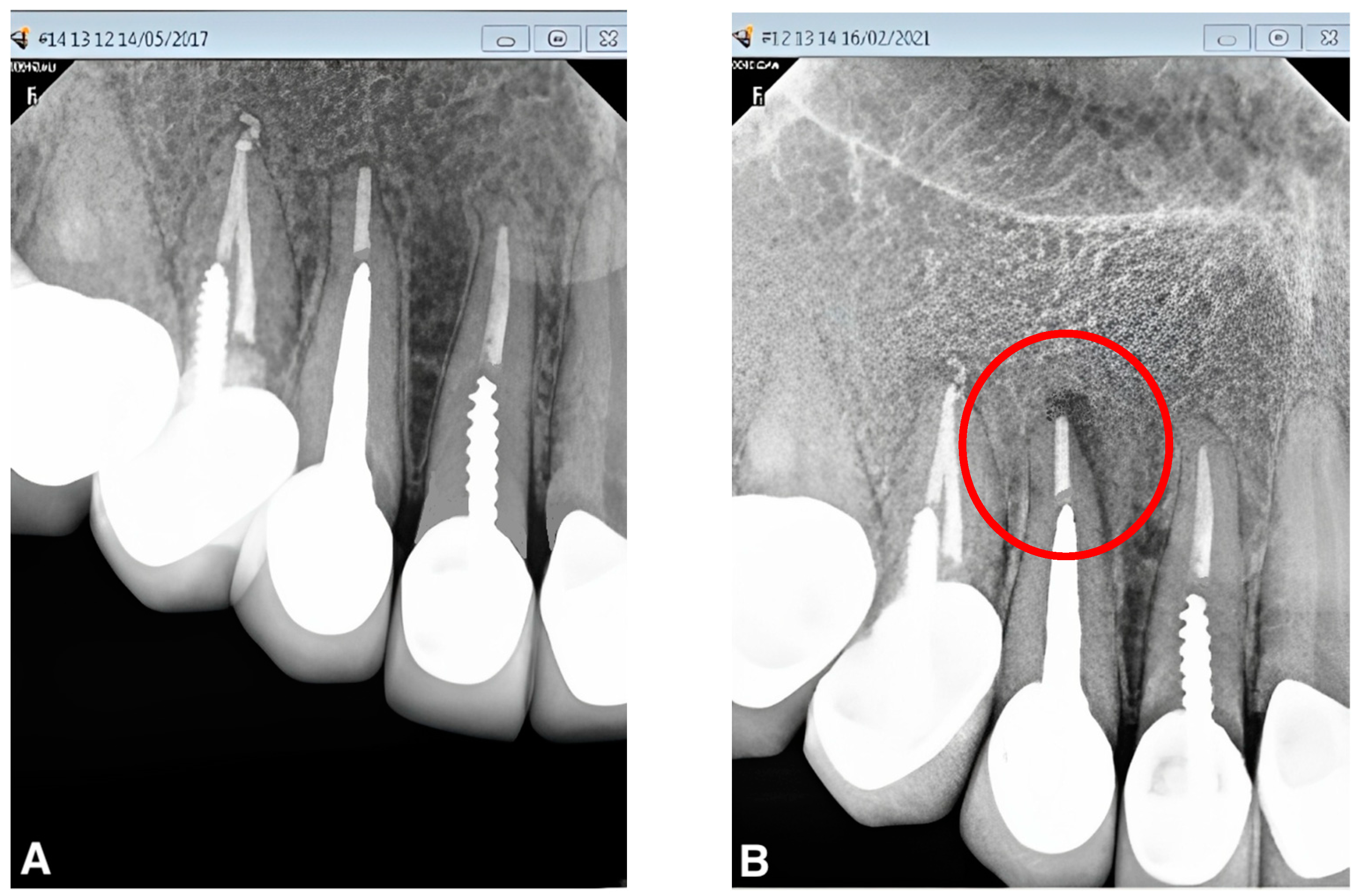
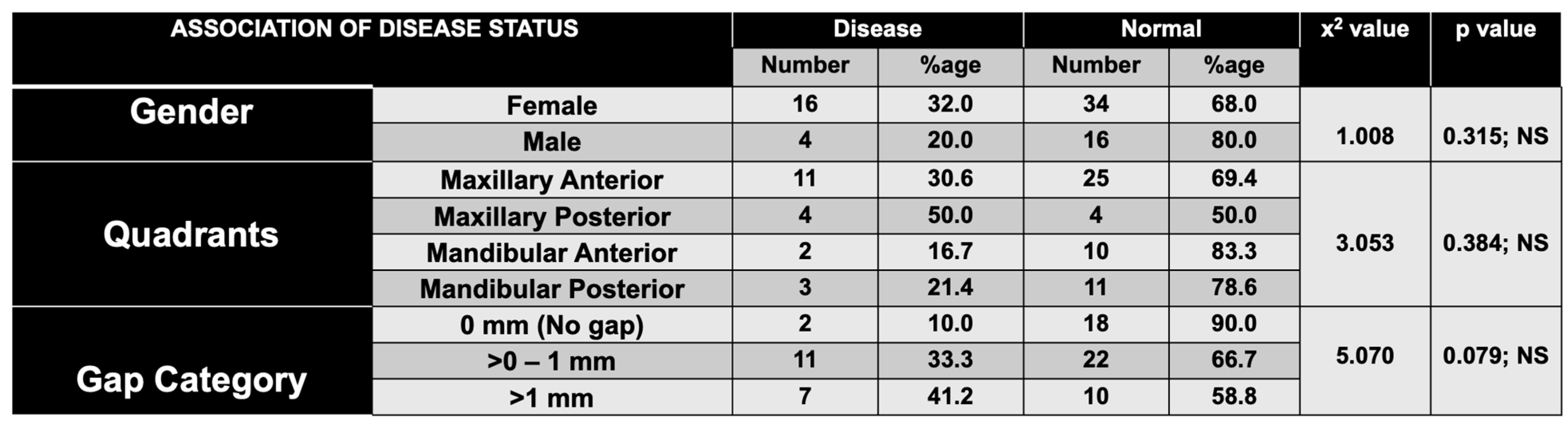
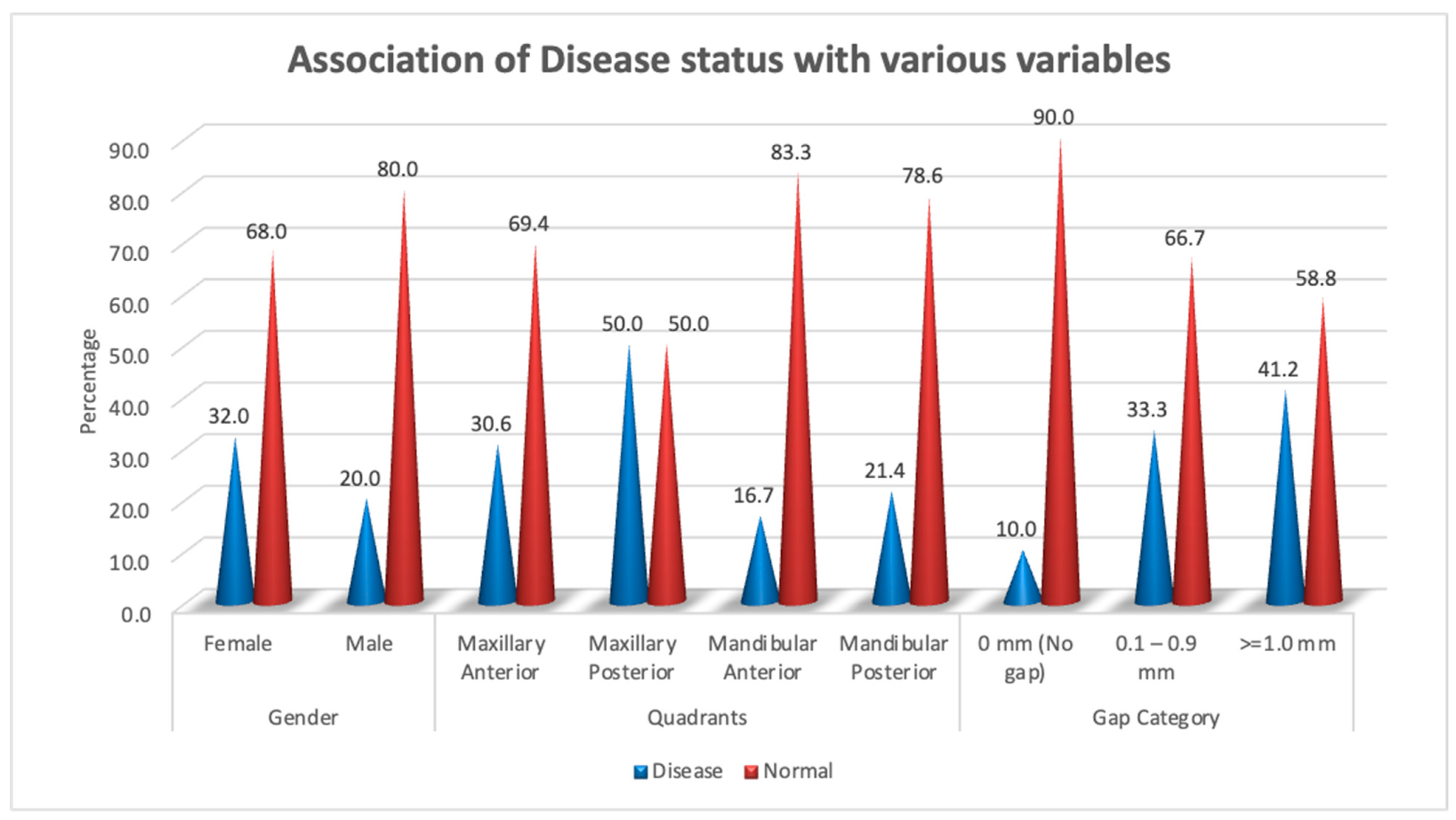
A healthy periapex PAI 1 was described as a healthy periapex, which had the normal width of permanent ligament space and surrounding bone that looked normal. The evaluation of all other PAI scores (2,3,4,5) was mentioned as apical periodontitis. The chi-square test was employed for statistical analysis, with a significance level of p < 0.05. Out of 70 recalled patients, the male students had performed a total of 20 post and core treatments, whereas the female undergraduate students had completed post and core treatments for 50 cases. A total of 90% (n = 18) of the teeth in group I with no gap between the residual gutta-percha and the post were found to be healthy, while 10% (n = 2) were found to be diseased (Figure 1). In group II, there were 66.7% (n = 22) of normal teeth and 33.3% (n = 11) of diseased teeth, with a gap of more than 0 mm to less than 1 mm between the post end and the remaining gutta-percha (Figure 2). However, 58.8% (n = 10) of group III patients with a gap of more than 1 mm between the post end and the remaining gutta-percha were found to be healthy, whereas 41.2% (n = 7) were found to be diseased. (Figure 3). A total of 32% (n = 16) endodontically treated teeth were found diseased and treated by the female students while 68% (n = 34) of teeth were found normal. A total of 20% (n = 4) endodontically treated teeth were found diseased and treated by the male students while 80% (n = 16) of teeth were found normal. (Figure 4 and Figure 5) The quadrant wise treated teeth included for follow up examinations were 36 maxillary anteriors, 8 maxillary posteriors, 12 mandibular anteriors, and 14 mandibular posteriors. Among the maxillary anteriors, 69.4% (n = 25) of teeth were found normal however 30.6% (n = 11) of teeth were found diseased. Among the maxillary posteriors, 50% (n = 4) of teeth were found normal however 50% (n = 4) of teeth were found diseased. Among the mandibular anteriors, 83.3% (n = 10) of teeth were found normal however 16.7% (n = 2) of teeth were found diseased. Among the mandibular posteriors, 78.6% (n = 11) of teeth were found normal however 21.4% (n = 3) of teeth were found diseased. (Figure 4 and Figure 5).
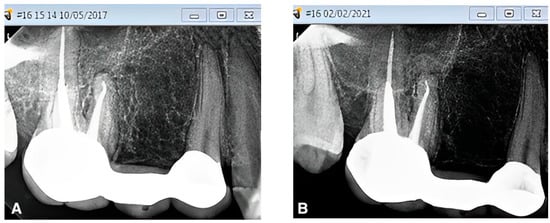
Figure 1.
(A,B). Peri-apical radiograph in Group I (no gap between cemented post and remaining gutta-percha) showing the PAI status, before and after 4 years of follow up using the CS-R4 program.

Figure 2.
(A,B). Peri-apical radiograph in Group II (gap of >0 but <1 mm between cemented post and remaining gutta-percha) showing the PAI status, before and after 4 years of follow up using the CS-R4 program.
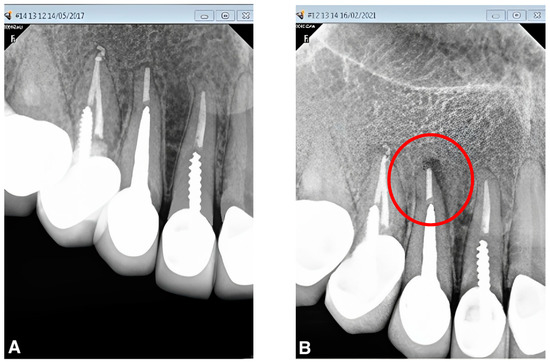
Figure 3.
(A,B). Peri-apical radiograph in Group III (gap of >1 mm between cemented post and remaining gutta-percha) showing the PAI status, before and after 4 years with periodontal inflammation and bone loss (red circle) of follow up using the CS-R4 program.
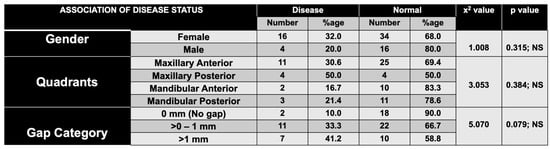
Figure 4.
Association of disease status with respect to gender, quadrant, and gap categories. NS = non-significant.
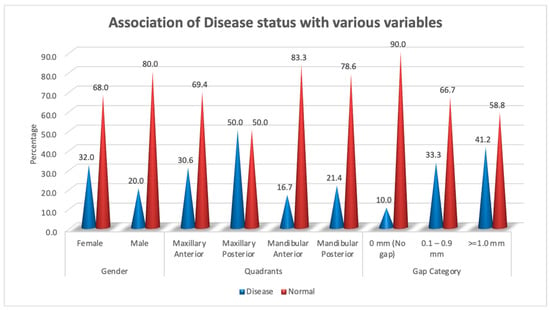
Figure 5.
Graphic illustration of association of disease status with respect to gender, quadrant, and gap categories.
4. Discussion
The cemented posts were divided into three groups based on the distance between the post end and the remaining gutta-percha: groups I had no space, group II had gaps that ranged from more than zero to less than one millimeter, whereas group III had gaps that were more than one millimeter. The gap between the post end and the residual gutta-percha was found to be >0.1 to less than 1 mm in group II, and 1 mm or more in group III for a total of 71.4% (n = 50) of the teeth treated by the undergraduate students. The frequency of a similar phenomenon was previously reported by Grieve and McAndrew who found gaps in 57% of cases examined [24]. The results of the current study showed that in endodontically treated teeth with post and core, the clinical outcome was considerably unfavorable when the space between the post end and residual gutta-percha was greater than 1 mm. The microleakage of saliva, dye, and anaerobic bacteria after post space preparation may explain the reason for these observations [25,26,27]. A total of 28.6% (n = 20) endodontically treated teeth were found diseased while 71.4% (n = 50) of teeth were found to be healthy. The findings of the current investigation were generally consistent with earlier literature. There was a gap between the remaining gutta-percha and the cemented post end in 58 (61.7%) of the treated teeth. Of all the cases, 37 cases (61%) were considered to be unhealthy, including those without a space between the post and the gutta-percha [19]. In group I, 90% of the teeth and in group II 66.7% of teeth were evaluated as normal; however, in group III 41.2% teeth were found diseased. The post and core treatments carried out by the undergraduate students may have contributed to the fact that the good favorable clinical outcome among the patients in this study was slightly lower than that reported in the literature. The performance rates of students who committed more procedural mistakes than experienced operators were found to be less favorable (48–70%) [28]. The most likely cause of this gap can be explained by the fact that there may be an inaccurate impression of the post space by the undergraduate students for cast post and core. For undergraduate students, however, it would have been challenging to choose the correct post size that matched the post area that had been made with the universal drill for the prefabricated glass fiber post. The present study utilized both the techniques of prefabricated glass fiber posts as well as of custom cast posts. Contrary to posterior teeth, due to their curved roots and elliptical or ribbon-shaped canals, anterior teeth give efficient retention and support via relatively long posts with a circular cross section. The metal cast posts are customized to the precise anatomy of the root canal which enhances the resistance and retention forms compared to prefabricated posts. In addition, cast post-and-core is the best treatment option when the angle of the core needs to be modified in relation to the root, when compromised root canal treated teeth serve as an abutment for a long span bridge, precise attachment or telescopic crown; or when compromised root filled teeth are subjected to extensive occlusal forces.
The method used to remove the gutta-percha from the root canal and the amount of gutta-percha left in the root canal have an impact on the integrity of the apical seal during post and core treatment. It can also be affected by the timing of the post space preparation, type of sealer used, and the obturation technique of how well the apical seal holds up during post space preparation [29]. Additionally, a pathway for bacterial invasion and recurrence of infection of the root canal system may also be created by the residual filling becoming loose, twisted, or vibrated during post space preparation [30,31]. It may be difficult to maintain the required post length for retention and a sufficient amount of gutta-percha for an adequate apical seal. According to research by Abramovitz et al., an apical seal is directly proportional to the length of the remaining obturated material in the root canal. It is important to maintain 4–5 mm of the remaining obturating material in the apical area to provide a safe margin [32]. However, it might not be possible to maintain the 4–5 mm of apical remaining gutta-percha in all post and core treated teeth. According to Haddix et al. [10], it may be essential to extend post preparations such that at-least 3 mm of the remaining gutta-percha is left in the root canal in cases where the root length is short. It is clinically accepted to extend the post space preparations such that 3 mm to 5 mm of gutta-percha remains at the apex of the tooth to maintain the apical seal. The dentinal walls of the post space prepared in the root canal must be clean for cement to adhere effectively [33]. To facilitate the cementation of the post with an adhesive resin cement and create hybrid zones between the resin cement and the dentinal tubules, the post space preparation should have a dentinal wall [34,35]. Remnants of root canal filling material should not be left inside the root canal, as they cannot provide reliable cementation or bonding to the dentinal walls [36,37]. The amount of filling material left on the canal walls is reduced as the canal is enlarged beyond the initial preparation size [38].
An unsatisfactory clinical outcome was observed in 50% of the maxillary posterior teeth where there was a gap of more than 1 mm between the post and the gutta-percha. These findings are consistent with those of some research studies, which found that treating anterior teeth had a more favorable outcome than treating posterior teeth [39,40]. Even though there are a number of different factors related to the clinical outcome of treatment, the anatomy of a multi-rooted tooth probably presents greater difficulties for the operator, especially for an undergraduate student. The post drill should have the same diameter as the prepared canal in order to reduce the amount of radicular dentine removal and retain the tooth’s fracture resistance. Since the educational institutions inside the Kingdom of Saudi Arabia have separate male and female training sections, where male undergraduate students can treat only male patients and female undergraduate students can treat only female patients, it was also planned for the present study to identify the treatment outcome performed by male and female undergraduate students separately. The inclusion of gender differences may have indicated competence gaps between undergraduate students of both sexes and may have called for more training for the identified gender. In the past, extracted natural teeth have been used to teach post- and core-treatment techniques in preclinical simulation clinics. The current experiences with natural teeth constraints include ethical obstacles, cross-infection needs, finding teeth with the appropriate tooth structure, and procuring teeth with the proper root canal anatomy. Natural tooth variations make it difficult to standardize, replicate, and maintain consistency in instructions and teaching by the instructors. This can lead to a diverse range of learning experiences for students. The use of artificial typodont teeth in simulation teaching for post and core training in fixed prosthodontics has several advantages, including uniformity of teeth, uniformity of techniques, lifelike appearance, facilitation of repeatable practical demonstrations, and being readily available. However, the anatomical simulation of real teeth, surface textures that differ from real teeth, and the expense of getting real teeth, models, and manikins are some of the known limitations. In addition cast post and core may not be indicated in teeth that cannot accommodate additional root preparation resulting from inadequate root dimensions or unsuitable internal morphology such as mandibular incisors and is another limitation of the study. According to Martino’s survival analysis, post-and-core restoration has a greater chance of lasting when the root of a tooth is encircled by more than 75% bone. Additionally, compared to the posts placed in the anterior area, post-and-core restorations placed in posterior teeth are considerably more likely to be successful. Compared to posts cemented with glass ionomer cement, posts cemented with resin or zinc phosphate cement had a much higher survival rate. Compared to a composite resin foundation or an interim restoration, the placement of a complete coverage crown has improved survival rates in the following order from highest to lowest: metal-ceramic, complete ceramic, complete metal [41]. The number of remaining walls could be another essential factor for root-filled teeth with post and core for their survival. Comparing the teeth with more than one wall to those with none or just one remaining wall, it appears that the survival rates of the latter are worse. The presence of proximal contacts enhances the survival probability of root filled teeth. Terminal teeth, and more so, those without any neighboring contacts, have inferior survival.
5. Conclusions
After the root-canal treatment, posts should be cemented such that the coronal end of the remaining gutta-percha is in contact with the apical end of post. An increase in gap between the remaining portion of gutta-percha and the apical part of the post end may result in an unhealthy periapical condition that is more likely to be accompanied by bone loss and periodontal disease. For all types of posts, an intraoral radiograph must be taken to measure the distance between the post end and the remaining gutta-percha prior to cementation. The undergraduate students’ preclinical laboratory training was adequate and clinically acceptable in terms of the space between cemented post ends and the remaining gutta-percha.
Author Contributions
Conceptualization, M.E.S., M.A., H.N., H.F.J., S.S.A., N.M.A. and S.M.A.; methodology, M.E.S., M.A., H.N., H.F.J., S.S.A., N.M.A. and S.M.A.; software, M.E.S., M.A., H.N. and, H.M.H.; validation, M.E.S., M.A., H.N., H.F.J., S.S.A., N.M.A. and S.M.A.; formal analysis, M.E.S., M.A. and H.N.; investigation, M.E.S., M.A. and H.N.; resources, H.M.H., J.A.F., M.A.O., H.A.A., H.A.D., N.H., A.M.M. and M.I.H.; data curation, H.M.H., J.A.F., M.A.O., H.A.A., H.A.D., N.H., A.M.M. and M.I.H.; writing—original draft preparation, M.E.S., M.A., H.N., H.F.J., S.S.A., N.M.A. and S.M.A.; writing—review and editing, M.E.S., M.A., H.N., H.F.J., S.S.A., N.M.A., S.M.A., H.M.H., J.A.F., M.A.O., H.A.A., H.A.D., N.H., A.M.M. and M.I.H.; supervision, M.E.S., M.A., H.N., H.F.J., S.S.A., N.M.A. and S.M.A.; project administration, M.E.S., M.A. and H.N. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The research protocol was approved by the standing committee for scientific research ethics, Jazan University (Reference number: REC42/1/051).
Informed Consent Statement
Not applicable.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Dudley, J. Implants for ageing population. Aust. Dent. J. 2015, 60, 28–43. [Google Scholar] [CrossRef] [PubMed]
- Torabinejad, M.; Anderson, P.; Bader, J.; Brown, L.J.; Chen, L.H.; Goodacre, C.J.; Kattadiyil, M.T.; Kutsenko, D.; Lozada, J.; Patel, R.; et al. Outcomes of root canal treatment and restoration, implant-supported single crowns, fixed partial dentures, and extraction without replacement: A systematic review. J. Prosthet. Dent. 2007, 98, 285–311. [Google Scholar] [CrossRef] [PubMed]
- Goracci, C.; Ferrari, M. Current perspectives on post systems: A literature review. Aust. Dent. J. 2011, 56, 77–83. [Google Scholar] [CrossRef]
- Theodosopoulou, J.N.; Chochlidakis, K.M. A systematic review of dowel (post) and core materials and systems. J. Prosthodont. 2009, 18, 464–472. [Google Scholar] [CrossRef]
- Schwartz, R.S.; Robbins, J.W. Post placement and restoration of endodontically treated teeth: A literature review. J. Endod. 2004, 30, 289–301. [Google Scholar] [CrossRef]
- Caputo, A.A.; Standlee, J.P. Pins and posts—Why, when and how. Dent. Clin. N. Am. 1976, 20, 299–311. [Google Scholar] [CrossRef]
- Mattison, G.D.; Delivanis, P.D.; Thacker, R.W.; Hassell, K.J. Effect of post preparation on the apical seal. J. Prosthet. Dent. 1984, 51, 785–789. [Google Scholar] [CrossRef] [PubMed]
- Cooney, J.P.; Caputo, A.A.; Trabert, K.C. Retention and stress distribution of tapered-end endodontic posts. J. Prosthet. Dent. 1986, 55, 540–546. [Google Scholar] [CrossRef]
- Jotkowitz, A.; Samet, N. Rethinking ferrule—A new approach to an old dilemma. Br. Dent. J. 2010, 209, 25–33. [Google Scholar] [CrossRef]
- Haddix, J.E.; Mattison, G.D.; Shulman, C.A.; Pink, F.E. Post preparation techniques and their effect on the apical seal. J. Prosthet. Dent. 1990, 64, 515–519. [Google Scholar] [CrossRef] [PubMed]
- Dhaded, N.; Uppin, V.M.; Dhaded, S.; Patil, C. Evaluation of immediate and delayed post space preparation on sealing ability of Resilon-Epiphany and Gutta percha-AH plus sealer. J. Conserv. Dent. 2013, 16, 514–517. [Google Scholar] [CrossRef] [PubMed]
- Attam, K.; Talwar, S. A laboratory comparison of apical leakage between immediate versus delayed post space preparation in root canals filled with Resilon. Int. Endod. J. 2010, 43, 775–781. [Google Scholar] [CrossRef]
- Madison, S.; Zakariasen, K.L. Linear and volumetric analysis of apical leakage in teeth prepared for posts. J. Endod. 1984, 10, 422–427. [Google Scholar] [CrossRef]
- Neagley, R.L. The effect of dowel preparation on the apical seal of endodontically treated teeth. Oral Surg. Oral Med. Oral Pathol. 1969, 28, 739–745. [Google Scholar] [CrossRef]
- Haralur, S.B.; Al-Malki, A.E. Student perception about efficacy of preclinical Fixed prosthodontic training to facilitate smooth transition to clinical context. J. Educ. Health Promot. 2014, 3, 73. [Google Scholar]
- Velayo, B.C.; Stark, P.C.; Eisen, S.E.; Kugel, G. Using dental students’ preclinical performance as an indicator of clinical success. J. Dent. Educ. 2014, 78, 823–828. [Google Scholar] [CrossRef] [PubMed]
- Perry, S.; Bridges, S.; Burrow, M.F. A review of the use of simulation in dental education. Simul. Healthc. 2015, 10, 31–37. [Google Scholar] [CrossRef] [PubMed]
- Dudley, J. In vitro assessment of simulation teeth in a pre-clinical teaching program. Saudi J. Oral Sci. 2018, 5, 75–79. [Google Scholar] [CrossRef]
- Joshua, M.; Iris, S.G.; Ayelet, G.; Benny, P. The Effect of the Distance between Post and Residual Gutta-Percha on the Clinical Outcome of Endodontic Treatment. J. Endod. 2005, 31, 177–179. [Google Scholar]
- Baruah, K.; Mirdha, N.; Gill, B.; Bishnoi, N.; Gupta, T.; Baruah, Q. Comparative Study of the Effect on Apical Sealability with Dif-ferent Levels of Remaining Gutta-Percha in Teeth Prepared to Receive Posts: An in vitro Study. Contemp. Clin. Dent. 2018, 9 (Suppl. S2), S261–S265. [Google Scholar]
- Reyhani, M.F.; Yavari, H.; Ghasemi, N.; Rahimi, S.; Barhaghi, M.H.; Mokhtari, H.; Sarikhani, P. Comparing the Coronal Seal of Dif-ferent Thicknesses of MTA with Gutta-Percha after Post Space Preparation. Sci. World J. 2015, 2015, 708639. [Google Scholar]
- Naim, H.; Ahmad, M.; Ageeli, A.A.; Abuarab, R.K.; Sayed, M.E.; Dewan, H.; Chohan, H.; Alshehri, A.H.; Wadei, M.H.D.A.; Alqahtani, S.M.; et al. Radiographic Evaluation of the Gap between Cemented Post and Remaining Gutta-Percha in Endodontically Treated Teeth Performed by Undergraduate Students: A Retrospective Cross-Sectional Study. Medicina 2023, 59, 502. [Google Scholar] [CrossRef]
- Orstavik, D. Time-course and risk analyses of the development and healing of chronic apical periodontitis in man. Int. Endod. J. 1996, 29, 150–155. [Google Scholar] [CrossRef] [PubMed]
- Grieve, A.R.; McAndrew, R. A radiographic study of post-retained crowns in patients attending a dental hospital. Br. Dent. J. 1993, 174, 197–201. [Google Scholar] [CrossRef] [PubMed]
- Barrieshi, K.M.; Walton, R.E.; Johnson, W.T.; Drake, D.R. Coronal leakage of mixed anaerobic bacteria after obturation and post space preparation. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 1997, 84, 310–314. [Google Scholar] [CrossRef]
- Wu, M.K.; Pehlivan, Y.; Kontakiotis, E.G.; Wesselink, P.R. Microleakage along apical root fillings and cemented posts. J. Prosthet. Dent. 1998, 79, 264–269. [Google Scholar] [CrossRef]
- Karapanou, V.; Vera, J.; Cabrera, P.; White, R.R.; Goldman, M. Effect of immediate and delayed post preparation on apical dye leakage using two different sealers. J. Endod. 1996, 22, 583–585. [Google Scholar] [CrossRef]
- Friedman, S. Treatment outcome and Prognosis of Endodontic Therapy. In Essential Endodontology; Orstavik, D., Pitt Ford, T.R., Eds.; Blackwell: Oxford, UK, 1998; pp. 367–391. [Google Scholar]
- Nagas, E.; Karaduman, E.; Sahin, C.; Uyanik, O.; Canay, S. Effect of timing of post space preparation on the apical seal when using different sealers and obturation techniques. J. Dent. Sci. 2016, 11, 79–82. [Google Scholar] [CrossRef]
- Padmanabhan, P.; Das, J.; Kumari, R.V.; Pradeep, P.R.; Kumar, A.; Agarwal, S. Comparative evaluation of apical microleakage in immediate and delayed post space preparation using four different root canal sealers: An in vitro study. J. Conserv. Dent. 2017, 20, 86–90. [Google Scholar] [PubMed]
- Chen, G.; Chang, C. The effect of immediate and delayed post-space preparation using extended working time root canal sealers on apical leakage. J. Dent. Sci. 2013, 8, 31–36. [Google Scholar] [CrossRef]
- Abramovitz, L.; Lev, R.; Fuss, Z.; Metzger, Z. The unpredictability of seal after post space preparation: A fluid transport study. J. Endod. 2001, 27, 292–295. [Google Scholar] [CrossRef]
- Morris, M.D.; Lee, K.W.; Agee, K.A.; Bouillaguet, S.; Pashley, D.H. Effects of sodium hypochlorite and RC-Prep on bond strengths of resin cement to endodontic surfaces. J. Endod. 2001, 27, 753–757. [Google Scholar] [CrossRef] [PubMed]
- Mannocci, F.; Innocenti, M.; Ferrari, M.; Watson, T.F. Confocal and scanning electron microscopic study of teeth restored with fiber posts, metal posts, and composite resins. J. Endod. 1999, 25, 789–794. [Google Scholar] [CrossRef] [PubMed]
- Ferrari, M.; Mannocci, F. A 1-bottle adhesive system for bonding a fiber post into a root canal: A SEM evaluation of the post-resin interface. Int. Endod. J. 2000, 33, 397–400. [Google Scholar] [CrossRef]
- Boone, K.J.; Murchison, D.F.; Schindler, W.G.; Walker, W.A., 3rd. Post Retention: The Effect of Sequence of Post- Space Preparation, Cementation Time, and Different Sealers. J. Endod. 2001, 27, 768–771. [Google Scholar] [CrossRef]
- Serafino, C.; Gallina, G.; Cumbo, E.; Ferrari, M. Surface debris of canal walls after post space preparation in endodontically treated teeth: A scanning electron microscopic study. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2004, 97, 381–387. [Google Scholar] [CrossRef]
- Hassanloo, A.; Watson, P.; Finer, Y.; Friedman, S. Retreatment efficacy of the Epiphany soft resin obturation system. Int. Endod. J. 2007, 40, 633–643. [Google Scholar] [CrossRef] [PubMed]
- Friedman, S.; Abitbol, S.; Lawrence, H.P. Treatment outcome in endodontics. The Toronto study. Phase I: Initial treatment. J. Endod. 2003, 29, 787–793. [Google Scholar] [CrossRef]
- Field, J.W.; Gutmann, J.L.; Solomon, E.S.; Rakusin, H. A clinical radiographic retrospective assessment of the success rate of single-visit root canal treatment. Int. Endod. J. 2004, 37, 70–82. [Google Scholar] [CrossRef]
- Martino, N.; Truong, C.; Clark, A.E.; O’Neill, E.; Hsu, S.M.; Neal, D.; Esquivel-Upshaw, J.F. Retrospective analysis of survival rates of post-and-cores in a dental school setting. J. Prosthet. Dent. 2020, 123, 434–441. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).