Towards a New Paradigm for Digital Health Training and Education in Australia: Exploring the Implication of the Fifth Industrial Revolution
Abstract
:Featured Application
Abstract
1. Introduction
2. Digital Health: Barrier and Solutions
2.1. Security and Privacy
2.2. Traceability and Safety
2.3. Standardisation and Interoperability
2.4. Resilience and Sustainability
2.5. Regulatory Policy and Framework
2.6. Equity
2.7. Education, Training and Awareness
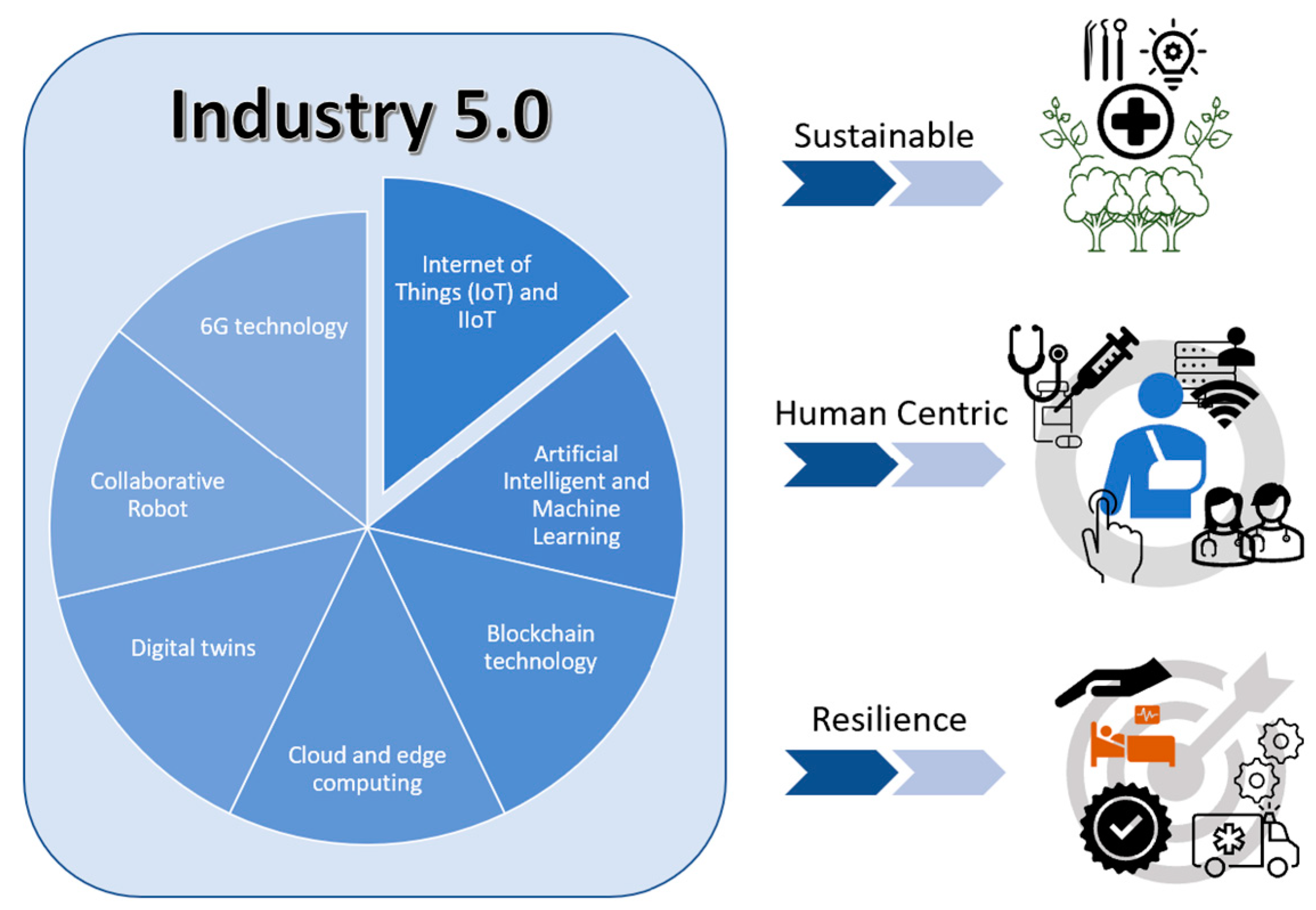
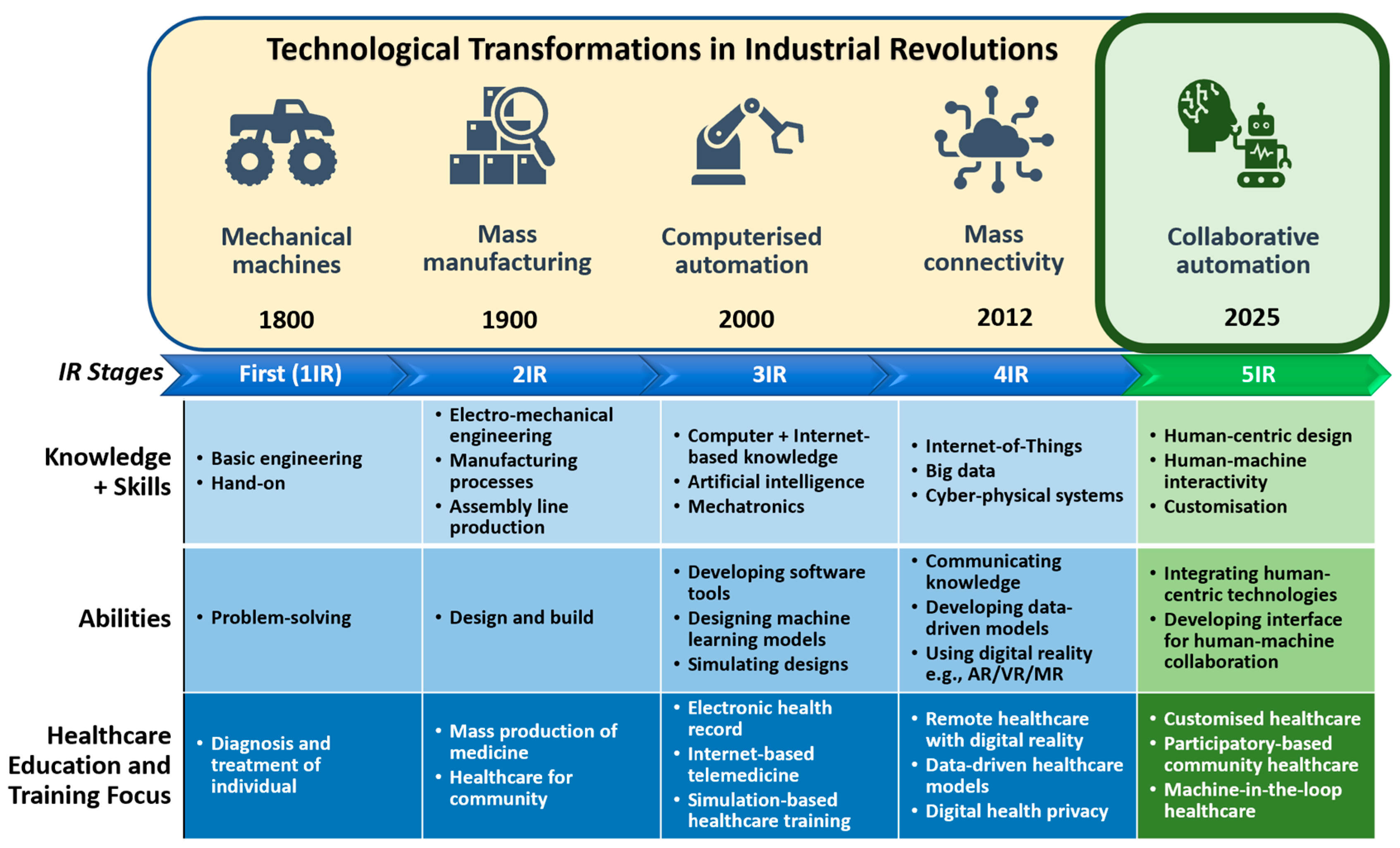
3. An outlook on the Integration of Industry 5.0 and Digital Health
3.1. Enabling Technologies
3.2. Prospects, Issues, and Challenges for the Healthcare Workforce
3.3. Australian Educational Context in Digital Health
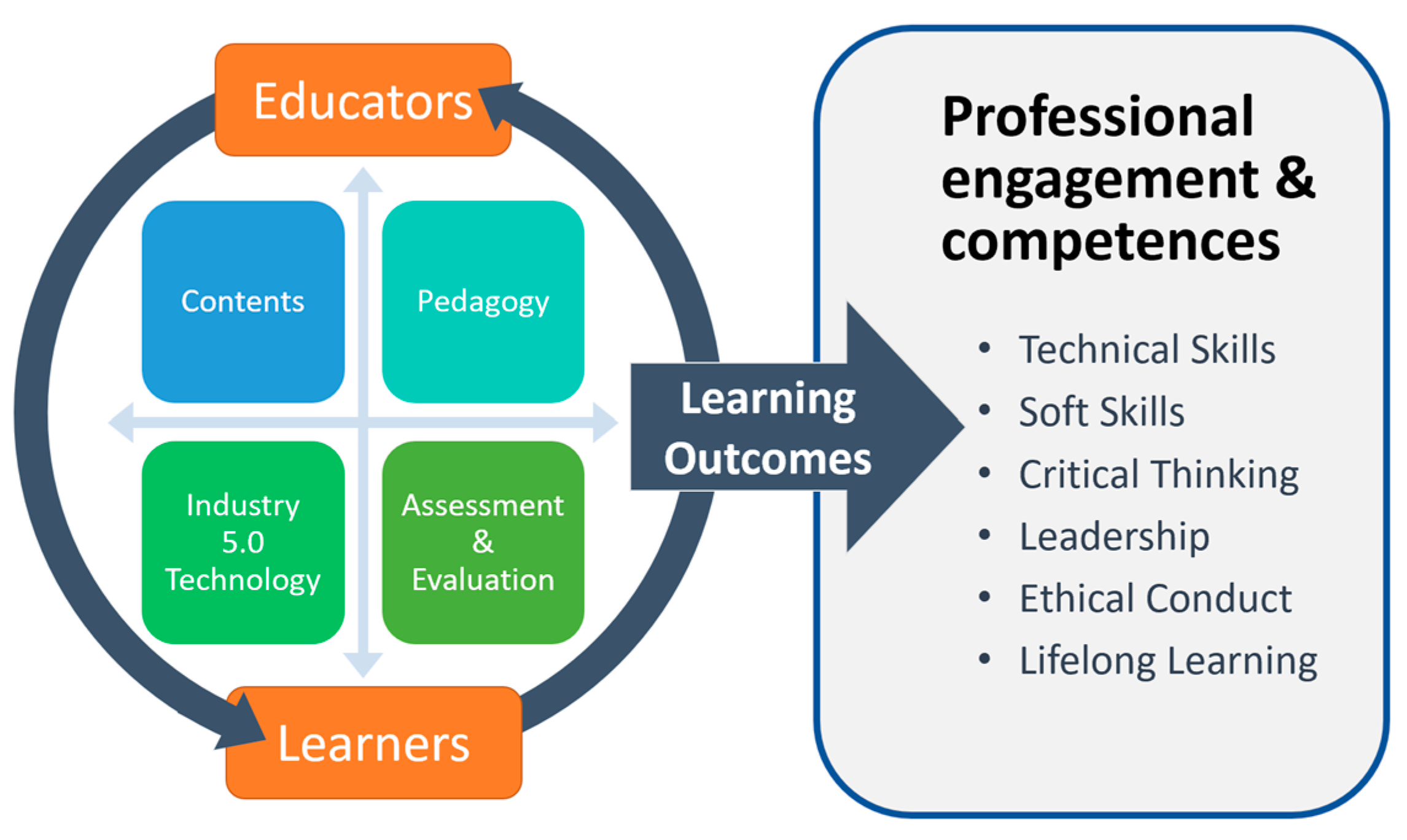
4. The Fifth Industrial Revolution and a New Teaching Paradigm for Digital Health
4.1. Learning Content and Source
4.2. Infrastructure, Resources and Technologies
4.3. Strategies to Reinvent Education Pedagogy
4.3.1. Experiential Learning in Project-Based Learning
4.3.2. Collaborative Learning
4.3.3. Transdisciplinary Learning
4.3.4. Lifelong Learning
4.3.5. Assessment Model
- Standardised assessments, such as hands-on laboratory work and structured clinical assessments;
- Reflective learning, involving self-analysing of a person’s own experiences and learning from past behaviours in order to maintain up-to-date knowledge and skills;
- Capstone projects;
- Electronic examination that contains different written examination formats, including short-answer, multiple-choice questions as an option.
4.3.6. Guided by Ethics
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| University/Title of Certificate | Entry Requirements | Subjects/Topics Covered | Outcomes |
|---|---|---|---|
| Australian College of Nursing/ Graduate Certificate in Digital Health 1 | Bachelor’s of Nursing or registered nurse equivalent qualification Or be currently employed in the clinical area of specialisation | Complete all of the following:
| Five major outcomes:
|
| Australian Catholic University/ Graduate Certificate in Digital Health 2 | Bachelor’s degree in health Bachelor’s degree in information technology | Complete any five subjects from below:
| Three major outcomes:
|
| Curtin University/Graduate Certificate in Big Data and Digital Health 3 | Bachelor’s degree or equivalent | Complete all of the following:
| Six major outcomes:
|
| Flinders University/Graduate Certificate in Digital Health Management 4 | healthcare or related undergraduate degree or equivalent qualification | Complete all the below:
| Three major outcomes:
|
| Griffith University/Graduate Certificate in Digital Health 5 | Bachelor’s degree; or a health-related diploma PLUS two years relevant work experience in the health- or age-care sector; or a minimum of five years equivalent full-time work experience in administrative, management and leadership roles within healthcare organisations | Complete all of the following:
complete any one of the following options:
| Two major outcomes:
|
| La Trobe University/Graduate Certificate in Digital Health 6 | Australian bachelor’s degree (or equivalent) | Complete any four subjects from the following options:
| Three major outcomes:
|
| Queensland University of Technology/Graduate Certificate in Digital Health Leadership and Management 7 | Bachelor’s degree (or higher qualification) in any discipline or diploma in any discipline followed by at least three (3) years professional experience, including at least one year in a supervisory or leadership role in any field | Complete all of the following:
| Five major outcomes:
|
| RMIT University/Graduate Certificate in Digital Health 8 | Bachelor’s degree or equivalent, or higher-level qualification, in any discipline and at least 1 year’s full-time experience in a health care or social setting Or At least five years full-time experience working in health or social care | Complete all of the following:
complete any one from the following options:
| Four major outcomes:
|
| The University of Sydney/Graduate Certificate in Digital Health and Data Science 9 | An honours bachelor’s degree or A bachelor’s degree and a minimum of two years of relevant work experience | Complete all of the following:
| Two major outcomes:
|
| The University of Queensland/ Graduate Certificate in Clinical Informatics and Digital Health 10 | An honours bachelor’s degree or A bachelor’s degree and two years of relevant work experience | Complete all of the following:
| Two major outcomes:
|
| University of Melbourne/ Graduate Certificate in Health Informatics and Digital Health 11 | A health-related degree or equivalent; or an undergraduate degree in a cognate discipline or equivalent | Complete all of the following:
| Three major outcomes:
|
| University of Tasmania/ Graduate Certificate in Digital Health 12 | Bachelor level (AQF7) or higher (or equivalent); in healthcare, or communications technology or Be working in a healthcare or IT setting | Complete all of the following:
| Four major outcomes:
|
References
- Petersen, A. Digital Health and Technological Promise: A Sociological Inquiry; Taylor & Francis Group: Milton, Abingdon, UK, 2019. [Google Scholar]
- Surya Darmawan, E.; Laksono, S. The New Leadership Paradigm in Digital Health and Its Relations to Hospital Services. J. Ilmu Kesehat. Masy. 2021, 12, 89–103. [Google Scholar] [CrossRef]
- Smuck, M.; Odonkor, C.A.; Wilt, J.K.; Schmidt, N.; Swiernik, M.A. The emerging clinical role of wearables: Factors for successful implementation in healthcare. NPJ Digit. Med. 2021, 4, 45. [Google Scholar] [CrossRef] [PubMed]
- Zuehlke, D. SmartFactory—Towards a factory-of-things. Annu. Rev. Control 2010, 34, 129–138. [Google Scholar] [CrossRef]
- European Commission; Directorate-General for Research Innovation; Breque, M.; De Nul, L.; Petridis, A. Industry 5.0: Towards a Sustainable, Human-Centric and Resilient European Industry; Publications Office: Luxembourg, 2021. [Google Scholar]
- Lu, Y.; Zheng, H.; Chand, S.; Xia, W.; Liu, Z.; Xu, X.; Wang, L.; Qin, Z.; Bao, J. Outlook on human-centric manufacturing towards Industry 5.0. J. Manuf. Syst. 2022, 62, 612–627. [Google Scholar] [CrossRef]
- European Commission; Directorate-General for Research Innovation; Renda, A.; Schwaag Serger, S.; Tataj, D.; Morlet, A.; Isaksson, D.; Martins, F.; Mir Roca, M. Industry 5.0, a transformative Vision for Europe: Governing Systemic Transformations towards a Sustainable Industry; Publications Office of the European Union: Luxembourg, 2022. [Google Scholar]
- Kolade, O.; Owoseni, A. Employment 5.0: The work of the future and the future of work. Technol. Soc. 2022, 71, 102086. [Google Scholar] [CrossRef]
- Vicente, A.M.; Ballensiefen, W.; Jönsson, J.-I. How personalised medicine will transform healthcare by 2030: The ICPerMed vision. J. Transl. Med. 2020, 18, 180. [Google Scholar] [CrossRef]
- Ong, J.; Parchment, V.; Zheng, X. Effective regulation of digital health technologies. J. R. Soc. Med. 2018, 111, 439–443. [Google Scholar] [CrossRef]
- Johnston, C. Digital Health Technologies: Law, Ethics, and the Doctor-Patient Relationship; Taylor & Francis Group: Milton, Abingdon, UK, 2022. [Google Scholar]
- Linwood, S.L. Digital Health; Exon Publications: Brisbane City, Australia, 2022; p. 148. [Google Scholar]
- O’Connor, G.E.; Myrden, S.; Alkire, L.; Lee, K.; Köcher, S.; Kandampully, J.; Williams, J.D. Digital health experience: A regulatory focus perspective. J. Interact. Mark. 2021, 56, 121–136. [Google Scholar] [CrossRef]
- Mbunge, E.; Muchemwa, B.; Jiyane, S.e.; Batani, J. Sensors and healthcare 5.0: Transformative shift in virtual care through emerging digital health technologies. Glob. Health J. 2021, 5, 169–177. [Google Scholar] [CrossRef]
- Janssen, A.; Kay, J.; Talic, S.; Pusic, M.; Birnbaum, R.J.; Cavalcanti, R.; Gasevic, D.; Shaw, T. Electronic Health Records That Support Health Professional Reflective Practice: A Missed Opportunity in Digital Health. J. Healthc. Inform. Res 2022, 6, 375–384. [Google Scholar] [CrossRef]
- Mondal, R.; Mishra, S. The Clinical Challenges for Digital Health Revolution. In Digital Health Transformation with Blockchain and Artificial Intelligence, 1st ed.; Chakraborty, C., Ed.; CRC Press: Boca Raton, FL, USA, 2022; p. 339. [Google Scholar]
- Elenko, E.; Speier, A.; Zohar, D. A regulatory framework emerges for digital medicine. Nat. Biotechnol. 2015, 33, 697–702. [Google Scholar] [CrossRef] [PubMed]
- Vignali, V.; Hines, P.A.; Cruz, A.G.; Ziętek, B.; Herold, R. Health horizons: Future trends and technologies from the European Medicines Agency’s horizon scanning collaborations. Front. Med. 2022, 9. [Google Scholar] [CrossRef] [PubMed]
- Ceross, A.; Bergmann, J. Evaluating the Presence of Software-as-a-Medical-Device in the Australian Therapeutic Goods Register. Prosthesis 2021, 3, 221–228. [Google Scholar] [CrossRef]
- Iqbal, J.D.; Biller-Andorno, N. The regulatory gap in digital health and alternative pathways to bridge it. Health Policy Technol. 2022, 11, 100663. [Google Scholar] [CrossRef]
- Torous, J.; Stern, A.D.; Bourgeois, F.T. Regulatory considerations to keep pace with innovation in digital health products. NPJ Digit. Med. 2022, 5, 121. [Google Scholar] [CrossRef]
- Haverinen, J.; Keränen, N.; Falkenbach, P.; Maijala, A.; Kolehmainen, T.; Reponen, J. Digi-HTA: Health technology assessment framework for digital healthcare services. Finn. J. eHealth eWelfare 2019, 11, 326–341. [Google Scholar] [CrossRef] [Green Version]
- Yan, K.; Balijepalli, C.; Druyts, E. The Impact of Digital Therapeutics on Current Health Technology Assessment Frameworks. Front. Digit. Health 2021, 3, 667016. [Google Scholar] [CrossRef]
- Mathews, S.C.; McShea, M.J.; Hanley, C.L.; Ravitz, A.; Labrique, A.B.; Cohen, A.B. Digital health: A path to validation. NPJ Digit. Med. 2019, 2, 38. [Google Scholar] [CrossRef] [Green Version]
- Rowen, D.; Azzabi Zouraq, I.; Chevrou-Severac, H.; van Hout, B. International Regulations and Recommendations for Utility Data for Health Technology Assessment. PharmacoEconomics 2017, 35, 11–19. [Google Scholar] [CrossRef]
- Von Huben, A.; Howell, M.; Carrello, J.; Norris, S.; Wortley, S.; Ritchie, A.; Howard, K. Application of a health technology assessment framework to digital health technologies that manage chronic disease: A systematic review. Int. J Ttechnol. Assess. Health Care 2022, 38, e9. [Google Scholar] [CrossRef]
- Richardson, S.; Lawrence, K.; Schoenthaler, A.M.; Mann, D. A framework for digital health equity. NPJ Digit. Med. 2022, 5, 119. [Google Scholar] [CrossRef] [PubMed]
- Lawrence, K. Digital Health Equity. In Digital Health; Linwood, S.L., Ed.; Exon Publications: Brisbane, Australia, 2022. [Google Scholar]
- Kaihlanen, A.-M.; Virtanen, L.; Buchert, U.; Safarov, N.; Valkonen, P.; Hietapakka, L.; Hörhammer, I.; Kujala, S.; Kouvonen, A.; Heponiemi, T. Towards digital health equity - A qualitative study of the challenges experienced by vulnerable groups in using digital health services in the COVID-19 era. BMC Health Serv. Res. 2022, 22, 188. [Google Scholar] [CrossRef] [PubMed]
- Kyaw, B.M.; Saxena, N.; Posadzki, P.; Vseteckova, J.; Nikolaou, C.K.; George, P.P.; Divakar, U.; Masiello, I.; Kononowicz, A.A.; Zary, N.; et al. Virtual Reality for Health Professions Education: Systematic Review and Meta-Analysis by the Digital Health Education Collaboration. J. Med. Internet Res. 2019, 21, e12959. [Google Scholar] [CrossRef] [Green Version]
- Tudor Car, L.; Soong, A.; Kyaw, B.M.; Chua, K.L.; Low-Beer, N.; Majeed, A. Health professions digital education on clinical practice guidelines: A systematic review by Digital Health Education collaboration. BMC Med. 2019, 17, 139. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dunleavy, G.; Nikolaou, C.K.; Nifakos, S.; Atun, R.; Law, G.C.Y.; Tudor Car, L. Mobile Digital Education for Health Professions: Systematic Review and Meta-Analysis by the Digital Health Education Collaboration. J. Med. Internet Res. 2019, 21, e12937. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Raja Santhi, A.A.; Muthuswamy, P.P. Industry 5.0 or industry 4.0S? Introduction to industry 4.0 and a peek into the prospective industry 5.0 technologies. Int. J. Interact. Des. Manuf. 2023, 17, 947–979. [Google Scholar] [CrossRef]
- Huang, S.; Wang, B.; Li, X.; Zheng, P.; Mourtzis, D.; Wang, L. Industry 5.0 and Society 5.0—Comparison, complementation and co-evolution. J. Manuf. Syst. 2022, 64, 424–428. [Google Scholar] [CrossRef]
- Breque, M.; De Nul, L.; Petridis, A. Industry 5.0: Towards a sustainable, human-centric and resilient European industry; Publications Office of the European Union: Luxembourg, 2021. [Google Scholar]
- Moosavi, J.; Bakhshi, J.; Martek, I. The application of industry 4.0 technologies in pandemic management: Literature review and case study. Healthc. Anal. 2021, 1, 100008. [Google Scholar] [CrossRef]
- Kasza, J. Forth Industrial Revolution (4 IR): Digital Disruption of Cyber – Physical Systems. World Sci. News 2019, 134, 118–147. [Google Scholar]
- Adel, A. Future of industry 5.0 in society: Human-centric solutions, challenges and prospective research areas. J. Cloud Comput. 2022, 11, 40. [Google Scholar] [CrossRef]
- Sahal, R.; Alsamhi, S.H.; Brown, K.N. Personal Digital Twin: A Close Look into the Present and a Step towards the Future of Personalised Healthcare Industry. Sensors 2022, 22, 5918. [Google Scholar] [CrossRef] [PubMed]
- Haghi, M.; Thurow, K.; Stoll, R. Wearable Devices in Medical Internet of Things: Scientific Research and Commercially Available Devices. Healthc. Inf. Res 2017, 23, 4–15. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fatima, Z.; Tanveer, M.H.; Waseemullah; Zardari, S.; Naz, L.F.; Khadim, H.; Ahmed, N.; Tahir, M. Production Plant and Warehouse Automation with IoT and Industry 5.0. Appl. Sci. 2022, 12, 2053. [Google Scholar] [CrossRef]
- Chi, H.R.; Wu, C.K.; Huang, N.-F.; Tsang, K.-F.; Radwan, A. A Survey of Network Automation for Industrial Internet-of-Things Towards Industry 5.0. IEEE Trans. Ind. Inform. 2023, 19, 2065–2077. [Google Scholar] [CrossRef]
- Zong, L.; Memon, F.H.; Li, X.; Wang, H.; Dev, K. End-to-End Transmission Control for Cross-Regional Industrial Internet of Things in Industry 5.0. IEEE Trans. Ind. Inform. 2022, 18, 4215–4223. [Google Scholar] [CrossRef]
- Glaros, C.; I. Fotiadis, D. Wearable Devices in Healthcare. In Intelligent Paradigms for Healthcare Enterprises; G. Silverman, B., Jain, A., Ichalkaranje, A., C. Jain, L., Eds.; Springer: Berlin/Heidelberg, Germany, 2005; pp. 237–264. [Google Scholar]
- Wan, S.; Nappi, M.; Chen, C.; Berretti, S. Guest Editorial Emerging IoT-Driven Smart Health: From Cloud to Edge. IEEE J.Biomed.Health Inform. 2022, 26, 937–938. [Google Scholar] [CrossRef]
- Shahzadi, S.; Iqbal, M.; Dagiuklas, T.; Qayyum, Z.U. Multi-access edge computing: Open issues, challenges and future perspectives. J. Cloud Comput. 2017, 6, 30. [Google Scholar] [CrossRef]
- Abiodun, K.M.; Adeniyi, E.A.; Awotunde, J.B.; Chakraborty, C.; Aremu, D.R.; Adebiyi, A.A.; Adebiyi, M.O. Blockchain and Internet of Things in Healthcare Systems Prospects, Issues, and Challenges. In Digital Health Transformation with Blockchain and Artificial Intelligence, 1st ed.; Chakraborty, C., Ed.; CRC Press: Boca Raton, FL, USA, 2022; p. 339. [Google Scholar]
- Swain, A.; Mohanta, B.K.; Jena, D. Security, Privacy Issues, and Challenges in Adoption of Smart Digital Healthcare. In Digital Health Transformation with Blockchain and Artificial Intelligence, 1st ed.; Chakraborty, C., Ed.; CRC Press: Boca Raton, 2022; p. 339. [Google Scholar]
- Arumugam, S.K.; Sharma, A.M. Chapter Four—Blockchain: Opportunities in the healthcare sector and its uses in COVID-19. In Lessons from COVID-19; Kaklauskas, A., Abraham, A., Okoye, K., Guggari, S., Eds.; Academic Press: Cambridge, MA, USA, 2022; pp. 61–94. [Google Scholar]
- Qahtan, S.; Sharif, K.Y.; Zaidan, A.A.; Alsattar, H.A.; Albahri, O.S.; Zaidan, B.B.; Zulzalil, H.; Osman, M.H.; Alamoodi, A.H.; Mohammed, R.T. Novel Multi Security and Privacy Benchmarking Framework for Blockchain-Based IoT Healthcare Industry 4.0 Systems. IEEE Trans.Industr. Inform. 2022, 18, 6415–6423. [Google Scholar] [CrossRef]
- Academy of Medical Royal Colleges. Artificial Intelligence in Healthcare; Academy of Royal Medical Colleges: London, UK, 2019; p. 40. [Google Scholar]
- Yigzaw, K.Y.; Olabarriaga, S.D.; Michalas, A.; Marco-Ruiz, L.; Hillen, C.; Verginadis, Y.; de Oliveira, M.T.; Krefting, D.; Penzel, T.; Bowden, J.; et al. Chapter 14—Health data security and privacy: Challenges and solutions for the future. In Roadmap to Successful Digital Health Ecosystems; Hovenga, E., Grain, H., Eds.; Academic Press: Cambridge, MA, USA, 2022; pp. 335–362. [Google Scholar]
- Borges do Nascimento, I.J.; Marcolino, M.S.; Abdulazeem, H.M.; Weerasekara, I.; Azzopardi-Muscat, N.; Gonçalves, M.A.; Novillo-Ortiz, D. Impact of Big Data Analytics on People’s Health: Overview of Systematic Reviews and Recommendations for Future Studies. J. Med. Internet. Res. 2021, 23, e27275. [Google Scholar] [CrossRef]
- Mayer-Schönberger, V.; Ingelsson, E. Big Data and medicine: A big deal? J. Intern. Med. 2018, 283, 418–429. [Google Scholar] [CrossRef] [Green Version]
- Alazab, M.; Khan, L.U.; Koppu, S.; Ramu, S.P.; Iyapparaja, M.; Boobalan, P.; Baker, T.; Maddikunta, P.K.R.; Gadekallu, T.R.; Aljuhani, A. Digital Twins for Healthcare 4.0—Recent Advances, Architecture, and Open Challenges. IEEE Consum. Electron. Mag. 2022, 1–8. [Google Scholar] [CrossRef]
- Venkatesh, K.P.; Raza, M.M.; Kvedar, J.C. Health digital twins as tools for precision medicine: Considerations for computation, implementation, and regulation. NPJ Digit. Med. 2022, 5, 150. [Google Scholar] [CrossRef] [PubMed]
- Kaur, M.J.; Mishra, V.P.; Maheshwari, P. The Convergence of Digital Twin, IoT, and Machine Learning: Transforming Data into Action. In Digital Twin Technologies and Smart Cities; Farsi, M., Daneshkhah, A., Hosseinian-Far, A., Jahankhani, H., Eds.; Springer International Publishing: Cham, Switzerland, 2020; pp. 3–17. [Google Scholar]
- Wang, K.-J.; Lee, Y.-H.; Angelica, S. Digital twin design for real-time monitoring – a case study of die cutting machine. Int. J. Prod. Res. 2021, 59, 6471–6485. [Google Scholar] [CrossRef]
- Laubenbacher, R.; Sluka, J.P.; Glazier, J.A. Using digital twins in viral infection. Science 2021, 371, 1105–1106. [Google Scholar] [CrossRef] [PubMed]
- Hassani, H.; Huang, X.; MacFeely, S. Impactful Digital Twin in the Healthcare Revolution. Big Data Cogn. Comput. 2022, 6, 83. [Google Scholar] [CrossRef]
- Santos, J.A.M.; Lopes, M.R.; Viegas, J.L.; Vieira, S.M.; Sousa, J.M.C. Internal Supply Chain Digital Twin of a Pharmaceutical Company. IFAC-PapersOnLine 2020, 53, 10797–10802. [Google Scholar] [CrossRef]
- Holland, J.; Kingston, L.; McCarthy, C.; Armstrong, E.; O’Dwyer, P.; Merz, F.; McConnell, M. Service Robots in the Healthcare Sector. Robotics 2021, 10, 47. [Google Scholar] [CrossRef]
- Roshan, M.C.; Pranata, A.; Isaksson, M. Robotic Ultrasonography for Autonomous Non-Invasive Diagnosis—A Systematic Literature Review. IEEE Trans. Med. Robot. Bionics 2022, 4, 863–874. [Google Scholar] [CrossRef]
- Bader, K.B.; Hendley, S.A. In Vitro Testing of a Cobot System to Assist Histotripsy Clot Ablation. In Proceedings of the 2020 IEEE International Ultrasonics Symposium (IUS), Las Vegas, NV, USA, 7–11 September 2020; pp. 1–3. [Google Scholar]
- Lopes, D.; Coelho, L.; Silva, M.F. Development of a Collaborative Robotic Platform for Autonomous Auscultation. Appl. Sci. 2023, 13, 1604. [Google Scholar] [CrossRef]
- Kim, J.H. 6G and Internet of Things: A survey. J. Manag. Anal. 2021, 8, 316–332. [Google Scholar] [CrossRef]
- Salameh, A.I.; El Tarhuni, M. From 5G to 6G—Challenges, Technologies, and Applications. Future Internet 2022, 14, 117. [Google Scholar] [CrossRef]
- Dao, N.-N. Internet of wearable things: Advancements and benefits from 6G technologies. Future Gener. Comput. Syst. 2023, 138, 172–184. [Google Scholar] [CrossRef]
- Javed, A.R.; Shahzad, F.; Rehman, S.u.; Zikria, Y.B.; Razzak, I.; Jalil, Z.; Xu, G. Future smart cities: Requirements, emerging technologies, applications, challenges, and future aspects. Cities 2022, 129, 103794. [Google Scholar] [CrossRef]
- Graur, F.; Puia, A.; Mois, E.I.; Moldovan, S.; Pusta, A.; Cristea, C.; Cavalu, S.; Puia, C.; Al Hajjar, N. Nanotechnology in the Diagnostic and Therapy of Hepatocellular Carcinoma. Materials 2022, 15, 3893. [Google Scholar] [CrossRef]
- Woźniak, M.; Płoska, A.; Siekierzycka, A.; Dobrucki, L.W.; Kalinowski, L.; Dobrucki, I.T. Molecular Imaging and Nanotechnology—Emerging Tools in Diagnostics and Therapy. Int. J. Mol. Sci. 2022, 23, 2658. [Google Scholar]
- Volkmar, W.; Tamer, E.; Beat, F.; Amy, B. The Growing Field of Nanomedicine and Its Relevance to Pharmacy Curricula. Am. J. Pharm. Educ. 2021, 85, 8331. [Google Scholar] [CrossRef]
- Barton, A.E.; Borchard, G.; Wacker, M.G.; Pastorin, G.; Saleem, I.Y.; Chaudary, S.; Elbayoumi, T.; Zhao, Z.; Flühmann, B. Need for Expansion of Pharmacy Education Globally for the Growing Field of Nanomedicine. Pharmacy 2022, 10, 17. [Google Scholar] [CrossRef]
- Li, J.; Carayon, P. Health Care 4.0: A Vision for Smart and Connected Health Care. IISE Trans. Healthc. Syst. Eng. 2021, 11, 171–180. [Google Scholar] [CrossRef]
- Williams, G.A.; Jacob, G.; Rakovac, I.; Scotter, C.; Wismar, M. Health professional mobility in the WHO European Region and the WHO Global Code of Practice: Data from the joint OECD/EUROSTAT/WHO-Europe questionnaire. Eur. J. Public Health 2020, 30, iv5–iv11. [Google Scholar] [CrossRef]
- Dumont, J.-C.; Zurn, P.; Church, J.; LeThi, C. International Mobility of Health Professionals and Health Workforce Management in Canada. In Myths and Realities; OECD Health Working Papers, No. 40; OECD Publishing: Paris, France, 2008. [Google Scholar] [CrossRef]
- Perezmitre, E.L.; Ali, S.; Peltonen, L.-M. Nursing Informatics Competencies for the Next Decade. In Nursing and Informatics for the 21st century, Embracing a Digital World: Nursing Education and Digital Health Strategies; Delaney, C.W., Ed.; Routledge: New York, NY, USA, 2022. [Google Scholar]
- Erkens, C.; Schimmer, T.; Dimich, N. Growing Tomorrow’s Citizens in Today’s Classrooms: Assessing Seven Critical Competencies (Teaching Strategies for Soft Skills and 21st-Century-Skills Assessment Methods); Solution Tree: Bloomington, IN, USA, 2018. [Google Scholar]
- Schwartz, J.; Hatfield, S.; Jones, R.; Anderson, S. What is the future of work? Redefining Work, Workforces, and Workplaces. Deloitte Insights, Deloitte Development LLC: Oakland, CA, USA, 2019; Available online: https://www2.deloitte.com/us/en/insights/focus/technology-and-the-future-of-work/redefining-work-workforces-workplaces.html (accessed on 16 January 2023).
- Rumbens, D.; Brown, D.; Bourke, J.; Ryan, L.; Mizrahi, J.; Smith, X. Directors’ playbook: The Future of Work; Research Series; Australian Institute of Company Directors: Sydney, Australia, 2018; Available online: https://www2.deloitte.com/content/dam/Deloitte/au/Documents/Economics/deloitte-au-economics-aicd-directors-playbook-future-work-291018.pdf (accessed on 16 January 2023).
- Australian Qualifications Framework Council. Australian Qualifications Framework. 2013. Available online: https://www.aqf.edu.au/publication/aqf-second-edition (accessed on 18 May 2023).
- Carayannis, E.G.; Christodoulou, K.; Christodoulou, P.; Chatzichristofis, S.A.; Zinonos, Z. Known Unknowns in an Era of Technological and Viral Disruptions—Implications for Theory, Policy, and Practice. J. Knowl. Econ. 2022, 13, 587–610. [Google Scholar] [CrossRef]
- Serger, S.; Malmberg, A.; Benner, M.; Goksör, M.; Hättestrand, C.; Kettis, Å.; Rindefjäll, T. Renewing Higher Education: Academic Leadership in Times of Transformation. Lund University: Lund, Sweden, 2021. [Google Scholar]
- Vilalta-Perdomo, E.; Michel-Villarreal, R.; Thierry-Aguilera, R. Integrating Industry 4.0 in Higher Education Using Challenge-Based Learning: An Intervention in Operations Management. Educ. Sci. 2022, 12, 663. [Google Scholar] [CrossRef]
- Carayannis, E.G.; Morawska-Jancelewicz, J. The Futures of Europe: Society 5.0 and Industry 5.0 as Driving Forces of Future Universities. J. Knowl. Econ. 2022, 13, 3445–3471. [Google Scholar] [CrossRef]
- Furusa, S.S.; Coleman, A. Factors influencing e-health implementation by medical doctors in public hospitals in Zimbabwe. S. Afr. J. Inf. Manag. 2018, 20, 1–9. [Google Scholar] [CrossRef]
- Mohamed Hashim, M.A.; Tlemsani, I.; Matthews, R. Higher education strategy in digital transformation. Educ. Inf. Technol. 2022, 27, 3171–3195. [Google Scholar] [CrossRef] [PubMed]
- Andrés Díaz, L. Engineering Education 5.0: Strategies for a Successful Transformative Project-Based Learning. In Insights Into Global Engineering Education After the Birth of Industry 5.0; Montaha, B., Ed.; IntechOpen: Rijeka, Croatia, 2022; Chapter 2; pp. 19–35. [Google Scholar]
- Martín Núñez, J.L.; Diaz Lantada, A. Artificial Intelligence Aided Engineering Education: State of the Art, Potentials and Challenges. Int. J. Eng. Educ. 2020, 36, 1740–1751. [Google Scholar]
- Rumbens, D.; Richardson, C.; Lee, C.; Mizrahi, J.; Roche, C. The Path to Prosperity: Why the Future of Work is Human. Deloitte: Sydney, Australia, 2019. [Google Scholar]
- Moraes, E.B.; Kipper, L.M.; Hackenhaar Kellermann, A.C.; Austria, L.; Leivas, P.; Moraes, J.A.R.; Witczak, M. Integration of Industry 4.0 technologies with Education 4.0: Advantages for improvements in learning. Interact. Technol. Smart Educ. 2022. ahead-of-print. [Google Scholar] [CrossRef]
- Catal, C.; Tekinerdogan, B. Aligning Education for the Life Sciences Domain to Support Digitalization and Industry 4.0. Procedia Comput. Sci. 2019, 158, 99–106. [Google Scholar] [CrossRef]
- Kuwabara, A.; Su, S.; Krauss, J. Utilizing digital health technologies for patient education in lifestyle medicine. Am. J. Lifestyle Med. 2020, 14, 137–142. [Google Scholar] [CrossRef]
- Pote, H.; Rees, A.; Holloway-Biddle, C.; Griffith, E. Workforce challenges in digital health implementation: How are clinical psychology training programmes developing digital competences? Digit. Health 2021, 7, 2055207620985396. [Google Scholar] [CrossRef]
- Diaz Lantada, A.; De Maria, C. Towards Open-Source and Collaborative Project-Based Learning in Engineering Education: Situation, Resources and Challenges. Int. J. Eng. Educ. 2019, 35, 1279–1289. [Google Scholar]
- Lundgren, C.; Molander, C. Teamwork in Medical Rehabilitation; Taylor & Francis Group: Portland, OR, USA, 2017. [Google Scholar]
- Broo, D.G.; Kaynak, O.; Sait, S.M. Rethinking engineering education at the age of industry 5.0. J. Ind. Inf. Integr. 2022, 25, 100311. [Google Scholar] [CrossRef]
- Broo, D.G. Transdisciplinarity and three mindsets for sustainability in the age of cyber-physical systems. J. Ind. Inf. Integr. 2022, 27, 100290. [Google Scholar] [CrossRef]
- Antoniou, P.E. Chapter Seven - Implementing digital learning for health. In Digital Innovations in Healthcare Education and Training; Konstantinidis, S.T., Bamidis, P.D., Zary, N., Eds.; Academic Press: Cambridge, MA, USA, 2021; pp. 103–125. [Google Scholar]
- Aungst, T.D.; Patel, R. Integrating digital health into the curriculum—considerations on the current landscape and future developments. J. Med. Educ. Curric. Dev. 2020, 7, 2382120519901275. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Azzopardi, L.M. Digital Health in Pharmacy Education: Faculty Perspective; International Pharmaceutical Federation (FIP): The Hague, The Netherlands, 2021. [Google Scholar]
- Longo, F.; Padovano, A.; Umbrello, S. Value-Oriented and Ethical Technology Engineering in Industry 5.0: A Human-Centric Perspective for the Design of the Factory of the Future. Appl. Sci. 2020, 10, 4182. [Google Scholar] [CrossRef]


| Enabling Technology in Industrial Revolution | Clinical Applications | References |
|---|---|---|
| Internet of Things (IoT) and Industrial Internet of Things (IIoT) |
| [40] |
| [41,42,43] | |
| [44] | |
| Cloud and Edge Computing |
| [45] |
| [46] | |
| Blockchain Technology for Healthcare |
| [47,48] |
| [49] | |
| [50] | |
| Artificial Intelligent (AI) and Machine Learning (ML) |
| [51] |
| [48,52] | |
| Big Data and Analytics |
| [53] |
| [54] | |
| Digital Twins and Real-Time Data |
| [55] |
| [56,57,58] | |
| [59] | |
| [60] | |
| [61] | |
| Collaborative Robots (Cobots) and Automation |
| [62] |
| [63,64] | |
| [65] | |
| 6G Technology |
| [66,67] |
| [68] | |
| [69] | |
| Nanotechnology |
| [70] |
| [71] | |
| [72,73] |
| University/Title of Certificate | Pedagogical Interaction | Technological Competences | Assessments | Industry Partners or Work Integrated Learning |
|---|---|---|---|---|
| Australian College of Nursing/Graduate Certificate in Digital Health 1 | Online | Machine Learning | Research-led teaching; Evidence-based | No |
| Australian Catholic University/Graduate Certificate in Digital Health 2 | Online, webinars, discussion forums | Not clear | Group work, essay; reflective journals; | No |
| Curtin University/Graduate Certificate in Big Data and Digital Health 3 | On campus; Online; | Machine learning for data analytics | Research Projects; Reflective journals; | No |
| Flinders University/Graduate Certificate in Digital Health Management 4 | On campus; Online | Virtual hospitals; intelligence, the Internet of Things (IoT), digital safety, and cybersecurity in the health- and age-care sectors | Not Clear | Recognised by the Australasian Institute of Digital Health and the Australasian College of Health Service Management for continuing professional development (CPD) points eligibility |
| Griffith University/Graduate Certificate in Digital Health 5 | On campus; Online; | Teaching focus: technologies associated with health information; data and information acquisition, structure, use and value; the ability to utilise digital health research, as well as project management skills, to support managing resources and delivering initiatives in health information applications | Reflective journals; | Accredited by the Australasian College of Health Service Management (ACHSM). |
| La Trobe University/Graduate Certificate in Digital Health 6 | On campus; Online; Role plays; Discussions; | Not clear; as general as the interface of healthcare and digital technologies | Presentation; Reports; | No |
| Queensland University of Technology/Graduate Certificate in Digital Health Leadership and Management 7 | On campus; Online | Not clear | Not clear | No |
| RMIT University/Graduate Certificate in Digital Health 8 | Online learning; structured hand-on activities; | AT and IoT, electronic health records (EHR) | Case study; reports; vodcast; presentation; project portfolio | Digital Health CRC, Telstra Health, AWS |
| The University of Sydney/Graduate Certificate in Digital Health and Data Science 9 | On campus | Different eHealth tools | Case study | No |
| The University of Queensland/Graduate Certificate in Clinical Informatics and Digital Health 10 | Online | Application/contextualisation; interaction/collaboration; reflection/evaluation [information from Discover UQ’s Graduate Certificate in Clinical Informatics and Digital Health—Faculty of Medicine—University of Queensland] | Not Clear | Eligible memberships of the Australian Institute of Digital Health support progression to a clinical fellowship with the Australian Institute of Digital Health (AIDH) |
| University of Melbourne/Graduate Certificate in Health Informatics and Digital Health 11 | Online, face-to-face, workshops, seminar of group interaction | health informatics tools; | Assignments; individual and team reports; quizzes; presentations. | No |
| University of Tasmania/Graduate Certificate in Digital Health 12 | Online | Electronic health records (EHR) | Presentation; Essay; Report | No |
| University/Title of Degrees | Outcomes | Pedagogical Interaction | Technological Competences | Assessments | Industry Partners or Work Integrated Learning |
|---|---|---|---|---|---|
| La Trobe University/Master of Digital Health # | Three major outcomes: 1. Demonstrate proficient knowledge about core health; 2. Use of information and technology in healthcare; 3. Understand public health policy and planning | Online, face-to-face, workshops, seminars of group interaction | health informatics tools; | Assignments, individual and team reports, quizzes, and presentations. | Not clear |
| The University of Sydney/Master of Digital Health and Data Science § | Two major outcomes: 1. Gain advanced skills to develop, implement, evaluate, and manage data-driven technologies; 2. Ultimately stand out in a global healthcare sector on the cusp of a major transformation through big data, machine learning, and computation. | Face-to-face | Not clear | Not clear | No |
| Flinders University/Bachelor of Health Science (Digital Health) ‡ | Nine major outcomes, including the aims to develop skills in identifying and utilizing big data sets ethically, applying knowledge of big data, visualisation, governance, and machine learning to effectively communicate health data, while maintaining cultural awareness and using in-demand technologies. | Online; face-to-face | Not clear | Essays and presentations, | Not clear |
| Western Sydney University/Master of Health Science (Digital Health) * | Three major outcomes: 1. Study contemporary issues associated with information management in healthcare organisations with the integration of a sound understanding of the impact of digital health; 2. Develop innovation and entrepreneurship and research and development in the digital health space | On campus; Online | Not clear | Work-integrated learning. A Master’s in Health Science (Health Service Management) has professional accreditation with the Australasian College of Health Service Management (ACHSM). |
| University/Title of Certificate | Courses Co-Delivered by School/Discipline Area | Approach to Addressing Issues in Section 2.1, Section 2.2, Section 2.3, Section 2.4, Section 2.5 and Section 2.6 | Industry 5.0 Integration Status |
|---|---|---|---|
| Australian College of Nursing/Graduate Certificate in Digital Health 1 | Nursing |
| Sustainable: Not clear Human Centric: Discuss the principles of user-centric design Resilience: Not clear |
| Australian Catholic University/Graduate Certificate in Digital Health 2 | Health Sciences, Information Technology, Law |
| Sustainable: address equity perspective of healthcare Human Centric: Not clear Resilience: explore risks and benefits of digital health developments |
| Curtin University/ Graduate Certificate in Big Data and Digital Health 3 | Health Sciences, Population Health, Computing and Mathematical Sciences |
| Sustainable: explore ways in which big data analytics can be used to reduce waste and inefficiency in healthcare systems Human Centric: Covers the importance of putting patients at the centre of digital health initiatives Resilience: Not clear |
| Flinders University/ Graduate Certificate in Digital Health Management 4 | Computer Science, Medicine |
| Sustainable: Not clear Human Centric: strong emphasis on patient engagement and ethical considerations in the use of digital health technologies. Resilience: explores ways in which digital health technologies bring disaster response, telemedicine, and remote patient monitoring |
| Griffith University/ Graduate Certificate in Digital Health 5 | Medicine, Nursing and Midwifery, Information and Communication Technology |
| Sustainable: explores development and implementation of projects and programs relating to this critical area in both organisations and professional practice Human Centric: Not Clear Resilience: Not Clear |
| La Trobe University/ Graduate Certificate in Digital Health 6 | Nursing and Midwifery, Psychology and Public Health, Computer Science and Information Technology |
| Sustainable: strong emphasis on reducing waste and inefficiency in healthcare systems by implementing automation Human Centric: Not Clear Resilience: enhancing the capacity of healthcare systems to respond to crises and emergencies |
| Queensland University of Technology/Graduate Certificate in Digital Health Leadership and Management 7 | Computer Science, Management |
| Sustainable: consider the environmental and resource implications of digital health technologies and develop solutions that efficiently utilise resources while minimising waste and energy consumption Human Centric: prioritise a patient-centred approach Resilience: Not Clear |
| RMIT University/ Graduate Certificate in Digital Health 8 | Health and Biomedical Sciences, Engineering |
| Sustainable: exploring automating processes and reducing the use of paper-based systems in digital health solutions Human Centric: Strong emphasis on patients centric in digital health systems design, services, and ubiquity of technologies, applied telehealth and virtual care Resilience: Not Clear |
| The University of Sydney/Graduate Certificate in Digital Health and Data Science 9 | Public Health, Computer Science |
| Sustainable: By analysing large amounts of data, healthcare professionals can identify areas where resources are being underutilised and implement strategies to reduce waste and improve efficiency Human Centric: Not Clear Resilience: importance of using the data to its stakeholders (patients, clinicians, society etc.) by taking into account of the ethics, privacy, security and measurable benefits |
| The University of Queensland/ Graduate Certificate in Clinical Informatics and Digital Health 10 | Health and Rehabilitation Sciences, Information Technology, Electrical Engineering |
| Sustainable: Focus on entrepreneurship to drive innovation and entrepreneurship in digital health Human Centric: No Clear Resilience: specifically on the use of data analytics |
| University of Melbourne/Graduate Certificate in Health Informatics and Digital Health 11 | Engineering, Health Sciences |
| Sustainable: Focus on usage of information and communication technologies in healthcare, including the rise of Digital Health, eHealth, Mobile Health and Telehealth Human Centric: Not Clear Resilience: Critically evaluate approaches to information systems and information technology in contemporary healthcare |
| University of Tasmania/ Graduate Certificate in Digital Health 12 | Medicine, Health Sciences |
| Sustainable: Not Clear Human Centric: Not Clear Resilience: Focus on security and data while also considering ethical, social and economic considerations. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pang, T.Y.; Lee, T.-K.; Murshed, M. Towards a New Paradigm for Digital Health Training and Education in Australia: Exploring the Implication of the Fifth Industrial Revolution. Appl. Sci. 2023, 13, 6854. https://doi.org/10.3390/app13116854
Pang TY, Lee T-K, Murshed M. Towards a New Paradigm for Digital Health Training and Education in Australia: Exploring the Implication of the Fifth Industrial Revolution. Applied Sciences. 2023; 13(11):6854. https://doi.org/10.3390/app13116854
Chicago/Turabian StylePang, Toh Yen, Tsz-Kwan Lee, and Manzur Murshed. 2023. "Towards a New Paradigm for Digital Health Training and Education in Australia: Exploring the Implication of the Fifth Industrial Revolution" Applied Sciences 13, no. 11: 6854. https://doi.org/10.3390/app13116854







